Abstract
Thyrotropin-releasing hormone (TRH) is a neuropeptide that initiates its effects in mice by interacting with two G protein-coupled receptors, TRH receptor type 1 (TRH-R1) and TRH receptor type 2 (TRH-R2). Two previous reports described the effects of deleting TRH-R1 in mice. TRH-R1 knockout mice exhibit hypothyroidism, hyperglycemia, and increased depression and anxiety-like behavior. Here we report the generation of TRH-R2 knockout mice. The phenotype of these mice was characterized using gross and histological analyses along with blood hematological assays and chemistries. Standard metabolic tests to assess glucose and insulin tolerance were performed. Behavioral testing included elevated plus maze, open field, tail suspension, forced swim and novelty-induced hypophagia tests. TRH-R2 knockout mice are euthyroid with normal basal and TRH-stimulated serum levels of thyroid-stimulating hormone (TSH, thyrotropin), are normoglycemic and exhibit normal development and growth. Female, but not male, TRH-R2 knockout mice exhibit moderately increased depression-like and reduced anxiety-like phenotypes. Because the behavioral changes in TRH-R1 knockout mice may have been caused secondarily by their hypothyroidism whereas TRH-R2 knockout mice are euthyroid, these data provide the first evidence for the involvement of the TRH/TRH-R system, specifically extrahypothalamic TRH/TRH-R2, in regulating mood and affect.
Keywords: Thyrotropin-releasing hormone, Thyrotropin-releasing hormone receptors, Depression, Anxiety, Extrahypothalamic TRH, Behavioral changes, Neurotransmitter, Neuromodulator, TRH-R2-deficient mouse
INTRODUCTION
Thyrotropin-releasing hormone (TRH) is a tripeptide agonist that initiates its effects by activating two G protein-coupled receptors, TRH receptor type 1 (TRH-R1) and TRH receptor type 2 (TRH-R2) (see (Sun et al, 2003) for review). Activation of these receptors appears to initiate a number of effects within the central nervous system. TRH receptors are expressed in the anterior pituitary and respond to hypothalamic TRH by activating the hypothalamic-pituitary-thyroid (HPT) axis and consequently regulating metabolism. TRH and its corresponding receptors are also expressed extrahypothalamically in various brain regions including the limbic system and cortex. Because of its presence outside of the HPT axis, TRH is also considered a neurotransmitter or neuromodulator (Gary et al, 2003). The function of extrahypothalamic TRH has been inferred from pharmacological studies using TRH and its analogues showing a wide array of actions including arousal, increased locomotor activity, antidepressant and anxiolytic effects (Pekary et al, 2005; Sattin, 1999; Gutierrez-Mariscal et al, 2008).
Studies have linked TRH and its receptors to psychiatric disorders. Hypothyroidism causes depression, loss of energy and weight gain and within the HPT axis, a number of subtle abnormalities have been found in individuals with major depression including blunted TSH response to TRH and absence of nocturnal TSH surge (Bartalena et al, 1990). Also, decreased TRH gene expression was observed in the hypothalamus of depressed patients (Alkemade et al, 2003). TRH and its receptors in the limbic system and cortex are believed to mediate the endogenous and exogenous effect TRH on affect, mood and arousal (Gary et al, 2003; Yarbrough et al, 2007) but it has been notoriously difficult to separate the hypothalamic and extrahypothalamic functions of TRH and to assign specific functions and behaviors to extrahypothalamic TRH.
TRH-R1 was initially cloned from a mouse pituitary tumor cDNA library (Straub et al, 1990) and then orthologous receptors were cloned from a number of different species, including rat (de la Pena et al, 1992; Zhao et al, 1992; Sellar et al, 1993), chicken (Sun et al, 1998), cow (Takata et al, 1998), Catostomus commersoni (Harder et al, 2001) and humans (Duthie et al, 1993; Matre et al, 1993). The human TRH-R1 is 90% and 89% homologous to the mouse and rat receptors at the DNA level, respectively; the three receptors exhibit approximately 95% homology at the amino acid level. TRH-R2 was identified in rat (Cao et al, 1998; Itadani et al, 1998; O’Dowd et al, 2000), mouse (Harder et al, 2001) and Catostomus commersoni (Harder et al, 2001); TRH-R2 has not been described in humans. Amino acid sequence alignments of the two types of TRH receptors from the same species reveal a 50% overall identity. TRH-R1 and TRH-R2 bind TRH with equal affinities but exhibit a different distribution of expression in rats. In particular, TRH-R1 is expressed at high levels whereas TRH-R2 is not expressed or expressed at very low levels within the anterior pituitary gland, and the distribution of their expression within the rat brain is mostly non-overlapping. Of note, TRH-R2 is expressed within the limbic system (O’Dowd et al, 2000).
Two previous reports described the generation and characterization of TRH-R1-deficient mice (Rabeler et al, 2004; Zeng et al, 2007). TRH-R1-deficient mice exhibit “tertiary hypothyroidism” with low levels of thyroid hormones, and mild hyperglycemia. Zeng et al. found that the TRH-R1-deficient mice they generated, in contrast to those generated by Rabeler et al., did not exhibit developmental abnormalities but displayed increased depression-like and increased anxiety-like behaviors. Because the mice studied by Zeng et al. were hypothyroid, it is not possible to determine whether the depression- and anxiety-like signs were caused by TRH-R1 deficiency outside of the HPT axis or the changes associated with tertiary hypothyroidism. TRH-deficient mice have been generated and characterized also (Yamada et al, 1997). Similar to TRH-R1-deficient mice, TRH-deficient mice are hypothyroid and hyperglycemic. To our knowledge, no behavioral studies of TRH-deficient mice have been reported.
Herein we report the generation and characterization of TRH-R2 knockout mice. We show that TRH-R2-deficient mice are euthyroid with normal thyroxine and normal basal and TRH-stimulated serum levels of thyroid-stimulating hormone (TSH, thyrotropin), are normoglycemic and exhibit normal development and growth. Interestingly, female, but not male, TRH-R2 knockout mice exhibit moderately increased depression-like and reduced anxiety-like phenotypes.
MATERIALS AND METHODS
Construction of targeting vector and generation of TRH-R2 knock-out mice
Genomic clones spanning the entire mouse TRH-R2 gene were isolated by screening a BAC mouse genomic library (129/SvJ, Bac Mouse I PCR library screening service, Genome Systems Inc., St. Louis, Missouri) with primers specific for the third exon (sense primer: 5’-TTTCCTGGACCCCTGGGGTCCTGCTG-3’; anti-sense primer: 5’-GGGAAGCAGCTGCTGCTGGACCTGAGAC-3’). The clones were characterized in detail by standard molecular biology techniques. A 13 kb Bgl II-Bgl II DNA fragment including the TRH-R2 gene missing the first exon and the first 130 bp of the first intron were subcloned into the BamH I site of the pBluescript SK II (-) vector (Stratagene). A 1243 bp DNA fragment including the second exon and the second intron was subcloned into the EcoR I-BamH I sites of the pLoxpneo vector (Yang et al, 1998). The resulting construct was cleaved with Hpa I and Not I followed by insertion of a 9 kb DNA fragment which is 3’ to the third exon of the TRH-R2 gene. The replacement vector finally contained 10.2 kilobases of homologous genomic DNA in which the third exon of the TRH-R2 gene was removed and replaced by a loxp-Neo-loxp cassette. The finished construct, pTRH-R2neo, is shown in Fig. 1.
Figure 1.
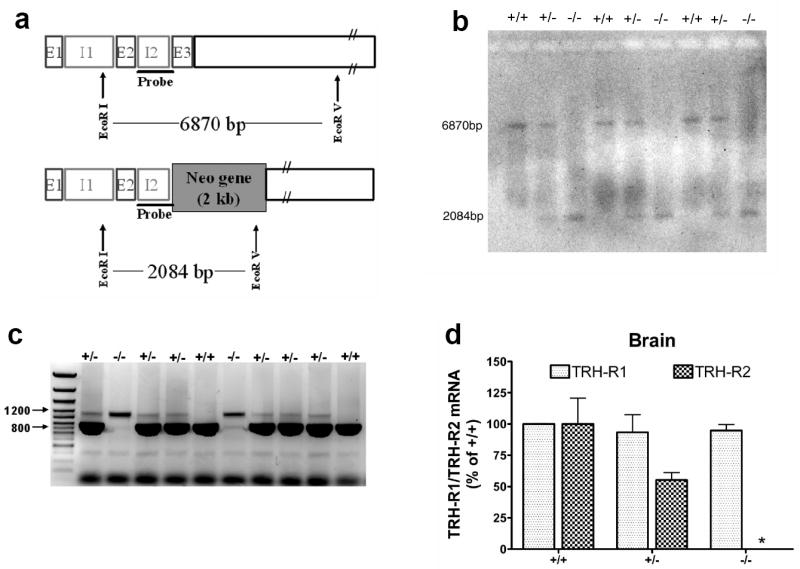
Targeting vector for TRH-R2 knockout and genotyping. Schematic representation of the targeting vector (a). E1, 2, 3 – Exon 1, 2, 3; I1, 2 – Intron 1, 2. Representative Southern blot (b) and PCR (c) analysis of wild type (+/+), heterozygous (+/-) and homozygous mice (-/-). qRT-PCR analysis of whole brain mRNA (d). The asterisk indicates that no TRH-R2 mRNA was detected in homozygous mice (-/-).
TC1 ES cells (Deng et al, 1996) were transfected with Not I-digested pTRH-R2neo and selected with G418 and 1-(2-deoxy-2-fluoro-β-D-arabinofuranosyl-5-iodouracil (FIAU). ES cell colonies that were resistant to both G418 and FIAU were analyzed by Southern blotting for homologous recombination events within the TRH-R2 locus. Genomic DNAs from these clones and the parental TC1 cell line were digested with EcoR I and EcoR V and then probed with a 5’-flanking probe specific to the TRH-R2 gene. The 5’ probe is a 416 bp Sma I-Sma I fragment. Homologous recombinant cell clones were identified by Southern blot analysis as described below. These ES cells were injected into 3.5 day old 129/Svev blastocysts that were subsequently implanted into pseudopregnant recipients. The resulting chimeras were mated with 129/Svev females and germline transmission of the mutant allele was identified by Southern blot analysis. The mutant mice were backcrossed 4 times to the 129 background.
Genotype determination
For DNA preparation, ES cells or mouse tails were incubated overnight at 55°C in extraction buffer (100 mM Tris·HCl pH 8.5, 200 mM NaCl, 5 mM EDTA, 0.2% SDS, 200 μg/ml Proteinase K) followed by 15 min at 80°C.
Southern blot
The DIG High Primer DNA Labeling and Detection Starter Kit II (Roche Molecular Biochemicals, Mannheim, Germany) was used for Southern blot assay. Briefly, DNA (10 μg) was digested with EcoRI and EcoRV, size separated on a 0.8% agarose gel, and then capillary-transferred to a nylon membrane (Hybond N, Amersham Bioscience, Braunschweig, Germany). The membranes were hybridized using a probe which was a digoxigenin-labeled 416 bp Sma I-Sma I fragment specific for a region upstream of the third exon of the TRH-R2 gene that was not included in the targeting vector. Signals were analyzed by exposing to X-ray film (Eastman Kodak Company, Rochester, NY).
PCR analysis
PCR was carried out by using the Expand Long Template PCR System (Roche Molecular Biochemicals). The primer pair generating an 800 bp product specific for the wild-type gene was: sense: 5’-GGGCAGCCTTCCTGAAACTGTGCTGGTGCCGGGCAG -3’; anti-sense: 5’-CTTGCACATTCGGGGTCAAGTGGCTTCTTGATGGAG -3’. The primer pair generating a 1200 bp product specific for the neo gene was: sense: 5’-GACGTGACAAATGGAAAGTAGCACGTCTCACTAGTC-3’; anti-sense: 5’-CAGAAGAACTCGTCAAGAAGGCGATAGAAGGCGATG-3’.
Quantitative RT-PCR
Total RNA was purified, reverse-transcribed and transcript levels of selected genes were measured by qRT-PCR. In brief, total brain RNA was purified using an RNeasy Mini Kit (Qiagen) and first strand cDNA was prepared using a High Capacity cDNA Archive Kit (Applied Biosystems). PCR was performed in 25 μl reactions in 96-well plates using cDNA prepared from 100 ng of total RNA and Universal PCR Master Mix (Applied Biosystems). Primers and probes were Assay-on-Demand (Applied Biosystems). The Ct values for TRH-R mRNAs were normalized to GAPDH and the levels measured in wild type mice (Ct = 25 for TRH-R1 and TRH-R2) were set at 100%. The levels of TRH-R2 mRNA in TRH-R2-/- mice were undetectable (Ct > 37).
Animal care
All animal protocols used in these studies were approved by the National Institute of Diabetes and Digestive and Kidney Diseases and the Weill Cornell Medical College Animal Care and Use Committees. We housed mice in microisolator cages (Labproducts) in a specific pathogen-free barrier facility with an air shower entrance.
Pathology analysis and blood chemistries
Gross and histological analyses, and blood hematological assays and chemistries were performed by the Office of Research Services/Division of Veterinary Resources, National Institutes of Health.
Metabolic testing
Analysis of growth and glucose/insulin homeostasis including glucose and insulin tolerance tests on normal and high fat diets were performed by the Mouse Metabolism Laboratory of the National Institute of Diabetes and Digestive and Kidney Diseases Intramural Research Program under the direction of Dr. Oksana Gavrilova. Glucose tolerance test: Mice were fasted for 14-16 hours. Sterile glucose (2 g/kg; dissolved in phosphate buffered saline; volume: 0.1-0.2 ml/mouse) was injected at time zero (i.p. glucose tolerance test). Blood samples (20-30 μl) were taken from the tail vein just prior to the injection (0 min), 15, 30, 60 and 120 min after the glucose injection. Blood glucose and insulin levels were determined. Insulin tolerance test: Freely fed mice were injected i.p. with human insulin (0.75 U/kg). Blood samples (20-30 μl) were taken from the tail vein just prior to the injection (0 min) and 15, 30, 60 and 120 min after the insulin injection. Blood glucose levels were measured with Glucometer Elite (Bayer Healthcare).
Thyroxine, TSH and Prolactin
Serum thyroxine was assayed by Gammacoat Total T4 Radioimmunoassay Kit (DiaSorin Inc., Stillwater, MN). Serum TSH levels were measured in blood obtained by retro-orbital sampling before (basal) and 30 min after intraperitoneal injection of TRH (5 μg/kg). TSH was measured by radioimmunoassay using highly purified rat TSH (AFP11542B) for radioiodination, guinea pig anti-TSH antibody (AFP98991) and mouse TSH reference preparation (AFP51718MP). Serum prolactin was assayed using mouse prolactin (AFP10777D) for radioiodination, rabbit anti-mouse prolactin antibody (AFP131078) and mouse prolactin reference standard (AFP6476C). TSH and prolactin measurements were performed by Dr. A.F. Parlow of the NIDDK National Hormone and Pituitary Program.
Behavioral testing
Eight to twelve weeks old TRH-R2+/+ and -/- male and female littermates were tested in elevated plus maze (EPM), open field (OF), tail suspension test (TST), forced swim test (FST) and in the novelty-induced hypophagia test (NIHT). Mice were also tested for locomotor activity (LA) and prepulse inhibition (PPI). Three cohorts were tested in the following order: Cohort 1, (i) EPM, (ii) OF, (iii) LA, (iv) PPI, (v) FST; Cohorts 2 and 3, (i) FST, (ii) TST, (iii) NIHT. EPM, OF, LA and PPI data are not reported because no differences between the groups were found. Only one procedure was conducted per day.
TST
Mice were individually suspended by the tail using adhesive tape for 6 min. The session was videotaped and immobility was scored between 2 and 6 min by a trained observer who was blind to the genotype and male and female data were analyzed separately by t-test.
FST
Mice were placed in a clear, water-filled cylinder (diameter, 8 inch; depth, 5 inch) for 6 min (Porsolt et al., 1978) and immobility time of the mice was measured between 2 and 6 min from a recorded videotape. Water temperature was equilibrated to room temperature of 21°C. Mice were tested by an observer who was blind to the genotype of the mice. The male and female data were analyzed separately by t-test.
NIHT
The test consists of 3 days of training in the home cage followed by testing in the home cage and then in a novel cage environment. Littermates were single-housed for 3 days before training began. Then, for 3 consecutive days mice were presented with sweetened condensed milk (Carnation) diluted 1 to 3 with water for 30 min each day in LM Animal Farms Quick Quench Universal Water Bottle (5 oz, Petco) essentially as described by Dulawa et al. (Dulawa et al, 2004). Home cage testing occurred on day 4 by presenting the milk for 10 min in the dark and the latency to drink and the duration of drinking were recorded (dark or home cage latency and duration). Novel cage testing was on day 5 under bright lighting conditions and by placing the mice into new clean cages of the same dimensions as the home cage but without bedding. Latency to drink and duration of drinking were again recorded (light or novel cage latency and duration). All sessions were videotaped and scored by a trained observer who was blind to the genotype of the mice. Mice were tested only once. Statistical significance in the measures of latency and duration of drinking between TRH-R2+/+ and -/- littermates was established by t-test. Males and females were analyzed separately.
RESULTS
Generation of TRH-R2-deficient mice
As depicted in Figure 1a, the targeting vector was designed to delete exon 3 of the TRH-R2 coding region. Exon 3 was replaced by the neomycin-resistance gene. Homologous recombinants of the stably transfected embryonic stem (ES) clones obtained after antibiotic selection were identified by Southern analysis. Male chimeras generated by blastula injection were bred with 129Svev females with successful germ line transmission. The heterozygous mice (TRH-R2+/-) were apparently normal and subsequently gave rise to mice homozygous (TRH-R2-/-) for the mutant TRH-R2 locus with the expected frequency, indicating that the deletion of the TRH-R2 gene did not result in embryonic lethality. The animals were genotyped by Southern blot (Fig. 1b) and by PCR (Fig. 1c) using the probe and primers described in Experimental Procedures, respectively. Quantitative RT-PCR of brain RNA showed that TRH-R1 mRNA levels were the same in wild type, heterozygous and homozygous mutants whereas heterozygous mice exhibited 55% of the level of TRH-R2 mRNA found in wild type mice and the knockout mice did not express any TRH-R2 mRNA (Fig. 1d). It is noteworthy that TRH-R2-/- mice exhibited the same level of TRH-R1 as wild type mice even though they did not express TRH-R2.
General characterization of TRH-R2-/- mice
Male and female fertility in the TRH-R2-/- mice appeared normal; litter size was not affected. There was no difference in body weight at birth irrespective of the genotype of the mothers. Wild type and TRH-R2-/-littermate mice of both genders exhibited similar growth rates on normal and high fat diets. Adult TRH-R2-/- mice exhibited no pathology different from wild type littermates. There were no differences in body weights and organ weights of adult wild type and TRH-R2-/- mice. Routine blood chemistries were within normal limits and there were no differences between wild type and TRH-R2-/- mice.
Metabolic testing
On both a normal and high fat diet, both male and female TRH-R2-/- mice exhibited normal glucose and insulin levels (Fig. 2). TRH-R2-/- mice exhibited normal glucose and insulin tolerance tests also (data not shown).
Figure 2.
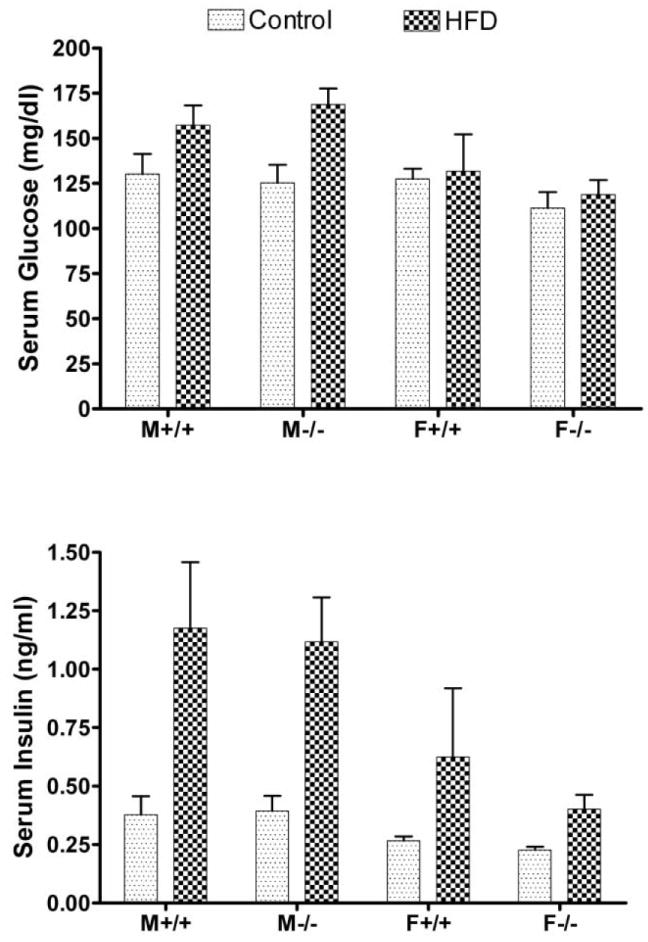
Serum glucose and insulin levels in wild type and TRH-R2-deficient mice on normal (Control) and high fat diets (HFD). TRH-R2 knockout mice exhibit normal glucose (upper panel) and insulin levels (lower panel) on Control and HFD. There was no difference in any of the values in wild type compared to TRH-R2-deficient mice.
Thyroxine, TSH and Prolactin
Serum thyroxine levels in male and female TRH-R2-/-mice were not different from controls: male wild type, 4.7±0.21; male ko, 4.0±0.20; female wild type, 2.4±0.10; and female ko, 2.60±0.33 μg/dl. Serum TSH levels were not different basally and responded to TRH with a similar increase in TSH in wild type and TRH-R2-/- mice of both genders (Fig. 3). Serum prolactin levels were not different from controls: male wild type, 8.5±2.3; male ko, 5.5±0.71; female wild type, 49±29; and female ko, 62±19 ng/ml.
Figure 3.
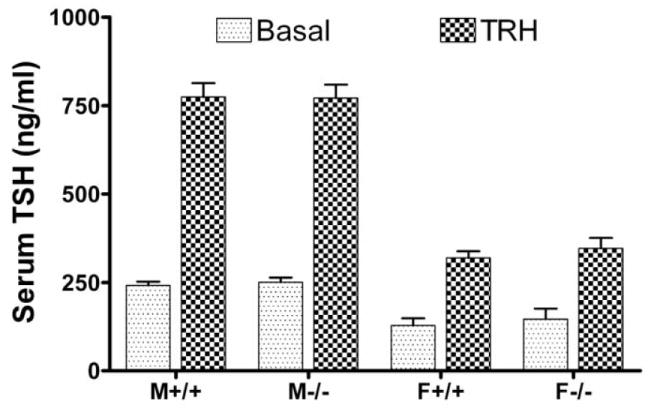
Basal and TRH-stimulated serum TSH levels in wild type and TRH-R2-deficient mice. Serum for TSH measurements were obtained just before TRH (5 μg/kg) administration i.p. (Basal) and 30 min after (TRH). There was no difference in any of the values in wild type compared to TRH-R2-deficient mice.
Behavioral testing
Since TRH has been linked to mood and anxiety disorders (Gary et al, 2003; Sattin, 1999; Gutierrez-Mariscal et al, 2008), TRH-R2-/- mice were tested in depression and anxiety-related behavioral paradigms. The tail suspension test (TST) and forced swim test (FST) are validated behavioral assays for assessing antidepressant activity. In these tests, animals are subjected to short term inescapable stress that normally elicits a rapid adaptation to immobile posture sometimes called “behavioral despair”. Immobility time is reduced by the acute administration of antidepressants and, as an extension of this finding, increased immobility time has been interpreted as depression-like behavior. Interestingly, female but not male TRH-R2-/-mice exhibited a significant increase in immobility time in TST (t-test; female: t=2.42, p=0.012, N=11 +/+ and 14 -/-; male: t=1.24, p=0.114, N=11 +/+ and 8 -/-) (Fig. 4). In FST, no significant difference was found but both male and female TRH-R2-/- mice showed a trend for increased immobility (t-test; female: t=1.62, p=0.057; male: t=1.47, p=0.076) (Fig. 4). These data suggest that female TRH-R2-/- mice have a mild depression-like behavior.
Figure 4.
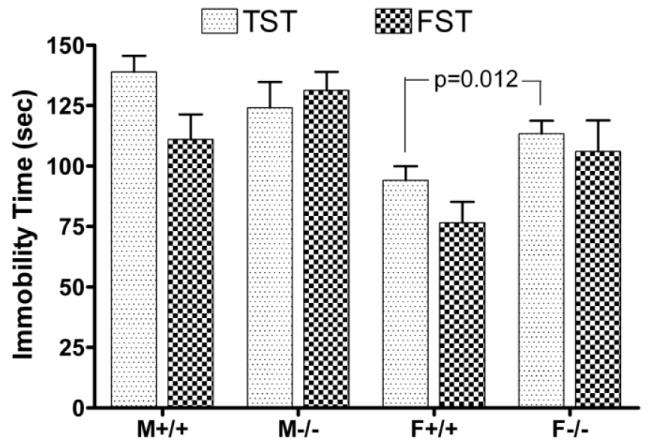
Results of tail suspension and forced swim tests in wild type and TRH-R2-deficient mice. Forced swim (FST) and tail suspension tests (TST) were performed as described in Experimental Procedures. Male and female data were analyzed separately by t-test.
A number of anxiety-related tests are available but only a few of them are validated by various classes of clinically relevant anxiolytics (including benzodiazepines and serotonin reuptake inhibitors). One of these assays is the novelty-induced hypophagia test (NIHT) (Dulawa et al, 2004). In this test, animals are provided with a familiar and highly palatable food (sweetened milk in our experiments) in a novel and brightly lit environment. In these conditions, animals are conflicted on whether to avoid or approach the food. Heightened fear and anxiety are reflected by an increase in the latency and a decrease in the duration of feeding and clinically used anxiolytics elicit opposite responses (Merali et al, 2003; Dulawa and Hen, 2005). Duration of feeding was significantly increased in female but not in male TRH-R2-/- mice (t-test; female: t=2.60, p=0.008, N=11 +/+ and 14 -/-) (Fig. 5). Consistent with a reduced anxiety level in females, the latency to eat was also reduced in female but not in male TRH-R2-/-mice but this effect was only a trend (t-test; female: t=1.47, p=0.077) (Fig. 5). In the familiar home cage environment in the dark, no difference in latency and duration was measured between TRH-R2+/+ and TRH-R2-/- littermates in either gender (data not shown) indicating that the observed novel cage effect in females was not due to a difference in motivation to feed.
Figure 5.
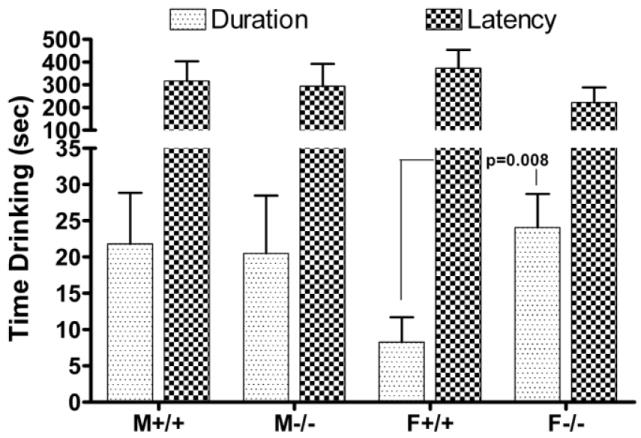
Results of the novelty-induced hypophagia test in wild type and TRH-R2-deficient mice. The novelty-induced hypophagia test (NIHT) was performed as described in Experimental Procedures; durations and latencies of drinking in novel cages were measured. Male and female data were analyzed separately by t-test.
DISCUSSION
The role of the TRH/TRH-R system in regulation the HPT axis is well known and the results of the previous studies in TRH-deficient (Yamada et al, 1997) and TRH-R1-deficient mice (Rabeler et al, 2004; Zeng et al, 2007) and the current studies in TRH-R2-deficient mice show that TRH-R1 is the physiological target of TRH in the TSH-producing cells of the anterior pituitary gland. The role of this system in regulation of glucose homeostasis is less well understood but both TRH-deficient and TRH-R1-deficient mice exhibit hyperglycemia. In contrast, TRH-R2-knockout mice exhibit normal glucose homeostasis even when given a high fat diet. Therefore, TRH regulation of glucose metabolism in rodents (Kulkarni et al, 1995; Yamada et al, 2000; Luo and Yano, 2004) is mediated by TRH-R1. Furthermore, it was suggested that the effect of TRH on glucose homeostasis is mediated, at least in part, by TRH-R1 expressed on insulin-secreting cells. It is noteworthy, therefore, that although TRH-R1 has been reported to be expressed in adult rodent islets at the mRNA and protein levels (Kulkarni et al, 1995; Luo and Yano, 2004), we have found no TRH-R mRNA in islets of Langerhans from adult humans (Mulla et al, 2008).
Besides its established neuroendocrine role in controlling TSH release, the TRH/TRH-R system has been proposed as a major regulatory system within the central nervous system including a role in the modulation of mood, arousal and circadian rhythm; functions thought to be impaired or altered in depression and anxiety (Gary et al, 2003; Yarbrough et al, 2007; Sattin, 1999; Pekary et al, 2006; Gutierrez-Mariscal et al, 2008). Here we tested if lack of TRH-R2 results in changes in depression- and anxiety-related behaviors. Both FST and TST indicated a moderate depression-like behavior in female but not male TRH-R2-/- mice. Although no animal model can reproduce the complex symptomatology of depression, it is believed that some aspects or endophenotypes of the disease can be reproduced in animals. In particular, disturbances in the monoamine system have long been implicated in depression and it is thought that FST and TST are assays to detect changes in monoaminergic activity. Indeed, depletion of serotonin increases while antidepressant-induced activation of serotonergic and/or noradrenergic neurotransmission reduces immobility time in FST and TST (Porsolt et al, 1978; Page et al, 1999; Cryan et al, 2002). We speculate that the increased immobility of TRH-R2-/- mice in the FST and TST indicates reduced serotonergic and/or adrenergic neurotransmission in these mice (Sattin et al, 2008). The depression-like behavior of TRH-R2-/- mice is also consistent with the reported antidepressant effect of TRH (Sattin, 1999) although not all studies support this effect (Gary et al, 2003). Another interesting aspect of the depression-like behavior of the TRH-R2 mice is the gender specificity of the phenotype. Not only is depression more prevalent in females, symptoms of major depression show gender differences (Khan et al, 2002).
A large body of human imaging studies and animal experiments suggest that depression and depression-like behavior are associated with a neuronal circuit composed of the anterior cingulate cortex and its connections with the limbic system that includes the amygdala and the hippocampus among other brain regions. TRH-R2 is expressed in these brain areas and it is particularly interesting that this receptor is the sole TRH-R in the cingulate cortex in the rat (O’Dowd et al, 2000). Since lesion of the anterior cingulate increases immobility in FST (Bissiere et al, 2008) and because FST activates the immediate early gene c-fos in this area (Duncan et al, 1996), we speculate that the absence of TRH-R2 in this region is especially relevant in the depression-like behavior of TRH-R2-/- mice. However, TRH-R2, together with TRH-R1, is also expressed in the amygdala and in the bed nucleus of the stria terminalis, other important regions in the regulation of mood and the role of this receptor pool may also play a role in the emergence of the phenotype in TRH-R2-/- mice. Indeed, the moderate phenotype we observed in TRH-R2-/- mice may be because TRH-R1, which signals via the same pathways as TRH-R2, is present in these regions.
The level of anxiety of TRH-R2 mice was tested in NIHT. Again, only female TRH-R2-/- mice showed abnormalities, specifically increased duration and reduced latency of feeding that are consistent with reduced anxiety. Although the depression-like and reduced anxiety-like behaviors of TRH-R2-/-mice seem contradictory because of the comorbidity of mood and anxiety disorders, these phenotypes represent only specific dimensions of these disorders and are uncoupled in some animal models. Indeed, 5-HT1A receptor and CREB deficient mice exhibit antidepressant-like and increased anxiety-like phenotypes (Parks et al, 1998; Sibille et al, 2000; Gur et al, 2007).
It is noteworthy that there are prominent similarities between control of central nervous system function by TRH-R1 and TRH-R2 and the better studied two receptor system for corticotropin–releasing hormone (CRH) (see (Steckler and Holsboer, 1999), for review). Like TRH-R1/TRH-R2, CRH receptor 1 (CRH1) and CRH receptor 2 (CRH2) exhibit different patterns of expression and activate multiple signaling pathways, and have been shown to mediate overlapping but different behaviors including control of mood.
In conclusion, female TRH-R2 knockout mice exhibit increased depression-like and reduced anxiety-like phenotypes. Although TRH-R1 knockout mice were reported to exhibit increased depression-like and increased anxiety-like behaviors they were hypothyroid and their behavioral changes may have been caused indirectly by hypothyroidism. TRH-R2 is not expressed in the anterior pituitary and TRH-R2-/- mice are euthyroid; thus, the data reported herein provide the first evidence of the involvement of extrahypothalamic TRH in regulating depression/anxiety-like behavior in mice and show that TRH-R2 mediates these behaviors.
Acknowledgments
We thank Dr. Chuxia Deng, Director, NIDDK Core Knockout Laboratory for advice and help in creating TRH-R2-deficient mice. We also thank Dr. Oksana Gavrilova, Director, NIDDK Mouse Metabolism Core Laboratory, for advice and help with analysis of growth and glucose/insulin homeostasis in TRH-R2-deficient mice. This work was supported by the Intramural Research Program, NIDDK, NIH and grants 5RO1 MH058669 and 1RO1 MH080194 to MT. BZ was supported by NIH predoctoral training grant 5T32DA007274.
Footnotes
DISCLOSURE/CONFLICT OF INTEREST The authors do not have direct or indirect conflicts of interest or biomedical financial interests to disclose.
References
- Alkemade A, Unmehopa UA, Brouwer JP, Hoogendijk WJ, Wiersinga WM, Swaab DF, et al. Decreased thyrotropin-releasing hormone gene expression in the hypothalamic paraventricular nucleus of patients with major depression. Mol Psychiatry. 2003;8:838–839. doi: 10.1038/sj.mp.4001364. [DOI] [PubMed] [Google Scholar]
- Bartalena L, Placidi GF, Martino E, Falcone M, Pellegrini L, Dell’Osso L, et al. Nocturnal serum thyrotropin (TSH) surge and the TSH response to TSH-releasing hormone: dissociated behavior in untreated depressives. J Clin Endocrinol Metab. 1990;71:650–655. doi: 10.1210/jcem-71-3-650. [DOI] [PubMed] [Google Scholar]
- Bissiere S, Plachta N, Hoyer D, McAllister KH, Olpe HR, Grace AA, et al. The rostral anterior cingulate cortex modulates the efficiency of amygdala-dependent fear learning. Biol Psychiatry. 2008;63:821–831. doi: 10.1016/j.biopsych.2007.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao J, O’Donnell D, Vu H, Payza K, Pou C, Godbout C, et al. Cloning and characterization of a cDNA encoding a novel subtype of rat thyrotropin-releasing hormone receptor. J Biol Chem. 1998;273:32281–32287. doi: 10.1074/jbc.273.48.32281. [DOI] [PubMed] [Google Scholar]
- Cryan JF, Markou A, Lucki I. Assessing antidepressant activity in rodents: recent developments and future needs. Trends Pharmacol Sci. 2002;23:238–245. doi: 10.1016/s0165-6147(02)02017-5. [DOI] [PubMed] [Google Scholar]
- de la Pena P, Delgado LM, del Camino D, Barros F. Two isoforms of the thyrotropin-releasing hormone receptor generated by alternative splicing have indistinguishable functional properties. J Biol Chem. 1992;267:25703–25708. [PubMed] [Google Scholar]
- Deng C, Wynshaw-Boris A, Zhou F, Kuo A, Leder P. Fibroblast growth factor receptor 3 is a negative regulator of bone growth. Cell. 1996;84:911–921. doi: 10.1016/s0092-8674(00)81069-7. [DOI] [PubMed] [Google Scholar]
- Dulawa SC, Hen R. Recent advances in animal models of chronic antidepressant effects: the novelty-induced hypophagia test. Neurosci Biobehav Rev. 2005;29:771–783. doi: 10.1016/j.neubiorev.2005.03.017. [DOI] [PubMed] [Google Scholar]
- Dulawa SC, Holick KA, Gundersen B, Hen R. Effects of chronic fluoxetine in animal models of anxiety and depression. Neuropsychopharmacology. 2004;29:1321–1330. doi: 10.1038/sj.npp.1300433. [DOI] [PubMed] [Google Scholar]
- Duncan GE, Knapp DJ, Johnson KB, Breese GR. Functional classification of antidepressants based on antagonism of swim stress-induced fos-like immunoreactivity. J Pharmacol Exp Ther. 1996;277:1076–1089. [PubMed] [Google Scholar]
- Duthie SM, Taylor PL, Anderson L, Cook J, Eidne KA. Cloning and functional characterisation of the human TRH receptor. Mol Cell Endocrinol. 1993;95:R11–15. doi: 10.1016/0303-7207(93)90043-j. [DOI] [PubMed] [Google Scholar]
- Gary KA, Sevarino KA, Yarbrough GG, Prange AJ, Jr, Winokur A. The thyrotropin-releasing hormone (TRH) hypothesis of homeostatic regulation: implications for TRH-based therapeutics. J Pharmacol Exp Ther. 2003;305:410–416. doi: 10.1124/jpet.102.044040. [DOI] [PubMed] [Google Scholar]
- Gur TL, Conti AC, Holden J, Bechtholt AJ, Hill TE, Lucki I, et al. cAMP response element-binding protein deficiency allows for increased neurogenesis and a rapid onset of antidepressant response. J Neurosci. 2007;27:7860–7868. doi: 10.1523/JNEUROSCI.2051-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez-Mariscal M, de Gortari P, Lopez-Rubalcava C, Martinez A, Joseph-Bravo P. Analysis of the anxiolytic-like effect of TRH and the response of amygdalar TRHergic neurons in anxiety. Psychoneuroendocrinology. 2008;33:198–213. doi: 10.1016/j.psyneuen.2007.11.002. [DOI] [PubMed] [Google Scholar]
- Harder S, Dammann O, Buck F, Zwiers H, Lederis K, Richter D, et al. Cloning of two thyrotropin-releasing hormone receptor subtypes from a lower vertebrate (Catostomus commersoni): functional expression, gene structure, and evolution. Gen Comp Endocrinol. 2001;124:236–245. doi: 10.1006/gcen.2001.7709. [DOI] [PubMed] [Google Scholar]
- Harder S, Lu X, Wang W, Buck F, Gershengorn MC, Bruhn TO. Regulator of G protein signaling 4 suppresses basal and thyrotropin releasing-hormone (TRH)-stimulated signaling by two mouse TRH receptors, TRH-R(1) and TRH-R(2) Endocrinology. 2001;142:1188–1194. doi: 10.1210/endo.142.3.8019. [DOI] [PubMed] [Google Scholar]
- Itadani H, Nakamura T, Itoh J, Iwaasa H, Kanatani A, Borkowski J, et al. Cloning and characterization of a new subtype of thyrotropin-releasing hormone receptors. Biochem Biophys Res Commun. 1998;250:68–71. doi: 10.1006/bbrc.1998.9268. [DOI] [PubMed] [Google Scholar]
- Khan AA, Gardner CO, Prescott CA, Kendler KS. Gender differences in the symptoms of major depression in opposite-sex dizygotic twin pairs. Am J Psychiatry. 2002;159:1427–1429. doi: 10.1176/appi.ajp.159.8.1427. [DOI] [PubMed] [Google Scholar]
- Kulkarni RN, Wang ZL, Akinsanya KO, Bennet WM, Wang RM, Smith DM, et al. Pyroglutamyl-phenylalanyl-proline amide attenuates thyrotropin-releasing hormone-stimulated insulin secretion in perifused rat islets and insulin-secreting clonal beta-cell lines. Endocrinology. 1995;136:5155–5164. doi: 10.1210/endo.136.11.7588254. [DOI] [PubMed] [Google Scholar]
- Luo LG, Yano N. Expression of thyrotropin-releasing hormone receptor in immortalized beta-cell lines and rat pancreas. J Endocrinol. 2004;181:401–412. doi: 10.1677/joe.0.1810401. [DOI] [PubMed] [Google Scholar]
- Matre V, Karlsen HE, Wright MS, Lundell I, Fjeldheim AK, Gabrielsen OS, et al. Molecular cloning of a functional human thyrotropin-releasing hormone receptor. Biochem Biophys Res Commun. 1993;195:179–185. doi: 10.1006/bbrc.1993.2027. [DOI] [PubMed] [Google Scholar]
- Merali Z, Levac C, Anisman H. Validation of a simple, ethologically relevant paradigm for assessing anxiety in mice. Biol Psychiatry. 2003;54:552–565. doi: 10.1016/s0006-3223(02)01827-9. [DOI] [PubMed] [Google Scholar]
- Mulla CM, Geras-Raaka E, Raaka BM, Gershengorn MC. Levels of TRH receptors activate programmed cell death in human pancreatic precursors. Pancreas. 2008 doi: 10.1097/MPA.0b013e31818d14a8. Published ahead of print, November 7, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dowd BF, Lee DK, Huang W, Nguyen T, Cheng R, Liu Y, et al. TRH-R2 exhibits similar binding and acute signaling but distinct regulation and anatomic distribution compared with TRH-R1. Mol Endocrinol. 2000;14:183–193. doi: 10.1210/mend.14.1.0407. [DOI] [PubMed] [Google Scholar]
- Page ME, Detke MJ, Dalvi A, Kirby LG, Lucki I. Serotonergic mediation of the effects of fluoxetine, but not desipramine, in the rat forced swimming test. Psychopharmacology (Berl) 1999;147:162–167. doi: 10.1007/s002130051156. [DOI] [PubMed] [Google Scholar]
- Parks CL, Robinson PS, Sibille E, Shenk T, Toth M. Increased anxiety of mice lacking the serotonin1A receptor. Proc Natl Acad Sci U S A. 1998;95:10734–10739. doi: 10.1073/pnas.95.18.10734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekary AE, Stevens SA, Sattin A. Circadian rhythms of TRH-like peptide levels in rat brain. Brain Res. 2006;1125:67–76. doi: 10.1016/j.brainres.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Pekary AE, Faull KF, Paulson M, Lloyd RL, Sattin A. TRH-like antidepressant peptide, pyroglutamyltyroslyprolineamide, occurs in rat brain. J Mass Spectrom. 2005;40:1232–1236. doi: 10.1002/jms.904. [DOI] [PubMed] [Google Scholar]
- Porsolt RD, Bertin A, Jalfre M. ”Behavioural despair” in rats and mice: strain differences and the effects of imipramine. Eur J Pharmacol. 1978;51:291–294. doi: 10.1016/0014-2999(78)90414-4. [DOI] [PubMed] [Google Scholar]
- Rabeler R, Mittag J, Geffers L, Ruther U, Leitges M, Parlow AF, et al. Generation of thyrotropin-releasing hormone receptor 1-deficient mice as an animal model of central hypothyroidism. Mol Endocrinol. 2004;18:1450–1460. doi: 10.1210/me.2004-0017. [DOI] [PubMed] [Google Scholar]
- Sattin A. The role of TRH and related peptides in the mechanism of action of ECT. J Ect. 1999;15:76–92. [PubMed] [Google Scholar]
- Sattin A, Pekary AE, Blood J. Escitalopram regulates expression of TRH and TRH-like peptides in rat brain and peripheral tissues. Neuroendocrinology. 2008;88:135–146. doi: 10.1159/000121595. [DOI] [PubMed] [Google Scholar]
- Sellar RE, Taylor PL, Lamb RF, Zabavnik J, Anderson L, Eidne KA. Functional expression and molecular characterization of the thyrotrophin-releasing hormone receptor from the rat anterior pituitary gland. J Mol Endocrinol. 1993;10:199–206. doi: 10.1677/jme.0.0100199. [DOI] [PubMed] [Google Scholar]
- Sibille E, Pavlides C, Benke D, Toth M. Genetic inactivation of the Serotonin(1A) receptor in mice results in downregulation of major GABA(A) receptor alpha subunits, reduction of GABA(A) receptor binding, and benzodiazepine-resistant anxiety. J Neurosci. 2000;20:2758–2765. doi: 10.1523/JNEUROSCI.20-08-02758.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckler T, Holsboer F. Corticotropin-releasing hormone receptor subtypes and emotion. Biol Psychiatry. 1999;46:1480–1508. doi: 10.1016/s0006-3223(99)00170-5. [DOI] [PubMed] [Google Scholar]
- Straub RE, Frech GC, Joho RH, Gershengorn MC. Expression cloning of a cDNA encoding the mouse pituitary thyrotropin-releasing hormone receptor. Proc Natl Acad Sci U S A. 1990;87:9514–9518. doi: 10.1073/pnas.87.24.9514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Lu X, Gershengorn MC. Thyrotropin-releasing hormone receptors -- similarities and differences. J Mol Endocrinol. 2003;30:87–97. doi: 10.1677/jme.0.0300087. [DOI] [PubMed] [Google Scholar]
- Sun YM, Millar RP, Ho H, Gershengorn MC, Illing N. Cloning and characterization of the chicken thyrotropin-releasing hormone receptor. Endocrinology. 1998;139:3390–3398. doi: 10.1210/endo.139.8.6133. [DOI] [PubMed] [Google Scholar]
- Takata M, Shimada Y, Ikeda A, Sekikawa K. Molecular cloning of bovine thyrotropin-releasing hormone receptor gene. J Vet Med Sci. 1998;60:123–127. doi: 10.1292/jvms.60.123. [DOI] [PubMed] [Google Scholar]
- Yamada M, Saga Y, Shibusawa N, Hirato J, Murakami M, Iwasaki T, et al. Tertiary hypothyroidism and hyperglycemia in mice with targeted disruption of the thyrotropin-releasing hormone gene. Proc Natl Acad Sci U S A. 1997;94:10862–10867. doi: 10.1073/pnas.94.20.10862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada M, Shibusawa N, Hashida T, Ozawa A, Monden T, Satoh T, et al. Expression of thyrotropin-releasing hormone (TRH) receptor subtype 1 in mouse pancreatic islets and HIT-T15, an insulin-secreting clonal beta cell line. Life Sci. 2000;66:1119–1125. doi: 10.1016/s0024-3205(00)00415-x. [DOI] [PubMed] [Google Scholar]
- Yang X, Li C, Xu X, Deng C. The tumor suppressor SMAD4/DPC4 is essential for epiblast proliferation and mesoderm induction in mice. Proc Natl Acad Sci U S A. 1998;95:3667–3672. doi: 10.1073/pnas.95.7.3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarbrough GG, Kamath J, Winokur A, Prange AJ., Jr Thyrotropin-releasing hormone (TRH) in the neuroaxis: therapeutic effects reflect physiological functions and molecular actions. Med Hypotheses. 2007;69:1249–1256. doi: 10.1016/j.mehy.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Zeng H, Schimpf BA, Rohde AD, Pavlova MN, Gragerov A, Bergmann JE. Thyrotropin-releasing hormone receptor 1-deficient mice display increased depression and anxiety-like behavior. Mol Endocrinol. 2007;21:2795–2804. doi: 10.1210/me.2007-0048. [DOI] [PubMed] [Google Scholar]
- Zhao D, Yang J, Jones KE, Gerald C, Suzuki Y, Hogan PG, et al. Molecular cloning of a complementary deoxyribonucleic acid encoding the thyrotropin-releasing hormone receptor and regulation of its messenger ribonucleic acid in rat GH cells. Endocrinology. 1992;130:3529–3536. doi: 10.1210/endo.130.6.1317787. [DOI] [PubMed] [Google Scholar]


