Abstract
Purpose
The purpose of this study was to describe how coping styles among African Americans with type 2 diabetes relate to diabetes appraisals, self-care behaviors, and health-related quality of life or well-being.
Methods
This cross-sectional analysis of baseline measures from 185 African Americans with type 2 diabetes enrolled in a church-based randomized controlled trial uses the theoretical framework of the transactional model of stress and coping to describe bivariate and multivariate associations among coping styles, psychosocial factors, self-care behaviors, and well-being, as measured by validated questionnaires.
Results
Among participants who were on average 59 years of age with 9 years of diagnosed diabetes, passive and emotive styles of coping were used most frequently, with older and less educated participants using more often passive forms of coping. Emotive styles of coping were significantly associated with greater perceived stress, problem areas in diabetes, and negative appraisals of diabetes control. Both passive and active styles of coping were associated with better diabetes self-efficacy and competence in bivariate analysis. In multivariate analysis, significant proportions of the variance in dietary behaviors and mental well-being outcomes (general and diabetes specific) were explained, with coping styles among the independent predictors. A positive role for church involvement in the psychological adaptation to living with diabetes was also observed.
Conclusions
In this sample of older African Americans with diabetes, coping styles were important factors in diabetes appraisals, self-care behaviors, and psychological outcomes. These findings suggest potential benefits in emphasizing cognitive and behavioral strategies to promote healthy coping outcomes in persons living with diabetes.
African Americans living with diabetes cope every day with stress from the disease itself, fear of complications secondary to diabetes, and other social factors. Among African Americans older than 20 years of age, 1 in 10 lives with type 2 diabetes, and among African American women older than age 55, rates are as high as 1 in 4.1 In addition to higher prevalence rates (1.8 times higher than Caucasian Americans), African Americans suffer greatly from the complications of diabetes, resulting in rates of blindness, kidney disease, and lower limb amputations that are 2 to 5 times that of Caucasian Americans.1 Given this context, it may be important to understand how African American adults with diabetes cope with the stress of living with diabetes.
Understanding how African Americans cope with diabetes is important to developing strategies for promoting healthful self-care behaviors and enhancing psychological and physical well-being. The relationships among coping, stress, and one’s appraisal of a stressful event or situation have been explored in a small number of studies among patients with diabetes.2–6 Only a few studies, however, specifically address the coping styles of African Americans with diabetes,7–10 and most have been qualitative research with very small study samples. More generally, racial differences in the use of coping strategies have been suggested. Studies suggest that Caucasians predominately use problem-solving coping mechanisms, whereas African Americans rely more on emotion-focused or affective coping and less on active forms of coping.11 In the diabetes context, studies list religious activity or spirituality as prevalent coping efforts among African Americans.10,12,13 Other research identifies family and individual resilience, as well as a strong value system, as inherent coping skills for African Americans.14 What is missing from the literature are quantitative data describing how African Americans with diabetes cope with the disease and how their coping styles relate to self-care behaviors and health-related well-being or quality of life.
The purpose of this study is to explore some of these issues by asking the following questions: (1) How do coping styles relate to self-care behaviors and measures of general and diabetes-related quality of life or well-being? (2) What is the association between coping styles and appraisals of diabetes control, competence, and self-efficacy? (3) How does spirituality or church involvement relate to coping styles, well-being, and self-care behaviors? The last question is especially important in this study because of the study sample (selected from church congregations) and research among African Americans that suggests a relationship between church/religious involvement and health.15,16
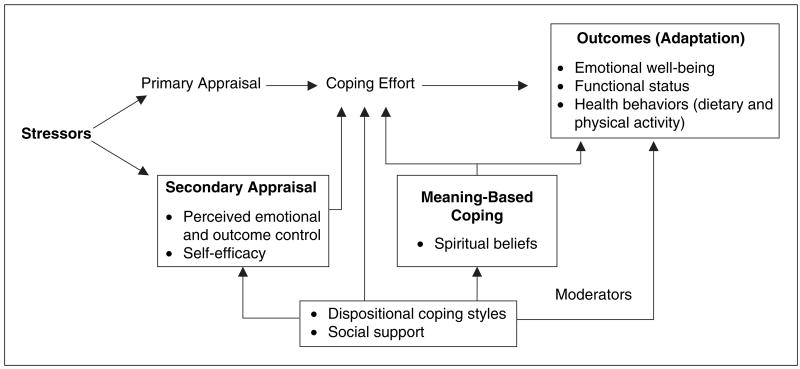
The transactional model of stress and coping17 serves as the theoretical framework (Figure 1) for this study. In this model, perceived stress is conceptualized as a “transactional phenomenon” between person and environment, such that the perception of the event (the appraisal) rather than the event itself determines the subsequent response or behavior. Coping is defined as constantly changing cognitive and behavioral efforts to manage specific internal and/or external demands that are considered taxing or exceeding the resources of an individual.18 Coping styles, in this transactional model, are considered dispositional traits that influence how stressful events are appraised and consequently have an effect on what strategies are used to manage or address the stressor.
Figure 1.
Transactional model of stress and coping17 emphasizing constructs (in boxes) measured in this study.
This study investigated 4 key concepts in the transactional model: dispositional coping styles, stress, secondary appraisals (perceptions of diabetes control, competence, and self-efficacy), and outcomes (self-care behaviors, functional status, and well-being). The transactional framework posits that in the presence of stressors, coping styles influence both secondary appraisals and outcomes—behavioral (self-care) and psychological (quality of life). Coping styles can, therefore, have a direct effect on emotional and physical outcomes of stress, as well as an indirect effect on how stressors are appraised and what is done as a result of the appraisal. In the transactional model, spiritual beliefs and the use of religion induce positive emotions that affect how the process of coping influences outcomes.17
Methods
Setting and Participants
The study staff enrolled members from 24 churches with type 2 diabetes who fit the following inclusion criteria: age 20 or older, diagnosis of type 2 diabetes defined as diagnosis of diabetes at age 20 or older and no history of ketoacidosis, clinical care provided by a primary care clinician, plans to reside within 50 miles of church for 1 year, and having a home phone or easy access to one. Exclusion criteria included the following: diabetes secondary to another condition, pregnancy/lactation, or inability to speak English. Each interested person was scheduled for a 90-minute enrollment visit at the church; additional baseline data were subsequently collected during 2 phone interviews. The Institutional Review Board at the University of North Carolina at Chapel Hill approved the study protocol, and prior to enrollment, each participant gave written informed consent.
Measures and Data Collection
Psychosocial measures
Measures include coping styles, perceived stress, diabetes and general health status, perceived diabetes competence, self-efficacy, perceived barriers, social support, spirituality, and church involvement. Each measure is briefly described below; all scales in these measures have acceptable internal reliability.
Coping styles
A 31-item adaptation of the Jalowiec coping styles measure19 was used. Three coping styles are measured: emotive (coping by emotional strategies such as worrying, getting mad, being nervous or depressed), passive (coping through strategies of acceptance), and active (coping by actions or making plans to act) coping. Factor analysis procedures were used to empirically define each scale. The internal reliability (coefficient alpha) for each scale is as follows: emotive coping (α = 0.80; 5 items), passive coping (α = 0.74; 9 items), and active coping (α = 0.69; 7 items).
Perceived stress
The Perceived Stress Scale (PSS) survey20 is a validated 14-item global measure of the degree to which situations in one’s life are perceived as stressful.
Diabetes and general health status
This validated 24-item measure of health status was developed for African Americans with type 2 diabetes.21 It includes 2 scales measuring social and mental well-being and a physical symptoms index. General health status was measured with the Short Form Health Survey (SF-36).22
Perceived diabetes competence and self-efficacy
Perceived Diabetes and Dietary Competence (PDDC)23 is a validated 20-item measure of one’s perceived level of competence and behavioral control in managing diabetes. The PDDC measure includes 3 scales: positive diabetes competence, negative dietary competence, and negative diabetes control.
Problem areas in diabetes
The Problem Areas In Diabetes (PAID) survey24 includes 20 items measuring the extent to which feelings about living with diabetes were perceived as problems in the past month.
Diabetes self-efficacy
An 11-item survey assessed how sure the respondent feels that he or she would “really stick with” performing diabetes regimen behaviors, including diet, physical activity, self-monitoring, taking medications, and checking feet. The internal reliability of this measure (measured in a sample of 200 African Americans with diabetes) is 0.80.
Spirituality and church involvement
Six items were selected from a survey used with a previous church-based intervention25 to assess spirituality (beliefs about prayer and God’s role in health) and church involvement.
Physiologic measures
These included hemoglobin A1c (A1c), weight, and blood pressure. Using a standard finger-stick technique, 5 μL of capillary blood was collected into a capillary collection vial (Bio-Rad, Hercules, California) and stored at 4°C for the A1c test. The Diabetes Diagnostic Laboratory (University of Missouri, Columbia) performed the analysis for A1c by automated affinity high-performance liquid chromatography (HPLC) on a Primus CLC-330 system (Primus Corp, Kansas City, Missouri). Weight was measured with electronic scales (Seca 770, Seca Corporation, Columbia, Maryland) and blood pressure by the Omron HEM-907 automated blood pressure monitor (Omron Healthcare, Inc, Banockburn, Illinois).
Physical activity (PA)
PA was objectively assessed by the Actigraph (Shalimar, Florida) monitor, formerly known as the CSA WAM 7164 Activity Monitor—a small, uniaxial accelerometer worn on the waist. The stages of behavioral change for PA (being truly physically active) were also assessed using a 6-stage algorithm and a long definition of PA.26 Each stage assesses current PA behaviors and plans for change in the next 30 days to 6 months, with stage 1 being not currently active and having no plans to change in the next 6 months and stage 6 being physically active for more than 6 months. For this report, the PA stage-of-change data were used.
Dietary behavior
Two self-reports of dietary intake were collected. One item27 assessed the number of days a diet for diabetes was followed, and stage of dietary change28,29 was determined using a 5-stage algorithm for 2 behaviors—avoiding foods high in saturated and trans fats and consuming meals with appropriate portions (3 sample meals using 3-dimensional food models were displayed during this assessment).
With the exception of measures of perceived stress level and stages of dietary and physical activity behavior change, which were administered face-to-face at the enrollment visit, all other surveys were administered over the telephone.
Statistical Analysis
Data analyses were conducted using SAS/STAT software (SAS Institute, Cary, North Carolina). Descriptive analyses included frequency distributions and cross-tabulations. For categorical variables, chi-square tests of association were used to evaluate statistically significant relationships. For continuous variables, F tests or their equivalents were used to assess differences between means except when comparisons were performed on ordinal variables. When comparisons between means were performed on ordinal variables, a test accounting for the ordered nature of responses was used; results approximate those of a t test. Pearson product moment correlation coefficients were used to evaluate the relative direction and strength of associations between the 3 types of coping and all other variables of interest. Significant results from the categorical, continuous, and ordinal results were used to determine variables to include in a series of multivariate linear regression models to assess the influence of coping styles on behavioral and psychological outcomes while accounting for the influences of self-appraisal of diabetes control, self-efficacy, spiritual beliefs, and other descriptive covariates. For all tests, statistical significance was based on an alpha of < 0.05.
Results
Study participants (Table 1) can be characterized as mostly women with an average age of 59 years, body mass index (BMI) of 35, 9 years of diagnosed diabetes (median of 6 years), and A1c of 7.8%. The treatment regimen for most participants included only hypoglycemic agents; about 13% to 16% were treated with either insulin or diet alone or a combination of insulin and tablets. These characteristics describe 92% (185/201) of the total study sample. When compared with participants who did not complete the coping styles survey, no differences were found in age, education, years with diagnosed diabetes, or A1c. Because study participants were enrolled from within churches, this study analyzed the possible effect of being in a particular church on means for coping styles and outcomes variables. No significant differences were found among churches.
Table 1.
Participant Characteristics (N = 185)
| Characteristic | Value |
|---|---|
| Age, y | 58.9 ± 12.2 |
| Gender, % | |
| Female | 64.9 |
| Body mass index | 34.9 ± 7.6 |
| Diagnosed diabetes, y | 9.29 ± 8.3 |
| Median (IQR) | 6.0 (12.0) |
| A1c | 7.8 ± 1.8 |
| Diabetes treatment, % | |
| Insulin only | 13.5 |
| Tablets only | 57.3 |
| Combined insulin + tablets | 16.2 |
| Diet only | 13.0 |
| Educational attainment, y | 12.3 ± 3.0 |
| Employed, % | 45.4 |
| Annual household income,a % | |
| <$10 000 | 13.5 |
| $10 000–$29 000 | 20.0 |
| $30 000–$49 000 | 12.4 |
| $50 000–$69 000 | 6.5 |
| >$70 000 | 7.6 |
| Unknown | 40.0 |
Values are mean ± SD unless otherwise indicated. IQR, interquartile range.
n = 74 (40%) of the sample elected not to provide income data.
Study participants reported using passive forms of coping most frequently, followed by emotive and active styles. Table 2 shows the correlations between coping styles and 3 categories of factors: demographic, psychosocial, and behavioral. Among demographic factors, the strongest associations were observed between passive coping and both age and educational attainment. Older persons and those with lower levels of educational attainment reported using passive forms of coping more frequently. Weak but significant direct associations were observed with BMI and both emotive and active coping. In comparing group means, no significant gender differences in coping styles were found, but among the unemployed, both passive and emotive styles of coping were used more frequently.
Table 2.
Correlation With Demographic, Psychosocial, and Behavioral Factors
| Coping Style |
|||
|---|---|---|---|
| Emotive | Passive | Active | |
| Demographic Factors | |||
| Age | −0.08 | 0.28*** | −0.05 |
| Body mass index | 0.17* | −0.12 | 0.15* |
| Educational attainment | −0.06 | −0.30**** | 0.17* |
| Years with diagnosed diabetes | −0.04 | 0.17* | −0.02 |
| Hemoglobin A1c | 0.09 | −0.03 | −0.05 |
| Psychosocial factors | |||
| Perceived stress | 0.62**** | −0.16* | −0.02 |
| Problem Areas in Diabetes (PAID) | 0.42**** | −0.10 | 0.08 |
| Negative diabetes control | 0.28*** | 0.08 | 0.05 |
| Perceived diabetes competence | −0.13 | 0.29**** | 0.24** |
| Self-efficacy (diabetes) | −0.16* | 0.31**** | 0.22** |
| Diabetes-related quality of life, mental well-being | −0.30**** | −0.13 | −0.16* |
| General–mental well-being (n =155) | −0.52**** | 0.03 | 0.02 |
| General–physical well-being (n =155) | −0.07 | −0.08 | 0.04 |
| Spirituality and health | 0.00 | 0.23** | 0.11 |
| Church services attended monthly | −0.13 | −0.04 | −0.19* |
| Behavioral factors | |||
| Stage of behavioral change: | |||
| Dietary fat (saturated fatty acids, trans fat) | −0.02 | 0.18* | 0.26*** |
| Portion control | −0.20** | 0.01 | 0.05 |
| Physical activity | −0.11 | 0.00 | −0.08 |
| Number of days following diet for diabetes | 0.10 | −0.25*** | −0.28*** |
Pearson product moment correlations.
P < .05.
P < .01.
P < .001.
P < .0001.
Among the psychosocial factors, a number of significant associations were observed with emotive coping. Participants who reported frequent use of emotive coping also perceived greater levels of stress, more problem areas in diabetes, and negative appraisals of diabetes control. In contrast, emotive coping was negatively associated with both diabetes-specific and general mental well-being scores. Passive and active coping were directly associated with appraisals of diabetes self-efficacy and competence. Using single-item measures of spirituality (as it relates to health) and church involvement, it was observed that more frequent use of passive coping was directly related to beliefs that one’s health “is mostly in God’s hands,” and more active coping styles were associated with fewer church services attended monthly.
Coping styles were only weakly related to dietary behaviors and unrelated to physical activity behaviors. Active styles of coping were more common among participants who reported that they were currently avoiding saturated and trans fats in their diet and following a diet for diabetes most days of the week; similar associations were observed for passive coping styles. Only emotive coping styles were associated with portion control (with more frequent use of emotive coping associated with larger meal portions).
The multivariate analysis results in Table 3 provide some insight into how significant coping styles are while adjusting for demographic and other psychosocial factors. In the models presented, 1 or more coping styles explained a significant amount of the differences in self-care or well-being outcomes. Coping styles were independent predictors of only 3 outcomes—dietary behavior, and mental well-being (general and diabetes related). Coping styles did not, however, independently explain physical activity behaviors, stages of dietary behavior change, or physical functioning. For dietary behaviors expressed as the number of days following a diet for diabetes, 26% of the variance was explained by the model, and independent predictors included active coping, dietary self-efficacy, and BMI. More frequent use of active coping styles, higher dietary self-efficacy, and lower BMI were predictive of following a diet for diabetes most days of the week.
Table 3.
Multiple Linear Regression Analysis for Behavioral and Psychological Outcomes
| Variable | Coefficient (β) | Standard Error | 95% Confidence Interval | t Value | P |
|---|---|---|---|---|---|
| Behavioral outcome: Number of days following diet for diabetes (R 2 = 0.26; n = 152; df = 12; F = 4.17, P <.0001) | |||||
| Intercept | 2.06 | 1.00 | 0.09 to 4.03 | 2.06 | .04 |
| Secondary appraisals | |||||
| Dietary self-efficacy | 0.44 | 0.14 | 0.16 to 0.73 | 3.06 | .00 |
| Negative dietary competence | −0.16 | 0.13 | −0.42 to 0.11 | −1.18 | .24 |
| Negative diabetes control | 0.10 | 0.12 | −0.15 to 0.35 | 0.78 | .44 |
| Coping style | |||||
| Emotive | −0.07 | 0.14 | −0.33 to 0.20 | −0.40 | .60 |
| Passive | −0.06 | 0.13 | −0.32 to 0.20 | −0.45 | .65 |
| Active | 0.43 | 0.13 | 0.17 to 0.70 | 3.31 | .00 |
| Covariates | |||||
| Body mass index (BMI) | −0.02 | 0.01 | −0.04 to −0.00 | −2.36 | .00 |
| Gender | −0.10 | 0.16 | −0.42 to 0.22 | −0.59 | .55 |
| Number of years at church | −0.14 | 0.15 | −0.44 to 0.16 | −0.91 | .36 |
| Number of services attended per month | −0.15 | 0.19 | −0.54 to 0.23 | −0.80 | .42 |
| Employment status | −0.25 | 0.16 | −0.57 to 0.06 | −1.58 | .12 |
| Perceived Stress Scale (PSS) | −0.17 | 0.15 | −0.47 to 0.14 | −1.09 | .28 |
| Psychological outcomes (R2 = 0.41; n = 151; df = 12; F = 8.05, P <.0001) | |||||
| 1. Mental well-being (general health) | |||||
| Intercept <.0001 | 66.27 | 8.13 | 50.19 to 82.34 | 8.15 | |
| Secondary appraisals | |||||
| Dietary self-efficacy | −0.15 | 1.18 | −2.49 to 2.19 | −0.13 | .90 |
| Negative dietary competence | 0.63 | 1.10 | −1.55 to 2.80 | 0.57 | .57 |
| Negative diabetes control | −0.82 | 1.02 | −2.85 to 1.20 | −0.81 | .42 |
| Coping style | |||||
| Emotive | −3.60 | 1.12 | −5.81 to −1.39 | −3.22 | .00 |
| Passive | −0.20 | 1.07 | −2.33 to 1.92 | −0.19 | .85 |
| Active | 0.00 | 1.07 | −2.11 to 2.11 | 0.00 | .99 |
| Covariates | |||||
| BMI | 0.09 | 0.08 | −0.06 to 0.26 | 1.17 | .24 |
| Gender | 1.20 | 1.33 | −1.43 to 3.83 | 0.90 | .37 |
| Number of years at church | −1.58 | 1.26 | −4.07 to 0.92 | −1.25 | .21 |
| Number of services attended per month | 3.53 | 1.57 | 0.42 to 6.64 | 2.24 | .03 |
| Employment status | 2.04 | 1.30 | −0.54 to 4.61 | 1.31 | .19 |
| PSS | −5.32 | 1.25 | −7.78 to −2.82 | −4.23 | <.0001 |
| 2. Diabetes mental well-being (R2 = 0.47; n = 152; df = 12; F= 10.09, P < .0001) | |||||
| Intercept | 4.97 | 0.62 | 3.74 to 6.21 | 7.97 | <.0001 |
| Secondary appraisals | |||||
| Dietary self-efficacy | −0.01 | 0.09 | −0.19 to 0.17 | −0.14 | .89 |
| Negative dietary competence | −0.01 | 0.08 | −0.18 to 0.15 | −0.15 | .88 |
| Negative diabetes control | −0.41 | 0.08 | −0.57 to −0.26 | −5.27 | <.0001 |
| Coping style | |||||
| Emotive | −0.01 | 0.09 | −0.18 to 0.16 | −0.12 | .90 |
| Passive | −0.08 | 0.08 | −0.25 to 0.08 | −0.98 | .33 |
| Active | −0.20 | 0.08 | −0.37 to −0.04 | −2.48 | .01 |
| Covariates | |||||
| BMI | 0.01 | 0.01 | −0.01 to 0.02 | 0.97 | .33 |
| Gender | 0.20 | 0.10 | −0.00 to 0.40 | 1.97 | .05 |
| Number of years at church | −0.18 | 0.10 | −0.37 to 0.01 | −1.87 | .06 |
| Number of services attended per month | 0.27 | 0.12 | 0.03 to 0.51 | 2.24 | .03 |
| Employment status | 0.08 | 0.10 | −0.12 to 0.28 | 0.80 | .43 |
| PSS | −0.34 | 0.10 | −0.53 to −0.15 | −3.51 | .00 |
In a model explaining 47% of the variance in diabetes mental well-being, active coping along with perceived stress, church involvement as measured by monthly church services attendance, and negative perceptions of diabetes control emerged as independent predictors. These findings suggest that more positive outcomes for diabetes-related mental well-being are explained by less frequent use of active coping styles, more positive appraisals of diabetes control, and greater church involvement. For general mental well-being, emotive coping emerged as an independent predictor along with church involvement, in a model explaining 41% of the variance. More positive general mental well-being was independently explained by less frequent use of emotive coping and more frequent church involvement. In both models for mental well-being, perceived stress was also an independent predictor, with lower levels associated with better mental well-being. It should be noted that passive coping styles did not uniquely explain any of the variance in either behavioral or psychosocial outcomes.
Discussion
This research investigated how coping styles relate to diabetes appraisals and outcomes of self-care and well-being. The influence of spiritual beliefs and church involvement on these outcomes was also explored. In this sample of African Americans with type 2 diabetes, negative appraisals of being able to control diabetes and efficacy in self-care were associated with emotive styles of coping, whereas both passive and active coping styles suggested more positive appraisals. In explaining self-care behaviors, only an active coping style was shown to positively influence dietary behaviors while controlling for other influences. For outcomes of both general and diabetes-specific well-being, less frequent use of active and emotive coping styles was associated with more positive outcomes. These findings suggest that different coping strategies are used in adapting to different dimensions of living with diabetes, with more active forms having a more positive influence on self-care behaviors and less active styles being beneficial to psychological outcomes. Moreover, the findings suggest a positive role for church involvement in the psychological adaptation to living with diabetes and general well-being among African Americans.
In reviewing the findings relative to the transactional model and the research questions, several important points should be made. First, in the transactional model, coping styles can have a direct effect on outcomes of stressful events, as well as a moderating effect on outcomes through appraisals of the stressors. The research findings in this study support the direct effect of coping styles on outcomes, and for the diabetes-related mental well-being outcome, there is some evidence for a moderating effect of emotive coping styles through appraisals of diabetes control. Second, active styles of coping seem to have different effects on self-care and psychological outcomes. The positive effect on dietary self-management behaviors would be expected given the positive associations between active forms of coping and better diabetes outcomes shown in other diabetes research,2,3,30 but the negative association with diabetes mental well-being was unexpected and requires further scrutiny. At least 1 study3 has shown that older persons with type 2 diabetes who have low educational attainment seldom use active forms of coping. Similarly, in this study’s sample of older African Americans, active styles of coping were less frequently used. The observed negative association of active coping and diabetes mental well-being may be related to the early stages of addressing a new diabetes-related stressor.
Third, although coping styles were associated with secondary appraisals of diabetes control, competence, and efficacy, there were no direct associations between coping styles and measures of physical status or metabolic control. Although no direct relationship was found between coping styles and metabolic control, the data from this study, like that of others,31 support the relationship between appraisals of control and A1c. Similar to the findings of Macrodimitris and Endler,31 this study found a significant association between perceived behavioral control of diabetes (a secondary appraisal) and A1c levels (r = 0.20, P < .01 for negative perceptions of diabetes control). Fourth, this research provides some evidence for the psychological benefits of church involvement to mental well-being, which is in line with what the transactional model asserts.
What appears consistent in this research and other studies on coping with diabetes is that emotive forms of coping are associated with negative appraisals and outcomes,4,8,31,32 and passive styles of coping are most often used among patients with type 2 diabetes.2–3,7–9 The positive effect of church attendance on mental well-being is also consistent with other research among African Americans15 and the general population.33–36 It appears that no other research among African Americans with diabetes has investigated the relationship between church involvement and well-being outcomes. Unlike other research among African Americans with diabetes,8,9 this study did not find any gender differences in types of coping styles; both of these studies, however, had very small samples (N < 43) and used different measures of coping.
Although important to understanding how African Americans cope with the stresses of diabetes, these research findings are limited in a few meaningful ways. The study population represents a convenience sample, which limits the generalizability of the data to the larger population of African Americans with diabetes. As with most of the research related to coping styles, the relationships described are generally based on cross-sectional data and measures of coping that do not necessarily reflect how a person copes with the specific health condition but instead assess general coping strategies. If you consider, however, that lifestyle behaviors such as diet, physical activity, and managing stress are not compartmentalized into what is diabetes related versus what is not, then general coping strategies should apply in a diabetes context. This research is also limited by self-reported measures of self-care behaviors. Despite these limitations, the study findings provide a meaningful starting point in formulating research questions that will inform not only future research to more fully elucidate coping processes among African Americans with diabetes but also the design of research interventions and educational strategies to improve the behavioral and psychological adaptation of African Americans living with diabetes.
Implications
This research provides information about African Americans with diabetes that may help to inform the development of strategies to promote better disease adaptation and self-management. It also fills a gap in the diabetes literature by reporting quantitative data on coping styles relative to self-care behaviors and quality-of-life outcomes from a larger sample of African Americans than other reports in the literature to date. Some potential implications of this research include (1) the need for additional research to identify strategies for increasing the use of more active forms of coping among patients with type 2 diabetes, particularly in the context of self-care behaviors, and (2) the potential for improving the adjustment to living with diabetes through better self-management by emphasizing behavioral strategies to address the negative effects of emotive coping. Diabetes interventions that include problem-solving or cognitive-behavioral therapies have been shown to improve quality of life (more so than educational interventions),37 and more recently, the American Association of Diabetes Educators has added “healthy coping” to its list of 7 key self-care behaviors in diabetes management.38 In the case of older African Americans living with diabetes, these research findings also suggest a role for spiritual beliefs in promoting healthy coping as a diabetes management outcome.
Acknowledgments
This study was supported by cooperative agreement number U48/CCU409660 with the Centers for Disease Control and Prevention (CDC), Special Interest Project #22PR-99. The authors are indebted to the church leadership and congregants of the 24 North Carolina churches whose involvement made this study possible.
References
- 1.American Diabetes Association. [Accessed December 28, 2006];African American and Diabetes Facts. Available at: http://www.diabetes.org/communityprograms-and-localevents/africanamerican/facts.jsp.
- 2.Coelho R, Amorim I, Prata J. Coping styles and quality of life in patients with non-insulin-dependent diabetes mellitus. Psychosomatics. 2003;44:312–318. doi: 10.1176/appi.psy.44.4.312. [DOI] [PubMed] [Google Scholar]
- 3.Karlsen B, Idsoe T, Dirdal I, Rokne Hanestad B, Bru E. Effects of a group-based counselling programme on diabetes-related stress, coping, psychological well-being and metabolic control in adults with type 1 or type 2 diabetes. Patient Educ Couns. 2004;53:299–308. doi: 10.1016/j.pec.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 4.Sanden-Eriksson B. Coping with type-2 diabetes: the role of sense of coherence compared with active management. J Adv Nurs. 2000;31:1393–1397. doi: 10.1046/j.1365-2648.2000.01410.x. [DOI] [PubMed] [Google Scholar]
- 5.Trief PM, Himes CL, Orendorff R, Weinstock RS. The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care. 2001;24:1384–1389. doi: 10.2337/diacare.24.8.1384. [DOI] [PubMed] [Google Scholar]
- 6.Willoughby DF, Kee C, Demi A. Women’s psychosocial adjustment to diabetes. J Adv Nurs. 2000;32:1422–1430. doi: 10.1046/j.1365-2648.2000.01620.x. [DOI] [PubMed] [Google Scholar]
- 7.Degazon CE. Coping, diabetes, and the older African-American. Nurs Outlook. 1995;43:254–259. doi: 10.1016/s0029-6554(95)80090-5. [DOI] [PubMed] [Google Scholar]
- 8.DeCoster VA, Cummings S. Coping with type 2 diabetes: do race and gender matter? Soc Work Health Care. 2004;40:37–53. doi: 10.1300/j010v40n02_03. [DOI] [PubMed] [Google Scholar]
- 9.Moody-Ayers SY, Stewart AL, Covinsky KE, Inouye SK. Prevalence and correlates of perceived societal racism in older African-American adults with type 2 diabetes mellitus. J Am Geriatr Soc. 2005;53:2202–2208. doi: 10.1111/j.1532-5415.2005.00501.x. [DOI] [PubMed] [Google Scholar]
- 10.Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23:928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 11.Knight BG, Silverstein M, McCallum TJ, Fox LS. A sociocultural stress and coping model for mental health outcomes among African American caregivers in Southern California. J Gerontol B Psychol Sci Soc Sci. 2000;55:142–150. doi: 10.1093/geronb/55.3.p142. [DOI] [PubMed] [Google Scholar]
- 12.Anderson RM, Funnell MM, Arnold MS, Barr PA, Edwards GJ, Fitzgerald JT. Assessing the cultural relevance of an education program for urban African Americans with diabetes. Diabetes Educ. 2000;26:280–289. doi: 10.1177/014572170002600208. [DOI] [PubMed] [Google Scholar]
- 13.Chin MH, Polonsky TS, Thomas VD, Nerney MP. Developing a conceptual framework for understanding illness and attitudes in older, urban African Americans with diabetes. Diabetes Educ. 2000;26:439–449. doi: 10.1177/014572170002600311. [DOI] [PubMed] [Google Scholar]
- 14.Daly A, Jennings J, Beckett JO, Leashore BR. Effective coping strategies of African Americans. Soc Work. 1995;40:240–249. [Google Scholar]
- 15.Brown DR, Gary LE. Religious involvement and health status among African-American males. J Natl Med Assoc. 1994;86:825–831. [PMC free article] [PubMed] [Google Scholar]
- 16.Holt CL, McClure SM. Perceptions of the religion-health connection among African American church members. Qual Health Res. 2006;16:268–281. doi: 10.1177/1049732305275634. [DOI] [PubMed] [Google Scholar]
- 17.Wenzel L, Glanz K, Lerman C. Stress, Coping, and Health Behavior. 3. San Francisco: Jossey-Bass; 2002. [Google Scholar]
- 18.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- 19.Jalowiec A, Murphy SP, Powers MJ. Psychometric assessment of the Jalowiec Coping Scale. Nurs Res. 1984;33:157–161. [PubMed] [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 21.Elasy TA, Samuel-Hodge CD, DeVellis RF, Skelly AH, Ammerman AS, Keyserling TC. Development of a health status measure for older African-American women with type 2 diabetes. Diabetes Care. 2000;23:325–329. doi: 10.2337/diacare.23.3.325. [DOI] [PubMed] [Google Scholar]
- 22.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Samuel-Hodge CD, DeVellis RF, Ammerman A, Keyserling TC, Elasy TA. Reliability and validity of a measure of perceived diabetes and dietary competence in African American women with type 2 diabetes. Diabetes Educ. 2002;28:979–988. doi: 10.1177/014572170202800612. [DOI] [PubMed] [Google Scholar]
- 24.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 25.Ammerman A, Washington C, Jackson B, et al. The PRAISE! project: a church-based nutrition intervention designed for cultural appropriateness, sustainability, and diffusion. Health Promot Pract. 2002;3:286–301. [Google Scholar]
- 26.Reed GR, Velicer WF, Prochaska JO, Rossi JS, Marcus BH. What makes a good staging algorithm: examples from regular exercise. Am J Health Promot. 1997;12:57–66. doi: 10.4278/0890-1171-12.1.57. [DOI] [PubMed] [Google Scholar]
- 27.Michigan Diabetes Research and Training Center. [Accessed December 28, 2006];Survey Instruments. Available at: http://www.med.umich.edu/mdrtc/survey/index.html.
- 28.Curry SJ, Kristal AR, Bowen DJ. An application of the stage model of behavior change to dietary fat reduction. Health Educ Res. 1992;7:97–105. doi: 10.1093/her/7.1.97. [DOI] [PubMed] [Google Scholar]
- 29.Hargreaves MK, Schlundt DG, Buchowski MS, Hardy RE, Rossi SR, Rossi JS. Stages of change and the intake of dietary fat in African-American women: improving stage assignment using the Eating Styles Questionnaire. J Am Diet Assoc. 1999;99:1392–1399. doi: 10.1016/S0002-8223(99)00338-7. [DOI] [PubMed] [Google Scholar]
- 30.Hartemann-Heurtier A, Sultan S, Sachon C, Bosquet F, Grimaldi A. How type 1 diabetic patients with good or poor glycemic control cope with diabetes-related stress. Diabetes Metab. 2001;27:553–559. [PubMed] [Google Scholar]
- 31.Macrodimitris SD, Endler NS. Coping, control, and adjustment in type 2 diabetes. Health Psychol. 2001;20:208–216. [PubMed] [Google Scholar]
- 32.Peyrot M, McMurry JF, Jr, Kruger DF. A biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherence. J Health Soc Behav. 1999;40:141–158. [PubMed] [Google Scholar]
- 33.Ellison CG, Boardman JD, Williams DR, Jackson JS. Religious involvement, stress, and mental health: findings from the 1995 Detroit Area Study. Social Forces. 2001;80:215–249. [Google Scholar]
- 34.Harris RC, Dew MA, Lee A, et al. The role of religion in heart-transplant recipients’ long-term health and well-being. J Relig Health. 1995;34:17–32. doi: 10.1007/BF02248635. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell J, Weatherly D. Beyond church attendance: religiosity and mental health among rural older adults. J Cross Cult Gerontol. 2000;15:37–54. doi: 10.1023/a:1006752307461. [DOI] [PubMed] [Google Scholar]
- 36.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87:957–961. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Steed L, Cooke D, Newman S. A systematic review of psychosocial outcomes following education, self-management and psychological interventions in diabetes mellitus. Patient Educ Couns. 2003;51:5–15. doi: 10.1016/s0738-3991(02)00213-6. [DOI] [PubMed] [Google Scholar]
- 38.Mulcahy K, Maryniuk M, Peeples M, et al. Diabetes self-management education core outcomes measures. Diabetes Educ. 2003;29:768–803. doi: 10.1177/014572170302900509. [DOI] [PubMed] [Google Scholar]