The recognition of sepsis is a crucial aspect in the management of critically ill patients. Recent guidelines strongly recommend the initiation of broad-spectrum antibiotic therapy within 1 hour after the recognition of a case of sepsis (1). The adjustment of antibiotic therapy is also recommended once the involved pathogen is identified (1). The current microbiological diagnosis of sepsis is based on blood culture. However, blood culture systems suffer from several limitations such as lack of rapidity and, in cases such as polymicrobial infections, low sensitivity (6). Support for cultural approaches is therefore needed, and well-designed molecular assays could improve the diagnostic flowchart (5, 6). Under this perspective, we have recently evaluated a molecular assay for the diagnosis of sepsis (LightCycler SeptiFast test; Roche Molecular Systems) (3). SeptiFast is a multiplex real-time PCR-based assay, allowing for the detection of a wide panel of bacterial and mycotic pathogens directly from blood (2). DNA is extracted by mechanical lysis with ceramic beads in a Magnalyzer instrument (Roche Molecular Systems), and after purification, it is processed in three parallel real-time PCRs (gram-positive, gram-negative, fungi). The detection of amplicons is based on dual fluorescent resonance energy transfer probes targeting the internal transcribed spacer (ITS) regions. ITS regions are species-specific multicopy noncoding sequences interspaced among conserved bacterial and fungal ribosomal DNA (4, 7). Finally, a dedicated software (SeptiFast identification software) calculates the specific melting profile of ITS-amplified products, thus allowing identification of the pathogen at the species level (2). From our experience with a cohort of neutropenic patients, SeptiFast featured sensitivity at least comparable to that observed with blood culture and a dramatically shorter turnaround time (3). For example, in a case of polymicrobial sepsis, the rapid identification of involved pathogens allowed for a prompt adjustment of therapy. Blood cultures and intravascular catheter tip culture were performed on a persistently febrile patient with multiple myeloma. Empirical intravenous antibiotic therapy with linezolid (600 mg every 12 h) and ceftriaxone (2 g once a day [QD]) was then started. In parallel, 1.5 ml of KEDTA-treated blood was also taken to perform SeptiFast. After only 6 hours, the presence of DNA belonging to Pseudomonas aeruginosa, Stenotrophomonas maltophilia, and Candida albicans was reported to the department (Fig. 1). Levofloxacin (500 mg QD) and fluconazole (400 mg QD) were then promptly added to the therapy. In the following days, the molecular results were then confirmed by culture-based approaches. Blood cultures turned positive on day 1 for gram-negative rods with Pseudomonas sp.-like morphology. Only on day 3 was the definitive identification for Pseudomonas aeruginosa and Stenotrophomonas maltophilia obtained. No growth of Candida albicans was detected in blood culture bottles after 5 days of incubation. Notwithstanding, on day 3, Candida albicans was detected on plates from catheter tip culture. The susceptibility profiles were obtained for all pathogens and confirmed the appropriateness of the therapeutic adjustment performed after the molecular results were obtained.
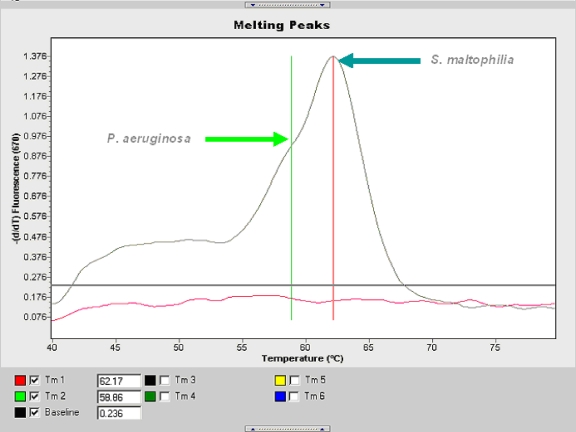
FIG. 1.
Melting curve registrations, allowing for identification at the species level of Pseudomonas aeruginosa (melting temperature, 58.86°C) and Stenotrophomonas maltophilia (melting temperature, 62.17°C).
This is an example of how a rapid, molecular-based diagnosis could result in better therapeutic management of critically ill patients, also leading to a more rational use of anti-infectious agents.
Footnotes
Published ahead of print on 26 January 2009.
REFERENCES
- 1.Dellinger, R. P., M. M. Levy, J. M. Carlet, J. Bion, M. M. Parker, R. Jaeschke, K. Reinhart, D. C. Angus, C. Brun-Buisson, R. Beale, T. Calandra, J. F. Dhainaut, H. Gerlach, M. Harvey, J. J. Marini, J. Marshall, M. Ranieri, G. Ramsay, J. Sevransky, B. T. Thompson, S. Townsend, J. S. Vender, J. L. Zimmerman, and J. L. Vincent. 2008. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit. Care Med. 36296-327. [DOI] [PubMed] [Google Scholar]
- 2.Lehmann, L. E., K. P. Hunfeld, T. Emrich, G. Haberhausen, H. Wissing, A. Hoeft, and F. Stuber. 2008. A multiplex real-time PCR assay for rapid detection and differentiation of 25 bacterial and fungal pathogens from whole blood samples. Med. Microbiol. Immunol. 197313-324. [DOI] [PubMed] [Google Scholar]
- 3.Mancini, N., D. Clerici, R. Diotti, M. Perotti, N. Ghidoli, D. De Marco, B. Pizzorno, T. Emrich, R. Burioni, F. Ciceri, and M. Clementi. 2008. Molecular diagnosis of sepsis in neutropenic patients with haematological malignancies. J. Med. Microbiol. 57601-604. [DOI] [PubMed] [Google Scholar]
- 4.Mancini, N., C. M. Ossi, M. Perotti, M. Clementi, D. B. Digiulio, J. M. Schaenman, J. G. Montoya, N. B. McClenny, G. J. Berry, L. F. Mirels, M. G. Rinaldi, and A. W. Fothergill. 2005. Molecular mycological diagnosis and correct antimycotic treatments. J. Clin. Microbiol. 433584-3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nolte, F. S., and A. M. Caliendo. 2007. Molecular detection and identification of microorganisms. In P. R. Murray (ed.), Manual of clinical microbiology, 9th ed., vol. 1. ASM Press, Washington, DC.
- 6.Peters, R. P., M. A. van Agtmael, S. A. Danner, P. H. Savelkoul, and C. M. Vandenbroucke-Grauls. 2004. New developments in the diagnosis of bloodstream infections. Lancet Infect. Dis. 4751-760. [DOI] [PubMed] [Google Scholar]
- 7.Pryce, T. M., S. Palladino, I. D. Kay, and G. W. Coombs. 2003. Rapid identification of fungi by sequencing the ITS1 and ITS2 regions using an automated capillary electrophoresis system. Med. Mycol. 41369-381. [DOI] [PubMed] [Google Scholar]