Abstract
Background: With the aging of the world's population, the social and economic implications of osteoporotic fractures are at epidemic proportions. This study was performed to test the hypothesis that a proximal humeral fracture is an independent risk factor for a subsequent hip fracture and that the risk of the subsequent hip fracture is highest within the first five years after the humeral fracture.
Methods: A cohort of 8049 older white women with no history of a hip or humeral fracture who were enrolled in the Study of Osteoporotic Fractures was followed for a mean of 9.8 years. The risk of hip fracture after an incident humeral fracture was estimated with use of age-adjusted Cox proportional hazards regression analysis with time-varying variables; women without a humeral fracture were the reference group. Cox regression analysis was used to evaluate the timing between the proximal humeral and subsequent hip fracture. Risk factors were determined on the basis of a review of the current literature, and we chose the variables that were most predictive and easily ascertained in a clinical setting.
Results: Three hundred and twenty-one women sustained a proximal humeral fracture, and forty-four of them sustained a subsequent hip fracture. After adjustment for age and bone mineral density, the hazard ratio for hip fracture for subjects with a proximal humeral fracture relative to those without a proximal humeral fracture was 1.83 (95% confidence interval = 1.32 to 2.53). After multivariate adjustment, this risk appeared attenuated but was still significant (hazard ratio = 1.57; 95% confidence interval = 1.12 to 2.19). The risk of a subsequent hip fracture after a proximal humeral fracture was highest within one year after the proximal humeral fracture, with a hazard ratio of 5.68 (95% confidence interval = 3.70 to 8.73). This association between humeral and hip fracture was not significant after the first year, with hazard ratios of 0.87 (95% confidence interval = 0.48 to 1.59) between one and five years after the humeral fracture and 0.58 (95% confidence interval = 0.22 to 1.56) after five years.
Conclusions: In this cohort of older white women, a proximal humeral fracture independently increased the risk of a subsequent hip fracture more than five times in the first year after the humeral fracture but was not associated with a significant increase in the hip fracture risk in subsequent years.
Level of Evidence: Prognostic Level II. See Instructions to Authors for a complete description of levels of evidence.
Osteoporosis and associated fragility fractures are a major health concern and a source of substantial morbidity and mortality around the world. It was estimated that, in 2006 in the United States, the economic burden associated with hip fractures alone might have been in excess of $20 billion1-9. As the world's population increases and ages, the number of hip fractures will continue to grow. In addition to the increased mortality associated with hip fractures, the related loss of independence and function and the increased burden on family and caregivers can be onerous10-13. Given the enormous social and monetary costs of hip fractures, their prevention is a pressing concern.
It is well established that patients who have had a single fragility fracture are at significantly increased risk of having a second fracture in the future14-16. Proximal humeral fractures represent a unique subset of osteoporotic fractures; up to 73% of these fractures occur in women, making them the second most common upper-extremity fractures17-19. A proximal humeral fracture also appears to be a risk factor for the subsequent occurrence of other incident fractures, including those at the hip20,21. Johnell et al. evaluated the timing of subsequent fragility fractures after an individual had sustained an incident fracture of the spine, proximal part of the humerus, or hip. They found that the risk was highest immediately following the incident fracture and that the risk decreased with time22. However, that study was limited by the fact that the authors did not control for many important risk factors, such as bone mineral density. Still, these data suggest that a fracture of the proximal part of the humerus may be predictive of an increased risk of a subsequent hip fracture.
Interestingly, the mechanism of proximal humeral fractures tends to be more similar to that of hip fractures than to that of any other osteoporotic fracture; i.e., they occur when the individual is unable to break his or her forward or oblique fall and therefore lands directly onto the shoulder or hip23,24. Given the similar mechanisms of the fractures, it is intuitive that the timing of a hip fracture would be relatively close to the timing of a proximal humeral fracture and likely would place the patient at higher risk for sustaining a subsequent hip fracture.
The purpose of this study was to further evaluate the relationship between fractures of the proximal part of the humerus and fractures of the hip in an elderly female patient population while adjusting for bone mineral density and other important covariates. We hypothesized that individuals who sustained a proximal humeral fracture would be at higher risk for a subsequent hip fracture and that the hip fracture would tend to occur within five years after the fracture of the proximal part of the humerus.
Materials and Methods
Participants
The Study of Osteoporotic Fractures is a prospective multicenter cohort study of 9704 women sixty-five years of age and older who were enrolled from September 1986 to October 1988 in four separate geographic areas of the United States (Baltimore, Maryland; Minneapolis, Minnesota; Portland, Oregon; and Monongahela Valley, Pennsylvania). The institutional review boards at the individual study sites approved the study, and all of the women provided written informed consent. Women were recruited if they were sixty-five or older, community dwelling, and able to walk and had not had a bilateral hip replacement. A complete description of the methods of patient recruitment as well as of the inclusion and exclusion criteria have been provided previously25,26. The women were followed prospectively at regular intervals for up to ten years. The participants returned for seven examinations at approximately two-year intervals and were contacted by telephone or postcard every four months to ascertain fracture history; the follow-up rate was 99%, and the accuracy of the patients' self-report of fractures was 90%27. From 1997 to 1998, a cohort of black women was added to the study; this cohort was excluded from the present study because of the low risk of osteoporotic fractures in these women and the considerably shorter follow-up time28.
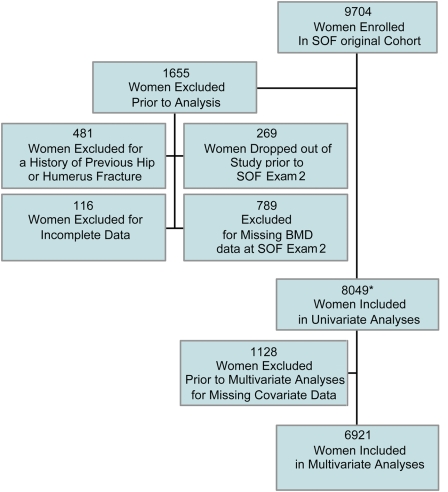
The original cohort of the Study of Osteoporotic Fractures included 9704 women, of whom 1655 (17%) were excluded from our study because of missing data regarding prior fracture status or age (116 women), lack of complete follow-up (269 women dropped out before the second examination performed for the Study of Osteoporotic Fractures), a history of a hip or humeral fracture prior to the second examination (481 women), or missing bone-mineral-density data at the time of the second examination for the Study of Osteoporotic Fractures (789 women). The second examination was used as the baseline for analysis as bone mineral density, an important risk factor, was measured at that visit but not at the first examination. A total of 8049 women (83%) were entered into our present study, and their information was used in the univariate Cox regression analyses. Fewer than 8049 women were included in some univariate Cox regression analyses because of missing values for the predictor variable. A total of 1128 (12%) were excluded from the final multivariate analysis because of missing data regarding one or more of the covariates listed below; this left 6921 women (71%) to be analyzed in the multivariate Cox regression model (Fig. 1).
Fig. 1.
Flow diagram demonstrating the number of subjects excluded from analysis and the time points at which they were excluded. *A maximum of 8049 women were included in the univariate analysis, but not all subjects had complete data sets for evaluation. The patients with missing data were excluded from the individual univariate analysis of the variable(s) for which data were missing, but they were included in all analyses of the available variables. The number of women included in the individual analyses ranged from 6153 to 8049. SOF = Study of Osteoporotic Fractures, and BMD = bone mineral density.
Ascertainment of Incident Fractures
The study subjects were asked to notify their local clinical site after the occurrence of any fracture. Additionally, participants were contacted every four months by letter or telephone to ask if a fall or fracture had occurred in the preceding four months. When fractures were reported, the treating physician was contacted and the anatomic location and circumstances were established. Fractures were then confirmed by central review of the community radiologist's report or of preoperative radiographs as previously described by Nevitt et al.27. A fracture of the proximal part of the humerus was defined as one in the proximal one-third of the humerus. For the purposes of our study, a non-humeral fracture, non-hip was defined as a fracture of the wrist, pelvis, finger, clavicle, elbow, rib, ankle, hand, face, toe, foot, heel, leg, knee, or distal part of the femur.
Ascertainment of Variables
Candidate variables for inclusion in the multivariate analyses were identified from among common risk factors for hip and humeral fractures reported in prior studies25,29-32. At the first examination for the Study of Osteoporotic Fractures, participants were asked to self-report age, height, and nonpregnant weight at the age of twenty-five years; parental history of fractures; physician-diagnosed fractures since the age of twenty-five; estrogen therapy, currently and in the previous year; current usage of long-acting benzodiazepines; overall health status; number of falls within the last year; and number of hours spent standing or walking each day. Depth perception was assessed with use of the Howard-Dolman device and scored as the standard deviation, in centimeters, of four trials33.
At the second examination for the Study of Osteoporotic Fractures, hip bone mineral density was measured with use of dual x-ray absorptiometry (QDR-1000; Hologic, Waltham, Massachusetts). Current height (as measured with a stadiometer) and weight and the ability to rise from a chair without using the arms were documented during the physical examination.
For the purposes of our study, the second examination was considered to be the baseline examination for analysis and all covariates that were available at multiple time points, including health status as self-rated on a scale of 1 (excellent) to 5 (very poor), use of the arms to rise from a chair, walking for exercise, number of hours standing or walking each day, visual depth perception, weight gain since the age of twenty-five years, total hip bone mineral density, estrogen use, and history of falls within the last year. This was done in order to include bone mineral density, which was not measured until the second examination. All patients who sustained a fracture of the hip or proximal part of the humerus between the first and second examinations were excluded from the analysis. An average of 2.04 years elapsed between the first and second examinations. Information about the use of long-acting benzodiazepines, height at the age of twenty-five, and maternal history of hip fracture (after the age of fifty) was collected only at the first examination, and this information was used for the patients included in our study.
Statistical Analysis
Cox proportional hazards models were used to quantify the association between incident humeral fracture and the risk of subsequent hip fracture. All models were adjusted for current age and total hip bone mineral density. Each observation in the Cox regression was left-censored at the age at which the subject entered the study and either ended at the time of hip fracture or was right-censored at the end of the follow-up period.
Humeral fracture was handled as a time-dependent variable. Each participant's study period was divided into two intervals: one prior to a humeral fracture, and one following a humeral fracture and ending at the time of a hip fracture or at the end of the follow-up period. Patients who did not sustain a proximal humeral fracture were evaluated from the time of the second examination through the end of the follow-up period. Non-humeral fracture, as a time-dependent variable, was treated similarly.
Control variables that were available at multiple times were also handled as time-dependent variables. These included self-rated health status, use of the arms to rise from a chair, walking for exercise, number of hours standing or walking each day, visual depth perception, weight gain since the age of twenty-five, total hip bone mineral density, estrogen use, and history of falls within the last year. As mentioned, information about use of long-acting benzodiazepines, height at the age of twenty-five, and maternal history of hip fracture (after the age of fifty) were collected only at the first examination, and these were used as time-constant covariates. The data setup of the time-dependent variables was handled by the traditional method used for survival analysis with time-dependent variables34. Each subject's time in the study was partitioned into intervals such that the value of all variables remained constant within each time interval.
Multivariate Cox regression analysis was used to test the association between incident humeral fracture and subsequent hip fracture, with adjustment for selected control variables. Control variables were selected by forward stepwise regression (p < 0.05 for inclusion), with total hip bone mineral density and age always being included in the model. The control variables included in the final multivariate proportional hazards model were self-reported health status, height at the age of twenty-five, history of recent falls, depth perception, and prior non-humeral fracture. After selection of control variables for and running of the final model without reference to the incident humeral fracture, the incident humeral fracture variable was added into this model and the model was rerun.
The potential confounding role of a non-humeral fracture was evaluated with two methods. First, we calculated the risk due to the humeral fracture in a multivariate model that included a covariate indicating a prior non-humeral fracture after the second examination. This method controlled for the non-humeral fracture by modeling—i.e., by use of a covariate. We also calculated the risk due to the humeral fracture by using a multivariate model but excluding time intervals following any non-humeral fracture. This method controls for the non-humeral fracture by eliminating any periods of observation after such a fracture has occurred.
In order to examine whether the risk of a subsequent hip fracture attributable to an incident humeral fracture changes over the time elapsed after the humeral fracture, two multivariate models categorizing time after the humeral fracture as a time-dependent variable were used. The three post-humeral fracture intervals were less than one year, one to five years, and more than five years after the humeral fracture, with subjects not sustaining an incident humeral fracture utilized as the reference group for all analyses. The first of the two multivariate models adjusted only for age and bone mineral density, whereas the second model adjusted for age, bone mineral density, and the control variables selected in the forward stepwise selection process (described above). Each of these two multivariate models provided an estimate of the hazard ratio for hip fracture specific to each post-humeral fracture time interval (less than one year, one to five years, and more than five years) relative to the risk in subjects without a humeral fracture.
Source of Funding
No outside funding was used in support of this research. The Study of Osteoporotic Fractures is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, and 2 R01 AG027574-22A1.
Results
The mean duration of follow-up of the 8049 women included in the analysis was 9.8 years (range, zero to ten years). Of the 321 women who sustained a proximal humeral fracture after baseline (the second examination for the Study of Osteoporotic Fractures), forty-four (13.7%) sustained a subsequent hip fracture (13.9 fractures per 1000 patient years). Of the women who did not sustain a proximal humeral fracture, 739 (9.6%) sustained a subsequent hip fracture (9.7 fractures per 1000 patient years). Patient demographics are outlined in Table I.
TABLE I.
Baseline Data for Patients Evaluated*
| No. for Whom Data Available | Value | |
|---|---|---|
| Age at 2nd examination†(yr) | 8049 | 73 ± 5 |
| Total hip bone mineral density†(g/cm2) | 8049 | 0.76 ± 0.13 |
| Calcaneal bone mineral density†(g/cm2) | 8024 | 0.41 ± 0.09 |
| Height at age of 25 yr†‡(cm) | 7904 | 163 ± 6 |
| Depth perception (per 10 times standard deviation of 4 Howard-Dolman optical distance scores)†(cm) | 7820 | 2.13 ± 2.49 |
| Weight gain since age of 25 yr†(kg) | 7642 | 10.2 ± 10.3 |
| Maternal history of hip fracture after age of 50 yrठ| 6153 | 13 |
| Estrogen use§ | 8045 | 15 |
| Use of long-acting benzodiazepines at baselineठ| 8008 | 9 |
| Self-reported health status (on a scale of 1-5)† | 8049 | 1.84 ± 0.70 |
| Walking for exercise§ | 8049 | 52 |
| Standing or walking <4 hr/day§ | 8039 | 9 |
| Use of arms to rise from chair§ | 8045 | 4 |
| History of falls§ | 8048 | 31 |
All measures were recorded at the second examination, except where indicated.
The values are given as the mean and standard deviation.
The value was unavailable at the second examination, and the value at the first examination was used.
The values are given as the percentage.
An incident humeral fracture was associated with an 83% increase in the risk of a subsequent incident hip fracture, after adjustment for age and total hip bone mineral density (Table II). A non-humeral fracture, height at the age of twenty-five years, depth perception, maternal history of a hip fracture after the age of fifty, health status, walking for exercise, standing or walking for less than four hours per day, use of the arms to rise from a chair, and a history of falls were also modestly associated with an incident hip fracture, after adjustment for age and total hip bone mineral density (Table II). These findings were consistent with previously reported results, and the factors were considered for inclusion in the multivariate model25.
TABLE II.
Effect of Risk Factors for Hip Fracture, Adjusted for Age and Total Hip Bone Mineral Density
| Risk Factor | No. for Whom Data Available | Hazard Ratio (95% Confidence Interval) | P Value |
|---|---|---|---|
| Total hip bone mineral density (per 1 standard deviation decrease*) | 8049 | 2.11 (1.94 to 2.29) | <0.001 |
| Humeral fracture | 8049 | 1.83 (1.32 to 2.53) | <0.001 |
| Non-humeral fracture | 8049 | 1.43 (1.20 to 1.72) | <0.001 |
| Height at age of 25 yr (per 10 cm) | 7904 | 1.41 (1.24 to 1.61) | <0.001 |
| Depth perception (per 10 times standard deviation of 4 Howard-Dolman optical distance scores) | 7851 | 1.43 (1.13 to 1.82) | 0.003 |
| Weight gain since age of 25 yr (per 10 kg) | 7823 | 0.94 (0.85 to 1.04) | 0.2 |
| Maternal history of hip fracture after age of 50 yr | 6153 | 1.33 (1.06 to 1.66) | 0.013 |
| Estrogen use | 8048 | 1.09 (0.86 to 1.40) | 0.5 |
| Use of long-acting benzodiazepines at baseline | 8008 | 0.98 (0.75 to 1.23) | 0.9 |
| Self-reported health status (on a scale of 1-5) | 8049 | 1.33 (1.20 to 1.46) | <0.001 |
| Walking for exercise | 8049 | 0.85 (0.73 to 0.99) | 0.04 |
| Standing or walking <4 hr/day | 8046 | 1.27 (1.04 to 1.55) | 0.02 |
| Use of arms to rise from chair | 8046 | 1.37 (1.12 to 1.67) | 0.002 |
| History of falls | 8049 | 1.38 (1.18 to 1.61) | <0.001 |
1 standard deviation = 0.133 g/cm2. Total hip bone mineral density was adjusted for age only.
The final multivariate model showed that the hazard ratio for subsequent hip fracture following a proximal humeral fracture was 1.57 (95% confidence interval = 1.12 to 2.19), after adjustment for age, total hip bone mineral density, self-reported health status, height at the age of twenty-five, recent falls, depth perception, and prior non-humeral, non-hip fracture. The hip fracture risk following the humeral fracture was greater than the risk conferred by a non-humeral, non-hip fracture that occurred after the second examination (hazard ratio = 1.28, 95% confidence interval = 1.06 to 1.55) (Table III). Total hip bone mineral density also had a strong association with subsequent hip fracture (hazard ratio = 2.08 per each one standard deviation decrease; 95% confidence interval = 1.91 to 2.27).
TABLE III.
Final Multivariate Cox Proportional Hazards Model for Hip Fracture, Including Humeral Fracture as a Risk Factor (N = 6921 Subjects)
| Risk Factor | Hazard Ratio (95% Confidence Interval) | P Value |
|---|---|---|
| Total hip bone mineral density (per 1 standard deviation decrease*) | 2.08 (1.91 to 2.27) | <0.001 |
| Self-reported health status (on a scale of 1-5) | 1.24 (1.12 to 1.38) | <0.001 |
| Height at age of 25 yr (per 10 cm) | 1.39 (1.22 to 1.59) | <0.001 |
| History of falls | 1.29 (1.10 to 1.52) | 0.002 |
| Depth perception (per 10 times standard deviation of 4 Howard-Dolman optical distance scores) | 1.53 (1.19 to 1.97) | 0.001 |
| Non-humeral fracture | 1.28 (1.06 to 1.55) | 0.01 |
| Humeral fracture | 1.57 (1.12 to 2.19) | 0.009 |
1 standard deviation = 0.133 g/cm2.
The adjusted hazard ratio for an incident hip fracture following a humeral fracture compared with time intervals without, or prior to, a humeral fracture changed very little if a history of a non-humeral, non-hip fracture was not included as a covariate (Table IV). Excluding the follow-up time after a non-humeral, non-hip fracture increased the estimated adjusted excess risk of a hip fracture attributable to a prior humeral fracture from 57% to 95% (Table IV). The comparison in Table IV shows that there is no conclusive evidence of a confounding effect from a non-humeral fracture. The confidence interval around each hazard ratio estimate in Table IV overlaps each of the other hazard ratio estimates, and therefore non-humeral, non-hip fractures have no clear confounding effect on the association between a humeral and a subsequent hip fracture. In fact, adjustment for non-humeral fractures tends to strengthen the evidence of the risk associated with humeral fractures, since (1) the estimated hazard ratio increases after the exclusion of the time interval after the humeral fracture and (2) controlling for the non-humeral fracture through use of a covariate has a very minor impact on the estimated hazard ratio, decreasing it very slightly.
TABLE IV.
Analysis of Potential Confounding of the Hip Fracture-Humeral Fracture Relationship by a History of Non-Humeral Fracture
| Hazard Ratio for Humeral Fracture (95% Confidence Interval) | P Value | |
|---|---|---|
| Final multivariate model* including humeral fracture, with final model controlling for history of non-humeral fracture | 1.57 (1.12 to 2.19) | 0.009 |
| Final multivariate model* including humeral fracture, without control for history of non-humeral fracture | 1.63 (1.16 to 2.28) | 0.004 |
| Final multivariate model* including humeral fracture but excluding time intervals after non-humeral fracture | 1.95 (1.31 to 2.91) | 0.001 |
Includes self-reported health status, height at the age of twenty-five years, a history of recent falls, depth perception, and a history of non-humeral, non-hip fracture, unless otherwise noted.
When the follow-up time after a humeral fracture was segmented, the humeral fracture was found to confer a six-times higher risk of incident hip fracture during the first year after the humeral fracture, after adjustment for age and total hip bone mineral density (Table V). Little change was noted in the strength of this association with further adjustment for self-reported health status, height at the age of twenty-five, recent falls, depth perception, and prior non-humeral, non-hip fracture. No significant association between humeral fractures and incident hip fractures during follow-up time periods after one year was found when the hazard ratios in those periods were compared with those in the time interval without, or prior to, a humeral fracture (Table V). This lack of significance, however, should not be interpreted as no difference. The hazard ratios in the periods of one to five years and more than five years after humeral fracture, as compared with those in the period without, or prior to, a humeral fracture, have wide confidence intervals, allowing the possibility of both no difference in risk as well as either a positive or a negative impact on risk. Because of the small numbers of total person-years and hip fractures during the periods one to five years and more than five years after the humeral fracture, this study was not sufficiently powered to detect some clinically relevant differences that may occur in these two periods compared with the findings in the time interval without, or prior to, a humeral fracture. A post-hoc power analysis in which we assumed that a hazard ratio of >1.2 or <0.8 constituted a clinically relevant difference showed that the study had very low (approximately 10%) power to detect such a difference. Importantly, the difference between hazard ratios in the first year after humeral fracture and those in either of the two subsequent periods was very large and also significant.
TABLE V.
Risk of a Hip Fracture Over Time Following a Humeral Fracture
| Period | Hazard Ratio, Adjusted for Age and Bone Mineral Density (95% Confidence Interval) | Hazard Ratio, Adjusted for Age, Bone Mineral Density, and Variables from the Final Multivariate Model* (95% Confidence Interval) |
|---|---|---|
| Before humeral fracture | 1.00 | 1.00 |
| 1st yr after humeral fracture | 6.16 (4.01 to 9.44) | 5.68 (3.70 to 8.73) |
| 1-5 yr after humeral fracture | 1.16 (0.67 to 2.02) | 0.87 (0.48 to 1.59) |
| >5 yr after humeral fracture | 0.64 (0.24 to 1.71) | 0.58 (0.22 to 1.56) |
Self-reported health status, height at the age of twenty-five years, a history of recent falls, depth perception, and a history of non-humeral, non-hip fracture.
Discussion
In this cohort of older, community-dwelling women, an incident proximal humeral fracture significantly increased the risk of a subsequent hip fracture, with the risk being six times higher within the first year following the proximal humeral fracture after we controlled for other important risk factors in a multivariate analysis. The association between proximal humeral and subsequent hip fractures was not significant during time intervals of greater than one year after the incident humeral fracture. Although our study could have missed a modest persistent association between incident humeral and subsequent hip fractures occurring at more than one year after the humeral fracture, it was clear that the increased risk of hip fracture attributable to a prior humeral fracture sharply waned after one year of follow-up.
Few investigators have examined the risk of hip fracture after a proximal humeral fracture or, importantly, the timing of those subsequent fractures. In studies in which this relationship was evaluated20,22,35, sample sizes were small, the subjects were from a single geographic region, or the authors did not control for important risk factors when evaluating the times of subsequent fractures.
Lauritzen et al. found that women between sixty and seventy-nine years of age who had previously sustained a fracture of the proximal part of the humerus had a relative risk of sustaining a hip fracture of 2.520. However, this study included women from only one geographic area and the follow-up period was relatively short (3.7 years). This is of importance because of the geographic variability in hip-fracture incidence noted by other authors17,36. In contrast, women from four different geographic regions were analyzed in the current study. This likely increased the heterogeneity of the evaluated patient population and may make the results more representative when applied to the women of the United States as a whole.
Johnell et al. reported an increased risk of hip fracture following an incident humeral fracture, with the increased risk persisting for up to five years after the incident fracture22. The absence of a significant increase in hip-fracture risk beyond one year after the humeral fracture in our study may be related to our adjustment for additional important covariates that have been shown to increase the risk of a subsequent hip fracture, especially bone mineral density; it may also be due to either an absence of risk or a lack of power to detect a modest risk. We previously showed a modest increase in the risk of subsequent hip fracture following a non-spine, non-hip fracture after controlling for age and bone mineral density35. The adjusted hazard ratio was 1.70 (95% confidence interval = 1.30 to 2.22) during the first five years of follow-up. The risk was attenuated but still significantly increased during the five-to-ten and more-than-ten-year follow-up periods (hazard ratios of 1.32 and 1.21, respectively) in that study. The reason for the nonsignificant association between humeral fractures more than one year old and subsequent hip fracture in the current study, a finding that is in contrast to those of the previously published studies, is not clear, although our study may have been underpowered to detect a modest persistent association between humeral fractures and hip fractures occurring after more than one year of follow-up. Although the associations between prior humeral fractures as well as non-spine, non-hip fractures and subsequent hip fractures were also noted to wane with follow-up time in the study by Johnell et al.22 and our previous study35, the associations were still significant after one year in both of those studies. One can speculate that, in the initial time following a proximal humeral fracture, the effect of both environmental and medical interventions has not yet been fully realized, so the patients are still at risk for additional falls and subsequent fractures. Additionally, one can conjecture that a proximal humeral fracture and subsequent immobilization may affect the patient's ability to walk and perform activities of daily living safely. Furthermore, decreased balance and reaction time may predispose patients to future falls and fractures.
The results of the current study have important implications for the clinical evaluation, treatment, and prevention of future fractures in patients who have sustained a proximal humeral fracture. They demonstrate that the most dangerous time with regard to the risk of a subsequent hip fracture is within a year after the proximal humeral fracture and therefore intervention following a humeral fracture should be initiated without delay to reduce the risk of subsequent fractures. Studies have suggested that oral bisphosphonates begin to reduce the risk of fractures within three to six months after they are started37. In addition to the initiation of medical treatment of osteoporosis, steps should be taken to prevent falls in the at-risk population, as nearly 80% of proximal humeral fractures and 90% of hip fractures are related to falls from a standing height38,39. A recent meta-analysis demonstrated the need for a multifaceted approach to the prevention of falls in hospitals and nursing homes and that no single intervention had a significant effect in a hospital setting40. Although the patients in that study were evaluated in a hospital or nursing home setting (unlike our patients, who were community dwellers), the patients in our study also likely needed a multifaceted approach to the prevention of additional falls, whether it be assistive devices at home, adjustment of medications, or evaluation of environmental factors that lead to falls as well as the initiation of medical therapy for osteoporosis. Recent guidelines for the prevention of falls by the elderly formulated by the American Geriatrics Society, the British Geriatrics Society, and the American Academy of Orthopaedic Surgeons serve as a useful resource in the evaluation and prevention of falls in the geriatric population41. It is also important to note that the risk of a subsequent fracture is increased after a proximal humeral fracture not only in women but also in men, as noted by Ettinger et al.42.
This study has numerous strengths. To our knowledge, we were the first to assess how the association of humeral fractures with subsequent hip fractures changes over time, in an analysis adjusted for hip bone mineral density and other covariates. Second, because we used humeral fractures occurring after the second examination for the Study of Osteoporotic Fractures as a time-varying predictor, we were able to very accurately assess the time since the predictor fracture. Third, this study was of a large cohort of elderly women, in whom incident hip fractures are ascertained with 99% accuracy28. Additionally, the women in our study were from four different geographic regions of the United States so the results are likely more generalizable to the older white female population of the United States than are results of women from a single geographic region.
This study also has important limitations. Participants in the Study of Osteoporotic Fractures were community-dwelling white women sixty-five years of age and older who had volunteered for inclusion in the study. They likely represent a healthier population in comparison with similarly aged individuals living in nursing home or assisted-living environments, and our conclusions may not apply to individuals living in those settings. Because the risk of proximal humeral fractures in people of other ethnicities is typically lower than that in the white population, generalizations regarding fracture risk may not be applicable to individuals of other racial backgrounds. In addition, sex-related differences in fracture incidence make the results less meaningful for the male population.
Fracture occurrence was determined initially on the basis of self-report and was confirmed by radiographs or radiographic reports. However, this possible limitation is mitigated by the fact that ascertainment of incident hip and humeral fractures in the Study of Osteoporotic Fractures has been shown to be highly accurate27. The number of potential risk factors considered in the multivariate analysis was limited in comparison with the numbers of risk factors for hip fractures reported in previous studies. The variables were chosen in the hope of defining easily identifiable and clinically relevant risk factors that could be ascertained quickly in a clinical setting. This may have led to an overestimation of the effect of proximal humeral fractures. However, the variables used in the analysis were based on the most predictive variables reported in the current literature, and both age and bone mineral density were controlled for in all analyses. Those two variables have consistently been shown to be the most significant risk factors for osteoporotic fractures.
The data retrieved from the Study of Osteoporotic Fractures is based on self-reported questionnaires and is subject to error and patient bias. Recall bias may be of particular importance with regard to questions about height and weight at the age of twenty-five, given the time that had elapsed between when the participants were twenty-five and when they enrolled in the study. Although the rate of follow-up of patients enrolled in the Study of Osteoporotic Fractures was excellent, approximately 1700 patients were excluded from our univariate analysis because of missing or incomplete data, and an additional 1100 were excluded from the multivariate analysis. However, the remaining number of participants with complete follow-up was still quite large and allowed meaningful evaluation and statistical analysis.
In conclusion, the current study supports our hypothesis that a proximal humeral fracture is an independent risk factor for subsequent hip fracture. Importantly, the time of greatest risk is the first year following the proximal humeral fracture, with the risk of an incident hip fracture attributable to a prior humeral fracture waning sharply after that. This small window of time provides an opportunity to implement medical and environmental interventions that may decrease the risk of subsequent hip fractures and their cost to the patient and to society. 
Supplementary Material
Disclosure: The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. A commercial entity (Roche, Inc.) paid or directed in any one year, or agreed to pay or direct, benefits of less than $10,000 to a research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which one or more of the authors, or a member of his or her immediate family, is affiliated or associated.
A commentary is available with the electronic versions of this article, on our web site (www.jbjs.org) and on our quarterly CD-ROM/DVD (call our subscription department, at 781-449-9780, to order the CD-ROM or DVD).
Investigation performed at the Department of Orthopaedics, University of Washington, Seattle, Washington
References
- 1.Blackman DK, Kamimoto LA, Smith SM. Overview: surveillance for selected public health indicators affecting older adults—United States. MMWR CDC Surveill Summ. 1999;48:1-6. [PubMed] [Google Scholar]
- 2.Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;252:163-6. [PubMed] [Google Scholar]
- 3.Ray NF, Chan JK, Thamer M, Melton LJ 3rd. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res. 1997;12:24-35. [DOI] [PubMed] [Google Scholar]
- 4.Allander E, Gullberg B, Johnell O, Kanis JA, Ranstam J, Elffors L. Circumstances around the fall in a multinational hip fracture risk study: a diverse pattern for prevention. MEDOS Study Group. Mediterranean Osteoporosis Study. Accid Anal Prev. 1998;30:607-16. [DOI] [PubMed] [Google Scholar]
- 5.Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364-70. [DOI] [PubMed] [Google Scholar]
- 6.Vellas BJ, Albarede J, Garry PJ. Facts and research in gerontology. New York: Springer; 1993. Increasing number of hip fractures: are the elderly at greater risk of hip fracture today than yesterday? p 121-9.
- 7.Lyons AR. Clinical outcomes and treatment of hip fractures. Am J Med. 1997;103:51S-64S. [DOI] [PubMed] [Google Scholar]
- 8.Yan L, Zhou B, Prentice A, Wang X, Golden MH. Epidemiological study of hip fracture in Shenyang, People's Republic of China. Bone. 1999;24:151-5. [DOI] [PubMed] [Google Scholar]
- 9.Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Järvinen M. Hip fractures in Finland between 1970 and 1997 and predictions for the future. Lancet. 1999;353:802-5. [DOI] [PubMed] [Google Scholar]
- 10.Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285-9. [DOI] [PubMed] [Google Scholar]
- 11.Schneider EL, Guralnik JM. The aging of America. Impact on health care costs. JAMA. 1990;263:2335-40. [PubMed] [Google Scholar]
- 12.Meunier PJ. Epidemiology and prevention of hip fractures. In: Proceedings of the XIXth ILAR Congress of Rheumatology; Singapore; Communication Consultants; 1997. p. 5-8.
- 13.Aharonoff GB, Koval KJ, Skovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma. 1997;11:162-5. [DOI] [PubMed] [Google Scholar]
- 14.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721-39. [DOI] [PubMed] [Google Scholar]
- 15.Wu F, Mason B, Horne A, Ames R, Clearwater J, Liu M, Evans MC, Gamble GD, Reid IR. Fractures between the ages of 20 and 50 years increase women's risk of subsequent fractures. Arch Intern Med. 2002;162:33-6. [DOI] [PubMed] [Google Scholar]
- 16.Haentjens P, Autier P, Collins J, Velkeniers B, Vanderschueren D, Boonen S. Colles fracture, spine fracture, and subsequent risk of hip fracture in men and women. A meta-analysis. J Bone Joint Surg Am. 2003;85:1936-43. [DOI] [PubMed] [Google Scholar]
- 17.Karagas MR, Baron JA, Barrett JA, Jacobsen SJ. Patterns of fracture among the United States elderly: geographic and fluoride effects. Ann Epidemiol. 1996;6:209-16. [DOI] [PubMed] [Google Scholar]
- 18.Seeley DG, Browner WS, Nevitt MC, Genant HK, Scott JC, Cummings SR. Which fractures are associated with low appendicular bone mass in elderly women? The Study of Osteoporosis Factors Research Group. Ann Intern Med. 1991;115:837-42. [DOI] [PubMed] [Google Scholar]
- 19.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87-92. [DOI] [PubMed] [Google Scholar]
- 20.Lauritzen JB, Schwarz P, McNair P, Lund B, Transbøl I. Radial and humeral fractures as predictors of subsequent hip, radial or humeral fractures in women, and their seasonal variation. Osteoporos Int. 1993;3:133-7. [DOI] [PubMed] [Google Scholar]
- 21.Robinson CM, Royds M, Abraham A, McQueen MM, Court-Brown CM, Christie J. Refractures in patients at least forty-five years old. A prospective analysis of twenty-two thousand and sixty patients. J Bone Joint Surg Am. 2002;84:1528-33. [DOI] [PubMed] [Google Scholar]
- 22.Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15:175-9. [DOI] [PubMed] [Google Scholar]
- 23.Wei TS, Hu CH, Wang SH, Hwang KL. Fall characteristics, functional mobility and bone mineral density as risk factors of hip fracture in the community-dwelling ambulatory elderly. Osteoporos Int. 2001;12:1050-5. [DOI] [PubMed] [Google Scholar]
- 24.Palvanen M, Kannus P, Parkkari J, Pitkäjärvi T, Pasanen M, Vuori I, Järvinen M. The injury mechanisms of osteoporotic upper extremity fractures among older adults: a controlled study of 287 consecutive patients and their 108 controls. Osteoporos Int. 2000;11:822-31. [DOI] [PubMed] [Google Scholar]
- 25.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767-73. [DOI] [PubMed] [Google Scholar]
- 26.Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, Mascioli SR, Scott JC, Seeley DG, Steiger P, Vogt T. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990;263:665-8. [PubMed] [Google Scholar]
- 27.Nevitt MC, Cummings SR, Browner WS, Seeley DG, Cauley JA, Vogt TM, Black DM. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992;135:490-9. [DOI] [PubMed] [Google Scholar]
- 28.Farmer ME, White LR, Brody JA, Bailey KR. Race and sex differences in hip fracture incidence. Am J Public Health. 1984;74:1374-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelsey JL, Browner WS, Seeley DG, Nevitt MC, Cummings SR. Risk factors for fractures of the distal forearm and proximal humerus. The Study of Osteoporotic Fractures Research Group. Am J Epidemiol. 1992;135:477-89. Erratum in: Am J Epidemiol. 1992;135:1183. [DOI] [PubMed] [Google Scholar]
- 30.Hagino H, Fujiwara S, Nakashima E, Nanjo Y, Teshima R. Case-control study of risk factors for fractures of the distal radius and proximal humerus among the Japanese population. Osteoporos Int. 2004;15:226-30. [DOI] [PubMed] [Google Scholar]
- 31.Lee SH, Dargent-Molina P, Bréart G; EPIDOS Group. Epidemiologie de l'Osteoporose Study. Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res. 2002;17:817-25. [DOI] [PubMed] [Google Scholar]
- 32.Nguyen TV, Center JR, Sambrook PN, Eisman JA. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Am J Epidemiol. 2001;153:587-95. [DOI] [PubMed] [Google Scholar]
- 33.Gibson JJ. The perception of the visual world. Boston: Houghton Mifflin; 1950.
- 34.Hosmer DW, Lemeshow S. Applied survival analysis: regression modeling of time to event data. New York: Wiley; 1999.
- 35.Schousboe JT, Fink HA, Lui LY, Taylor BC, Ensrud KE. Association between prior non-spine non-hip fractures or prevalent radiographic vertebral deformities known to be at least 10 years old and incident hip fracture. J Bone Miner Res. 2006;21:1557-64. [DOI] [PubMed] [Google Scholar]
- 36.Lauderdale DS, Thisted RA, Goldberg J. Is geographic variation in hip fracture rates related to current or former region of residence? Epidemiology. 1998;9:574-7. [PubMed] [Google Scholar]
- 37.Silverman SL, Watts NB, Delmas PD, Lange JL, Lindsay R. Effectiveness of bisphosphonates on nonvertebral and hip fractures in the first year of therapy: the risedronate and alendronate (REAL) cohort study. Osteoporos Int. 2007;18:25-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lind T, Krøner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108:285-7. [DOI] [PubMed] [Google Scholar]
- 39.Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int. 1993;52:192-8. [DOI] [PubMed] [Google Scholar]
- 40.Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, Vanoli A, Martin FC, Gosney MA. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49:664-72. [PubMed] [Google Scholar]
- 42.Ettinger B, Ray GT, Pressman AR, Gluck O. Limb fractures in elderly men as indicators of subsequent fracture risk. Arch Intern Med. 2003;163:2741-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.