Abstract
Objective
To examine the effect of capitated transportation brokerage services on Medicaid beneficiaries’ access to care and expenditures.
Data Sources/Study Setting
The study period from 1996 to 1999 corresponds to the period of a natural experiment during which Georgia and Kentucky implemented transportation brokerage services. Effects were estimated for asthmatic children and diabetic adults.
Study Design
We used difference-in-differences models to assess the effects of transportation brokerage services on access to care, measured by Medicaid expenditures and health services use. The study design is strengthened by the staggered implementation dates between states and within each state.
Principal Findings
For asthmatic children, transportation brokerage services increased nonemergency transportation expenditures and the likelihood of using any services; reductions in monthly expenditures more than offsetting the increased transportation costs. For diabetic adults, nonemergency transportation costs decreased despite increased monthly use of health services; average monthly medical expenditures and the likelihood of hospital admission for an ambulatory care-sensitive condition (ACSC) also decreased.
Conclusions
The shift to transportation brokerage services improved access to care among Medicaid beneficiaries and decreased the expenditures. The increase in access combined with reduced hospitalizations for asthmatic children and ACSC admissions for diabetic adults are suggestive of improvements in health outcomes.
Keywords: Nonemergency medical transportation, capitated transportation payments, health care expenditures
Transportation can be a major access barrier to timely health care for low-income populations. The literature shows two distinct health effects of poor transportation: less use of preventive and primary care, and more use of the emergency department (Wilson and Jonathan 2000; Johnson and Rimsza 2004; Arcury et al. 2005). These associations are particularly significant for those people who live in rural areas, and are also found for medical care services such as prescription drugs and pediatric dental care (Saunders 1987; Mofidi, Rozier, and King 2002). The provision of and access to reliable transportation increases the likelihood of primary care physician visits in the pediatric population (Johnson and Rimsza 2004), HIV-positive adults (Messeri et al. 2002), and frequent emergency room users (Nemet and Bailey 2000; Baren et al. 2001). Overall, these studies suggest that provision of reliable transportation services is important to enable patients to have access regular and preventive care.
Transportation is a particularly important issue for Medicaid, both because Medicaid beneficiaries represent a vulnerable population and because states are concerned with controlling costs. By 2001, 10 percent of the Medicaid population (about four million beneficiaries nationwide) relied primarily on Medicaid to pay for transportation services to get to medical appointments (Rafael 2001). Nonemergency medical transportation (NEMT) services are federally mandated Medicaid services to meet the transportation needs of vulnerable populations. However, many states found that transportation costs were high under fee-for-service arrangements, in which transportation providers typically billed Medicaid based on reported trips and miles. Anecdotal reports indicate that to get higher reimbursement, some providers generated phantom trips, inflated mileage, and misclassified eligible clients. Absence of oversight further exacerbated the possibility of transportation-related fraud and abuse. Finally, inefficient and limited provision of NEMT services could potentially increase total Medicaid expenditures via delayed and expensive care.
By 2001, 21 states contracted with brokers (i.e., profit or nonprofit organizations) to manage nonemergency transportation services on a capitated basis for Medicaid beneficiaries (Rafael 2001). The goal of transportation brokerage services is to provide reliable transportation for Medicaid beneficiaries at minimum cost. Before transportation brokerage services, Medicaid funding for NEMT services was strictly cost based. Under transportation brokerage services, all nonemergency transportation services are included in capitated rates that are adjusted by beneficiaries’ health status and by geographic area (e.g., urban or rural). The brokers are responsible for negotiating payment rates with transportation providers, beneficiaries’ service eligibility verification, timely transportation reservation, and monitoring quality of services (Kulkarni 2000; Rafael 2001). The success of transportation brokerage services also depends on the expanded availability of transportation in underserved areas. Brokers therefore reach out to eligible beneficiaries by giving out public transportation schedules, providing user-friendly trip reminders, and educating beneficiaries about the available transportation options.
A review of the brief literature suggests that states that contracted with transportation brokerage services improved cost savings and quality (O’Connell et al. 2002; Dai 2005). One study using Florida data suggests that transportation brokerage services are associated with substantially decreased unit cost per trip and more accountability (Dai 2005). A study of the effect of prior-approval requirement for Medicaid transportation services in Indiana found a decrease in primary care visits and prescription refills, but did not find any measurable short-term effects on health outcomes (Tierney et al. 2000). However, the relatively short study period in the latter study to assess health outcomes—6 months each in the pre- and postperiods—and the limited study sample (from just one large hospital) may hinder the determination of the true effect of the changes in the system.
This study examines how transportation brokerage services affect beneficiaries’ access to care, expenditures, and health services use using a longitudinal panel data set over 4 years in two states. We address three research questions. First, do transportation brokerage services directly affect transportation expenditures? Second, do transportation brokerage services have spill-over effects, leading to changes in other Medicaid expenditures? Third, do transportation brokerage services lead to changes in health services use? With various types of expenditures and selected medical conditions, we assess the comprehensive effects of transportation brokerage services.
The staggered implementation of transportation brokerage services in Georgia and Kentucky provide a natural experiment. We compare how measures of access to care and health services use changed after the implementation of transportation brokerage services for two groups of patients with chronic conditions. The results provide new insights into how Medicaid beneficiaries gain access to care under a system of capitated rates for nonemergency transportation services.
METHODS
Georgia and Kentucky were chosen to study the effects of transportation brokerage services for four reasons. These states implemented transportation brokerage services at different times, allowing each state to be a control for the other. They had similar fee-for-service payments for NEMT during the preperiod. They had a similar percentage of NEMT spending to total Medicaid costs during the preperiod. Both states had similar concerns in the preperiod about overpayment by Medicaid, and about lack of coordination leading to lack of access to health care. They had the same type of NEMT payment in the postperiod. In sum, the study design is strong because these two states were similar in the preperiod, and implemented similar programs at different times.
The study period is from 1996 through 1999. Georgia implemented transportation brokerage services statewide in 1997, while Kentucky implemented gradually by county starting in 1998. The staggered implementation times across the two states allows us to estimate difference-in-differences models. This study design is therefore far stronger than a simple pre–post design, allowing for controls for time trends. To reduce the underlying heterogeneity that characterizes the full Medicaid population, we focus our analysis on two groups of beneficiaries (defined in more detail in “Data”): children with asthma and adults with diabetes.
Expenditures
Medicaid expenditures are modeled as a function of transportation brokerage services, time trends, and individual-level characteristics. Monthly individual-level expenditures are based on paid claims and represent the amount reimbursed to the provider through Medicaid. We analyze total expenditures and six additional mutually exclusive specific types of expenditures: outpatient, inpatient, pharmacy, emergency room, ambulance, and NEMT expenditures. Total expenditures are the sum of all expenditures except NEMT and ambulance transport. For ambulance expenditures, we only use Georgia claims, because the Kentucky claims do not contain ambulance expenditures. For emergency room and pharmacy expenditures, we dropped observations in Kentucky in the postperiod, because Kentucky transportation brokerage services do not provide pharmacy trips, and emergency room claims are not recorded separately from inpatient claims beginning from 1998. All expenditures were adjusted for inflation to December 1999, using the consumer price index for medical care (Bureau of Labor Statistics 2004). Time fixed effects were also included to account for any underlying time trends, not necessarily linear, that could be correlated with the transportation brokerage services implementation. Finally, we control for omitted time-invariant individual characteristics with individual fixed effects.
The main explanatory variable of interest is state implementation of transportation brokerage services. Changing to brokered transportation could affect the dependent variables in two ways: the probability of any use, and the amount of use for those who have any use. Therefore, each type of Medicaid expenditures was analyzed in a separate two-part model. The two-part model allows estimating separate effects for probability and extent of expenditures (Duan et al. 1984). An ordinary least squares (OLS) linear probability model is used to estimate the probability of any health care use in a month. Program treatment effects from a difference-in-differences study design are easier to interpret in a linear probability model than in a logit or probit model. Interaction effect in logit and probit models is more complicated to compute, but usually similar in magnitude to that in the linear probability model (Ai and Norton 2003; Norton, Wang, and Ai 2004). In the second part, an OLS model predicts logged monthly expenditures, conditional on any use, for the subset of the sample with positive expenditures. Because the continuous dependent variables are logged to reduce the influence of outliers, smearing factors are calculated to adjust for potentially nonnormal errors when transforming the results from log-dollars to dollars (Duan 1983).
Incremental effects of transportation brokerage services are estimated with the smearing factor and adjusted for heteroskedasticity (Manning 1998). To test the significance of incremental effects, we computed bootstrapped standard errors based on 200 draws (Ai and Norton 2000). Estimated incremental effects inform the two-part models that are negative and statistically significant and indicate a decrease in monthly expenditures per person.
Use of Certain Health Services
We also analyzed two specific measures of monthly health services use attributable to the selected medical conditions (asthma or diabetes). One measure is any emergency room use, and the other is ambulatory care-sensitive condition (ACSC) admissions. Emergency room use and ACSC admissions are broadly felt to represent potentially preventable health service use. We estimated linear probability models for these two measures, controlling for the same set of covariates (including individual fixed effects) as in the expenditure models.
DATA
The study sample includes all Medicaid beneficiaries under age 65 in both states. To perform individual-level analysis, both claims and eligibility files are used. The claims files include information about medical expenditures, provider characteristics, diagnosis-related group codes, and dates of service incurred. The eligibility files include beneficiaries’ demographic information and eligibility status in each month, which allows us to distinguish months of zero use from months of noneligibility. All claims of the same person in the analysis are included to estimate the changes in expenditures by type of services.
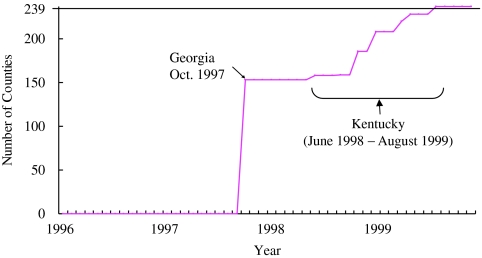
While Georgia implemented statewide transportation brokerage services in October 1997, Kentucky started a pilot program in five counties from June 1998 (Wilson et al. 2000). Georgia has 159 counties and Kentucky has 120. In Kentucky, 53 counties in 1998 and 67 counties in 1999 implemented transportation brokerage services (Hager et al. 2004). Figure 1 shows the number of counties by implementation dates. Counties with primary care case management program (PCCM) are included in the study because all medical services are reimbursed on fee-for-service basis in addition to a $3 per person per month PCCM fee. Individuals living in counties with a full-risk capitated health maintenance organization (HMO) are excluded because encounter data are not available in the Medicaid claims files. In counties with voluntary HMO enrollment, Medicaid beneficiaries are more likely to enroll if they are in good health. Out of a total of 279 counties in Georgia and Kentucky, 43 counties (15 percent) with HMOs were excluded from the study, leaving a total of 236 counties.
Figure 1.
Transportation Brokerage Services Implementation Dates by Counties
Note: There are a total of 279 counties in Georgia and Kentucky. The study sample includes 239 counties in two states, excluding counties with HMOs.
Source: CMS, Medicaid Program Statistics, Medicaid Statistical Information System
We also analyzed data for two specific populations defined by a chronic illness: children with asthma and adults with type 2 diabetes. To help ensure comparable enrollees in both the pre- and postperiods, the study samples are restricted to beneficiaries who were eligible for at least 1 month in both the pre- and postperiods. Children covered under the state children health insurance program (SCHIP) are excluded because they are not eligible for transportation brokerage services. Georgia's SCHIP program is separate from Medicaid, while Kentucky runs a combined program (Lo Sasso and Buchmueller 2004), but our analysis is restricted to Medicaid beneficiaries. Finally, we used a 40 percent random sample from each study population to minimize computational processing time for bootstrapped estimates.
The groups are identified using ICD-9 codes, National Drug Codes, and eligibility-type codes. For identifying children with asthma, eligibility requirements include children aged 0–18 years who had (1) any health care use during the study years with a diagnosis of asthma (International Classification of Diseases, Ninth Revision [ICD-9] 493.XX) and (2) prescribed asthma medication. The asthma children random sample includes 22,327 children in Georgia and 14,385 children in Kentucky. The final sample has 1,139,803 observations on 36,712 children at the person-month level. For children with asthma, the average monthly NEMT expenditures was $2, and 3 percent used NEMT services (see Table 1). The average total health care expenditure per child per month was $122, and 51 percent of the sample did not have any health care expenditures in a month. The average monthly outpatient expenditure per child is $76, and 56 percent of the observations had no outpatient expenditures in a given month. The sample is 51 percent male, 27 percent African American, and 2 percent Hispanic. Inpatient admissions with any of the ICD-9 codes for ACSC as the primary reason are considered as ACSC admissions. About 0.3 percent of the sample had an ACSC admission in a month. Emergency room use due to asthma per month was <0.1 percent.
Table 1.
Descriptive Statistics for Study Populations
|
Children with Asthma† |
Adults with Diabetes‡ |
|||
|---|---|---|---|---|
| Variables | Mean | (SD) | Mean | (SD) |
| Transportation expenditures | ||||
| NEMT expenditures | $2.01 | (43.08) | $9.68 | (79.56) |
| Pr(NEMT expenditures>0) | .03 | (.16) | .06 | (.23) |
| NEMT expenditures, if positive | $78.98 | (258.55) | $165.49 | (287.04) |
| Ambulance expenditures | $0.58 | (32.14) | $3.05 | (38.26) |
| Pr(ambulance expenditures>0) | .002 | (.045) | .02 | (.12) |
| Ambulance expenditures, if positive | $287.55 | (655.85) | $196.62 | (237.54) |
| Health care expenditures | ||||
| Total expenditures* | $121.78 | (687.69) | $434.03 | (1,410.42) |
| Pr(total expenditures>0) | .49 | (.49) | .65 | (.48) |
| Total expenditures, if positive | $248.14 | (965.54) | $663.49 | (1,699.63) |
| Inpatient expenditures | $23.86 | (577.84) | $131.55 | (1,144.41) |
| Pr(inpatient expenditures>0) | .01 | (.11) | .05 | (.22) |
| Inpatient expenditures, if positive | $2,051.58 | (4,754.15) | $2,673.12 | (4,451.89) |
| Emergency room expenditures | $2.21 | (56.72) | $3.45 | (28.47) |
| Pr(emergency room expenditures>0) | .04 | (.19) | .04 | (.20) |
| Emergency room expenditures, if positive | $56.72 | (47.42) | $79.52 | (112.33) |
| Outpatient expenditures | $75.82 | (608.41) | $216.84 | (1,142.09) |
| Pr(outpatient expenditures>0) | .44 | (.49) | .54 | (.49) |
| Outpatient expenditures, if positive | $174.32 | (913.19) | $404.19 | (1,534.82) |
| Prescription drug expenditures | $22.37 | (91.59) | $110.54 | (298.60) |
| Pr(prescription drug expenditures>0) | .24 | (.43) | .50 | (.49) |
| Prescription drug expenditures, if positive | $91.59 | (257.40) | $222.94 | (393.41) |
| Health services use | ||||
| ACSC admissions | .003 | (.053) | .005 | (.068) |
| Emergency room use due to diabetes | .0007 | (.027) | .002 | (.039) |
| Individual characteristics | ||||
| Age (years) | 5.48 | (4.48) | 46.92 | (11.84) |
| Male | .51 | (.49) | .38 | (.48) |
| Black | .27 | (.44) | .35 | (.48) |
| Hispanic | .02 | (.14) | .01 | (.08) |
Children with asthma: the total of 1,139,803 observations at the person month level on 36,712 unique children.
Adults with diabetes: the total of 687,858 observations at the person month level on 18,336 unique adults.
Total expenditures are sum of monthly Medicaid expenditures per person, excluding transportation expenditures.
Eligibility criteria for diabetic adults include person aged 19–64 years who had (1) any health care use during the study years with a diagnosis of type 2 diabetes (ICD-9 codes 250.XX) and (2) prescribed diabetes medication. The adult random sample includes 12,884 adults with type 2 diabetes in Georgia and 5,452 adults in Kentucky. The final study sample has 687,858 observations on 18,336 adults at the person-month level. About 13 percent (=2,319 adults) are disabled dually eligible persons, and about 4.5 percent (=828 adults) used a nursing home during the study period. Adults with diabetes showed higher monthly expenditures and worse health status than children. The average monthly NEMT expenditures was $10, and 6 percent of monthly observations used NEMT services (see Table 1). The average total health care expenditures per person per month was $434, although 35 percent of monthly observations did not have any Medicaid health care expenditures. The monthly average outpatient expenditure is $217, and 46 percent of the sample did not have any outpatient expenditures in a given month. The average age is 47, and the study sample is 38 percent male, 35 percent African American, and 1 percent Hispanic. Monthly ACSC admissions and emergency room use due to diabetes were 0.5 and 0.2 percent, respectively.
RESULTS
Direct Effects on Transportation Expenditures
We first examined the direct effects of transportation brokerage services on NEMT and ambulance expenditures. NEMT expenditures decreased among adults with diabetes, but increased among children with asthma (see Table 2). Before transportation brokerage services, adults with diabetes might have overused these services, while children with asthma might have underused them.
Table 2.
Results for Monthly Medicaid Expenditures and Health Services Use
|
Children with Asthma† |
Adults with Diabetes ‡ |
|||||
|---|---|---|---|---|---|---|
| Likelihood of Use (Percentage Point) | Level of Use Conditional on Some Use (ln($)) | Incremental Effect ($) | Likelihood of Use (Percentage Point) | Level of Use Conditional on Some Use (ln($)) | Incremental Effect ($) | |
| Directs effects | ||||||
| NEMT | .05551*** | −2.022*** | 9.71*** | −.0365*** | −.711*** | −11.74*** |
| (.00068) | (.032) | (1.15) | (.0012) | (.029) | (1.14) | |
| Ambulance | −.00196*** | −.25 | −.73 | −.0022 | −.21** | −1.15 |
| (.00064) | (.27) | (4.41) | (.0014) | (.11) | (6.69) | |
| Spill-over effects | ||||||
| Total | .0486*** | −.2098*** | −17.80*** | .0108*** | −.0731*** | −17.79*** |
| (.0019) | (.0080) | (1.24) | (.0019) | (.0078) | (2.47) | |
| Inpatient | −.00479*** | −.09 | −3.78** | .0019 | −.152*** | −8.86 |
| (.00048) | (.12) | (1.77) | (.0012) | (.048) | (24.94) | |
| Emergency room | −.0027 | −.029 | −.20 | −.0016 | .044 | .03 |
| (.0017) | (.037) | (.43) | (.0019) | (.043) | (.56) | |
| Outpatient | .0504*** | −.2194*** | −16.41*** | .0477*** | −.159*** | −8.62*** |
| (.0019) | (.0098) | (3.03) | (.0023) | (.013) | (3.39) | |
| Prescription drug | −.0019 | −.014 | −.35 | .0076** | −.016 | −.08 |
| (.0034) | (.019) | (.69) | (.0033) | (.012) | (2.23) | |
| Health services use | ||||||
| CSC admissions | .00035 | −.00107** | ||||
| (.00021) | (.00033) | |||||
| ER use due to asthma | −.00038 | −.00058 | ||||
| (children) or diabetes (adults) | (.00020) | (.00033) | ||||
Significant at .001.
Significant at .05.
Children with asthma: For total, inpatient, and outpatient expenditures, the total number of observation is 1,139,803 at the person month level on 36,712 unique persons. For prescription drug and emergency room expenditures the total number of observation is 634,434 at the person month level on 22,327 observations. Incremental effects of expenditure variables are in dollar amount and calculated based on the sample of 800,000 observations.
Adults with diabetes: For total, inpatient, and outpatient expenditures, the total number of observation is 687,858 at the person month level on 18,336 unique persons. For prescription drug and emergency room expenditures, the total number of observation is 477,002 at the person month level on 12,884 observations. Incremental effects of expenditure variables are in dollar amount and calculated based on the sample of 480,000 observations.
All models control for person fixed effects, year fixed effects, and month dummy variables.
For children with asthma, the probability of any transportation use increased by 5.6 percentage points (from a mean of 2 percent in the preperiod), but expenditures per month (conditional on any transportation use) fell by 87 percent (.867=1−exp(−2.022)) (see Table 2). Combining the two models, the full incremental effect of transportation brokerage services is an increase in monthly per person expenditures of about $10 compared with the mean expenditures of $3 in the preperiod (in 1999 dollars). On the other hand, for adults with diabetes, the full incremental effect is a decrease in monthly NEMT expenditures per person of about $12 compared with mean expenditures of $13 in the preperiod (see Table 2). The probability of any use decreased by 3.7 percentage points (from a mean of 7.5 percent in the preperiod), and monthly expenditures (conditional on any transportation use) also fell by 51 percent. All coefficients are highly statistically significant.
Using only Georgia data, the results show that transportation brokerage services decreased ambulance use. The probability of any ambulance use in a month among children with asthma decreased by 0.2 percentage points (from a mean of 0.3 percent in the preperiod). The decreased probability of ambulance use among adults with diabetes was not statistically significant, but expenditures per month decreased by 19 percent. The incremental effects for all study samples are minimal decreases, which suggest that the effect of transportation brokerage services on ambulance expenditures was not significant.
Spill-Over Effects on Medical Services
The spill-over effects of transportation brokerage services are assessed for seven types of Medicaid services for the two study samples. Transportation brokerage services have significant effects on the likelihood of any health care use and Medicaid expenditures. Results from the two-part models on the five selected expenditures and from the linear probability models on the two health services use are listed in Table 2.
For children with asthma, monthly expenditures per person (conditional on any use) of total, inpatient, and outpatient services decreased significantly. The probability of any health care use in a month increased by 5 percentage points after the implementation of transportation brokerage services, while total expenditures per month (conditional on any health care use) fell by around 19 percent (−.189=1−exp(−.2098)). Mean monthly expenditures per person fell by $18 (compared with the mean expenditure of $135 in the preperiod).
Results support that transportation brokerage services decrease the use of and expenditures for inpatient services. The probability of any inpatient care decreased by 0.5 percentage points (from a mean of 1.2 percent), which translates into a 36 percent decrease. The incremental effect of a decrease in monthly inpatient expenditures of $4 per person is statistically significant. The incremental effects on the use and expenditures of emergency room are not statistically significant and minimal in magnitude.
The probability of any outpatient care is increased by 5 percentage points, while outpatient monthly expenditures per person (conditional on any outpatient care use) decreased by around 20 percent. The full incremental effect is a decrease in outpatient monthly expenditures of $16 per person (compared with the mean expenditure of $83). All coefficients are highly statistically significant. The effects on the use of and expenditures for prescription drug are minimal and not statistically significant.
Transportation brokerage services did not have significant effects on the use of certain health services among children with asthma. The probability of an ACSC admission in a month increased by 0.03 percentage points, from a mean of 0.27 percent. The probability of any emergency room use due to asthma decreased by 0.03 percentage points, from a mean of 0.09 percent. Neither coefficient was statistically significant.
For adults with diabetes, transportation brokerage services have positive effects on the likelihood of any health care use in a month. All types of monthly expenditures per person (conditional on any use) decreased, while the probability of using health care services, which include outpatient and prescription drug services increased. The probability of any health care use in a month increased by 1.1 percentage points after the implementation of transportation brokerage services, while expenditures per month (conditional on any health care use) fell by around 7 percent. The incremental effect is a decrease in monthly per person expenditures of about $18 (compared with the mean expenditure of $412 in the preperiod). All coefficients are highly statistically significant. As with the result for children with asthma, the decreased expenditures per month conditional on any use seem to outweigh the increased probability of using health care services.
After the implementation of transportation brokerage services, the use of outpatient services and prescription drugs by diabetic adults increased. All coefficients are highly statistically significant, except for monthly drug expenditures among people with some expenditures in a month. The probability of any outpatient care use increased by 4.8 percentage points, and monthly outpatient expenditures per person fell by 15 percent. The incremental effect is a decrease in monthly expenditures per person of about $9 (compared with the mean expenditure of $187). The probability of any prescription drug use increased by 0.8 percentage points, while monthly prescription drug expenditures per person decreased by 2 percent. Only the coefficient of probability is statistically significant.
The results do not strongly support that the shift to transportation brokerage services decrease the use of inpatient and emergency room among adults with diabetes. The probability of any inpatient care use increased by 0.2 percentage points (from mean of 5 percent), while expenditures per month decreased by around 14 percent. The incremental effect is a decrease in monthly inpatient expenditures per person of about $9 but not statistically significant. The decrease in the probability of emergency room use is small and not statistically significant.
Transportation brokerage services decreased the use of certain health services use among adults with diabetes. The probability of having an ACSC admission in a month decreased by 0.1 percentage points, from a mean of 0.5 percent, which represents a 22 percent decrease in monthly ACSC admissions. The probability of any emergency room use due to diabetes decreased by 0.06 percentage points, from a mean of 0.19 percent. The statistically significant coefficient of ACSC admissions suggests a higher likelihood of preventable health services use among adults with diabetes.
CONCLUSION
Expenditures
The shift to transportation brokerage services has significant effects on Medicaid beneficiaries’ access to care, as measured by different types of Medicaid expenditures and certain health services use. This study also finds different effects of transportation brokerage services for two different medical conditions. Monthly NEMT expenditures per person among adults with diabetes decreased. Either the cost per trip fell, or fewer trips occurred, or both. Anecdotal evidence that the cost per trip under capitated reimbursement was often much lower than under fee-for-service, due to greater efficiency and lower fraud and abuse, is consistent with Dai's (2005) findings in Florida. Capitated reimbursement could also provide incentives to withhold necessary transportation services, which could lead to decreased likelihood of use of medical services. However, if this explanation is true, then the access to care should decrease (i.e., decreased likelihood of using medical services among those who used less NEMT services); instead, the results show that the likelihood of using any service increased, thereby supporting the first explanation.
In contrast, the results for children with asthma show an increase in the monthly per person NEMT expenditure. Transportation brokerage services increased access to NEMT services for children with asthma; therefore, the increased use of NEMT services outweighed the decreased cost per trip. We do not have an explanation for why the results differ for children with asthma compared with adults with diabetes. Given the different type of illness and different decision maker (parent for a child compared with self for an adult), we would not necessarily expect the same effect for all subpopulations.
Health Service Use
Different spill-over effects of transportation brokerage services are found for health service use by medical conditions. For both study populations, the increased use of any health care services accompanied with decreased expenditures conditional on any use led to a decrease in total expenditures by $18 per person per month. Compared with average monthly total health care expenditures by study populations, these results imply a 13 percent decrease in total health care expenditures for children with asthma and 4 percent decrease for adults with diabetes.
Contrary to the findings by Tierney et al. (2000), the probability of using outpatient services under transportation brokerage services increased in both study populations. The effect on the use of inpatient services was negative and significant only among children with asthma, which suggests that the predicted substitution of outpatient services for inpatient services is supported among children with asthma. The effect on the use of inpatient services among adults with diabetes was positive but not significant, possibly because the adult study sample includes nonelderly disabled dually eligibles (13 percent) and nursing home users (4.5 percent).
The effects on certain health services use—monthly ACSC admissions and emergency room use due to asthma for children or diabetes for adults—only showed reductions from transportation brokerage services for monthly ACSC admissions for adults with diabetes. The findings of more use of outpatient services and decreased monthly ACSC admissions suggest that transportation brokers are not denying necessary services and that the access to appropriate health services among adults with diabetes improved. Effects on ACSC admissions or emergency room use for children with asthma, however, were statistically insignificant.
Limitations
The study has several limitations. First, the study used data from two states, raising concerns about generalizability to other states and the ability to control for confounding. However, the staggered implementation of transportation brokerage services between and within states controls for general trends and therefore makes the study design stronger than a simple pre–post design. Second, the magnitude of the effect depends in part on how efficient transportation services were before transportation brokerage services. The less efficient the fee-for-service transportation was, the more room for improvement by transportation brokerage services. Third, the two medical conditions analyzed, asthma and diabetes, are important in terms of beneficiaries’ health outcomes and increasing health care costs to individuals and society. The effects could be, however, different for other medical conditions. Further research with additional medical conditions may add more knowledge on the effects of transportation brokerage services. Fourth, the analysis on ambulance transport used only Georgia data because Kentucky data did not separately record ambulance transport use. The results, based on a simple pre–post comparison, still provide an understanding of the substitution effects between NEMT services and ambulance.
Policy Implications
The policy implications of these findings are potentially important. Transportation brokerage services were implemented as a cost-containment measure. Even though nonemergency transportation costs increased for children with asthma, access improved as measured by use of any health service, and total monthly expenditures declined on average by $18 per month, more than offsetting the increase in transportation expenses. Both transportation costs and Medicaid health service costs decreased for adults with diabetes, although access as measured by use of any service increased and ACSC admissions declined. Our results—which are based on large sample sizes, a study design that controls for contemporaneous changes, and are robust to changes in model specification—highlight the importance of transportation to health services.
The increase in access combined with reduced hospitalizations for asthmatic children and ACSC admissions for diabetic adults suggests improvements in health outcomes, assuming that the staggered study design controlled for any confounding. Any policy that leads to better health outcomes with lower expenditures is unambiguously good. Many states are implementing, or plan to implement, transportation brokerage services to reduce expenditures and improve quality. Because evidence from this study indicates that access to care and health outcomes are not adversely affected by the transportation brokerage services, the decrease in overall Medicaid expenditures reflects a more efficient system from an economic perspective. Care may be shifted to lower cost providers, resulting in more appropriate care and savings to Medicaid for the two important disease groups studied.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: LogistiCare and the LogistiCare Foundation provided partial funding to purchase data and to support a graduate research assistant. However, by prior agreement, neither LogistiCare nor the LogistiCare Foundation ever reviewed the article. We thank Kenneth Darter for helping us obtain Georgia Medicaid data, and Gerrie Barosso at ResDAC (CMS contract #: 500-051-0043) and Robyn Tomas at CMS for helping us obtain Kentucky Medicaid data. This research was funded by the LogistiCare Foundation and LogistiCare Inc.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Ai C, Norton E C. Standard Errors for the Retransformation Problem with Heteroscedasticity. Journal of Health Economics. 2000;19(5):697–718. doi: 10.1016/s0167-6296(00)00046-1. [DOI] [PubMed] [Google Scholar]
- Ai C, Norton E C. Interaction Terms in Logit and Probit Models. Economics Letters. 2003;80(1):123–9. [Google Scholar]
- Arcury T A, Gesler W M, Preisser J S, Sherman J, Perin J. The Effects of Geography and Spatial Behavior on Health Care Utilization among the Residents of a Rural Region. Health Services Research. 2005;40(1):135–55. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baren J M, Shofer F S, Ivey B, Reinhard S, DeGeus J, Stahmer S A, Panettieri R, Hollander J E. A Randomized, Controlled Trial of a Simple Emergency Department Intervention to Improve the Rate of Primary Care Follow-Up for Patients with Acute Asthma Exacerbations. Annals of Emergency Medicine. 2001;38(2):115–22. doi: 10.1067/mem.2001.116593. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. [accessed 2004];2004 “Consumer Price Index—All Urban Consumers” Available at http://www.bls.gov/data/
- Dai C. 2005. “The Efficiency of Organizational Forms: Evidence from Florida's Non-Emergency Medicaid Transportation Programs.” (Submitted for publication.)
- Duan N. Smearing Estimate—A Nonparametric Retransformation Method. Journal of the American Statistical Association. 1983;78(383):605–10. [Google Scholar]
- Duan N, Manning W G, Morris C N, Newhouse J P. Choosing between the Sample-Selection and Multi-Part Model. Journal of Business and Economic Statistics. 1984;2(3):283–9. [Google Scholar]
- Hager G, Hewlett T, Atchley L, Otto S. Frankfort, KY: Legislative Research Commission; 2004. Human Service Transportation Delivery: System Faces Quality, Coordination, and Utilization Challenges. Research Report No. 319. [Google Scholar]
- Johnson W G, Rimsza M E. The Effects of Access to Pediatric Care and Insurance Coverage on Emergency Department Utilization. Pediatrics. 2004;113:483–7. doi: 10.1542/peds.113.3.483. [DOI] [PubMed] [Google Scholar]
- Kulkarni M P. Fact Sheet: Medicaid Transportation Services. 2000. National Health Law Program.
- Lo Sasso A, Buchmueller T C. The Effect of the State Children's Health Insurance Program on Health Insurance Coverage. Journal of Health Economics. 2004;23(5):1059–82. doi: 10.1016/j.jhealeco.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Manning W G. The Logged Dependent Variable, Heteroscedasticity, and the Retransformation Problem. Journal of Health Economics. 1998;17(3):283–95. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- Messeri P A, Abramson D M, Aidala A, Lee F, Lee G. The Impact of Ancillary HIV Services on Engagement in Medical Care in New York City. AIDS Care. 2002;14(suppl 1):S15–29. doi: 10.1080/09540120220149948. [DOI] [PubMed] [Google Scholar]
- Mofidi M, Rozier R G, King R S. Problems with Access to Dental Care for Medicaid-Insured Children: What Caregivers Think. American Journal of Public Health. 2002;92(1):53–8. doi: 10.2105/ajph.92.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemet G F, Bailey A J. Distance and Health Care Utilization among the Rural Elderly. Social Science and Medicine. 2000;50(9):1197–208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- Norton E C, Wang H, Ai C. Computing Interaction Effects and Standard Errors in Logit and Probit Models. Stata Journal. 2004;4(2):154–67. [Google Scholar]
- O’Connell L, Grossardt T, Siria B, Marchand S, McDorman M. Efficiency through Accountability: Some Lessons from Kentucky's Improved Medicaid Transit Service. Journal of Transportation and Statistics. 2002;5(2/3):73–81. [Google Scholar]
- Rafael D. Medicaid Transportation: Assuring Access to Health Care. A Primer for States, Health Plans, Providers and Advocates. Washington, DC: Community Transportation Association of America (CTAA); 2001. [Google Scholar]
- Saunders C E. Patient Compliance in Filling Prescriptions after Discharge from the Emergency Department. American Journal of Emergency Medicine. 1987;5(4):283–6. doi: 10.1016/0735-6757(87)90351-2. [DOI] [PubMed] [Google Scholar]
- Tierney W M, Harris L E, Gaskins D L, Zhou X H, Eckert G J, Bates A S, Wolinsky F D. Restricting Medicaid Payments for Transportation: Effects on Inner-City Patients’ Health Care. American Journal of the Medical Sciences. 2000;319(5):326–33. doi: 10.1097/00000441-200005000-00010. [DOI] [PubMed] [Google Scholar]
- Wilson G, Nutt P, Atchley L, Huddleston D, Clark M, Hewlett T, Hood J. Progress Report on Coordinated Human Service Transportation System. Frankfort, KY: Legislative Research Commission, Program Review and Investigations Committee; 2000. [Google Scholar]
- Wilson K M, Jonathan D K. Adolescents Who Use the Emergency Department as Their Usual Source of Care. Archives of Pediatrics and Adolescent Medicine. 2000;154:361–5. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.