Abstract
Anxiety has both functionally appropriate and inappropriate consequences. Among patients with cardiac disease, anxiety can be functionally appropriate when it prompts an individual to quickly seek treatment for acute cardiac signs and symptoms. But anxiety may have medical or psychological consequences when it is persistent or severe, including difficulty adhering to prescribed treatments and making recommended lifestyle changes, adoption of or failure to change risky behaviors, increased risk for acute cardiac events, and increased risk for in-hospital complications after admission for acute coronary syndrome. Yet, because anxiety is a universal emotion that is managed without consequence by many people, its importance is often ignored by healthcare providers. The impact of psychosocial (with a major emphasis on anxiety) and behavioral variables on biological outcomes was examined systematically. The research included (1) examination and comparison of the intensity of anxiety in international samples of various critically, acutely, and chronically ill cardiac patients; (2) determination of differences between men and women in the expression of anxiety; (3) investigation of factors predictive of anxiety levels, including perceived control; (4) studies of healthcare providers' knowledge of anxiety assessment and providers' practices in assessing and managing anxiety; and (5) determination of the impact of anxiety on clinical outcomes in cardiac patients. The goal of this program of research is to improve patients' outcomes on a widespread basis by placing anxiety in the forefront of clinical cardiac practice.
Anxiety is the rust of life, destroying its brightness and weakening its power.
Tyron Edwards
It is the rare person who has not felt anxiety at one time or another. For most people, anxiety is transient and of small consequence. Some even seem to thrive on the stimulation of mild anxiety, and evidence suggests that creativity is enhanced slightly with anxiety. Because anxiety is a common emotion that is easily managed by most people, its consequences tend to be underappreciated. I present the outcomes of a program of research to delineate the manifestations and outcomes of anxiety in cardiovascular patients.
Despite notable advances in its management, cardiovascular disease remains the No. 1 cause of death and a major cause of disability among women and men in the United States and most developed countries. By the year 2020, cardiovascular disease is projected to be the No. 1 cause of death throughout the developed and developing world.1-3 The impact of demographic and clinical characteristics on the expression of acute cardiac events and on short- and long-term recovery has been well delineated.4 As a result, these demographic and clinical characteristics are used in clinical practice to project patients' risk for future events.
Far fewer investigations have focused on the impact of psychological risk factors on outcomes, despite evidence that the impact of psychological risk factors on morbidity and mortality is at least equal to the impact of demographic or clinical risk factors.5-7 Underappreciation of the role that psychological risk factors play in the development and progression of cardiovascular disease may be one reason that the morbidity and mortality of cardiovascular disease remain high. Anxiety symptoms and disorders are among the most prevalent psychiatric conditions.6 Given the prevalence of anxiety in the general population and in patients with cardiovascular disease, the potential for improving public health is high if anxiety is identified and treated appropriately.
The impact of psychological risk factors on morbidity and mortality is at least equal to the impact of demographic or clinical risk factors.
The Phenomenon of Anxiety
Anxiety is a negative emotion that occurs in response to perceived threats that can come from internal or external sources and can be real or imagined. Anxiety is characterized by a perceived inability to predict, control, or gain the preferred results when confronted with a threat.8 Anxiety, like all emotions, has cognitive, neurobiological, and behavioral components. Although anxiety often is comorbid with depression, it is a distinct emotion.6 Usually characterized as a detrimental emotion, anxiety can be protective when it triggers coping responses that protect an individual from threats. In this way, anxiety may be adaptive, but it becomes maladaptive when it increases or persists to such a degree that the individual can no longer function effectively in everyday life. At this stage, anxiety can have negative consequences for the individual.
Anxiety exists on a continuum from normal to pathological, and a number of anxiety disorders exist (panic disorder, phobic anxiety, generalized anxiety, anxiety reactions, chronic anxiety).6,8 Despite the variety of manifestations of anxiety, evidence indicates that anxiety reactions at all stages along the continuum have similar cognitive, neurobiological, and behavioral components, and clinically diagnosed anxiety and subclinical anxiety are not fundamentally different phenomena.6,8-10 Thus, the potential link between anxiety and risk for cardiovascular disease events has implications for persons who have signs or symptoms of anxiety, and not just patients in whom a clinical anxiety disorder has been diagnosed.6,10,11
Anxiety in Persons With Cardiovascular Disease
Anxiety is common, even more so than depression, among persons with chronic cardiovascular disease and among those coping with recovery from acute cardiac events or interventions.6,12-17 The prevalence of anxiety is high at approximately 70% to 80% among patients who have experienced an acute cardiac event; anxiety persists over the long term in about 20% to 25% of patients with cardiovascular disease.12,15,16 Even among patients with diagnosed cardiovascular disease who have not experienced an acute event or required intervention, the prevalence of anxiety is about 20% to 25%.14 Although anxiety is an expected and even normal reaction to an acute cardiac event or the threats of living with a chronic illness, anxiety that is persistent or extreme is not normal and has negative consequences for patients' health.5-7,11,13,14,18-21
Anxiety can hinder psychosocial adjustment to the chronicity of cardiovascular disease and physical recovery after an acute event. Higher anxiety is predictive of worse quality of life among patients with cardiovascular disease.18,22-24 Anxiety hinders patients' self-care abilities13,25; patients who are overly anxious often cannot learn or act on information about lifestyle changes and have difficulties adhering to prescriptions for medication, activity, and diet.25-27 Anxious patients experience problems coping with challenges; they perceive challenges as insurmountable barriers.25-27 Persistent anxiety is predictive of disability, increase in physical signs and symptoms, and worse functional status.28,29 Anxious patients with cardiovascular disease return to work at a slower rate or not at all compared with nonanxious patients.30 Anxiety also interferes with patients' return to sexual activity after an acute cardiovascular event.31 Patients with sustained anxiety may experience “cardiac invalidism,” a term that has fallen out of common use but that effectively describes a subset of patients with cardiovascular disease whose level of debilitation or disability after a diagnosis of cardiovascular disease or an acute event is unexplained by the severity of their physical condition.28,29,32
Despite the importance of anxiety to recovery in patients with cardiovascular disease, particularly patients with acute myocardial infarction (AMI), few investigators have examined the phenomenon. My colleagues and I have focused on anxiety in patients with AMI. Our results include the following.
Anxiety After AMI
Prevalence in an International Sample
Although the prevalence of anxiety in North American patients with AMI has been described,12,16 anxiety has not been studied in other cultures. Understanding anxiety from an international perspective is important because most likely anxiety is a significant threat to all AMI patients. In addition, the United States is increasingly multicultural, and we live in a world where a global perspective must be adopted by researchers to combat escalating global health problems.
My colleagues and I have shown (discussed more thoroughly later) that anxiety after AMI is associated with increased risk of in-hospital complications such as potentially lethal dysrhythmias, continued ischemia, and reinfarction.16,33 Anxiety also is associated with future coronary events and mortality months to years after AMI.34-36 People from all cultures and countries experience anxiety.37 However, cultural or ethnic differences may be apparent in the expression of anxiety or in the biological response to anxiety.38 Culture also may influence perceptions of a stress-producing situation.39 For all of these reasons, investigation of anxiety after AMI in different cultural groups is essential. Accordingly, we conducted a prospective, comparative study to determine whether anxiety levels soon after AMI differed among patients from 5 different countries.40
In this study,40 as in all of our studies of anxiety, we used the anxiety subscale of the Brief Symptom Inventory41 to measure patients' perception of their current level of anxiety. This 6-item subscale is a reliable and valid measure of state anxiety in acutely ill persons.41 This instrument is sensitive for detection of anxiety and is easy for participants to complete. This subscale also was conceptually easier than many of the longer anxiety instruments to translate from English to Korean and Japanese. We have determined that it has excellent psychometric properties when used in patients with AMI and heart failure, and it appears to perform better than the more commonly used Spielberger State-Trait Anxiety Index.42 Using a scale of 0 to 4 (0 = not at all and 4 = extremely), participants rate their level of anxiety in response to the 6 items. The mean score represents the participant's overall level of anxiety. High standard deviations are common and reflect variability in the samples studied.41
Even in those with cardiovascular disease who have not suffered a cardiac event, incidence of anxiety is high.
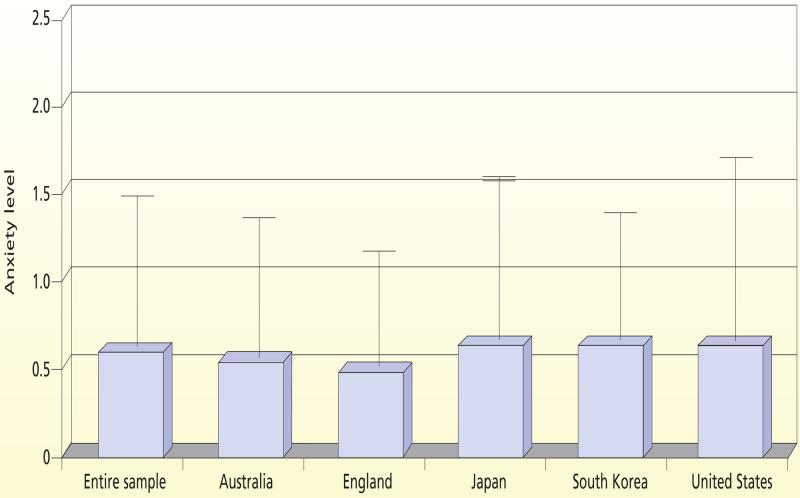
In our study,43 we enrolled 912 AMI patients from a combination of Western and Eastern cultures: 127 from Australia, 144 from England, 136 from Japan, 128 from South Korea, and 377 from the United States. The mean level of anxiety in the entire sample was 44% higher (0.62, standard deviation 0.76) than the normal mean level of 0.35 reported in a sample of healthy adults. Levels of anxiety seen in each country are illustrated in Figure 1. In all countries, patients reported high anxiety levels. A total of 46%, 35%, 43%, 52%, and 50% of patients in Australia, England, Japan, South Korea and the United States, respectively, reported anxiety levels higher than the normal reference mean.
Figure 1.
Mean anxiety levels (with standard deviations) soon after acute myocardial infarction in 912 patients from 5 countries. Anxiety was measured by using the anxiety subscale of the Brief Symptom Inventory; higher numbers indicate higher levels of anxiety.
Modified with permission from De Jong et al.40 Copyright Elsevier, 2004.
Although the anxiety level differed significantly among the countries overall, post hoc testing to discover which countries differed revealed that only England and the United States differed. Patients in England reported lower levels of anxiety than patients in the United States; however, this difference in anxiety level disappeared after we controlled for sociodemographic variables on which the countries differed. Thus, we found that anxiety level soon after AMI was similarly high among patients from 5 diverse countries. Despite the potential influence of culture on emotion,39,44,45 patients have similar emotional responses to AMI.
In summary, AMI patients from each country studied reported high levels of anxiety, suggesting that anxiety after AMI is a universal phenomenon. Given the potentially negative impact of anxiety on prognosis and quality of life after AMI, clinicians and researchers should continue to explore interventions to treat anxiety and minimize its untoward effects.
Differences in Anxiety Between Men and Women
Given the risks associated with anxiety after AMI, it is important to determine which groups of patients are particularly at risk for high anxiety. Women appear to have a higher risk than men do for elevated levels of negative emotions after acute coronary events. It is important to explore differences between the sexes in different cultures to improve planning for international public health initiatives and planning health priorities and initiatives in the United States, which has an increasingly diverse population. In accord with this reasoning, we conducted a sub-study46 of the international study just described to determine whether anxiety differed between men and women in this international sample.
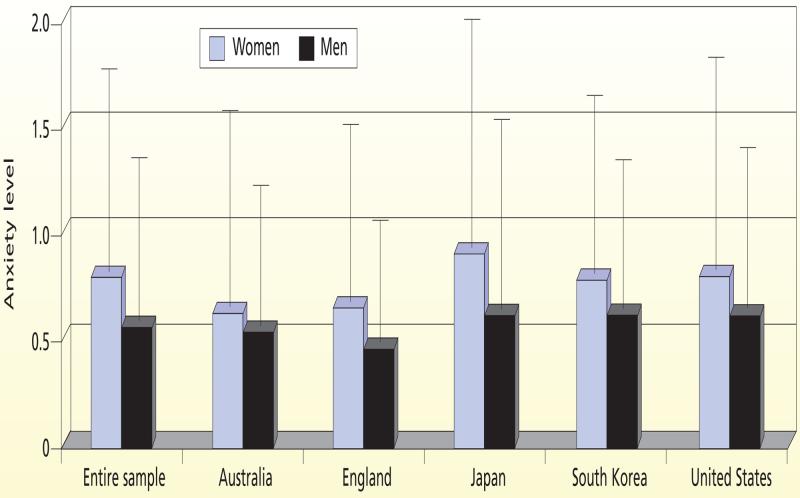
Overall, reported anxiety was significantly higher (P = .005) in women (mean 0.76, standard deviation 0.90) than in men (mean 0.57, standard deviation 0.70). Twice as many women (16%) as men (8%) reported levels of anxiety higher than those of psychiatric patients. This pattern of higher anxiety in women occurred in each country (Figure 2). We conducted 2-factor analyses of variance to determine whether an interaction was present between sex of the patient and sociodemographic variables (ie, age, marital status, education level) or clinical variables (ie, comorbid conditions, pain level, vital signs and Killip classification at admission, medications) that would affect the relationship between sex of the patient and anxiety level. None of these variables interacted with sex of the patient to produce an effect on anxiety.
Figure 2.
Differences between men and women in anxiety soon after acute myocardial infarction for 912 patients from 5 countries. Anxiety was measured by using the anxiety subscale of the Brief Symptom Inventory; higher numbers indicate higher levels of anxiety.
Modified with permission from Moser et al.46
In summary, women were more anxious than men soon after AMI, and this finding was consistent across the Western and Eastern cultures studied. Women reported mean anxiety levels 25% higher than those reported by men, and twice as many women as men in the sample reported anxiety in the extreme ranges. Anxiety should be assessed and managed in all patients, but clinicians must recognize those groups of patients who are at greatest risk for higher anxiety. One area for future research includes study of reasons why women of different cultures appear to be at higher risk than men for anxiety after AMI. Another area for future research is determining whether higher anxiety after AMI contributes to the poorer prognosis seen in women.
Relationship Between Anxiety and Cardiac Outcomes in Patients With Cardiovascular Disease
Studies of the relationship between anxiety and cardiovascular disease include studies among initially healthy persons followed up to detect the occurrence of cardiovascular disease and studies among patients with cardiovascular disease followed up to detect the occurrence of new events related to the cardiovascular disease. Among studies in initially healthy persons, most,47-50 although not all,51 results indicated that anxiety in its many forms was predictive of future AMI or death due to cardiovascular disease, independent of other major risk factors for these outcomes.
Results of studies of the association between anxiety in patients with cardiovascular disease and risk of subsequent cardiovascular disease events are more inconsistent. In 4 studies,16,34,35,52 elevated levels of anxiety were predictive of cardiovascular disease events (ie, reinfarction, unstable angina, death due to cardiovascular disease); in 3 studies,18,22,23,53 no association was detected between anxiety and outcomes of cardiovascular disease; and in 1 study,54 anxiety was associated with a survival advantage. In all but 1 of these studies, subjects were patients hospitalized or undergoing testing who were followed up for months to years to determine outcomes.
In the exception,16 we enrolled hospitalized patients with AMI and studied them during their hospitalization to examine risk of in-hospital complications. In all studies, anxiety was assessed as self-reported symptoms by using different psychometrically sound instruments. In each study, confounding variables were controlled. Despite these similarities in efforts to ensure rigor, this group of studies had different findings that left the research and clinical communities unsure how to interpret the evidence of a link between anxiety and outcomes of cardiovascular disease.55 Thus, further research was needed in this area.
Relationship Between Anxiety and In-Hospital Complications in Patients With AMI
Few investigators have examined the relationship between anxiety and in-hospital complications in patients with AMI. To provide definitive data, we conducted 2 studies designed to determine (1) the association between anxiety soon after AMI and incidence of subsequent in-hospital AMI complications,16 and (2) whether perceived control moderates any association between anxiety and in-hospital complications.33
Women were more anxious than men soon after an AMI—a finding consistent across the Western and Eastern cultures studied.
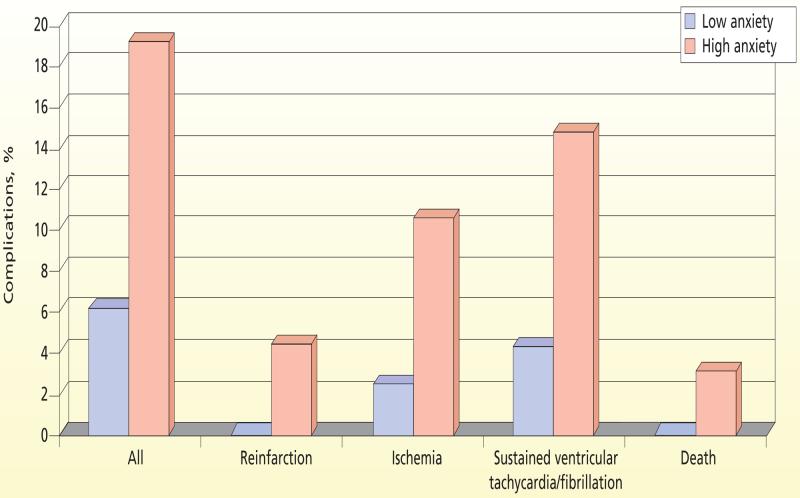
In the first study,16 we used the anxiety subscale of the Brief Symptom Inventory to assess anxiety level within 48 hours of the patient's arrival at the hospital in 86 patients with confirmed AMI. Inhospital complications were defined as reinfarction, recurrent ischemia, ventricular fibrillation, sustained ventricular tachycardia, and in-hospital death.
Mean anxiety level was 1.1 (standard deviation 0.93, range 0-3.3). This anxiety level is greater than the normal sample mean score of 0.35 and similar to the mean score of 1.7 for psychiatric inpatients. Only 26 patients (30%) had scores the same as or less than the norm of 0.35, and 22 patients (26%) had scores of 1.7 or higher. Any of the complications defined in this study occurred in 22 patients (26%). We compared the incidence of complications in patients with high anxiety with the incidence in patients with low levels of anxiety (Figure 3). Complications occurred in 20% of patients with higher anxiety versus 6% of patients with lower anxiety (P = .001). Multiple logistic regression was used to control for clinical and sociodemographic factors that might influence the incidence of complications. Age, sex, Killip classification, thrombolytic therapy regimen, and worst chest pain score were forced into the logistic regression model and then anxiety was forced into the model. The introduction of anxiety significantly improved the model (P = .001). This analysis showed that higher anxiety level was independently predictive of risk of complications. In the final model, only Killip classification (odds ratio 2.7, 95% confidence interval [CI] 1.9-4.7, P = .001) and anxiety (odds ratio 4.9, 95% CI 2.1-12.2, P = .003) contributed significantly to the model. Patients with Killip class II AMI had 2.7 times the risk of complications that patients with Killip class I AMI had. When the other factors were controlled for, patients with higher anxiety had 4.9 times greater risk of complications than did patients with lower anxiety.
Figure 3.
Comparison of complication rates between patients with acute myocardial infarction who had low levels of anxiety and patients with acute myocardial infarction who had high levels of anxiety.
Modified with permission from Moser et al.33
Anxiety among initially healthy persons often predicts future acute myocar-dial infarction or death due to cardiovascular disease, independent of other major risk factors.
In the second study,33 we recruited a larger, more diverse sample and considered the interaction of perceived control with anxiety. Our previous work indicated that perceived control moderates dysphoria,19,56-60 and so we hypothesized that perceived control might moderate the relationship between anxiety and complications. We interviewed 536 patients with AMI (mean age 62 years, standard deviation 14 years, 34% female) within 72 hours of admission. Anxiety was measured by using the Brief Symptom Inventory, and perceived control was assessed by using the Cardiac Attitudes Scale.19
Complications were defined as reinfarction, recurrent ischemia, ventricular tachycardia, ventricular fibrillation, and cardiac death. Patients with high levels of anxiety had more complications than did patients with low levels (P < .001). In multivariate logistic regression analysis, higher anxiety was associated with increased risk for complications (odds ratio 1.8, 95% CI 1.4-2.2; P = .001), independent of age, diabetes, previous AMI, type of AMI, and Killip class. The association between anxiety and complications was moderated by perceived control. For patients with low perceived control, 20% of low-anxiety versus 80% of high-anxiety patients had complications (odds ratio 2.0, 95% CI 1.1-3.9, P = .01). In patients with high perceived control, risk did not differ significantly (P > .05) on the basis of anxiety level.
In summary, these 2 studies show that anxiety is independently associated with a higher risk of in-hospital complications in patients with AMI. This relationship is attenuated in patients with high perceived control. Interventions that increase patients' perception of control may help diminish the link between anxiety and poorer outcomes.
Assessment and Management of Anxiety
Given the negative impact of anxiety in cardiac patients, it is essential that clinicians accurately determine which patients have anxiety and then effectively manage that anxiety. Unfortunately, anxiety is rarely considered by clinicians in their routine assessments, and the management of anxiety is not emphasized. In addition, no standardized management regimens for anxiety seem to be available. To better understand anxiety assessment and management practices, we conducted a number of studies that provided data helpful for understanding cardiac critical care practice.
In the first study,61 we examined the extent to which anxiety in patients with AMI hospitalized in the cardiac critical care unit was assessed by clinicians and how clinicians' assessments compared with patients' assessments of the patients' anxiety. Of 101 patients studied, only 45 patients (45%) had any anxiety assessment documented. Of these 45 patients, 26 (58%) were described as anxious without an additional modifier to describe the level of anxiety. Among these 45 patients, 11 (24%) had documentation of behaviors of anxiety, again without modifiers to indicate level of anxiety. All patients were divided into 4 groups on the basis of their self-reported anxiety score (assessed by means of the Spielberger State Anxiety Index). The percentages of patients in whom clinicians recorded an anxiety assessment were similar in the 4 groups.
When patients' self-assessments were compared with their clinicians' assessments, no association was found between the two. Thus, we found that anxiety was not routinely assessed even though close to half of the patients studied reported moderate or extreme anxiety. When anxiety was assessed by a nurse or a physician, patients' self-rating of anxiety poorly matched the clinician's rating. The lack of attention to the appropriate assessment of anxiety suggests that a simple, easy-to-use instrument that discriminates levels of anxiety is needed.
On the basis of these findings, we sought to determine clinicians' anxiety assessment and management practices at a number of sites across the United States. We conducted a survey of critical care nurses by using a random sample of members of the American Association of Critical-Care Nurses.62-65 A total of 783 nurses participated. Of these, 74% thought that anxiety is potentially harmful (mean score 4.1, standard deviation 0.8, where 1 = no harm and 5 = life-threatening harm), that anxiety management is important (mean score 4.8, standard deviation 0.6, where 1 = not important and 5 = very important), and that effective anxiety management is beneficial (mean score 4.6, standard deviation 0.6, where 1 = no benefit and 5 = profound benefit).63 A majority reported using pharmacological management of anxiety; most also used interventions related to providing information and communication. Fewer used the presence of a patient's family member for anxiety alleviation or reported using stress-reduction techniques.
Nurses responding to the survey indicated that agitation, increased blood pressure, increased heart rate, patients' verbalization of anxiety, and restlessness are the most important indicators of anxiety to consider when assessing for anxiety.64 In the qualitative arm of the same study, nurses reported that they most often used restlessness, increased heart rate, agitation, increased blood pressure, increased respiratory rate, and increased diaphoresis as indications of anxiety.65 Less than 5% of nurses considered a patient's verbalization of anxiety as an important element in their anxiety assessment.
These findings are of concern because physiological signs and symptoms of anxiety may not be useful in assessing acutely ill patients for anxiety. To determine the extent to which heart rate and blood pressure were related to level of anxiety, we studied these parameters in patients with chronic advanced heart failure, patients with AMI, and healthy persons.66 We found no association between anxiety and heart rate or diastolic blood pressure in any of the 3 groups. Higher anxiety was associated with lower systolic blood pressure in patients with AMI (r = -0.23, P < .05) and in healthy persons (r = -0.27, P < .05). Mean systolic blood pressure, diastolic blood pressure, and heart rate were similar for subjects in high- and low-anxiety subgroups among patients and healthy persons. A comparison of medications between the high- and low-anxiety groups revealed no differences that would account for these findings. Thus, increased heart rate and blood pressure do not reflect level of anxiety accurately and should not be used to assess anxiety in acutely ill patients. Clinicians who use changes in heart rate or blood pressure as indicators of anxiety may not recognize and then treat anxiety, potentially placing patients at risk for the consequences of untreated anxiety.
Increased heart rate and blood pressure do not reflect level of anxiety accurately and should not be used to assess anxiety in acutely ill patients.
Summary
Anxiety is common among cardiac patients, has potentially serious consequences if untreated, and yet is infrequently assessed or managed appropriately. Anxiety assessment and treatment should be a part of the care of every cardiac patient in order to enhance recovery and decrease patients' risk of recurrent cardiac events. Further research in this area should be focused on delineating the mechanisms whereby anxiety causes poorer outcomes. We hypothesize that both physiological (eg, activation of the sympathetic nervous system) and behavioral (eg, poor adherence) mechanisms mediate the link between anxiety and poor outcomes, and we are testing this hypothesis. Research in this area is important to help clinicians determine the best ways to manage patients to decrease the adverse effects of anxiety. It is also vital to develop and test interventions that both decrease anxiety and improve the adverse outcomes associated with anxiety. In this regard, the role of nonpharmacological and pharmacological strategies must be investigated. Ultimately, the goal of our program of research will be realized if all clinicians realize the importance of anxiety to their patients' outcomes and seriously engage in assessment and management of anxiety.
Footnotes
FINANCIAL DISCLOSURES Funding for studies reported in this article was received from an AACN Sigma Theta Tau Research Grant; Bennett-Puritan AACN Mentorship Award; Sigma Theta Tau; Philips Medical-AACN Research Award; and a National Institutes of Health, National Institute of Nursing Research grant, R01 NR008567.
eLetters Now that you've read the article, create or contribute to an online discussion about this topic using eLetters. Just visit www.ajcconline.org and click “Respond to This Article” in either the full-text or .pdf view of the article.
About the Author Debra K. Moser is a professor and holds the Gill Endowed Chair of Nursing at the University of Kentucky College of Nursing in Lexington.
SEE ALSO For more about the relationship between stress and cardiac outcomes, visit http://ccn.aacnjournals.org and read the article by Bally and colleagues, “Effects of Patient-Controlled Music Therapy During Coronary Angiography on Procedural Pain and Anxiety Distress Syndrome” (Critical Care Nurse, April 2003).
To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 809-2273 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org.
Presented May 21, 2007, at the AACN National Teaching Institute, Atlanta, Georgia.
REFERENCES
- 1.Chockalingam A, Balaguer-Vintro I, Achutti A, et al. The World Heart Federation's white book. Impending global pandemic of cardiovascular diseases: challenges and opportunities for the prevention and control of cardiovascular diseases in developing countries and economies in transition. Can J Cardiol. 2000;16:227–229. [PubMed] [Google Scholar]
- 2.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 3.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [published correction appears in Circulation. 2007;115(5):e172] [DOI] [PubMed] [Google Scholar]
- 4.Breithardt G, Borggrefe M, Fetsch T, Bocker D, Makijarvi M, Reinhardt L. Prognosis and risk stratification after myocar-dial infarction. Eur Heart J. 1995;16(suppl G):10–19. doi: 10.1093/eurheartj/16.suppl_g.10. [DOI] [PubMed] [Google Scholar]
- 5.Kubzansky LD, Kawachi I. Going to the heart of the matter: do negative emotions cause coronary heart disease? J Psychosom Res. 2000;48:323–337. doi: 10.1016/s0022-3999(99)00091-4. [DOI] [PubMed] [Google Scholar]
- 6.Kubzansky LD, Kawachi I, Weiss ST, Sparrow D. Anxiety and coronary heart disease: a synthesis of epidemiological, psychological, and experimental evidence. Ann Behav Med. 1998;20:47–58. doi: 10.1007/BF02884448. [DOI] [PubMed] [Google Scholar]
- 7.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 8.Barlow DH. Anxiety and Its Disorders. Guilford Press; New York, NY: 1988. [Google Scholar]
- 9.Lewis MA, Haviland JM, editors. Fear and Anxiety as Emotional Phenomena: Clinical Phenomenology, Evolutionary Perspectives, and Information-Processing Mechanisms. Guilford Press; New York, NY: 1993. Handbook of Emotions. [Google Scholar]
- 10.Smith TW, Ruiz JM. Psychosocial influences on the development and course of coronary heart disease: current status and implications for research and practice. J Consult Clin Psychol. 2002;70:548–568. doi: 10.1037//0022-006x.70.3.548. [DOI] [PubMed] [Google Scholar]
- 11.Kubzansky LD, Kawachi I, Spiro A, III, Weiss ST, Vokonas PS, Sparrow D. Is worrying bad for your heart? A prospective study of worry and coronary heart disease in the Normative Aging Study. Circulation. 1997;95:818–824. doi: 10.1161/01.cir.95.4.818. [DOI] [PubMed] [Google Scholar]
- 12.Crowe JM, Runions J, Ebbesen LS, Oldridge NB, Streiner DL. Anxiety and depression after acute myocardial infarction. Heart Lung. 1996;25:98–107. doi: 10.1016/s0147-9563(96)80111-7. [DOI] [PubMed] [Google Scholar]
- 13.Malan SS. Psychosocial adjustment following MI: current views and nursing implications. J Cardiovasc Nurs. 1992;6(4):57–70. doi: 10.1097/00005082-199207000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Januzzi JL, Jr, Stern TA, Pasternak RC, DeSanctis RW. The influence of anxiety and depression on outcomes of patients with coronary artery disease. Arch Intern Med. 2000;160:1913–1921. doi: 10.1001/archinte.160.13.1913. [DOI] [PubMed] [Google Scholar]
- 15.Moser DK, McKinley S, Riegel B, Doering LV, Garvin BJ. Perceived control reduces in-hospital complications associated with anxiety in acute myocardial infarction [abstract] Circulation. 2002;106:II–369. [Google Scholar]
- 16.Moser DK, Dracup K. Is anxiety early after myocardial infarction associated with subsequent ischemic and arrhythmic events? Psychosom Med. 1996;58:395–401. doi: 10.1097/00006842-199609000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Sirois BC, Burg MM. Negative emotion and coronary heart disease: a review. Behav Modif. 2003;27:83–102. doi: 10.1177/0145445502238695. [DOI] [PubMed] [Google Scholar]
- 18.Mayou RA, Gill D, Thompson DR, Day A, Hicks N, Volmink J, Neil A. Depression and anxiety as predictors of outcome after myocardial infarction. Psychosom Med. 2000;62:212–219. doi: 10.1097/00006842-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Moser DK, Dracup K. Psychosocial recovery from a cardiac event: the influence of perceived control. Heart Lung. 1995;24:273–280. doi: 10.1016/s0147-9563(05)80070-6. [DOI] [PubMed] [Google Scholar]
- 20.Rozanski A, Bairey CN, Krantz DS, et al. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med. 1988;318:1005–1012. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 21.Rozanski A, Krantz DS, Bairey CN. Ventricular responses to mental stress testing in patients with coronary artery disease: pathophysiological implications. Circulation. 1991;83(4 suppl):III137–III144. [PubMed] [Google Scholar]
- 22.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Effects of depression and anxiety on mortality and quality-of-life 4 months after myocardial infarction. J Psychosom Res. 2000;49:229–238. doi: 10.1016/s0022-3999(00)00170-7. [DOI] [PubMed] [Google Scholar]
- 23.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Do depression and anxiety predict recurrent coronary events 12 months after myocardial infarction? QJM. 2000;93(11):739–744. doi: 10.1093/qjmed/93.11.739. [DOI] [PubMed] [Google Scholar]
- 24.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Mortality and quality of life 12 months after myocardial infarction: effects of depression and anxiety. Psychosom Med. 2001;63:221–230. doi: 10.1097/00006842-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Maeland JG, Havik OE. After the myocardial infarction: a medical and psychological study with special emphasis on perceived illness. Scand J Rehabil Med Suppl. 1989;22:1–87. [PubMed] [Google Scholar]
- 26.Rose SK, Conn VS, Rodeman BJ. Anxiety and self-care following myocardial infarction. Issues Ment Health Nurs. 1994;15:433–444. doi: 10.3109/01612849409006919. [DOI] [PubMed] [Google Scholar]
- 27.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Predictors of attendance at cardiac rehabilitation after myocardial infarction. J Psychosom Res. 2001;51:497–501. doi: 10.1016/s0022-3999(01)00225-2. [DOI] [PubMed] [Google Scholar]
- 28.Sullivan MD, LaCroix AZ, Baum C, Grothaus LC, Katon WJ. Functional status in coronary artery disease: a one-year prospective study of the role of anxiety and depression. Am J Med. 1997;103:348–356. doi: 10.1016/s0002-9343(97)00167-8. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan MD, LaCroix AZ, Spertus JA, Hecht J. Five-year prospective study of the effects of anxiety and depression in patients with coronary artery disease. Am J Cardiol. 2000;86:1135–1138. A1136, A1139. doi: 10.1016/s0002-9149(00)01174-7. [DOI] [PubMed] [Google Scholar]
- 30.Havik OE, Maeland JG. Patterns of emotional reactions after a myocardial infarction. J Psychosom Res. 1990;34:271–285. doi: 10.1016/0022-3999(90)90083-g. [DOI] [PubMed] [Google Scholar]
- 31.Rosal MC, Downing J, Littman AB, Ahern DK. Sexual functioning post-myocardial infarction: effects of beta-blockers, psychological status and safety information. J Psychosom Res. 1994;38:655–667. doi: 10.1016/0022-3999(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 32.Sykes DH, Evans AE, Boyle DM, McIlmoyle EL, Salathia KS. Discharge from a coronary care unit: psychological factors. J Psychosom Res. 1989;33:477–488. doi: 10.1016/0022-3999(89)90009-3. [DOI] [PubMed] [Google Scholar]
- 33.Moser DK, Riegel B, McKinley S, Doering LV, An K, Sheahan S. Impact of anxiety and perceived control on in-hospital complications after acute myocardial infarction. Psychosom Med. 2007;69:10–16. doi: 10.1097/01.psy.0000245868.43447.d8. [DOI] [PubMed] [Google Scholar]
- 34.Frasure-Smith N, Lesperance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol. 1995;14:388–398. doi: 10.1037//0278-6133.14.5.388. [DOI] [PubMed] [Google Scholar]
- 35.Denollet J, Brutsaert DL. Personality, disease severity, and the risk of long-term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation. 1998;97:167–173. doi: 10.1161/01.cir.97.2.167. [DOI] [PubMed] [Google Scholar]
- 36.Thomas SA, Friedmann E, Wimbush F, Schron E. Psychological factors and survival in the Cardiac Arrhythmia Suppression Trial (CAST): a reexamination. Am J Crit Care. 1997;6:116–126. [PubMed] [Google Scholar]
- 37.Lepine JP. Epidemiology, burden, and disability in depression and anxiety. J Clin Psychiatry. 2001;62(suppl 13):4–12. [PubMed] [Google Scholar]
- 38.Lin KM. Biological differences in depression and anxiety across races and ethnic groups. J Clin Psychiatry. 2001;62(suppl 13):13–21. [PubMed] [Google Scholar]
- 39.Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: implications for diagnosis and treatment. J Clin Psychiatry. 2001;62(suppl 13):22–30. [PubMed] [Google Scholar]
- 40.De Jong MJ, Chung ML, Roser LP, et al. A five-country comparison of anxiety early after acute myocardial infarction. Eur J Cardiovasc Nurs. 2004;3:129–134. doi: 10.1016/j.ejcnurse.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 41.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 42.Abu Ruz MA, Lennie TA, Riegel B, et al. Anxiety can be measured quickly and reliably in patients hospitalized for acute myocardial infarction [abstract] Circulation. 2005;112:II–392. doi: 10.1097/JCN.0b013e3181b56626. [DOI] [PubMed] [Google Scholar]
- 43.Derogatis LP. BSI, Brief Symptom Inventory: Administration, Scoring, and Procedure Manual. National Computer Systems Inc; Minneapolis, MN: 1993. [Google Scholar]
- 44.Draguns JG, Tanaka-Matsumi J. Assessment of psychopathology across and within cultures: issues and findings. Behav Res Ther. 2003;41:755–776. doi: 10.1016/s0005-7967(02)00190-0. [DOI] [PubMed] [Google Scholar]
- 45.Taylor-Piliae RE, Molassiotis A. An exploration of the relationships between uncertainty, psychological distress and type of coping strategy among Chinese men after cardiac catheterization. J Adv Nurs. 2001;33:79–88. doi: 10.1046/j.1365-2648.2001.01640.x. [DOI] [PubMed] [Google Scholar]
- 46.Moser DK, Dracup K, Doering LV, et al. Sex difference in anxiety early after acute myocardial infarction: an international perspective. Psychosom Med. 2003;65:511–516. doi: 10.1097/01.psy.0000041543.74028.10. [DOI] [PubMed] [Google Scholar]
- 47.Kawachi I, Colditz GA, Ascherio A, et al. Prospective study of phobic anxiety and risk of coronary heart disease in men. Circulation. 1994;89:1992–1997. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- 48.Kawachi I, Sparrow D, Vokonas PS, Weiss ST. Symptoms of anxiety and risk of coronary heart disease: the Normative Aging Study. Circulation. 1994;90:2225–2229. doi: 10.1161/01.cir.90.5.2225. [DOI] [PubMed] [Google Scholar]
- 49.Haines AP, Imeson JD, Meade TW. Phobic anxiety and ischaemic heart disease. Br Med J (Clin Res Ed) 1987;295(6593):297–299. doi: 10.1136/bmj.295.6593.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol. 1992;135:854–864. doi: 10.1093/oxfordjournals.aje.a116381. [DOI] [PubMed] [Google Scholar]
- 51.Martin RL, Cloninger CR, Guze SB, Clayton PJ. Mortality in a follow-up of 500 psychiatric outpatients, I: total mortality. Arch Gen Psychiatry. 1985;42:47–54. doi: 10.1001/archpsyc.1985.01790240049005. [DOI] [PubMed] [Google Scholar]
- 52.Herrmann C, Brand-Driehorst S, Kaminsky B, Leibing E, Staats H, Ruger U. Diagnostic groups and depressed mood as predictors of 22-month mortality in medical inpatients. Psychosom Med. 1998;60:570–577. doi: 10.1097/00006842-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med. 2000;247:629–639. doi: 10.1046/j.1365-2796.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- 54.Herrmann C, Brand-Driehorst S, Buss U, Ruger U. Effects of anxiety and depression on 5-year mortality in 5,057 patients referred for exercise testing. J Psychosom Res. 2000;48:455–462. doi: 10.1016/s0022-3999(99)00086-0. [DOI] [PubMed] [Google Scholar]
- 55.Bunker SJ, Colquhoun DM, Esler MD, et al. “Stress” and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178:272–276. doi: 10.5694/j.1326-5377.2003.tb05193.x. [DOI] [PubMed] [Google Scholar]
- 56.Moser DK, Dracup K. Role of spousal anxiety and depression in patients' psychosocial recovery after a cardiac event. Psychosom Med. 2004;66:527–532. doi: 10.1097/01.psy.0000130493.80576.0c. [DOI] [PubMed] [Google Scholar]
- 57.Evangelista LS, Moser D, Dracup K, Doering L, Kobashigawa J. Functional status and perceived control influence quality of life in female heart transplant recipients. J Heart Lung Transplant. 2004;23:360–367. doi: 10.1016/S1053-2498(03)00196-7. [DOI] [PubMed] [Google Scholar]
- 58.Dracup K, Evangelista LS, Doering L, Tullman D, Moser DK, Hamilton M. Emotional well-being in spouses of patients with advanced heart failure. Heart Lung. 2004;33:354–361. doi: 10.1016/j.hrtlng.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 59.Dracup K, Westlake C, Erickson VS, Moser DK, Caldwell ML, Hamilton MA. Perceived control reduces emotional stress in patients with heart failure. J Heart Lung Transplant. 2003;22:90–93. doi: 10.1016/s1053-2498(02)00454-0. [DOI] [PubMed] [Google Scholar]
- 60.Moser DK, Dracup K. Impact of cardiopulmonary resuscitation training on perceived control in spouses of recovering cardiac patients. Res Nurs Health. 2000;23:270–278. doi: 10.1002/1098-240x(200008)23:4<270::aid-nur3>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 61.O'Brien JL, Moser DK, Riegel B, Frazier SK, Garvin BJ, Kim KA. Comparison of anxiety assessments between clinicians and patients with acute myocardial infarction in cardiac critical care units. Am J Crit Care. 2001;10:97–103. [PubMed] [Google Scholar]
- 62.Frazier SK, Moser DK, O'Brien JL, Garvin BJ, An K, Macko M. Management of anxiety after acute myocardial infarction. Heart Lung. 2002;31:411–420. doi: 10.1067/mhl.2002.129445. [DOI] [PubMed] [Google Scholar]
- 63.Frazier SK, Moser DK, Daley LK, et al. Critical care nurses' beliefs about and reported management of anxiety. Am J Crit Care. 2003;12:19–27. [PubMed] [Google Scholar]
- 64.Frazier SK, Moser DK, Riegel B, et al. Critical care nurses' assessment of patients' anxiety: reliance on physiological and behavioral parameters. Am J Crit Care. 2002;11:57–64. [PubMed] [Google Scholar]
- 65.Moser DK, Chung ML, McKinley S, et al. Critical care nursing practice regarding patient anxiety assessment and management. Intensive Crit Care Nurs. 2003;19:276–288. doi: 10.1016/s0964-3397(03)00061-2. [DOI] [PubMed] [Google Scholar]
- 66.De Jong MJ, Moser DK, An K, Chung ML. Anxiety is not manifested by elevated heart rate and blood pressure in acutely ill cardiac patients. Eur J Cardiovasc Nurs. 2004;3:247–253. doi: 10.1016/j.ejcnurse.2004.06.006. [DOI] [PubMed] [Google Scholar]