Abstract
Purpose
To assess the comprehension of common medical terms used in prostate cancer in patient education materials to obtain informed consent, and to measure outcomes after prostate cancer treatment. We address this issue among underserved, African-American men because of the increased cancer incidence and mortality observed in this population.
Patients and Methods
We reviewed patient education materials and prostate-specific quality-of-life instruments to identify technical terms describing sexual, urinary, and bowel function. Understanding of these terms was assessed in face-to-face interviews of 105, mostly African-American men, age ≥ 40, from two low-income clinics. Comprehension was evaluated using semiqualitative methods coded by two independent investigators. Demographics were collected and literacy was measured.
Results
Fewer than 50% of patients understood the terms “erection” or “impotent.” Only 5% of patients understood the term “incontinence” and 25% understood the term “bowel habits.” More patients recognized word roots than related terms or compound words (eg, “rectum” v “rectal urgency,” “intercourse” v “vaginal intercourse”). Comprehension of terms from all domains was statistically significantly correlated with reading level (P < .001). Median literacy level was fourth to sixth grade. Prostate cancer knowledge was poor. Many patients had difficulty locating key anatomic structures.
Conclusion
Limited comprehension of prostate cancer terms and low literacy create barriers to obtaining informed consent for treatment and to measuring prostate cancer outcomes accurately in our study population. In addition, the level of prostate cancer knowledge was poor. These results highlight the need for prostate cancer education efforts and outcomes measurements that consider literacy and use nonmedical language.
INTRODUCTION
Prostate cancer is the most commonly diagnosed noncutaneous cancer in men in the United States and the second leading cause of cancer death. It is estimated that 186,320 men were diagnosed with prostate cancer in 2008 and 28,660 men will die of it.1 For reasons that are unclear, prostate cancer disproportionately affects African-American men, who suffer an approximately 1.7 times increased incidence and 2.4 times increased cancer mortality compared with white men.2
Despite these statistics, prostate cancer screening and treatment are highly controversial.3–5 Prostate cancer screening has not yet been shown to increase overall survival or decrease cancer-specific mortality.5,6 Moreover, any potential survival benefit must be weighed against the adverse effects of standard treatments including impotence, incontinence, and bowel symptoms.7–12
Research in the past 13 years has shown that the adverse effects of early prostate cancer treatment are both prevalent and long-term.12–16 One large national study reported 63.5% of men treated with external beam radiation and 79.3% treated with radical prostatectomy were impotent 5 years after treatment.16 Consequently, most major US and Canadian medical organizations recommend that clinicians should not screen patients for prostate cancer without discussing the uncertain benefits and possible harms of prostate cancer screening.5,6,17–20
Therefore, physician-patient communication is central to the process of prostate cancer screening and treatment. Medical terminology for urinary, bowel, and sexual function is often used to explain the tradeoffs involved in prostate cancer screening, to obtain informed consent, and in patient education materials.7–10,21–31 In addition, this terminology is used to measure quality of life (QOL) and outcomes after prostate cancer treatment.14,32–37 Because prostate cancer disproportionately affects African-American men, we conducted structured interviews to evaluate comprehension of standard medical terms used in prostate health in an underserved, predominantly African-American population.
PATIENTS AND METHODS
Design of the Study
The study was conducted in two low-income, general medical clinics: the University Medical Associates Clinic at University of Virginia and the Central Virginia Community Health Center in Buckingham County, VA. Patients were considered eligible if they were English-speaking men ≥ age 40 years, able to give informed consent, and were neither physicians nor registered nurses. After permission was obtained from the patients' physicians, eligible participants were recruited in person for the interview. Four participants were self-referred. We completed 107 interviews between August 2000 and May 2002. Two patients were found to be ineligible. Ten men refused to participate, for a refusal rate of 4.2% of men eligible to be interviewed. There were 119 men willing to participate who provided contact information, but had scheduling difficulties.
The institutional review board of the University of Virginia approved the study for use in both clinics. Written informed consent was obtained from each patient after the interviewer read aloud the consent form and answered any of the patient's questions. Interviews were administered face-to-face and read aloud. Patients were remunerated $20.00.
Data Collection and Analysis
The questionnaire was developed based on a review of patient education materials for prostate cancer screening and treatment,23,26,38,39 and seven prostate-specific health status questionnaires used to measure prostate-specific QOL.14,32–37 Technical terms were identified in each instrument describing sexual, urinary, and bowel function. Comprehension of these twenty-eight terms was assessed with a series of questions that generally took the form: 1) Is ____ a word that you know? If the respondent replied “yes”, two further questions were asked: 2) What are the other words that you've heard for ____? 3) What happens when a man has ____? The content and structure of these questions were developed with a medical anthropologist (G.F.) based on ethnographic field methods.40 Prostate cancer knowledge was assessed using questions previously validated in a large survey of Canadian men.41 To assess comprehension of key anatomic structures, patients were shown two male anatomic drawings using anterior and midsagittal views and asked their location and function. Reading level was assessed using the Rapid Estimate of Adult Literacy in Medicine.42 Patients were asked to cross out two thirds of nine, 30% of 10, and 30% of 100 using stick figures to assess numeracy. Participants were asked to self-describe race, provide age, address, household income, highest grade level completed in school, insurance type, and describe their living arrangement at home. Before the study, the interview was tested for acceptability, content, wording, and burden on respondents and was found to be satisfactory.
Two trained interviewers, one female and one male, and the principal investigator (a female) conducted the interviews. Patient responses were captured in detailed written forms. All interviews were audiotaped and a random sample of 10% of all audiotapes were reviewed and compared with the written data for quality control. Two independent trained coders determined comprehension of prostate-specific terms according to specified criteria. Those patients who responded “no” to the question, “Is ____ a word that you know?” were scored as not understanding the term. The two coders independently, and blinded to each other's initial assessment, determined whether participants who responded “yes” to the question correctly understood or misinterpreted the term, based on the participant's responses to subsequent and related questions. Scores were then unblinded and scoring disagreements were reviewed by the two coders in an effort to reach consensus. Continued disagreements were reviewed by a tie-breaking third independent coder. Initial inter-rater agreement was 91.9%; failure to reach consensus was 0.23%.
Statistical Analysis
Analyses were conducted with the SAS statistical software package (SAS Institute, Cary, NC). Questions that were skipped by patients were excluded from analyses. Standard methods based on the binomial distribution were used to calculate CIs. Pearson correlation coefficients were used to estimate the association between literacy and the proportion of correctly identified terms in each domain (sexual function, urinary function, and bowel function). CIs and tests for the correlation coefficients were computed using the Fisher z-transformation.43
Qualitative Analysis
The inductive framework of grounded theory was used with content analysis to examine recurring themes in the misunderstanding of prostate cancer.44–48 Detailed written interview notes were reviewed by three authors (E.M.N., K.L.K., G.F.) and used to develop initial coding categories. Two authors (E.M.N., K.L.K.) then independently coded each interview using both notes and audiotaped data to refine themes and aggregate the data into qualitative domains and subcategories within those domains. Coding between the two authors was compared every four to five interviews and disagreements reconciled to consensus based on data. The coding framework was updated iteratively. Representative quotations were transcribed from audiotapes.
RESULTS
Patients
Patient demographics and study characteristics are summarized in Table 1. Patients were on average 58 years old (range, 40 to 89). Most patients (75%) self-described their race as African American or black, but a few men (11%) described their race as negro or colored. Thirteen percent of patients described themselves as white. Most patients lived in a rural residence according to year 2000 census criteria.49 Median annual household income was $16,000. Just more than half the patients were uninsured or had Medicaid. Most patients (65%) had not completed high school and 26% did not receive more than a grammar school education. Only three patients had completed four years of college. Fewer than half the patients read above the sixth grade level and 27% were illiterate or read at third grade level or lower. Twenty percent of the men were able to calculate both a fraction and a percent. There were nine men who reported that they were prostate cancer survivors and three men who reported that they had undergone transurethral resection of the prostate (TURP).
Table 1.
Patient Demographics and Study Characteristics (N = 105)
| Characteristic | No. | % |
|---|---|---|
| Average age, years | 58 | |
| Self-described race | ||
| African American | 91 | 87 |
| White | 14 | 13 |
| Rural residence | 74 | 70 |
| Income | ||
| Median household | 16,000 | |
| Median per household member | 6,800 | |
| Insurance | ||
| Uninsured | 32 | 30 |
| Medicaid | 22 | 21 |
| Private | 31 | 30 |
| Medicare | 17 | 16 |
| Do not know | 3 | 3 |
| Highest education | ||
| ≤ 6th grade | 27 | 26 |
| Middle school | 11 | 10 |
| Some high school | 30 | 29 |
| High school graduate | 23 | 22 |
| Some college | 14 | 13 |
| Literacy | ||
| Illiterate | 9 | 9 |
| ≤ 3rd grade | 19 | 18 |
| 4th-6th grade | 18 | 17 |
| 7th-8th grade | 26 | 25 |
| High school | 24 | 23 |
| Skip or no glasses | 9 | 9 |
| Numeracy | ||
| Calculated fraction correctly | 41 | 39 |
| Calculated percent correctly* | 32 | 30 |
| Both fraction and percent calculated correctly | 21 | 20 |
| Prostate cancer or TURP survivor† | 12 | 11 |
Abbreviation: TURP, transurethral resection of the prostate.
Patient must calculate both 30% of 10 and 30% of 100 correctly.
Thirty-three percent illiterate or ≤ 3rd grade reading level, 8% can calculate both fraction and percent correctly.
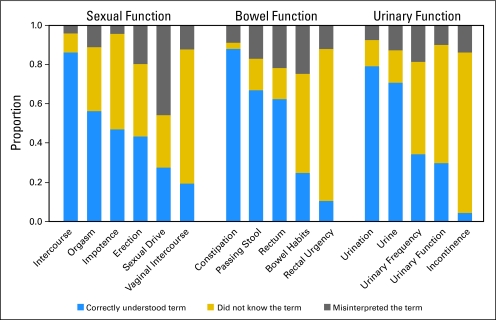
Prostate Cancer Terms
The understanding of prostate cancer terms among the men in our study population is described in Figure 1. In the domain of sexual function, the words “impotent” and “erection” were correctly understood by fewer than 50% of the men. Although “intercourse” was one of the best understood words in the interview, 68% of the men said they did not know the related compound term, “vaginal intercourse.” There were 65 patients (62%) who knew the word “rectum,” but only 23% said they knew the term “rectal urgency.” In the domain of urinary function, “urine” and “urination” were understood by 70% and 79% of men, respectively. Fewer than 50% of patients, however, correctly understood the derivative terms “urinary frequency” and “urinary function.” “Incontinence” was the least understood term in the interview; 95% of patients did not know the word or misinterpreted it. We found that understanding of terms in all three domains was correlated with literacy as measured by the Rapid Estimate of Adult Literacy in Medicine raw score (0 to 66, P < .001; Table 2).
Fig 1.
Comprehension of selected terms in the sexual, bowel, and urinary function domains by proportion of total study population (estimated with an SE that is no > 5 percentage points). Blue bars represent the proportion that correctly understood the term. Gold bars and gray bars represent the proportions that did not know the term and that misinterpreted the term, respectively.
Table 2.
Correlation Coefficients Between Literacy and the Proportion of Correctly Understood Terms in Each Domain
| Parameter | Domain |
||
|---|---|---|---|
| Sexual Function | Urinary | Bowel | |
| Literacy | 0.79 | 0.66 | 0.62 |
| 95% CI | 0.70 to 0.85 | 0.53 to 0.76 | 0.48 to 0.73 |
Anatomic Identification and Function
The ability to identify key anatomic structures and name their functions is presented in Table 3. The majority of men could not locate the prostate, 29% could not locate the bowels, and 35% could not locate the bladder. Most men could locate the penis. A few men who did not recognize the standard medical term when asked to “point to the penis” could still provide a correct colloquial name when asked “What do you call this?”
Table 3.
Anatomic Identification and Function
| Item | Correct Identification |
Correct Function (%) |
Correct Location (%) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rectum |
Term Other Than Rectum |
Penis |
Term Other Than Penis |
|||||||||
| All Men (N = 105) | 95% C | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | All Men (N = 105) | 95% CI | |
| Please point to the | ||||||||||||
| Bladder | 65 | 55 to 74 | 90 | 83 to 95 | ||||||||
| Bowels | 71* | 62 to 80 | 75 | 66 to 83 | ||||||||
| Prostate | 22 | 14 to 31 | 4 | 1 to 9 | ||||||||
| Penis | 84 | 75 to 90 | 89 | 81 to 94 | ||||||||
| Where would you feel rectal discomfort? | 46 | 36 to 56 | ||||||||||
| What do you call this? | ||||||||||||
| Rectum | 21 | 14 to 30 | 34 | 25 to 44 | 53 | 43 to 63 | ||||||
| Penis | 78 | 69 to 86 | 11 | 6 to 19 | 91 | 84 to 96 | ||||||
Not including 12% who pointed to the rectum.
Misunderstanding of the Prostate and Prostate Cancer
There were 91 men (87%) who had heard of the prostate, but only 62 (59%) could name something that goes wrong with it and just two men could describe the function of the prostate. Quantitative analysis demonstrated that overall prostate cancer knowledge was poor even among survivors of prostate cancer and TURP (Table 4). Only three men of 105 were able to name race as a risk factor. Further insight into patterns of misunderstanding was gained with qualitative analysis in which two broad themes emerged. The first major theme was “inability to distinguish the normal prostate from prostate cancer.” When asked “what does the prostate do?” one participant explained, “I guess it eats you up, I guess it's cancer.” Another patient, a prostate cancer survivor, replied, “it takes your nature [a colloquial term for sexual function] from you is one of the things it does. You have terrible pains from it too.” These data, combined with observations of the participants during the anatomic identification section of the interview, in which patients traced the rectum to locate the prostate, indicated that many patients understand the prostate only in the context of the physical exam used to screen for prostate cancer. Because knowledge of the prostate was acquired directly through the experience of digital rectal exam, 25% of interviewees thought the prostate was synonymous with prostate cancer, 17% thought that the prostate was located in the rectum, and 4% confused prostate cancer with colorectal cancer.
Table 4.
Prostate Cancer Knowledge
| Item | Correct |
Agree |
||||||
|---|---|---|---|---|---|---|---|---|
| All Men (N = 105) |
Cancer and TURP (n = 12) |
All Men (N = 105) |
Cancer and TURP (n = 12) |
|||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Chances of a man (African American) getting prostate cancer in his lifetime (1 in 5) | 17 | 10 to 26 | 17 | 0 to 38 | ||||
| Risk factors for prostate cancer | ||||||||
| Increasing age | 5 | 2 to 11 | 0 | 0 to 27 | ||||
| Family history | 2 | 0 to 7 | 0 | 0 to 27 | ||||
| Race | 3 | 1 to 8 | 8 | 0 to 38 | ||||
| Do not know | 42 | 32 to 52 | 42 | 15 to 72 | ||||
| Misinterpret | 51 | 41 to 61 | 50 | 21 to 79 | ||||
| Treatments for prostate cancer | ||||||||
| Surgery | 22 | 14 to 31 | 67 | 35 to 90 | ||||
| Radiation | 13 | 7 to 21 | 25 | 9 to 57 | ||||
| Brachytherapy | 2 | 0 to 7 | 8 | 0 to 38 | ||||
| Hormones | 4 | 1 to 9 | 25 | 9 to 57 | ||||
| Chemotherapy | 14 | 8 to 22 | 33 | 10 to 65 | ||||
| Adverse effects of prostate cancer treatment | ||||||||
| Sexual dysfunction | 7 | 3 to 13 | 25 | 9 to 57 | ||||
| Urinary dysfunction | 5 | 2 to 11 | 17 | 0 to 38 | ||||
| Bowel symptoms | 3 | 1 to 8 | 0 | 0 to 27 | ||||
| Hormone or chemotherapy adverse effects | 16 | 9 to 23 | 17 | 0 to 38 | ||||
| Most prostate cancer can be cured if it's caught early enough | 93 | 87 to 97 | 92 | 62 to 100 | ||||
| Most men who get prostate cancer will die of prostate cancer | 38 | 29 to 48 | 50 | 21 to 79 | ||||
| A man can have prostate cancer without pain or symptoms | 48 | 38 to 58 | 42 | 15 to 72 | ||||
| Most prostate cancer tumors are fast growing | 55 | 45 to 65 | 50 | 21 to 79 | ||||
| Compared to heart disease, do you know more, about the same, or less about prostate cancer? (knew less, %) | 55 | 45 to 65 | 50 | 21 to 79 | ||||
Abbreviation: TURP, transurethral resection of the prostate.
The second major theme to emerge in content analysis was “confusion of the urinary, bowel, and sexual function domains” used to discuss prostate cancer and measure QOL among survivors. Although assessment of these domains is an important objective of prostate cancer outcomes measurement,14,32–37 widespread domain confusion was evident among many patients. The misunderstandings illustrated in the following exchanges were prevalent and severe, raising the concern that lack of anatomic knowledge and unfamiliar medical terms render educational and informed consent materials, and current QOL instruments unreliable in our study population. Overall, 47% of patients confused bowel with urinary function, 32% confused urinary with sexual function, and 27% confused bowel with sexual function.
Question: What are the other words you've heard for urinary function?
Answer: Bowel movement.
Question: What does the rectum do?
Answer: …pee, urinatin' and all that stuff.
Question: What are the other words you've heard for bowel habits?
Answer: watchacall folks that, men using men, men going with men that's what I'm gettin' at.
Question: What happens when a man is incontinent?
Answer: …He's not able to satisfy his woman or to participate in satisfying his own self.
DISCUSSION
Historically, health literacy studies have placed an emphasis on reading skills and their relationship to clinical health outcomes.50–54 More recent studies have begun to consider mathematical skills and document complexity.55–62 The field of health literacy has long been aware that the language of medicine is distinct from spoken English used to communicate in life outside the hospital.63–66 Our study is not new in this regard. It is novel, however, for applying the ethnographic methodologies of cultural anthropology to examine in detail the assumptions about patient language, skills, and knowledge intrinsic to current QOL measures, cancer education, and informed consent interactions for prostate cancer.39 We were able to explore these assumptions among patients recruited from two low-income community clinics serving large populations of African-American men by acknowledging that doctors often use words that do not mean much to everyday people, reassuring participants that there are no right or wrong answers, and avoiding closed ended questions.
Our investigation revealed that widespread assumptions made in medical settings about the language for genitourinary function, reading skills, math skills, prostate cancer knowledge, and anatomic knowledge were inaccurate among patients in our study population. The greatest limitation of our research, however, is that we cannot say how generalizable our findings will be outside our small sample size from two clinics in a single geographic region. Nevertheless, our results are cause for concern. We found that the median reading level among men that we interviewed was fourth to sixth grade with 27% reading at third-grade level or lower. Only 20% could calculate a simple percent and fraction. We established that standard medical language for genitourinary function was not understood well. These terms are found in many patient education materials 18,21,25–30,67 and QOL questionnaires,14,32–37 and are likely to be used by physicians in discussions of prostate cancer screening and treatment.22–24,32 We assessed prostate cancer knowledge as well as anatomic function and location. Analysis showed that prostate cancer knowledge was poor even among patients who had undergone treatment for prostate cancer or TURP. Many patients had difficulty identifying key anatomic structures and their function. Most importantly, we found that many commonly used medical terms were completely unknown to a large proportion of patients and that comprehension was significantly correlated with health literacy. Much like a foreign language, our results showed that patients may understand a particular term relatively well, but may not recognize compound terms or related terms derived from the same word root (eg, intercourse v vaginal intercourse or rectum v rectal urgency, respectively). Similar results have been observed with difficulty understanding vaginal intercourse and anal intercourse in the National AIDS Behavioral Survey II.68
Because these assumptions about knowledge, skills, and language are made in consent documents,23,31 QOL measures,14,32–37 and patient education materials,18,21,25–30,67 it is doubtful their content is accessible to our study population. For instance, the Centers for Disease Control, the National Cancer Institute pamphlets,25,27 and the American Cancer Society (ACS) Web site67 all explain the adverse effects of early prostate cancer treatment in terms of impotence and incontinence, understood by fewer than 50% and 5% of study patients, respectively. When definitions are provided for these words, they are often couched in more medical terminology. Impotent is defined as “unable to have a spontaneous erection” on the ACS Web site,67 or discussed as “problems having or keeping an erection” in plain language materials,28,29 but neither impotent nor erection was understood by more than 50% of the patients we interviewed. Thus, even if these materials were read aloud to overcome literacy barriers, they may still be misunderstood by many men in our study. The math skills expected of the reader are also an issue. Both the ACS Web site67 and the Centers for Disease Control pamphlet25 use percentages, a calculation that only 30% of study patients could perform.
How can we apply our research findings to improve prostate cancer communication among underserved men? We can identify more accessible language for genitourinary function. Using the semiqualitative data culled from our research interviews, we have constructed a table of synonymous colloquial terms for the common medical words used for prostate cancer (Appendix Table A1, online only). We hope these findings will be useful to other investigators and caregivers as we apply these results in the next steps of our research plan. After confirming the social acceptability of alternative colloquial language, we have employed a process comparable to translation, and back translation of English to a foreign language, to adapt Patient-Oriented Prostate Utility Scale (PORPUS), a prostate-specific QOL measure.33,69 Current instruments are self-administered, require relatively high level reading skills, and use standard medical terms.14,32–37 Our adapted QOL instrument is a computerized, partially tailored script that is read aloud by an interviewer. The script begins by asking the patient to choose the words for urinary, bowel, and sexual function that he understands most easily. The interviewer selects these terms in the computer program, which automatically substitutes the chosen colloquial terms for the standard medical language validated in the original QOL measure. The program creates a partially tailored QOL instrument that can be read aloud by the interviewer. We will begin to test the adapted QOL measure among low-income prostate cancer survivors of all races shortly, with particular concern for underserved African-American men.
In addition, we urge caregivers not to assume that patients have a working knowledge of their internal anatomy and organ systems. A safer place to start teaching prostate cancer is based on what a patient sees in the mirror. We can explain anatomy step-wise, by teaching new structures in relation to external landmarks that every patient will know regardless of education. Similarly, we can explain function based on what a patient directly knows of his body from using the bathroom and having sexual relations. After identifying colloquial language that is more meaningful to the patient, it is important to begin teaching by anchoring our explanations in the common experiences of daily living—activities that every patient performs no matter how far they went in school. Lastly, we can use the qualitative analysis of misunderstandings of prostate cancer to inform subsequent explanations of prostate cancer screening in similar patient populations. Based on study data, we added a list of suggestions for caregivers to help clarify the digital rectal exam during prostate cancer screening using everyday language in an effort to prevent further misconceptions (Appendix).
Appendix
Clarification of the digital rectal exam to avoid misconceptions.
Every man starts out with a normal prostate gland that does not have cancer. However, a man's prostate can develop cancer as he gets older.
The normal prostate is involved in sex. It makes the fluid for sperm.
Even though that's where your doctor checks, the prostate is not located in the rectum and is not involved in bowel function. Your doctor feels the prostate through the wall of the rectum like a blind man reading Braille. If there is cancer in the prostate, the doctor may feel lumps or bumps.
Prostate cancer testing is different from colon cancer testing. The two cancers are different diseases.
The normal prostate gland is not directly involved in urinary or bowel function, but it is close neighbors with other structures that are—the bladder and the rectum. If the prostate develops cancer or the treatments for prostate cancer cause adverse effects, those neighboring organs can develop problems because they are so close to the prostate gland.
Note: Underlined medical terms may require further explanation or substitution with more familiar colloquial terms.
Table A1.
Table of Colloquial Expressions Synonymous to Common Medical Terms Used in Prostate Cancer
| Medical Term | |||||
|---|---|---|---|---|---|
| To Urinate | To Pass Stool or To Have a Bowel Movement | Rectum | Intercourse | Penis | Impotent |
| Colloquial synonym | |||||
| To make water | (To sit down) to go to the bathroom | Ass or asshole | Having sex | Peter | Won't get hard for sex |
| To pee | To shit | Butt or butt hole | Fucking | Dick | Can't get it up for sex |
| To take a leak | To do do | Tail or tail hole | Making love | Can't perform sex | |
| To piss | To go #2 | Rear or rear end | Screwing | ||
| To go to the bathroom | To take a dump | ||||
| To wet | To make solid waste | ||||
Note: Synonyms are derived from responses by participants who did not know or misinterpreted the medical term in the top row. Colloquial synonyms are listed in order from most commonly cited to least commonly cited. Underlining connotes terms determined to be socially acceptable in a medical setting through subsequent interviews in the same study population.
Footnotes
Supported by Grant No. DAMD17-00-1-0106 from the Congressionally Directed Medical Research Program in Prostate Cancer at the Department of Defense, Grant No. KO7CA085754 from the National Cancer Institute, and the Mellon Prostate Cancer Institute at the University of Virginia. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the Congressionally Directed Medical Research Program, the National Cancer Institute, the National Institutes of Health, or the Mellon Prostate Cancer Institute.
Presented in abstract format at the 37th and 42nd Annual Meetings American Society of Clinical Oncology, May 12-15, 2001, San Francisco, CA and June 2-6, 2006, Atlanta, GA.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Kerry L. Kilbridge, Gertrude Fraser, Murray Krahn, Elizabeth M. Nelson, Mark Conaway, Andrew Wolf, Debra Gong, Robert F. Nease, Alfred F. Connors
Financial support: Kerry L. Kilbridge, Alfred F. Connors
Administrative support: Kerry L. Kilbridge, Randall Bashore, Andrew Wolf, Michael J. Barry, Debra Gong, Alfred F. Connors
Provision of study materials or patients: Kerry L. Kilbridge, Randall Bashore, Andrew Wolf, Alfred F. Connors
Collection and assembly of data: Kerry L. Kilbridge, Murray Krahn, Elizabeth M. Nelson, Debra Gong, Alfred F. Connors
Data analysis and interpretation: Kerry L. Kilbridge, Gertrude Fraser, Murray Krahn, Elizabeth M. Nelson, Mark Conaway, Randall Bashore, Andrew Wolf, Michael J. Barry, Debra Gong, Robert F. Nease, Alfred F. Connors
Manuscript writing: Kerry L. Kilbridge, Gertrude Fraser, Murray Krahn, Mark Conaway, Randall Bashore, Andrew Wolf, Michael J. Barry, Debra Gong, Robert F. Nease, Alfred F. Connors
Final approval of manuscript: Kerry L. Kilbridge, Gertrude Fraser, Murray Krahn, Elizabeth M. Nelson, Mark Conaway, Randall Bashore, Andrew Wolf, Michael J. Barry, Debra Gong, Robert F. Nease, Alfred F. Connors
REFERENCES
- 1.Jemal A, Siegel R, Ward E, et al. Cancer Statistics, 2008. CA: Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA: Cancer Journal for Clinicians. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 3.Barry MJ. The PSA conundrum. Arch Intern Med. 2006;166:7–8. doi: 10.1001/archinte.166.1.7. [DOI] [PubMed] [Google Scholar]
- 4.Wilkinson S, Chodak G. Informed consent for prostate-specific antigen screening. Urology. 2003;61:2–4. doi: 10.1016/s0090-4295(02)02010-1. [DOI] [PubMed] [Google Scholar]
- 5.Wilt TJ, MacDonald R, Rutks I, et al. Systematic review: Comparative effectiveness and harms of treatments for clinically localized prostate cancer. Ann Intern Med. 2008;148:435–448. doi: 10.7326/0003-4819-148-6-200803180-00209. [DOI] [PubMed] [Google Scholar]
- 6.Harris R, Lohr KN. Screening for prostate cancer: An update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:917–929. doi: 10.7326/0003-4819-137-11-200212030-00014. [DOI] [PubMed] [Google Scholar]
- 7.Quek ML, Penson DF. Quality of life in patients with localized prostate cancer. Urologic Oncology. 2005;23:208–215. doi: 10.1016/j.urolonc.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Kattan MW, Cowen ME, Miles BJ. A decision analysis for treatment of clinically localized prostate cancer. J Gen Intern Med. 1997;12:299–305. doi: 10.1046/j.1525-1497.1997.012005299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krahn MD, Mahoney JE, Eckman MH, et al. Screening for prostate cancer: A decision analytic view. JAMA. 1994;272:773–780. [PubMed] [Google Scholar]
- 10.Fleming C, Wasson JH, Albertsen PC, et al. A decision analysis of alternative treatment strategies for clinically localized prostate cancer. JAMA. 1993;269:2650–2658. [PubMed] [Google Scholar]
- 11.Cantor SB, Spann SJ, Volk RJ, et al. Prostate cancer screening: A decision analysis. J Family Pract. 1995;41:33–41. [PubMed] [Google Scholar]
- 12.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 13.Litwin MS, Hays RD, Fink A, et al. Quality-of-life outcomes in men treated for localized prostate cancer. JAMA. 1995;273:129–135. doi: 10.1001/jama.273.2.129. [DOI] [PubMed] [Google Scholar]
- 14.Talcott JA, Rieker P, Clark JA, et al. Patient-reported symptoms after primary therapy for early prostate cancer: Results of a prospective cohort study. J Clin Oncol. 1998;16:275–283. doi: 10.1200/JCO.1998.16.1.275. [DOI] [PubMed] [Google Scholar]
- 15.Fowler FJ, Jr, Barry MJ, Lu-Yao G, et al. Effect of radical prostatectomy for prostate cancer on patient quality of life: Results from a Medicare survey. Urology. 1995;45:1007–1013. doi: 10.1016/s0090-4295(99)80122-8. discussion 1013-1015, 1995. [DOI] [PubMed] [Google Scholar]
- 16.Potosky AL, Davis WW, Hoffman RM, et al. Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: The prostate cancer outcomes study. J Natl Cancer Inst. 2004;96:1358–1367. doi: 10.1093/jnci/djh259. [DOI] [PubMed] [Google Scholar]
- 17.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006 CA. Cancer Journal for Clinicians. 2006;56:11–25. doi: 10.3322/canjclin.56.1.11. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Cancer Society. Understanding the Pros and Cons of Prostate Testing. 2008 http://www.cancer.ca/ccs/internet/standard/0,3182,3172_13271_1858613010_langId-en,00.html.
- 19.Carroll P, Coley C, McLeod D, et al. For the American Urological Association: Prostate-specific antigen best practice policy–part I: Early detection and diagnosis of prostate cancer. Urology. 2001;57:217–224. doi: 10.1016/s0090-4295(00)00993-6. [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Institute. Prostate Cancer: Screening, Health Professional Version, U.S. National Institute of Health. 2008 http://www.cancer.gov/cancertopics/pdq/screening/prostate/healthprofessional/allpages#Section_20.
- 21.National Cancer Institute. Prostate Cancer Treatment: Treatment Option Overview, Patient Version, U.S. National Institute of Health. 2008 http://www.cancer.gov/cancertopics/pdq/treatment/prostate/patient/allpages.
- 22.Saigal CS, Gornbein J, Nease R, et al. Predictors of utilities for health states in early stage prostate cancer. J Urol. 2001;166:942–946. [PubMed] [Google Scholar]
- 23.Wolf AM, Nasser JF, Wolf AM, et al. The impact of informed consent on patient interest in prostate-specific antigen screening. Arch Intern Med. 1996;156:1333–1336. [PubMed] [Google Scholar]
- 24.Chan EC, Sulmasy DP. What should men know about prostate-specific antigen screening before giving informed consent? Am J Med. 1998;105:266–274. doi: 10.1016/s0002-9343(98)00257-5. [DOI] [PubMed] [Google Scholar]
- 25.Cancer Screening. A decision guide for African Americans. Atlanta, GA: CDC publication 99-6792; 2007. [Google Scholar]
- 26.The PSA decision. What you need to know. Hanover, NH: Foundation for Informed Medical Decision Making; 2000. (videotape) [Google Scholar]
- 27.What you need to know about prostate cancer. National Cancer Institute; 2005. NIH publication 05-1576. [Google Scholar]
- 28.Holmes-Rovner M, Stableford S, Fagerlin A, et al. Evidence-based patient choice: A prostate cancer decision aid in plain language. BMC Med Inform Decis Mak. 2005;5:16–26. doi: 10.1186/1472-6947-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fagerlin A, Holmes-Rovner M, Rovner D, et al. Making the choice: Deciding what to do about early-stage prostate cancer. Lansing, MI: Michigan Cancer Consortium Prostate Cancer Action committee; 2004. [Google Scholar]
- 30.Fagerlin A, Rovner D, Stableford S, et al. Patient education materials about the treatment of early-stage prostate cancer: A critical review. Ann Intern Med. 2004;140:721–728. doi: 10.7326/0003-4819-140-9-200405040-00012. [DOI] [PubMed] [Google Scholar]
- 31.Taylor KL, Africano NL, Schwartz M, et al. Prostate cancer screening at National Cancer Institute comprehensive and clinical cancer centers. J Natl Cancer Inst. 2004;96:414–415. doi: 10.1093/jnci/djh073. [DOI] [PubMed] [Google Scholar]
- 32.Litwin M, Hays R, Fink A, et al. The UCLA prostate cancer index: Development, reliability, and validity of health-related quality of life measure. Med Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Ritvo P, Irvine J, Naglie G, et al. Reliability and validity of the PORPUS, a combined psychometric and utility-based quality-of-life instrument for prostate cancer. J Clin Epidemiol. 2005;58:466–474. doi: 10.1016/j.jclinepi.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Esper P, Mo F, Chodak G, et al. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate (FACT-P) instrument. Urology. 1997;50:920–928. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- 35.Potosky AL, Harlan LC, Stanford JL, et al. Prostate cancer practice patterns and quality of life: The Prostate Cancer Outcomes Study. J Natl Cancer Inst. 1999;91:1719–1724. doi: 10.1093/jnci/91.20.1719. [DOI] [PubMed] [Google Scholar]
- 36.Barry M, Fowler F, O'Leary M, et al. The American Urological Association symptom index for benign prostatic hyperplasia: The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 37.Wei JT, Dunn RL, Litwin MS, et al. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- 38.American Cancer Society. Managing Incontinence After Treatment for Prostate Cancer. American Cancer Society; 1998. Pamphlet 98-80-No. 4535-CC. [Google Scholar]
- 39.Questions and Answers About the Prostate-Specific Antigen (PSA) Test. Washington, DC: National Cancer Institute; 2000. http://cis.nci.nih.gov/fact/5_29.htm. [Google Scholar]
- 40.Spradley J. Asking Descriptive Questions, The Ethnographic Interview. Belmont, CA: Wadsworth Group; 1979. pp. 78–91. [Google Scholar]
- 41.Mercer SL, Goel V, Levy IG, et al. Prostate cancer screening in the midst of controversy: Canadian men's knowledge, beliefs, utilization and future intentions. Canadian Journal of Public Health. 1997;88:327–332. doi: 10.1007/BF03403900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davis T, Long S, Jackson R, et al. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 43.Rosner B. Fundamentals of Biostatistics. Boston, MA: PWS-Kent Publishing Company; 1990. [Google Scholar]
- 44.Krippendorf K. Content Analysis: An Introduction to Its Methodology. Beverly Hills, CA: Sage; 1980. [Google Scholar]
- 45.Morse JM. Critical Issues in Qualitative Research Methods. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 46.Rubin HJ, Rubin IS. Qualitative Interviewing: The Art of Hearing Data. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- 47.Strauss AL. Qualitative Analysis for Social Scientists. Cambridge, MA: Cambridge University Press; 1987. [Google Scholar]
- 48.Strauss AL, Corbin J. Basics of Qualitative Research. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 49.U.S. Census Bureau. Census 2000 Urban and Rural Classification. http://www.census.gov/geo/www/ua/ua_2k.html.
- 50.Health literacy. Report of the Council on Scientific Affairs: Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281:552–557. [PubMed] [Google Scholar]
- 51.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 52.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 53.Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 54.Berkman ND, DeWalt DA, Pignone MP, et al. ed Evidence Rep. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Literacy and Health Outcomes: Evidence Report / Technology Assessment No. 87. (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under contact # 290-02-0016) [Google Scholar]
- 55.Mosenthal PB, Kirsch IS. A new measure of assessing document complexity: The PMOSE/IKIRSCH document readability formula. J Adol Adult Lit. 1998;41:638–657. [Google Scholar]
- 56.Woloshin S, Schwartz LM, Welch HG. The effectiveness of a primer to help people understand risk: Two randomized trials in distinct populations. Ann Intern Med. 2007;146:256–265. doi: 10.7326/0003-4819-146-4-200702200-00004. [DOI] [PubMed] [Google Scholar]
- 57.Schwartz LM, Woloshin S, Welch HG. Can patients interpret health information? An assessment of the medical data interpretation test. Med Decis Making. 2005;25:290–300. doi: 10.1177/0272989X05276860. [DOI] [PubMed] [Google Scholar]
- 58.Schwartz LM, Woloshin S, Black WC, et al. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 59.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: Suggested best practices and future recommendations. Med Decis Making. 2007;27:696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 60.Lipkus IM, Klein WM, Rimer BK. Communicating breast cancer risks to women using different formats. Cancer Epidemiol Biomarkers Prev. 2001;10:895–898. [PubMed] [Google Scholar]
- 61.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention. Scientific and technical information simply put. Atlanta, GA: Office of Communication; 1999. [Google Scholar]
- 63.Ong LM, de Haes JC, Hoos AM, et al. Doctor-patient communication: A review of the literature. Soc Sci Med. 1995;40:903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 64.Hadlow J, Pitts M. The understanding of common health terms by doctors, nurses and patients. Soc Sci Med. 1991;32:193–196. doi: 10.1016/0277-9536(91)90059-l. [DOI] [PubMed] [Google Scholar]
- 65.Bourhis RY, Roth S, MacQueen G. Communication in the hospital setting: A survey of medical and everyday language use amongst patients, nurses and doctors. Soc Sci Med. 1989;28:339–346. doi: 10.1016/0277-9536(89)90035-x. [DOI] [PubMed] [Google Scholar]
- 66.Gibbs RD, Gibbs PH, Henrich J. Patient understanding of commonly used medical vocabulary. J Fam Pract. 1987;25:176–178. [PubMed] [Google Scholar]
- 67.American Cancer Society. Detailed Guide: Prostate Cancer Surgery. 2008 http://www.cancer.org/docroot/CRI/content/CRI_2_4_4X_Surgery_36.asp?sitearea=
- 68.Binson D, Catania J. Respondents' understanding of the words used in sexual behavior questions. Public Opin Q. 1998;62:190–208. [Google Scholar]
- 69.Krahn M, Ritvo P, Irvine J, et al. Patient and community preferences for outcomes in prostate cancer: Implications for clinical policy. Med Care. 2003;41:153–164. doi: 10.1097/00005650-200301000-00017. [DOI] [PubMed] [Google Scholar]