Abstract
Background
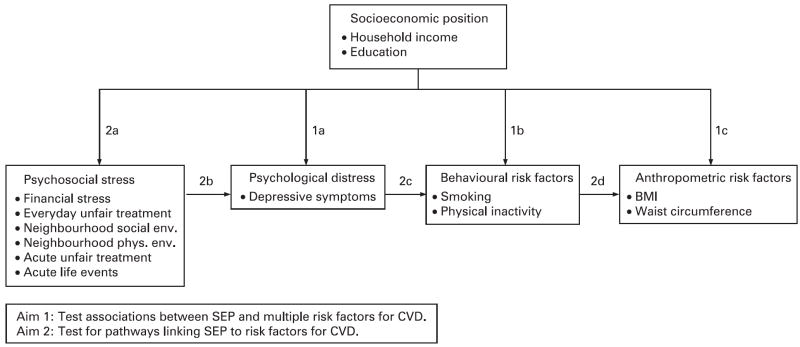
The study was designed to provide evidence of a cascade effect linking socioeconomic position to anthropometric indicators of cardiovascular disease (CVD) risk through effects on psychosocial stress, psychological distress and health-related behaviours, and consider implications for disease prevention and health promotion.
Methods
A cross-sectional stratified two-stage probability sample of occupied housing units in three areas of Detroit, Michigan, was used in the study. 919 adults aged ≥25 years completed the survey (mean age 46.3; 53% annual household income <$20 000; 57% non-Hispanic black, 22% Latino, 19% non-Hispanic white). Variables included self-report (eg, psychosocial stress, depressive symptoms, health behaviours) and anthropometric measurements (eg, waist circumference, height, weight). The main outcome variables were depressive symptoms, smoking status, physical activity, body mass index and waist circumference.
Results
Income was inversely associated with depressive symptoms, likelihood of current smoking, physical inactivity and waist circumference. These relationships were partly or fully mediated by psychosocial stress. A suppressor effect of current smoking on the relationship between depressive symptoms and waist circumference was found. Independent effects of psychosocial stress and psychological distress on current smoking and waist circumference were found, above and beyond the mediated pathways.
Conclusions
The results suggest that relatively modest improvements in the income of economically disadvantaged people can set in motion a cascade of effects, simultaneously reducing exposure to stressful life conditions, improving mental well-being, increasing health-promoting behaviours and reducing anthropometric risks associated with CVD. Such interventions offer important opportunities to improve population health and reduce health disparities.
Cardiovascular disease (CVD) is the largest contributor to all-cause mortality in the USA. Despite declines over the past 30 years, socioeconomic and racial disparities in CVD have increased because of uneven changes across population subgroups.1 2 Persistent relationships between socioeconomic position (SEP) and health over time have led to the development of conceptual models that posit that SEP influences health by contributing to unequal exposures to environments that erode health and unequal access to resources that promote or protect health.3-5
Substantial evidence links SEP with patterns of CVD morbidity and mortality.1 5-9 Furthermore, research has established associations between SEP and psychosocial stress,10-12 psychological distress,11 13 14 behavioural risks associated with CVD15-17 and anthropometric risk factors for CVD.6 18-20
Evidence from longitudinal studies suggests that psychosocial indicators substantially mediate long-term effects of SEP on health.5 21 Potential pathways for mediation effects between SEP and CVD include effects of psychosocial stress on depressed mood,11 14 22 23 smoking,24 physical inactivity24 and central adiposity.25-27 Depressive symptoms have been associated with smoking,15 physical inactivity28 29 and increased risk of cardiovascular mortality.22
Building on this research, we examined evidence for a chain of effects that link SEP to CVD risk through multiple pathways (fig 1), within a multiethnic urban sample. We first tested associations between SEP and psychological distress (depressive symptoms), behavioural risk factors (smoking, physical inactivity) and anthropometric risk factors for CVD (body mass index (BMI), waist circumference) (fig 1, pathways 1a–c). Next, we considered evidence for a cascade of effects, with SEP linked to psychological distress through exposure to psychosocial stress (fig 1, pathway 2a–b); psychosocial distress influencing behavioural risk factors (pathway 2c); and behavioural risk factors influencing anthropometric risk factors (pathway 2d). Understanding the nature of this presumed causal chain is critical to the development of effective interventions and policies to reduce socioeconomic disparities in cardiovascular risk.
Figure 1.
Conceptual model of pathways linking socioeconomic position, psychosocial stress, psychological distress and behavioural and anthropometric cardiovascular risk factors. BMI, body mass index; CVD, cardiovascular disease; SEP, socioeconomic position.
METHODS
The relationships between SEP and CVD in the Detroit metropolitan area are similar to those described above. Three-year age-adjusted heart disease mortality in Detroit, Michigan (2001–2003), is over two times higher than in neighbouring Oakland County, where household incomes are double and home values are triple those for Detroit (table 1). In 2000, 83% of the population of Oakland County was white, whereas in Detroit 82% of the population was African American.35 36 Therefore, African Americans disproportionately bear the increased risk of CVD mortality experienced by Detroit residents. CVD mortality rates also vary within Detroit. The 3-year age-adjusted average CVD mortality rate (2000–2002) in east Detroit was 523.9; in northwest Detroit, 395.3; and in southwest Detroit, 426.9.37
Table 1.
Median household income, median home value and age-adjusted 3-year average mortality due to heart disease for Detroit City, Oakland County and Michigan
Sample
Data for this study were drawn from the Healthy Environments Partnership (HEP) community survey, one component of a community-based participatory research study involving academic, health care and community-based organisations in Detroit, Michigan.38 The University of Michigan Institutional Review Board for Protection of Human Subjects approved the HEP study in January 2001.
The HEP survey is a stratified two-stage probability sample of occupied housing units, designed for 1000 completed interviews with adults age ≥25 years across three areas of Detroit, allowing for comparisons of residents of similar demographics across geographic areas of the city. The final sample consisted of 919 face-to-face interviews: interviews were completed with 75% of households in which an eligible respondent was identified and 55% of households with a known or potential respondent.38 Although the proportion of missing data was very low for variables used in this analysis, given the complex sample design used in the HEP survey data collection, we used multiple imputation procedures derived from Bayesian models to impute missing values39 using the %IMPUTE routine (SAS add-in Iveware software http://www.isr.umich.edu/src/smp/ive/). This imputation enabled us to incorporate design-based features (weight, strata and primary sampling unit) in our analysis, obtaining correct standard error estimates and producing the correct confidence intervals for our comparison and estimates.40-42
Measures
Dependent variables included psychological distress and behavioural and anthropometric indicators of CVD risk. Psychological distress was assessed using the short form43 of the Center for Epidemiologic Studies Depressive Symptoms (CES-D) scale44 (Cronbach’s alpha, 0.65). Behavioural indicators included smoking (0 = never; 1 = former; 2 = current) and physical activity constructed as a composite of minutes of moderate and vigorous physical activity per week, divided into quintiles (1 = low; 5 = high). Results were similar for models using continuous and categorical scalings of physical activity, so findings are presented using the continuous version.
Anthropometric measures were calculated from objective measurements of height, weight and measured waist circumference taken at the time of the interview. They included a continuous indicator of BMI calculated as (weight in pounds)/ (height in inches)2 × 703; and waist circumference in centimetres. We tested categorical versions of waist circumference using gender-specific cut points (88 cm/36 inches for women; 102 cm/40 inches for men) for high and low risk, and BMI (<25, normal; 25–29, overweight; ≥30, obese). Results were similar and findings for continuous versions are presented.
Other covariates included in the models were: age (years); gender (0 = male; 1 = female); marital status (1 = not married; 0 = currently married); and number of people in the household. Self-reported race and ethnicity were categorised as non-Hispanic black, non-Hispanic white and Latino. Indicators of SEP were household income (≤$10K, $10–19.9K, $20–34.9K, ≥$35K) and education (<12 years, 12 years, >12 years).
We included four indicators of chronic psychosocial stress. Everyday unfair treatment45 is the mean of five items that assess the frequency of experiences of unfair treatment such as poorer service than other people in restaurants or stores, or being treated with less courtesy or respect than other people, in the previous 12 months (Cronbach’s alpha, 0.77). Response categories ranged from 1 = never to 5 = always.
An index of financial vulnerability was constructed as the mean of two items assessing financial strain. Responses to “If you lost all your current sources of household income—your wages, public assistance or other sources of income—how long could you continue to live at your current address and standard of living?” were coded from 1 = >1 year to 5 = <1 month. Responses to the second item, difficulty paying for basics such as food, housing, medical care and heating, were coded from 1 = not difficult at all to 4 = very difficult, and rescaled to a five-point item by multiplying by 5/4. The final mean of both items is a five-point index with 1 = less financial vulnerability to 5 = more financial vulnerability.
We included two indicators of chronic stressful neighbourhood conditions. Neighbourhood social environment is a mean scale of six items assessing the frequency with which respondents indicated that events such as gang activity, shootings or theft were a problem in their neighbourhood. Response categories ranged from 1 = never to 5 = always (Cronbach’s alpha, 0.83). Neighbourhood physical environment is a mean scale of seven items assessing agreement with statements such as, “houses in my neighbourhood are generally well maintained” (reverse coded) and “there is air pollution like diesel from trucks or pollution from factories or incinerators in my neighbourhood”. Response categories ranged from 1 = strongly disagree to 5 = strongly agree (Cronbach’s alpha, 0.69).
Two indicators of acute stressful life events were included. Acute unfair treatment45 is a dichotomous variable indicating whether the respondent reported any of seven experiences with acute unfair treatment (eg, unfair treatment concerning work, treated unfairly by police or immigration officials) in the past year (0 = none; 1 = one or more). Acute life events is a dichotomous variable indicating whether the respondent reported any of nine major life events in the past year (0 = none; 1 = one or more). Examples of scale items include death of a loved one, and family member or close friend with major illness or injury.
ANALYSIS
We used multinomial regression models for categorical dependent variables,46 and ordinary least squares regression techniques for continuous outcomes. Model 1 tests the hypothesis that SEP predicts variations in each dependent variable, above and beyond the effects of demographic control variables. In addition, in order to explicitly test the hypothesis that indicators of psychosocial stress mediate relationships between SEP and indicators of CVD risk, we test relationships between SEP and each indicator of psychosocial stress.47 Model 2 tests the contributions of indicators of chronic and acute stress to psychological, behavioural and anthropometric CVD risk factors. Model 3 tests the contribution of psychological distress to models predicting behavioural and anthropometric indicators of CVD risk. Model 4 tests the contribution of behavioural risk factors to anthropometric indicators of CVD risk. All models are adjusted for sample weights for unequal probabilities of selection within each stratum and to match the sample to Census 2000 population distributions for the study areas.
RESULTS
Descriptive statistics illustrating study variables adjusted for the sample weights are shown in table 2. Participants’ mean age was 46 years, 52% were women (632 unweighted cases), 26% were currently married and 57% were non-Hispanic black, 22% Latino and 19% non-Hispanic white. One-third (33%) reported education beyond high school and 23% reported annual household incomes of >$35K. Thirty-seven per cent reported that they currently smoked, 24% never engaged in physical activity, mean BMI was 31, and mean waist circumference was 98 centimetres (about 39 inches). Results from tests for multicollinearity among the independent variables showed variance inflation factors of 1.3–1.6, well below the cut point of 4.0 commonly considered indicative of multicollinearity. Similarly, tolerances ranged from 0.61 to 0.76, comfortably above the levels of ≤0.20 considered to be indicative of multicollinearity.
Table 2.
Descriptive statistics for study variables – full sample (N = 919)
| Unweighted |
Weighted descriptive statistics |
||||
|---|---|---|---|---|---|
| N | Per cent | Mean | SD | Range | |
| Age | 919 | 46.3 | 0.8 | 25.0–96.0 | |
| Female | 632 | 52.3 | |||
| Male | 287 | 47.7 | |||
| Not married | 689 | 73.6 | |||
| Currently married | 230 | 26.4 | |||
| Number of people in household | 919 | 2.8 | 0.1 | 1.0–11.0 | |
| Non-Hispanic black | 522 | 56.8 | |||
| Hispanic/Latino | 182 | 22.2 | |||
| Non-Hispanic white | 199 | 18.8 | |||
| Other | 16 | 2.3 | |||
| Education | |||||
| <High school | 327 | 37.3 | |||
| High school graduate | 259 | 29.5 | |||
| >High school | 321 | 33.2 | |||
| Income | |||||
| <$10 000 | 250 | 27.3 | |||
| $10 000–$19 999 | 238 | 26.0 | |||
| $20 000–$34 999 | 230 | 23.6 | |||
| ≥$35 000 | 201 | 23.0 | |||
| Everyday unfair treatment | 918 | 1.7 | <0.0 | 1.0–5.0 | |
| Acute unfair treatment (any in last 12 months = 1) | 263 | 29.0 | |||
| Financial vulnerability | 919 | 3.1 | 0.1 | 1.1–5.0 | |
| Neighbourhood social environment | 919 | 2.7 | 0.1 | 1.0–5.0 | |
| Neighbourhood physical environment | 919 | 2.9 | 0.1 | 1.0–5.0 | |
| Acute life events (any in last 12 months = 1) | 655 | 71.1 | |||
| Symptoms of depression | 919 | 2.6 | <0.0 | 1.4–4.7 | |
| Current smoker | 347 | 37.0 | |||
| Former smoker | 197 | 22.6 | |||
| Never smoker | 375 | 40.4 | |||
| Physical activity level | 919 | 1.9 | 0.1 | 0.0–4.0 | |
| BMI | 919 | 30.8 | 0.2 | 15.8–61.8 | |
| Waist circumference (cm) | 919 | 98.0 | 0.6 | 34.0–162.0 | |
Data are weighted to adjust for sampling design. BMI, body mass index.
Results presented in table 3 provide partial support for our hypothesis that SEP is associated with multiple CVD risk factors. Household income <$10K was positively associated with depressive symptoms (p<0.001), current smoking (p = 0.05), physical inactivity (p<0.05) and waist circumference (p<0.05). Income $10–19K was also positively associated with depressive symptoms (p<0.01). Relationships between income and BMI were in the expected direction but not statistically significant.
Table 3.
Depressive symptoms, smoking, physical activity, BMI and waist circumference regressed on education, income, everyday unfair treatment, acute unfair treatment, financial vulnerability, neighbourhood social environment stress, neighbourhood physical environment stress and acute life events (controlling for age, gender, marital status, number in household unit, race and ethnicity, not shown)
| Depressive symptoms |
Former smoking |
Current smoking |
Physical activity |
BMI |
Waist circumference |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 1 |
Model 2 |
Model 1 |
Model 2 |
Model 1 |
Model 2 |
Model 1 |
Model 2 |
Model 1 |
Model 2 |
|
| Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | |
| Intercept | 2.60*** | 1.40*** | −1.51** | −2.47** | 0.89 | −1.53 | 3.57 | 4.02 | 26.47*** | 24.13*** | 85.70*** | 75.55*** |
| Education (>High school referent) | ||||||||||||
| <High school | 0.03 | 0.05 | −0.19 | −0.16 | 0.36 | 0.40 | −0.41** | −0.32* | −0.42 | −0.49 | −2.34 | −2.03 |
| High school graduate | −0.02 | 0.01 | 0.08 | 0.09 | 0.57** | 0.63** | −0.15 | −0.16 | −0.80 | −0.76 | −1.29 | −1.12 |
| Income (≥$35 000 referent) | ||||||||||||
| <$10 000 | 0.28*** | 0.19** | 0.11 | 0.07 | 0.80* | 0.56 | −0.42* | −0.28 | 0.88 | 0.39 | 4.24* | 3.22 |
| $10 000–19 999 | 0.19** | 0.15* | −0.06 | −0.07 | 0.50 | 0.34 | −0.13 | −0.02 | 0.17 | −0.19 | 0.11 | −0.58 |
| $20 000–34 999 | −0.02 | −0.03 | 0.06 | 0.05 | 0.20 | 0.14 | −0.07 | −0.01 | 0.42 | 0.26 | 0.42 | 0.24 |
| Psychosocial stress measures | ||||||||||||
| Everyday unfair treatment | 0.23*** | 0.22 | 0.13 | 0.04 | 0.53 | 1.97 | ||||||
| Acute unfair treatment | 0.11* | 0.04 | 0.16 | 0.30* | −0.54 | −0.03 | ||||||
| Financial vulnerability | 0.04* | −0.01 | 0.20* | −0.14** | 0.27 | 0.25 | ||||||
| Neighbourhood social environment | 0.09*** | 0.09 | 0.14 | −0.06 | −0.01 | 0.37 | ||||||
| Neighbourhood physical environment | 0.02 | −0.02 | 0.24* | −0.06 | 0.01 | 0.29 | ||||||
| Acute life events | 0.18*** | 0.27 | 0.59* | 0.03 | 1.03 | 4.13** | ||||||
| Adjusted R2 | 0.09 | 0.28 | 0.08 | 0.10 | 0.02 | 0.02 | 0.04 | 0.05 | ||||
| F statistic/significance for change | 39.56** | 3.89** | 1.18 | 2.97** | ||||||||
| df = 231.1./−2log likelihood | 10.9/1768.7 | 6.2/17360.4 | 10.9/1768.7 | 6.2/17360.4 | ||||||||
| G statistic/significance for change | 32.3** | 32.3** | ||||||||||
BMI, body mass index; df, degrees of freedom.
p<0.05,
p<0.01,
p<0.001.
Participants who had completed high school were more likely than those with some college to report current smoking (p<0.01), and those with less than a high school education were less likely to report physical activity (p<0.05). A significant association between <12 years of education and depressive symptoms when income was not included in the model (results not shown) was no longer significant when income was included in model 1. Coefficients for relationships between education and psychosocial stressors and anthropometric indicators were not statistically significant.
Results shown in model 2 (table 3) indicate that psychosocial stressors are associated with four of the five CVD risk factors examined here. Everyday (p<0.001) and acute (p<0.05) unfair treatment, financial vulnerability (p<0.05), neighbourhood social environment (p<0.001) and acute life events (p<0.001) are each significantly associated with symptoms of depression. Regression coefficients for relationships between income and depressive symptoms were reduced by 32% (income <$10K) and 21% (income $10–19.9K), but remained statistically significant. Model 2 accounted for three times the proportion of variance in depressive symptoms explained in model 1 (28% versus 9%).
Indicators of financial vulnerability (p<0.05), neighbourhood physical environment (p<0.05), and acute life events (p<0.05) were significantly associated with current smoking. The inclusion of psychosocial stressors reduced the association between income <$10K and current smoking to non-significance, and the amount of variance explained by the model increased significantly (p = 0.01).
Financial vulnerability (p<0.01) and acute unfair treatment (p<0.05) were significantly and negatively associated with level of physical activity. The inclusion of psychosocial stressors in model 2 reduced the relationship between income <$10K and physical activity to non-significance, and between education below high school and physical activity by 21% (p<0.05), and increased the amount of variation explained significantly (p<.01). Finally, acute life events was significantly associated with waist circumference (p<0.01) and reduced the relationship between income <$10K and waist circumference in model 1 to non-significance.
To test the hypothesis that indicators of psychosocial stress mediate relationships between SEP and symptoms of depression, smoking, physical activity and waist circumference, we examined relationships between indicators of psychosocial stress, income and education. After controlling for other demographic variables, we found no relationship between education and any of the indicators of psychosocial stress considered in these models (results not shown). Household income was significantly associated with financial vulnerability and acute life events (table 4). Combined with results shown in table 3, these findings provide evidence that is consistent with the hypothesis that relationships between income and symptoms of depression, current smoking, physical activity and waist circumference are partially or fully mediated through the effects of income on financial vulnerability and acute life events as indicators of psychosocial stress.
Table 4.
Everyday unfair treatment, acute unfair treatment, financial vulnerability, neighbourhood social environment, neighbourhood physical environment and acute life events regressed on household income (controlling for age, gender, marital status, number in household unit, race and ethnicity and education, not shown)
| Everyday unfair treatment |
Acute unfair treatment |
Financial vulnerability |
Neighbourhood social environment |
Neighbourhood physical environment |
Acute life events |
|
|---|---|---|---|---|---|---|
| Income (≥$35 000 referent) | Estimate | OR | Estimate | Estimate | Estimate | OR |
| <$10 000 | 0.15 | 1.09 | 1.09*** | −0.010 | −0.173 | 1.90* |
| $10 000–19 999 | 0.01 | 0.79 | 0.72*** | −0.046 | −0.093 | 1.95* |
| $20 000–34 999 | −0.04 | 1.02 | 0.50*** | −0.045 | −0.157 | 1.26 |
p<0.05,
p<0.001.
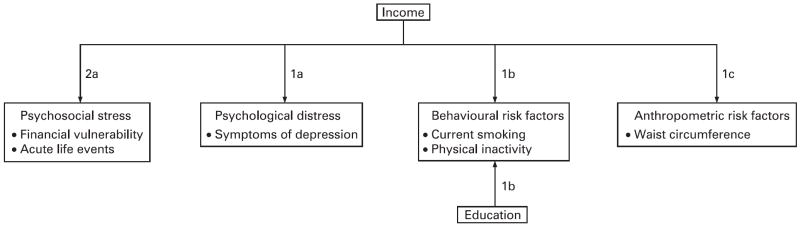
Results from table 3 (model 1) and table 4 are summarised in figure 2. Education, net of income, affects mainly smoking and physical activity, whereas income affects depressive symptoms and waist circumference in addition to smoking and physical activity. Overall, income is a more consequential risk factor for CVD in this population. Results shown in table 3 (model 2) indicate that relationships between income and four of the five indicators of CVD risk are at least partially mediated through increased levels of financial vulnerability and acute life events. Several additional indicators of psychosocial stress make significant independent contributions to the dependent variables, but we did not find evidence that they mediate relationships between SEP and indicators of CVD risk in this sample.
Figure 2.
Relationships between income and education, and psychosocial stress, psychosocial distress, behavioural and anthropometric risk factors (summary of results shown in table 3, model 1 and table 4). (Further details available online.)
Symptoms of depression and behavioural and anthropometric risk factors
Table 5 shows results from analyses testing the contributions of depressive symptoms (model 3); and behavioural risk factors (model 4).
Table 5.
Smoking, physical activity, BMI and waist circumference regressed on education, income, everyday unfair treatment, acute unfair treatment, financial vulnerability, neighbourhood social environment stress, neighbourhood physical environment stress, acute life events and depressive symptoms (controlling for age, gender, marital status, number in household unit, race and ethnicity, not shown)
| Former smoking |
Current smoking |
Physical activity |
BMI |
Waist circumference |
|||
|---|---|---|---|---|---|---|---|
| Model 3 |
Model 3 |
Model 3 |
Model 3 |
Model 4 |
Model 3 |
Model 4 |
|
| Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | Estimate | |
| Intercept | −1.93* | −2.47** | 4.13 | 23.42*** | 23.92*** | 71.38*** | 73.10*** |
| Education (>High school referent) | |||||||
| <High school | −0.14 | 0.36 | −0.31* | −0.52 | −0.30 | −2.18 | −1.97 |
| High school graduate | 0.10 | 0.64 | −0.16 | −0.77 | −0.41 | −1.16 | −0.70 |
| Income (≥$35 000 = referent) | |||||||
| <$10 000 | 0.12 | 0.46 | −0.27 | 0.29 | 0.50 | 2.65 | 2.80 |
| $10 000–19 999 | −0.04 | 0.26 | −0.01 | −0.26 | −0.10 | −1.01 | −0.77 |
| $20 000–34 999 | 0.04 | 0.18 | −0.01 | 0.27 | 0.35 | 0.33 | 0.41 |
| Psychosocial stress measures | |||||||
| Everyday unfair treatment | 0.29 | −0.03 | 0.05 | 0.41 | 0.36 | 1.28 | 1.17 |
| Acute unfair treatment | 0.06 | 0.09 | 0.31* | −0.60 | −0.50 | −0.36 | −0.07 |
| Financial vulnerability | 0.01 | 0.17* | −0.14** | 0.25 | 0.34 | 0.14 | 0.21 |
| Neighbourhood social environment | 0.11 | 0.08 | −0.05 | −0.06 | 0.04 | 0.12 | 0.08 |
| Neighbourhood physical environment | −0.02 | 0.23* | −0.06 | −0.00 | 0.13 | 0.22 | 0.39 |
| Acute life events | 0.31 | 0.48* | 0.04 | 0.94 | 1.18 | 3.60** | 3.92** |
| Symptoms of depression | −0.32 | 0.67*** | −0.07 | 0.51 | 0.96 | 2.97* | 3.71* |
| Current smoker | −3.23*** | −4.40** | |||||
| Former smoker | −0.49 | 0.98 | |||||
| Physical activity | −0.10 | −0.65 | |||||
| Adjusted R2 | 0.09 | 0.02 | 0.07 | 0.06 | 0.09 | ||
| F statistic/significance for change | 0.51 | 1.33 | 7.30*** | 5.95* | 5.71* | ||
| df = 23.1./−2log likelihood | 6.05/1709.3 | ||||||
| G statistic/significance for change | 57.45** | ||||||
BMI, body mass index; df, degrees of freedom.
p ≤0.05,
p≤0.01,
p≤0.001.
Results shown for model 3 indicate that depressive symptoms are significantly associated with current smoking (p<0.001) and waist circumference (p<0.05), but not physical activity or BMI, although the latter coefficients are in the expected direction. The inclusion of depressive symptoms in model 3 significantly improves the fit of the models for both current smoking (p<0.01) and waist circumference (p<0.05), indicating that depressive symptoms contribute independently to the explanatory value for these dependent variables. For each unit increase in depressive symptoms, there was a 2.97 cm increase in waist circumference.
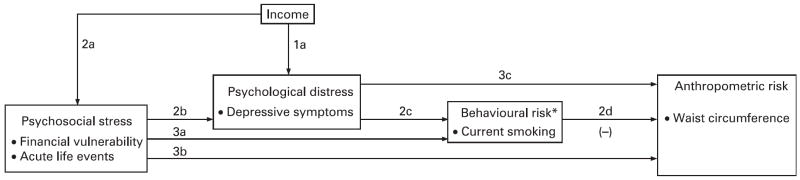
Results for model 4 indicate significant negative associations between current smoking and both BMI (p<0.001) and waist circumference (p<0.01). Relationships between physical activity and BMI and waist circumference were in the expected direction but were not statistically significant. The size of the coefficient for depressive symptoms increased from 0.51 to 0.96 for BMI (n.s.) and from 2.97 to 3.71 (p<0.05) for waist circumference. This suppression effect47 occurred because the direct effects of depressive symptoms on waist circumference were positive whereas the mediated effects (through probability of current smoking) were negative, so the full effects of depressive symptoms on waist circumference were not visible until the effect of current smoking was controlled. The addition of behavioural predictors in model 4 increased the overall explained variance for BMI from 0.02 to 0.07 (p<0.001) and for waist circumference from 0.06 to 0.09 (p<0.01). Findings from table 3 (model 2) and table 4 are summarised in figure 3.
Figure 3.
Relational pathways between income, psychosocial stress, psychological distress, current smoking, physical inactivity and waist circumference (summary of results shown in tables 3-5). (Further details available online.)
DISCUSSION
The results presented here are generally consistent with our hypothesised pathways linking SEP to CVD risk. As shown in figure 2, household income is significantly associated with four of the five CVD risk factors examined, and education is independently associated with two of the five. Overall, in this multiethnic, low–moderate income urban sample, income is a more substantial risk factor for CVD than education.
The findings presented in tables 3–5 and illustrated in figure 3 are generally consistent with the cascade of effects hypothesised. Psychosocial stress partially mediates relationships between income and psychological distress (2a–2b), psychological distress partially mediates relationships between psychosocial stress and behavioural risks (2b–2c) and current smoking suppresses (a form of mediation effect47) relationships between psychological distress and waist circumference (2c–2d).
We also find evidence of independent effects of psychosocial stress and psychological distress on current smoking and waist circumference, above and beyond the mediation effects described above. Specifically, psychosocial stress is associated with current smoking (3a) above and beyond effects mediated through psychological distress; and psychosocial stress (3b) and psychological distress (3c) are each associated with waist circumference, beyond effects mediated through current smoking. Thus, our final model suggests both mediating and cumulative effects of multiple factors.
Limitations
There are several limitations of the analyses reported here. The data are cross-sectional, and hence we cannot test the causal nature of associations between variables. Our models posit a primary direction of association, with low SEP associated with higher levels of psychosocial stress and psychological distress, contributing to heightened risk of smoking, physical inactivity and obesity. The hypothesised direction of effects is supported by a substantial literature,25-27 48 49 but it is also reasonable to expect some reciprocal effects (eg, depressive symptoms may predict obesity, but those who are obese may also be at increased risk of depressed mood). An important consideration for future analyses will be the availability of longitudinal data to further disentangle the direction and relative contributions of these effects.
The use of self-reported data for behavioural indicators used in this analysis is also a limitation. The reliability and validity of self-reports of current smoking and levels of physical activity may be influenced by memory, social acceptability or perceived stigma associated with these behaviours. These limitations would tend to bias results in the direction of underestimating effects. The measures included in these models are a subset of those that might influence CVD risk—other measures such as dietary practices should be incorporated in future analyses.
This study draws on data from an urban sample with a circumscribed range of household income: 80% of study participants reported annual household incomes <$35 000, with >50% reporting incomes <$20 000. Failure to find a statistically significant relationship between income and BMI, contrary to much of the literature in this area, may reflect the limited range of income in our sample, and also the known weaker relationship of income to BMI among racial/ethnic minority groups. For similar reasons, findings reported here may also underestimate relationships between income and our other indicators of cardiovascular risk.
We found modest evidence for independent effects of education, above and beyond the effects of household income. This finding may reflect the relative lack of variation in levels of education at the upper end of the educational spectrum (just 7% of participants reported completion of ≥4 years of college). It may also reflect the relatively smaller improvements in social and economic status realised by African Americans, who make up 57% of our sample, compared with whites with similar educational attainments.50-52 To the extent that relationships between education and health-related behaviours or anthropometric indicators operate through improved access to resources, residents of communities such as Detroit, with reduced structural access to economic, health and social resources, may realise fewer benefits from education than their counterparts in more affluent neighbourhoods. Future analyses should attempt to disentangle these individual and neighbourhood-level pathways through, for example, hierarchical linear modelling techniques.
Implications
Despite these limitations, findings presented here are consistent with evidence from cross-sectional and longitudinal studies that suggest that low SEP is associated with increased exposure to multiple risk factors for CVD. Furthermore, our results are consistent with conceptual models linking household income to cardiovascular risk through exposure to stressful life conditions, with subsequent effects on psychological distress and behavioural and anthropometric indicators.
These findings also highlight the complexity of risk. Several indicators of psychosocial stress included in our models were significantly associated with indicators of cardiovascular risk, but were not significantly associated with SEP in this sample. Everyday and acute unfair treatment have been previously demonstrated to be significantly associated with race,53 54 and may be one pathway through which racial disparities in cardiovascular risk occur independently of the well-established association of race and income in the US.3 55 Furthermore, measures of social and physical environment stress associated with some indicators of CVD risk were not significantly associated with household income in this sample, suggesting the need to better understand predictors of these stressors and their contributions to CVD risk. Such measures may be more reflective of neighbourhood-level economic inequalities not captured in this analysis, but demonstrated in previous studies to be associated with the unequal distribution of cardiovascular risk.55 Our results are consistent with models that position smoking as an intermediary within a chain of events linking low SEP to CVD through stressful life conditions and depressive symptoms. Smoking as a behavioural response to stress associated with low SEP appears to partially suppress associations between depressive symptoms and anthropometric indicators of risk. Until we account for the negative association between smoking and waist circumference, the relationship between depressive symptoms and waist circumference is partially obscured. These findings suggest the importance of understanding smoking behaviour as emerging within particular socioeconomic contexts associated with heightened stress and depressive symptoms. Interventions that focus solely on smoking without addressing associated economic and social inequalities address only one aspect of the multifaceted pathways linking unequal social positions to unequal risk of CVD.56 57
These results add weight to arguments regarding the importance of addressing social inequalities as a means to reduce health disparities.3 4 58 The finding that low income increases multiple risk factors in this sample with a relatively circumscribed range of household income suggests that even modest improvements in economic circumstances may contribute to population-level reductions in CVD risk. Interventions at more fundamental levels can set in motion a cascade of effects, including reduced exposure to stressful life conditions and improved mental well-being, with implications for multiple more proximate CVD risk factors. Such interventions offer important opportunities to improve population-level health and quality of life by reducing and eventually eliminating socioeconomic inequalities in health.
What is already known on this subject
The risk of cardiovascular disease (CVD), the largest contributor to all-cause mortality in the USA, varies by socioeconomic position (SEP). In addition, SEP is associated with multiple established risk factors for CVD.
What this study adds
We have drawn on a multiethnic sample from Detroit, Michigan, to test hypotheses linking SEP to CVD risk through a progression of effects that include exposure to stressful life conditions, psychological distress, behavioural risk factors and anthropometric indicators of CVD risk. Our results provide support for conceptual models that posit that SEP influences CVD risk in part through behavioural and anthropometric responses to psychosocial stress and distress.
Policy implications
These models and results suggest that interventions that improve the socioeconomic position of economically disadvantaged people can set in motion a cascade of effects, including reductions in exposure to stressful life conditions, improved mental well-being, increased physical activity, reductions in smoking, and reduced anthropometric risks associated with CVD.
Acknowledgments
The Healthy Environments Partnership (HEP) (www.hepdetroit.com) is affiliated with the Detroit Community–Academic Urban Research Center (www.sph.umich.edu/urc). We thank the members of HEP (who have included Boulevard Harambee, Brightmoor Community Center, Detroit Department of Health, Detroit Hispanic Development Corporation, Friends of Parkside, Henry Ford Health System, Southwest Detroit Environmental Vision, and the University of Michigan Schools of Public Health, Nursing, Social Work and the Survey Research Center) for their contributions to the work presented here. HEP is funded by the National Institute of Environmental Health Sciences, no. R01 ES10936. Finally, we thank Sue Andersen for her assistance with the preparation of this manuscript.
Footnotes
Competing interests: None.
Additional details for figures 2 and 3 are published online only at http://jech.bmj.com/content/vol62/issue7
References
- 1.Cooper R, Cutler JA, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102:3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 2.Williams DR. Race, socioeconomic status and health. Ann N Y Acad Sci. 1999;896:173–88. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 3.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ ethnic disparities in health. In: Smedley BD, Syme SL, editors. Promoting health: intervention strategies from social and behavioral research. Vol. 81. Washington, DC: National Academy Press; 2000. pp. 1–4. [PubMed] [Google Scholar]
- 4.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Social Behav. 1995;36(Special issue):80–94. [PubMed] [Google Scholar]
- 5.Marmot MG, Bosma H, Hemingway H, et al. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350:235–9. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- 6.Diez-Roux AV, Northridge ME, Morabia A, et al. Prevalence and social correlates of cardiovascular disease risk factors in Harlem. Am J Public Health. 1999;89:302–7. doi: 10.2105/ajph.89.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez-Roux A, Detrano R, Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112:1557–65. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 8.Rosvall M, Östergren P-O, Hedblad B, et al. Socioeconomic differences in the progression of sub-carotid atherosclerosis in middle-aged men and women with subclinical atherosclerosis in Sweden. Soc Sci Med. 2006;62:1785–98. doi: 10.1016/j.socscimed.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 9.Winkleby MA, Kraemer HC, Ahn DK, et al. Ethnic and socioeconomic differences in cardiovascular disease risk factors. JAMA. 1998;280:356–62. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]
- 10.Heslop P, Smith GD, Carroll D, et al. Perceived stress and coronary heart disease risk factors: the contribution of socio-economic position. Br J Health Psychol. 2001;6:167–78. doi: 10.1348/135910701169133. [DOI] [PubMed] [Google Scholar]
- 11.Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- 12.Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896:262–77. doi: 10.1111/j.1749-6632.1999.tb08121.x. [DOI] [PubMed] [Google Scholar]
- 13.Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92:624–31. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner RJ, Lloyd DA. The stress process and the social distribution of depression. J Health Soc Behav. 1999;40:374–404. [PubMed] [Google Scholar]
- 15.Ahluwalia IB, Mack KA, Mokdad A. Mental and physical distress and high-risk behaviors among reproductive-age women. Obstet Gynecol. 2004;104:477–83. doi: 10.1097/01.AOG.0000137920.58741.26. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics (NCHS) [14 July 2006];Health, United States. 2005 http://www.cdc.gov/nchs/data/hus/hus05.pdf. [PubMed]
- 17.Schoenborn CA, Adams PF, Barnes PM, et al. Vital health statistics, Series 10. Vol. 219. Hyattsville, MD: NCHS; 2004. Health behaviors of adults: United States, 1999–2001; pp. 1–79. [PubMed] [Google Scholar]
- 18.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 19.James SA, Fowler-Brown A, Raghunathan TE, et al. Life-course socioeconomic position and obesity in African American Women: the Pitt County Study. Am J Public Health. 2006;96:554–60. doi: 10.2105/AJPH.2004.053447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilsgaard T, Jacobsen BK, Arnesen E. Determining lifestyle correlates of body mass index using multilevel analyses: the Tromso Study, 1979–2001. Am J Epidemiol. 2005;162:1179–88. doi: 10.1093/aje/kwi328. [DOI] [PubMed] [Google Scholar]
- 21.House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Social Behav. 2002;43:125–42. [PubMed] [Google Scholar]
- 22.van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–22. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22:638–42. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- 25.Björntorp P. Heart and soul: stress and the metabolic syndrome. Scand Cardiovasc J. 2001;35:172–7. doi: 10.1080/140174301750305045. [DOI] [PubMed] [Google Scholar]
- 26.McEwen BS. Protective and damaging effects of stress mediators: central role of the brain. Prog Brain Res. 2000;122:25–34. doi: 10.1016/s0079-6123(08)62128-7. [DOI] [PubMed] [Google Scholar]
- 27.Vitaliano PP, Scanlan JM, Zhang J, et al. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002;64:418–35. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Brown WJ, Ford JH, Burton NW, et al. Prospective study of physical activity and depressive symptoms in middle-aged women. Am J Prev Med. 2005;29:265–72. doi: 10.1016/j.amepre.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 29.Motl RW, Konopack JF, McAuley E, et al. Depressive symptoms among older adults: long-term reduction after a physical activity intervention. J Behav Med. 2005;28:385–94. doi: 10.1007/s10865-005-9005-5. [DOI] [PubMed] [Google Scholar]
- 30.US Census Bureau. [28 December 2005];State and county quickfacts: Detroit (city), Michigan. 2005 last revised December 13, 2005, http://quickfacts.census.gov/qfd/states/26/2622000.html.
- 31.US Census Bureau. [28 December 2005];State and county quickfacts: Oakland County, Michigan. 2005 http://quickfacts.census.gov/qfd/states/26/26125.html.
- 32.Michigan Department of Community Health. [12 January 2007];Heart disease deaths and death rates, city of Detroit Health Department district residents, 1989–2005. 2006 http://www.mdch.state.mi.us/pha/osr/chi/cri/frame.html.
- 33.Michigan Department of Community Health. [29 September 2006];Mortality, natality and other vital statistics. 2005 http://www.michigan.gov/mdch.
- 34.US Census Bureau. [17 January 2006];State and county quickfacts: Michigan. 2005 last revised 12 January 2006, http://quickfacts.census.gov/qfd/states/26000.html.
- 35.Southeast Michigan Council of Governments. [11 September 2006];Community profile for Detroit City. 2006 http://www.semcog.org/Data/CommunityProfiles/index.htm.
- 36.Southeast Michigan Council of Governments. [11 September 2006];Community profile for Oakland County. 2006 http://www.semcog.org/Data/CommunityProfiles/index.htm.
- 37.Michigan Department of Community Health. [30 August 2004];Mortality Statistics. 2003 http://www.mdch.state.mi.us/pha/osr/chi/Deaths/frame.html.
- 38.Schulz AJ, Kannan S, Dvonch JT, et al. Social and physical environments and disparities in risk for cardiovascular disease: the Healthy Environments Partnership conceptual model. Environ Health Perspect. 2005;113:1817–25. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barnard J, Schenker N, Rubin DB. Multiple imputation. In: Smelser NJ, Baltes PB, editors. International encyclopedia of the social & behavior sciences. Amsterdam: Elsevier; 2004. pp. 10204–10. [Google Scholar]
- 40.Bryk AS, Raudenbush SW. Hierarchical linear models. Newbury Park, CA: Sage; 1992. [Google Scholar]
- 41.Rubin DB. Multiple imputation after 18+ years (with discussion) J Am Stat Assoc. 1996;91:473–89. [Google Scholar]
- 42.Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- 43.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D Depression Symptoms Index. J Aging Health. 1993;5:179–93. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 44.Radloff LS. The CES-D: a self-report depression scale for research on the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 45.Williams DR, Yu Y, Jackson J, et al. Racial differences in physical and mental health: socioeconomic status, stress and discrimination. J Health Psychol. 1997;2:335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 46.DeMaris A. A tutorial on logistic regression. J Marriage Fam. 1995;57:956–68. [Google Scholar]
- 47.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stansfield SA, Fuhrer R, Shipley MJ, et al. Psychological distress as a risk factor for coronary heart disease in the Whitehall II study. Int J Epidemiol. 2002;31:248–55. doi: 10.1093/ije/31.1.248. [DOI] [PubMed] [Google Scholar]
- 49.Steptoe A, Wardle J. Cardiovascular stress responsivity, body mass and abdominal adiposity. Int J Obesity. 2005;29:1329–37. doi: 10.1038/sj.ijo.0803011. [DOI] [PubMed] [Google Scholar]
- 50.Conley D. The racial wealth gap: origins and implications for philanthropy in the African American community. Nonprofit Voluntary Sector Q. 2000;29:530–40. [Google Scholar]
- 51.Massey DS, Denton NA. American apartheid: segregation and the making of the underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 52.Schulz AJ, Israel BA, Williams DR, et al. Social inequalities, stressors and self-reported health status among African American and white women in the Detroit metropolitan area. Soc Sci Med. 2000;51:1639–53. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- 53.Williams DR, Yu Y, Jackson JS, et al. Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. J Health Psychol. 1997;2:335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 54.Schulz AJ, Williams DR, Israel BA, et al. Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. J Health Soc Behav. 2000;41:314–32. [PubMed] [Google Scholar]
- 55.Diez-Roux A, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000;50:673–87. doi: 10.1016/s0277-9536(99)00320-2. [DOI] [PubMed] [Google Scholar]
- 56.James SA. Primordial prevention of cardiovascular disease among African Americans: A social epidemiological perspective. Prev Med. 1999;29(6 part 2):S84–9. doi: 10.1006/pmed.1998.0453. [DOI] [PubMed] [Google Scholar]
- 57.Graham H. Gender and class as dimensions of smoking behaviour in Britain: Insights from a survey of mothers. Soc Sci Med. 1994;38:691–8. doi: 10.1016/0277-9536(94)90459-6. [DOI] [PubMed] [Google Scholar]
- 58.Marmot M. Inequalities in health. N Engl J Med. 2001;345:134–6. doi: 10.1056/NEJM200107123450210. [DOI] [PubMed] [Google Scholar]