Abstract
AIM
The aim of this study was to compare patterns of utilization of NSAIDs for musculoskeletal disorders (MSD) by occupation in a general employed population.
METHODS
This was a secondary analysis of the CADEUS cohort study on 5651 actively employed patients, who submitted at least one claim for the reimbursement of a NSAID dispensation for a MSD between August 2003 and July 2004, in the French National Healthcare Insurance database. Questionnaires were sent to prescribing physicians to obtain diagnoses and the medical history, and to patients for their occupation, height and weight and smoking status. Multivariate logistic regression was used to study the determinants of a heavy use of NSAIDs defined as ‘over four dispensations in one year with less than two months between any two’.
RESULTS
Factors associated with heavy use of NSAIDs were age (Odds ratio (OR): 1.8 (ten years), 95% confidence interval (CI): 1.6–1.9), osteoarthritis (versus back pain) (OR: 1.8, 95% CI: 1.5–2.1), body mass index (superior to 30) (OR: 1.8, 95% CI: 1.5–2.2), and occupation (blue collar versus white collar workers) (OR: 1.4, 95% CI: 1.2–1.6). Blue collar workers also had a 20% higher prevalence of 5-year history of dyspepsia. No difference was observed between sexes or in the use of COX-2 selective inhibitors between occupations.
CONCLUSION
Factors associated with occupational constraints that contribute to the severity of MSDs, may explain the heavier use of NSAIDs among blue collar workers in spite of a concurrent and past medical history of adverse reactions to this type of medication.
Keywords: drug utilization, nonsteroidal anti-inflammatory drugs, occupations, pharmacoepidemiology
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
To our knowledge, no study has ever described the intensity of nonsteroidal anti-inflammatory drug (NSAID) utilization in an employed population by occupation.
As the use of NSAIDs carries a well-known risk of adverse effects, this risk adds to the burden of musculoskeletal disorders in employed populations.
Information on utilization of NSAIDs in this context will help to better characterize and prevent this risk.
WHAT THIS STUDY ADDS
In spite of a previous history of dyspepsia, blue collar workers had the highest rate of chronic and continuous utilization of nonselective NSAIDs.
No clustering of cyclooxygenase-2 selective NSAID utilization according to a previous history of dyspepsia was observed among blue collar workers.
The association between chronicity of NSAID utilization and occupation was independent of medical indication for the prescription and other lifestyle factors.
Musculoskeletal disorders (MSDs) are the first cause of disability in working populations worldwide [1]. Part of this burden is probably associated with adverse reactions to nonsteroidal anti-inflammatory drugs (NSAIDs), but no study to date has described the magnitude of the problem. In the year 2000, the French health authorities commissioned a large study called CADEUS (Cox-2 and conventional non-selective NSAIDs–description of users) to describe the population of users with respect to indication, medication utilization, especially gastroprotective agents, previous cardiovascular (CV) and gastrointestinal (GI) history [2]. The study confirmed, in the general adult population, the hypothesis of a channelling effect of selective cyclooxygenase (COX)-2 agents towards patients at higher GI risk or to older patients, but not at CV risk [3]. The CADEUS study provided a unique opportunity to look at NSAID utilization by occupation, accounting for diagnostic indication and history of gastric problems.
Methods
Briefly, the CADEUS study was a national prospective cohort study that included 45217 patients who received at least one prescription for NSAID by a physician between August 2003 and July 2004 in the French National Healthcare Insurance database that covers 83% of the population in France. Farmers and independent workers are covered by a different insurance and are not included in this study. Detailed methodology has been described elsewhere [2, 3]. During the study period, subjects who were ≥20 years old were randomly sampled every month without replacement within the database, among those who submitted a claim for an NSAID prescription (oral administration, initial or renewal) during the month preceding their sampling date. Another inclusion criterion was having submitted at least one claim for healthcare services in the 6 months previous to the NSAID prescription. The index date was the date of the NSAID prescription (Figure 1). Patients and their prescribing physicians were invited to participate by filling and returning by mail a questionnaire on socio-demographic characteristics, diagnosis associated with the NSAID prescription at inclusion in the cohort, past medical history, risk factors and hospitalizations since drug acquisition. Diagnoses and medical history were obtained from physicians using a checklist. Weight, height and current cigarette smoking were those reported by the patients. No reminder was sent. For each respondent, healthcare resources used in the 6 months before and 6 months after inclusion (12 months in total) were extracted from the database, which included all healthcare services reimbursed such as prescription drugs, physician and other health professional consultations, and hospitalizations. For prescription drugs it includes the name of the prescriber. As the response rate depended on both physicians and patients returning the mailed questionnaire and was expected to be low with this type of study, recruitment continued until the target number of subjects was reached. In the CADEUS study the final response rate was 20.9% for patients and 32.4% for physicians. Examination of nonresponders revealed no difference form responders by sex, age, geographical region, CV or GI medical history or delivery of NSAIDs and gastroprotective agents [4].
Figure 1.
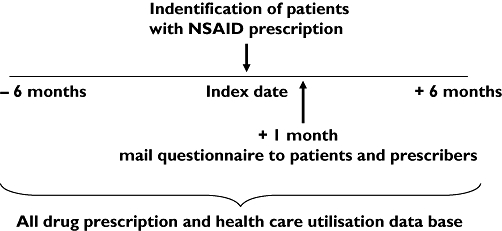
Summary of patients’ recruitment and data collection – August 2003 to July 2004
This analysis was restricted to individuals who reported being actively employed at the time of the survey. Patients reported their current occupation or, if not active at the time of the survey, the occupation they had held the longest. Occupations were divided into four categories: managerial and liberal professions; professions in education, healthcare and specialized technicians; administrative and utility services and commerce; and skilled and unskilled labour, material handlers and drivers. In the multivariate analysis, the first two categories were grouped under white collar workers and the last two under blue collar workers [5]. Drugs dispensed were coded in the database using the Anatomical Therapeutic Chemical (ATC) international classification system. For inclusion, NSAIDs with the M01A code were considered. Utilization of NSAID drugs was categorized in a semiquantitative indicator that combined the number of claims during the year of observation and the delays in days between each claim. Four groups were then created: punctual with one to three prescriptions in 1 year, intermittent with four to nine and at least one prescription-free interval of ≥2 months, chronic with four to nine and <2 months between any two successive prescriptions, and finally continuous with ≥10 prescriptions in 12 months. Medications other than NSAIDs used during the year of observation were described by their broad ATC category. For example, drugs with the codes A02B included all medications relative to peptic ulcer and GI reflux disorders and symptoms. Multivariate stepwise logistic regression explored the association between chronic utilization of NSAIDs (chronic and continuous vs. punctual and intermittent) and occupation, controlling for age, sex, diagnosis, body mass index (BMI), smoking and history of CV and GI problems. As the crude odds ratios (ORs) were very close to the adjusted, only the latter and their 95% confidence intervals (CIs) were reported. All analyses were performed using SAS (version 8.1; SAS Institute, Cary, NC, USA).
This protocol was approved by the French National Data Protection Commission and the French National Council of Physicians, which are the legal authorities in France for research on human subjects. Signed consent was obtained from all participating patients.
Results
The analysis included 5651 patients who were actively employed (21.2% of the original cohort). The mean age of the cohort was 44.6 years (SD 10.0) and women were over-represented with nearly 60% of the cohort (Table 1). By far the most frequent diagnostic category leading to a NSAID prescription was back pain with 55.2% of the cohort, followed with musculo-tendinous pain and strain (24.9%) and osteoarthritis (13.1%). The NSAID prescription was initial in 67.0% of subjects (incident users) and a renewal in 33.0%. The services and commerce grouping was the most frequent with one-third of the study population (33.3%), where younger women were predominant (Table 2). The second most frequent occupational grouping, labour, material handling and driving (26.4%), had a predominance of younger men. As expected, personal characteristics of the cohort varied widely between occupational groupings (Table 2). There was a 10% difference in the prevalence of smoking, with the highest proportion in the labour and drivers category. Alcohol consumption (at least one drink per week) also showed variations between occupational groups but with frequencies that were high overall. The proportion of workers with a BMI ≥30 rose across the four occupational categories with a five-point difference between the extremes. Differences were less marked for the past medical history of hypercholesterolaemia, diabetes and CV diseases, and correlated with the male : female ratio in each group. The distribution of dyspepsia, however, showed a 21.1% difference between the lowest prevalence (9.7%) in the category managerial and liberal professions and the highest prevalence (12.3%) in services and commerce.
Table 1.
Description of the population random sample of employed persons who submitted a claim for reimbursement* of a nonsteroidal anti-inflammatory drug (NSAID) prescription in France 2003–2004 (n = 5651)
| Age of patients (mean, SD) | 44.6 (10.0) |
| Age categories, years (%) | |
| 20–29 | 8.9 |
| 30–39 | 21.6 |
| 40–49 | 32.5 |
| 50–59 | 34.3 |
| 60+ | 2.7 |
| Gender of patients (%) | |
| Male | 40.4 |
| Female | 59.6 |
| Occupational category of patients (%) | |
| Managerial, liberal profession | 16.0 |
| Education, healthcare, technicians | 21.9 |
| Services and commerce | 33.3 |
| Labour, material handling, driving | 26.4 |
| Unknown | 2.4 |
| Indication for NSAID prescription (%) | |
| Back pain, low-back pain, sciatica | 55.2 |
| Sprain, tendonitis, muscular pain | 24.9 |
| Osteoarthritis lower and upper limbs | 13.1 |
| Other musculoskeletal disorders | 6.7 |
Reimbursement national database covers 83% of the population in France.
Table 2.
Risk factors and medical history in employed persons who submitted a claim for reimbursement* of a nonsteroidal anti-inflammatory drug prescription in France 2003–2004 (n = 5651)
| Managerial liberal prof. (902) | Education healthcare technicians (1240) | Services commerce (1882) | Labour drivers (1494) | |
|---|---|---|---|---|
| Gender of patients (% male) | 57.3 | 38.6 | 14.4 | 66.2 |
| Age of patients (mean, SD) | 48.7 (9.3) | 46.2 (9.6) | 44.1 (10.3) | 44.0 (10.0) |
| Current smoking (%) | 17.8 | 20.3 | 22.0 | 27.3 |
| Alcohol consumption (%)† | 77.2 | 67.1 | 49.7 | 62.9 |
| Body mass index (%) | ||||
| ≥25 | 41.1 | 43.8 | 40.4 | 52.4 |
| ≥30 | 9.9 | 12.1 | 13.7 | 15.2 |
| Past medical history (%) | ||||
| Hypercholesterolaemia | 8.9 | 7.1 | 7.0 | 8.6 |
| Diabetes | 1.5 | 1.6 | 1.5 | 2.1 |
| Cardiovascular diseases‡ | 1.5 | 0.9 | 0.8 | 1.8 |
| Dyspepsia | 9.7 | 10.1 | 12.3 | 11.9 |
Reimbursement national database covers 83% of the population in France.
Any consumption above one drink per week; 7.4% missing values.
Cardiovascular diseases = ischaemic, cardiac insufficiency and stroke.
Table 3 shows the drug prescriptions and medical consultations used in the cohort. Slightly over 10% of NSAID prescriptions were in the Coxib category, with a higher utilization in the category education, healthcare and technicians category (13.7%) than in the category labour and drivers (11.4%). The reverse pattern was observed in the use of analgesics, with a higher prevalence in the latter category (86.3%) and in the category services and commerce (86.7%). The category services and commerce also consumed more peptic ulcer medication (46.4%), CV and antihypertensive medication (52.4%), and psychotropic drugs (anxiolytics 31.4%, sedatives 22.2% and antidepressants 20.3%). Together, the services and commerce grouping, and the labour and drivers grouping (blue collar workers) had a lower prevalence of COX-2 utilization and a higher utilization of analgesics and peptic ulcer medication. Prevalence of consultation in physical therapy, rheumatology and gastroenterology was higher in the first two occupational groupings (white collar workers) than in the last two.
Table 3.
One-year consultations and drug prescriptions* in employed persons who submitted a claim for reimbursement† of a nonsteroidal anti-inflammatory drug (NSAID) prescription in France 2003–2004 (n = 5651)
| Managerial liberal prof. (902) | Education healthcare technicians (1240) | Services commerce (1882) | Labour drivers (1494) | |
|---|---|---|---|---|
| NSAID prescription‡ (%) | ||||
| Nonselective NSAIDs | 87.8 | 86.3 | 87.9 | 88.6 |
| COX-2 selective inhibitors | 12.2 | 13.7 | 12.1 | 11.4 |
| Other drug prescription§ (%) | ||||
| Analgesics¶ | 75.8 | 82.9 | 86.7 | 86.3 |
| Peptic ulcer medication | 41.3 | 41.9 | 46.4 | 43.7 |
| Cardiovascular–antihypertensive | 40.8 | 44.1 | 52.4 | 43.1 |
| Antihistamines | 29.7 | 26.1 | 29.3 | 24.0 |
| Anxiolytics | 21.3 | 22.5 | 31.4 | 20.7 |
| Hypnotics and sedatives | 14.9 | 16.4 | 22.2 | 16.7 |
| Antidepressants | 13.9 | 15.9 | 20.3 | 12.2 |
| Anti-asthmatics | 15.1 | 13.9 | 17.1 | 15.6 |
| Acetylsalicylic acid | 8.7 | 6.8 | 7.3 | 5.9 |
| Consultations (%) | ||||
| General practitioner | 93.9 | 98.2 | 98.8 | 99.1 |
| Physical therapy | 36.9 | 40.0 | 36.2 | 30.9 |
| Rheumatology | 19.4 | 15.4 | 16.4 | 13.6 |
| Gastroenterology | 5.3 | 5.4 | 4.4 | 3.7 |
At least one reimbursement in the national database.
Reimbursement national database covers 83% of the population in France.
By definition 100% of the study population received a prescription for an NSAID at least once
Drugs in the table have been dispensed at least once during the year of observation.
Excluding acetylsalicylic acid used at dosage for cardiovascular prevention.
There was a clear gradient in the proportion of chronic users of NSAIDs (vs. punctual users) across the four occupational groupings with, respectively, from managerial to labour, 13.9, 14.7, 16.5 and 16.6% (Table 4). The gradient was greater when looking at the continuous users with, respectively, 4.8, 7.7, 10.4 and 9.7%, and, when excluding Coxib users and retaining only nonselective NSAIDs, 2.1, 4.8, 6.5 and 6.6%. In the multivariate analyses, variables that were independently associated with chronic use of NSAIDs (chronic and continuous vs. punctual and intermittent) were age (10-year OR 1.8, 95% CI 1.6, 1.9), osteoarthritis diagnosis (vs. back pain OR 1.8, 95% CI 1.5, 2.1), having a BMI ≥30 (OR 1.8, 95% CI 1.5, 2.2) and being a blue collar worker (vs. white collar worker OR 1.4, 95% CI 1.2, 1.6) (Table 5). Sex was not associated with chronic or continuous use of NSAIDs when all variables were included in the model, and no interaction was found between occupation and any of the other variables in the model.
Table 4.
Profile* of nonsteroidal anti-inflammatory drug (NSAID) utilization by occupational category
| Managerial liberal prof. (902) | Education healthcare technicians (1240) | Services commerce (1882) | Labour drivers (1494) | |
|---|---|---|---|---|
| Categories of NSAID utilization (%)† | ||||
| All AINS | ||||
| Punctual | 66.3 | 61.5 | 56.1 | 55.6 |
| Intermittent | 15.0 | 16.1 | 17.0 | 18.2 |
| Chronic | 13.9 | 14.7 | 16.5 | 16.6 |
| Continuous | 4.8 | 7.7 | 10.4 | 9.7 |
| Nonselective NSAIDs | ||||
| Punctual | 69.1 | 63.9 | 61.2 | 59.1 |
| Intermittent | 12.5 | 14.1 | 15.6 | 16.0 |
| Chronic | 10.7 | 11.2 | 12.3 | 13.8 |
| Continuous | 2.1 | 4.8 | 6.5 | 6.6 |
| COX-2 selective inhibitors | ||||
| Punctual | 13.5 | 12.9 | 14.7 | 12.3 |
| Intermittent | 1.0 | 1.3 | 1.6 | 1.3 |
| Chronic | 3.1 | 3.2 | 3.7 | 3.1 |
| Continuous | 1.8 | 2.1 | 2.5 | 2.0 |
Categories of NSAID utilization defined by number of prescription reimbursed during one year: Punctual, 1–3; Intermittent, 4–9 with at least one 2-month prescription-free interval; Chronic, 4–9 with intervals between any two <2 months; Continuous, ≥10 prescriptions.
Percentages are not mutually exclusive; column total may add to >100%.
Table 5.
Factors associated with chronicity of nonsteroidal anti-inflammatory drug utilization in the active employed population*(n = 5249)
| Odds ratio | 95% CI | |
|---|---|---|
| Sex | ||
| Male | 1.0 | – |
| Female | 1.1 | 0.97, 1.3 |
| Age (10 years) | 1.8 | 1.6, 1.9 |
| Indication | ||
| Back pain | 1.0 | – |
| Osteoarthritis | 1.8 | 1.5, 2.1 |
| All others | 0.7 | 0.6, 0.8 |
| Occupation | ||
| White collar† | 1.0 | – |
| Blue collar | 1.4 | 1.2, 1.6 |
| Body mass index | ||
| <30 | 1.0 | – |
| ≥30 | 1.8 | 1.5, 2.2 |
Multiple stepwise logistic regression, model including all variables in the table; smoking and past history of gastrointestinal problems did not enter the final model; chronic users defined as ≥10 prescriptions issued in 1 year, or 4 to 9 with <2 months between two successive prescriptions.
White collar workers included the categories managerial and liberal professions, and professions in education and healthcare and specialized technicians; blue collar workers included the categories services and commerce, and labour, material handlers, drivers.
Discussion
This study has shown a 40% higher probability of chronic utilization of NSAIDs and a threefold higher proportion of continuous users among blue collar workers compared with their white collar counterparts. This result was consistent with a higher use of analgesics and NSAIDs in blue collar workers described earlier in the French population [6]. In our study, the association between occupational grouping and chronicity of utilization of NSAIDs for MSDs remained after controlling for sex, age, diagnosis, BMI, smoking and past history of GI problems. We could not measure the prevalence in the use of NSAIDs as the study population included only NSAID users. Mortensen et al. described the prevalence of NSAID utilization in blue and white collar workers from a National database study in Denmark [7] and showed prevalence rate ratios up to 1.6 in favour of blue collar workers. Our results are complementary, showing that the NSAID excess utilization in these workers is not only in terms of prevalence but also in intensity, with an OR of 1.4 for heavy utilization.
The main strength of the study was its mode of recruitment, which was without bias with regard to diagnosis or occupation. The French Insurance database includes 83% of the population and specifically excludes farmers and independent workers, to whom the results cannot be extrapolated. Few studies of this size have included information on diagnoses and medical history directly from the prescribing physician and on personal lifestyle factors from the patients. The main weakness resulting from this strategy was a low response rate, 20.9% for patients and 32.4% for physicians, which was comparable to other similar studies [8, 9]. This means that, to include 45 217 patients in this cohort, 222 879 patient–physician pairs had to be identified in the database and were contacted to fill out the study questionnaire. Due to the large population, no reminder was sent to nonresponders. The French Health Insurance database provided a description of nonresponding patients, allowing comparison with responders [2, 4]. The data suggested no evidence for major selection bias by age, gender, geographical area, history of CV or GI problems or prescription of NSAIDs or gastroprotective agents.
This study relied on drug dispensation as a measure of utilization. Discrepancies between physician prescribing, pharmacist dispensing and the actual consumption of a drug represent a limitation in the interpretation of this type of information. The accuracy of the French National Healthcare Insurance database has been evaluated at >98% after the introduction of the bar coding system at the pharmacies [10]. The issue of differences between dispensing and consumption has been looked at specifically in that database and was shown to be equivalent in drugs used for chronic conditions such as MSDs [11]. Nevertheless, the categories of utilization used in this analysis can only be broadly interpreted as intensity of utilization, punctual to continuous, over the study period. Another issue that represents a potential source of error in the actual prevalence of NSAID utilization is the use of over-the-counter medications. If these various effects were differential between occupations, they could bias be results by introducing a confounding effect. As drug dispensations were obtained from a large population database, and differences in the effect size for chronic utilization of NSAIDs by occupations were large, we do not believe that these potential biases could solely explain the results.
In this study, occupational groupings were broad, restricted to four categories into which patients self-selected in the questionnaire the category that fitted best their main occupation. Categories were named so that the first (managerial and liberal professions) would represent occupations with low physical demands, and the last (labour, material handlers and drivers) high physical demands. The notion of gradient of intensity of physical demands across the four categories remains therefore qualitative at best. The gradient in the proportion of smokers across the four occupational groupings provided evidence in support of a gradient with physical demands of the job, these two variables being known to correlate with socioeconomic status [1, 12].
As occupation is closely related to socioeconomic status, the excess use of NSAIDs among blue collar workers can reflect differences that are beyond occupation. Indeed, French surveys on adherence to clinical guidelines on osteoarthritis have shown that more than half of the patients treated believed that their medication was for long-term use [13]. However, physical constraints at the job, severity of MSD injuries and the precarious nature of the job are characteristics of unskilled blue collar workers that can explain a greater use of NSAIDs in relation to MSDs [14, 15]. Blue collar workers have been shown to have more disability from osteoarthritis, especially in occupations where osteoarthritis begins at a young age [16, 17].
Whatever the reasons for a greater use of NSAIDs among blue collar workers, the potential harm to the digestive system that can result is not speculative. The proportions of continuous NSAID users across the four occupational groupings (Table 4) was similar to the distribution of dyspepsia (Table 2) and of current use of anti-ulcer medications (Table 3). This is contrary to findings of three other studies that showed a lower use of nonselective NSAIDs in patients with a previous history of gastropathy or a prior prescription of gastroprotective agents, called channelling effect [3, 18]. In those studies, however, occupation was not accounted for in the analyses. It would therefore appear that the channelling of NSAID by digestive complications is confounded by occupation, which has concealed the real burden of NSAID secondary effects in blue collar occupational categories. In the CLASS study, for example, the incidence of symptomatic ulcers among chronic users of nonselective NSAIDs was 2.9% and for digestive complications 1.3% [19]. A 40% excess of heavy NSAID utilization among blue collar workers would translate into a significant excess of preventable events in these populations. In clinical practice guidelines for MSDs such as osteoarthritis, little is written concerning the occupational history [20]. Our study supports the recommendation of enquiring about occupation in the management of MSDs in order to reduce risks associated with the heavy utilization of NSAIDs. Further research should be conducted in order to better characterize GI risks associated with the chronic use of NSAIDs in blue collar workers. In conclusion, factors associated with occupational constraints that contribute to the severity of MSDs may explain the heavier use of NSAIDs among blue collar workers in spite of a concurrent and past medical history of adverse reactions to this type of medication.
Competing interests
None to declare.
The CADEUS study was conducted under a partnership agreement between the Caisse Nationale d'Assurance Maladie des Travailleurs Salariés, the Direction Générale de la Santé, the ComitéÉconomique des Produits de Santé, Pfizer Inc., Merck and Co. and Université Victor Segalen Bordeaux 2. The study was supported by Pfizer Inc. and Merck and Co. The authors gratefully thank all the patients and physicians who agreed to participate in this study. They also thank the persons who contributed to the study, the list of whom can be found at the following address: http://www.pharmacologie.u-bordeaux2.fr/CADEUS/.
REFERENCES
- 1.World Health Organization Scientific Group. Geneva: WHO; [last accessed 8 February 2008]. The Burden of Musculoskeletal Conditions at the Start of the New Millenium. WHO Technical Report Series 919. 218 pages. Available at http://whqlibdocint/trs/WHO_TRS_919.pdf. [PubMed] [Google Scholar]
- 2.Depont F, Fourrier A, Merliere Y, Droz C, Amouretti M, Begaud B, Benichou J, Moride Y, Blin P, Moore N, CADEUS Team The CADEUS study: methods and logistics. Pharmacoepidemiol Drug Saf. 2007;16:571–80. doi: 10.1002/pds.1348. [DOI] [PubMed] [Google Scholar]
- 3.Depont F, Fourrier A, Merliere Y, Droz C, Amouretti M, Begaud B, Benichou J, Moride Y, Velo GP, Sturkenboom M, Blin P, Moore N, on behalf of the CADEUS team Channelling of COX-2 inhibitors to patients at higher gastrointestinal risk but not at lower cardiovascular risk: the Cox2 inhibitors and tNSAIDs description of users (CADEUS) study. Pharmacoepidemiol Drug Saf. 2007;16:891–900. doi: 10.1002/pds.1388. [DOI] [PubMed] [Google Scholar]
- 4.Fourrier-Réglat A, Droz-Perroteau C, Bénichou J, Depont F, Amouretti M, Bégaud B, Moride Y, Blin P, Moore N, the CADEUS team Impact of prescriber nonresponse on patient representativeness. Epidemiology. 2008;19:186–90. doi: 10.1097/EDE.0b013e31816326e9. [DOI] [PubMed] [Google Scholar]
- 5.Hébert F, Duguay P, Massicotte P, Levy M. Revision of Occupational Categories Used in the Surveillance of Occupational Injuries. Montréal: Quebec Research Institute in Occupational Health and Safety; 1996. technical guide R-137. 52 pages (in French. [Google Scholar]
- 6.Fautrel B, Hilliquin P, Rozenberg S, Allaert FA, Coste P, Leclerc A, Rossignol M. Impact of osteoarthritis: results of a nationwide survey of 10 000 patients consulting for OA. Joint Bone Spine. 2005;72:235–40. doi: 10.1016/j.jbspin.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen JT, Olesen AV, Boggild H, Olsen J, Westgard-Nielsen NC. Socioeconomic correlates of drug use based on prescription data: a population-based cross-sectional register study in Denmark 1999. Dan Med Bull. 2007;54:62–6. [PubMed] [Google Scholar]
- 8.Czernichow S, Flahault A. Phone prompt or mailed reminder for increasing response rate among investigators? a randomized trial in the Sentinelles network. Rev Epidemiol Sante Publique. 2001;49:93–4. in French. [PubMed] [Google Scholar]
- 9.Harrison RA, Cock D. Increasing response to a postal survey of sedentary patients – a randomised controlled trial. BMC Health Serv Res. 2004;4:31. doi: 10.1186/1472-6963-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kusnik-Joinville O, Weill A, Salanave B, Ricordeau P, Allemand H. Prevalence and treatment of diabetes in France: trends between 2000 and 2005. Diabetes Metab. 2008;34:266–72. doi: 10.1016/j.diabet.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Noize P, Moore N, Lechevallier-Michel N, Fourrier-Réglat A, the 3C Study Group Comparison of patient interviews and computerized database for determination of drug exposure in pharmacoepidemiology: data from the Three-City (3C) study. Pharmacoepidemiol Drug Saf. 2006;15:S58–9. abstract. [Google Scholar]
- 12.Côté P, van der Velde G, Cassidy JD, Carroll LJ, Hogg-Johnson S, Holm LW, Carragee EJ, Haldeman S, Nordin M, Hurwitz EL, Guzman J, Peloso PM, Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4) Suppl.:S60–74. doi: 10.1097/BRS.0b013e3181643ee4. [DOI] [PubMed] [Google Scholar]
- 13.Denoeud L, Mazières B, Payen-Champenois C, Ravaud P. First line treatment of knee osteoarthritis in outpatients in France: adherence to the EULAR 2000 recommendations and factors influencing adherence. Ann Rheum Dis. 2005;64:70–4. doi: 10.1136/ard.2003.015263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bongers PM, Ijmker S, van den Heuvel S, Blatter BM. Epidemiology of work related neck and upper limb problems: psychosocial and personal risk factors (part I) and effective interventions from a bio behavioural perspective (part II) J Occup Rehabil. 2006;16:279–302. doi: 10.1007/s10926-006-9044-1. [DOI] [PubMed] [Google Scholar]
- 15.Leroux I, Dionne CE, Bourbonnais R, Brisson C. Prevalence of musculoskeletal activity limitation and associated factors among adults in the general population in the 1998 Quebec Health Survey. J Rheumatol. 2005;32:1794–804. [PubMed] [Google Scholar]
- 16.Rossignol M, Leclerc A, Allaert FA, Rozenberg S, Valat JP, Avouac B, Coste P, Litvak E, Hilliquin P. Primary osteoarthritis of hip, knee and hand in relation to occupational exposure. Occup Environ Med. 2005;62:772–7. doi: 10.1136/oem.2005.020057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossignol M, Leclerc A, Hilliquin P, Allaert FA, Rozenberg S, Valat JP, Avouac B, Coste P, Savarieau B, Fautrel B. Primary osteoarthritis and occupations: a national cross sectional survey of 10 412 symptomatic patients. Occup Environ Med. 2003;60:882–6. doi: 10.1136/oem.60.11.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moride Y, Ducruet T, Boivin JF, Moore N, Perreault S, Zhao S. Prescription channeling of COX-2 inhibitors and traditional nonselective nonsteroidal anti-inflammatory drugs: a population-based case–control study. Arthritis Res Ther. 2005;7:R333–42. doi: 10.1186/ar1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silverstein FE, Raich G, Goldstein JL, Simon LS, Pincus T, Whelton A, Makuch R, Eisen G, Agrawal NM, Stenson WF, Burr AM, Zhao WW, Kent JD, Lefkowith JB, Verburg KM, Geis GS. Gastrointestinal toxicity with celecocib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis. The CLASS study: a randomized controlled trial. JAMA. 2000;284:1247–55. doi: 10.1001/jama.284.10.1247. [DOI] [PubMed] [Google Scholar]
- 20.Poitras S, Avouac J, Rossignol M, Avouac B, Cedraschi C, Nordin M, Rousseaux C, Rozenberg S, Savarieau B, Thoumie P, Valat JP, Vignon E, Hilliquin P. A critical appraisal of guidelines for the management of knee osteoarthritis using Appraisal of Guidelines Research and Evaluation criteria. Arthritis Res Ther. 2007;9:R126. doi: 10.1186/ar2339. [DOI] [PMC free article] [PubMed] [Google Scholar]


