Abstract
Severe malaria is clinically similar other severe febrile illnesses. However, in endemic areas, parasitological confirmation of parasitemia is often unavailable or unreliable. False positive malaria microscopy is common. The most important consequence of treating only for malaria when no parasitemia exists is failure to address other life threatening conditions. Invasive bacterial infections are detected in up to a third of children with clinical features of severe malaria but a negative slide. Even among genuinely parasitized children, severe illness is not always due to malaria in endemic areas. We believe that routine use of parenteral antibiotics among children with a positive malaria slide and life-threatening disease is warranted because invasive bacterial infections are likely to be under-ascertained and are associated with increased mortality. Published data on co-morbidity with HIV infection and malnutrition are reviewed. A structured approach to assessment and care is essential, and is largely independent of underlying etiology.
INTRODUCTION
Malaria is one of the commonest causes of illness and death among children in sub-Saharan Africa. The Roll Back Malaria (RBM) partnership proposes to reduce by 75% the 2005 malaria burden by 2015.1 However, establishing the role of malaria in causing disease or death is not straightforward.2,3 Many of the effects of malaria on child health and survival are indirect;2 vital registration systems are often lacking; many childhood deaths occur without contact with medical services;4,5 data are often derived from verbal autopsy with poor specificity;6 health facility data reporting is incomplete and clinical diagnoses are often unconfirmed by laboratory tests.7 Consequently, empirical methods combining incidence, population and climate data are used to try and overcome these limitations.8 For clinicians working in endemic areas, a similar set of factors also limit the accurate diagnosis and treatment of individual severely ill children.
In this article, we aim to describe the problems associated with inaccurate diagnosis of malaria in the setting of frequent parasitemia and a high likelihood of other febrile diseases; to review existing data on three co-morbid conditions (invasive bacterial infection, HIV and malnutrition) on severe malaria in children and present further analyses of published data from Kilifi, Kenya on invasive bacterial infections.
SEARCH STRATEGY
We searched the literature primarily using Pubmed at http://www.ncbi.nlm.nih.gov/PubMed/. We initially searched for data on severe malaria among children in Africa, then studies elsewhere, in adults or non-severe malaria if these were relevant. All abstracts were read; if there was any doubt as to the relevance of the article then the complete article was sourced. Search phrases included, ‘malaria AND (misdiagnosis OR “mis-diagnosis” OR overdiagnosis OR “over-diagnosis”)’, ‘malaria AND (comorbidity OR “co-morbidity”)’, ‘malaria AND (bacteremia OR bacteremia OR sepsis OR septicemia OR septicemia OR meningitis OR pneumonia)’, ‘malaria AND (HIV OR AIDS OR “acquired immune deficiency syndrome” OR “human immunodeficiency virus”)’, ‘malaria AND (under-nutrition OR “under nutrition” OR “undernutrition” OR “mal-nutrition” OR malnutrition)’, Data on micronutrient deficiencies, helminth infections and the effects of malaria on the progression of HIV or malnutrition are not reviewed here.
For the purposes of this paper, over-diagnosis refers to diagnosis of malaria when no parasitemia exists. This may involve reaching the diagnosis despite reliable laboratory evidence of the absence of parasitemia, a false positive slide or an incorrect presumptive diagnosis of malaria without laboratory confirmation. Co-morbidity refers to the presence of one or more significant diseases in addition to malaria parasitemia.
THE PROBLEMS OF DIAGNOSIS
Severe malaria can be clinically indistinguishable from other common illnesses including pneumonia, meningitis and sepsis9-17 and in endemic areas, microscopy or other tests to confirm parasitemia are commonly unavailable or unreliable.18-23 At 10 Tanzanian hospitals, 39% of ‘positive’ malaria slides were false positives and at 17 Kenyan outpatient clinics, the positive predictive value of a ‘positive’ slide was only 22% (negative predictive value 93%) when compared to expert microscopy.19,24 Facilities to make diagnoses other than malaria are even less widespread.23 Microbiology facilities are rare, do not provide results within the first 48 hours when most deaths occur,25,26 are relatively insensitive and require quality control. Lack of confidence in laboratory services and the consequent ‘invisibility’ of other etiologies may lead clinicians to treat for malaria when the slide is negative, and not to investigate or treat other causes.7,19,21,24,27
The second problem is that severe illness in genuinely parasitaemic children is not always due to malaria. In endemic areas, as many as 80% of children in the community may be parasitaemic.28,29 An autopsy study of 31 Malawian children with positive microscopy who fulfilled WHO criteria for cerebral malaria revealed that 23% of deaths were from other causes.30 In Kenya, the cerebrospinal fluid of 9% of 49 children with WHO defined cerebral malaria revealed Herpes simplex type 1 infection.31
Although definitions of severe malaria based on attributable fraction by parasite density can be constructed,32 they apply to populations and only provide a measure of probability of malaria in individual children. Fundoscopy findings specific to cerebral malaria are described, 30,33,34 however these are unlikely to be reproducible by non-specialists outside a research setting and do not exclude significant co-morbidity.
OVER-DIAGNOSIS OF SEVERE MALARIA
The main consequence of over-diagnosis is failure to treat over causes of life-threatening disease. In a recent Tanzanian study of 4,474 severely ill patients at 10 hospitals, 54% had a negative malaria slide.7 Two thirds of slide negative patients were not treated with antibiotics, and a greater proportion of these individuals died (12%) compared to those with a positive slide (7%). The research group further reported that with the exception of children under 5 years in the highest transmission regions, most patients treated for malaria in North Eastern Tanzania had no evidence of parasitemia.19 Similarly, in Ghanaian and Nigerian studies, higher mortality was again observed among the slide negative patients.14,37 Significant over-diagnosis has also been reported amongst adults with a clinical diagnosis of cerebral malaria.21,35
Some insight into the causes of severe illness among slide negative children comes from studies in Kenya and Ghana: among Ghanaian children with signs of severe malaria, 40% of slide negative children were bacteremic36 and in Kenya, 30% children with a negative malaria slide and impaired consciousness or meningism had confirmed invasive bacterial infection.13 Although the difficulty in distinguishing bacterial sepsis and malaria is likely to be greatest among less experienced health workers working in poorly resourced settings, the Malawian data30 suggest that even with stringent application of the WHO clinical definitions by an experienced research group, mis-diagnosis is common.
There are less data on respiratory distress arising from metabolic acidosis, the other principal manifestation of severe malaria, which is common in other diseases.38 However, there is overlap in clinical features with pneumonia9,15 and community based programs are utilizing dual treatment where children meet criteria for both conditions. 15
The use of rapid diagnostic tests (RDTs) may be an alternative to microscopy and further studies are needed to determine their clinical and cost effectiveness.39,40 However, in a recent trial, clinicians prescribed antimalarials only in patients with a negative test as often with RDTs as with microscopy.41 The underlying problem appears to be that clinicians are often unsure of what to do when clinical features are compatible with malaria, but the malaria diagnostic test (one of the few tests often available) is negative.
The high case fatality (usually >10%)7,13,14 of severely ill children in this context should be reflected in approaches to management, especially the strategy for assessing and treating severely ill children with a negative or unknown malaria slide. The principal, treatable cause of severe illness among children with clinical features of severe malaria who are not parasitaemic is invasive bacterial infection. As with malaria, most deaths from invasive bacterial infection occur soon after admission,12,42 making effective initial supportive care vital.20 A structured approach to supportive treatment for any severely ill child including management of airway, breathing, circulation, shock, seizures, hypoxemia, severe anemia or hypoglycemia is essential (Box). Such an approach is the cornerstone of the early management of severe malaria and should not differ in other conditions, even when the etiology is unknown.
Box: Structured approach to the management of severely ill children with clinical features compatible with severe malaria (impaired consciousness, deep (acidotic) breathing or severe anemia).
Syndromes and their management are defined by the current WHO referral care guidelines.13,43 Children may meet criteria for more and one syndrome.
Does this child need immediate intervention including cardiopulmonary resuscitation (airway, breathing or circulation), oxygen, fluid resuscitation, urgent blood transfusion, glucose, or anticonvulsants?
Is this child severely malnourished? Fluid resuscitation and blood transfusion regimes differ in severe malnutrition. WHO recommends antibiotics, micronutrients and nutritional support for children with severe malnutrition, even if treatments for malaria or other conditions are being given.
Does this child have HIV infection? Antibiotic choices, and investigation or treatment for opportunistic infection may depend on HIV status. Offer diagnostic testing and counseling (DTC).
Does this child meet criteria for a clinical syndrome that indicates antibiotic treatment? The types of antibiotic and route of administration (oral vs. parenteral) will depend on the clinical syndrome—treat the most severe classification. Antibiotics should be started at admission.
Does this child have a clinical syndrome indicating antimalarial treatment? The need for antimalarials will depend on a history of fever (presumptive treatment in the absence of available microscopy in an endemic area) or having reliable microscopy. The type of drug and route of administration will depend on recognizing signs of severity.
Does this child have another obvious clinical diagnosis?
Does this child need a lumbar puncture?
What maintenance oxygen, fluids, glucose, anticonvulsants or other drugs are needed?
What level of observation or monitoring does this child need and when should this child be reviewed?
In seriously ill children with negative parasitological tests, parenteral antibiotics are essential. The choice of antibiotic should be guided by the clinical syndromes present (e.g. meningitis, pneumonia, severe malnutrition etc)13,43 and any tests that may be available. Where no specific syndrome is present in a severely ill child, the recommended combination of ampicillin and gentamicin to treat septicemia43 is supported by available data.44 Patterns of bacterial isolates and antimicrobial sensitivities may vary locally, however we advise caution in deviating from established guidelines unless there is proper quality control of the microbiology laboratory, ideally externally. The practice of starting antibiotics only if there is no response to antimalarial treatment is inappropriate because most deaths occur within the first 48 hours of admission 42.
SEVERE MALARIA AND INVASIVE BACTERIAL INFECTIONS
There have been several case series of bacteremia or meningitis among children with malaria.11,12,45-52 The key clinical question is: do children with severe malaria and confirmed parasitemia need to be treated presumptively with antibiotics? Dual treatment is commonly done, but is a controversial issue. No relevant randomized trials have been conducted.
Among 276 Gambian children with cerebral malaria at a referral hospital reported 14 (5%) to be bacteraemic,48 13 survived without antibiotic treatment. In Malawi, 4.6% of 1,388 children with severe malaria were bacteremic, without a statistically significant effect on outcome.53 Both studies concluded that routine, presumptive antibiotic treatment was not warranted on the basis of their data.
In a retrospective study of children admitted to Kilifi District Hospital, Kenya between 1993 and 1996, we reported that bacteraemia was associated with a greatly increased risk of death among children with severe malaria (33% vs. 10.4%, p<0.001)12. We subsequently conducted a prospective study of invasive bacterial infections (bacteraemia or meningitis) in relation to malaria between 1999 and 2001 among unselected admissions.42 Data on inpatient case fatality in relation to invasive bacterial infections with and without severe malaria were not presented in the original report, and this analysis is presented here.13 The methods have been previously described in detail.13 In this study of 11,847 acute paediatric admissions, 10,580 were age ≥60 days. Of these, 3,493 (33%) had signs of severe malaria (fever plus one or more of coma (Blantyre Coma Score ≤2), respiratory distress or hemoglobin <5 g/dl), and 1,516 (43%) of these had a positive malaria slide (14% of admissions).
Among those with a positive slide and signs of severe malaria, invasive bacterial infection was strongly associated with death (table 1) despite routine antibiotics, remarkably similar to our earlier findings.46 We speculated that our findings may be biased by the inclusion of children with evidence of concurrent conditions such as malnutrition, meningitis or lower respiratory tract infection. We therefore re-analysed our data from children with signs of severe malaria and a positive malaria slide, first excluding children with severe malnutrition and then excluding children with CSF evidence of meningitis and children meeting WHO clinical criteria for severe or very severe pneumonia (which include respiratory distress).43 We found a similar prevalence of invasive bacterial infection to the Gambian and Malawian studies, however there remained a strong association with mortality (Table).
Table. Prevalence and outcome of invasive bacterial infection among 3,493 children age ≥60 days consecutively admitted to Kilifi District Hospital with coma, respiratory distress or hemoglobin <5 g/dl.
| N | N (%) with detected invasive bacterial infection. | Case fatality with invasive bacterial infection | Case fatality without invasive bacterial infection | Odds ratio adjusted for age (95% CI) | |
|---|---|---|---|---|---|
| Malaria slide negative | 1,977 | 238 (12%) | 77/238 (32%) | 121/1,739 (7.0%) | 6.32 (4.54 to 8.78) |
| Malaria slide positive | 1,516 | 83 (5.5%) | 27/83 (33%) | 110/1,433 (7.7%) | 5.91 (3.58 to 9.75) |
| Malaria slide positive excluding children with severe malnutrition* | 1,154 | 45 (3.9%) | 11/45 (24%) | 70/1,109 (6.3%) | 4.91 (2.38 to 10.2) |
| Malaria slide positive excluding children with CSF evidence of meningitis† or meeting WHO criteria for pneumonia.‡ | 705 | 31 (4.4%) | 10/31 (32%) | 36/674 (5.3%) | 8.94 (3.88 to 20.6) |
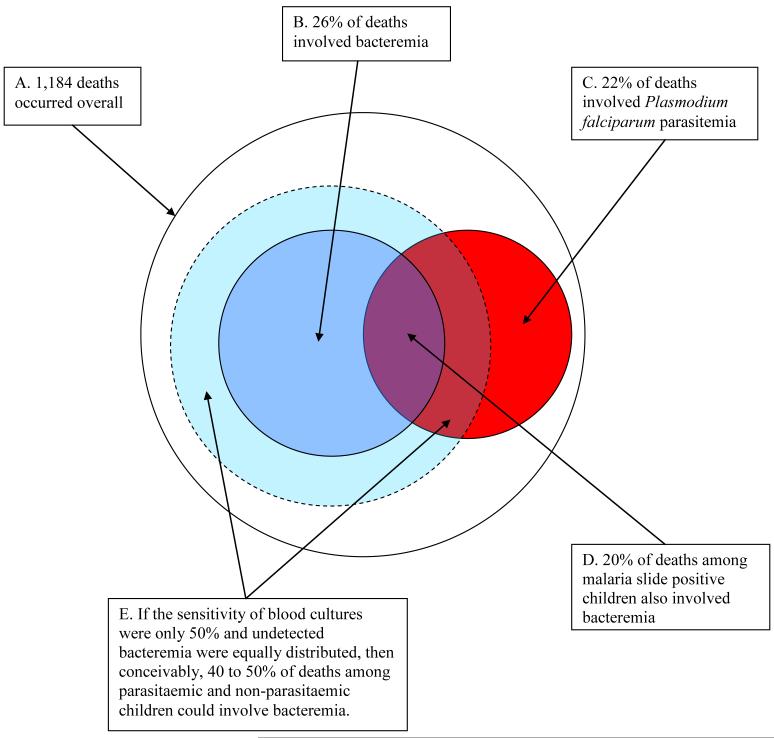
Blood culture is a very specific investigation but the sensitivity of a single culture sample can only be estimated indirectly since there is not an adequate ‘gold standard’. Partial antibiotic treatment, low-density bacteremia, low volume cultures and technical factors can result in failure to culture an organism. The sensitivity of blood cultures among Kenyan children was almost one third lower for cultured samples of 1 ml compared to those of 3 ml.42 In a large series of children with carefully defined clinical sepsis in Latin America, only 26% had positive bacterial cultures. 54 There was no difference in mortality between culture positive and negative children. Amongst Gambian children with lobar pneumonia, an organism was isolated in 52% but blood cultures were positive in only 18%.55 In the figure, we show the proportions of all deaths and malaria slide positive deaths that involved bacteremia in a study of more than 16,000 consecutive admissions.42 Superimposed are the estimated proportions of deaths involving bacteremia if blood culture were 50% sensitive (in practice sensitivity is likely to be even lower).
Figure. Malaria and invasive bacterial infection among 1,184 inpatient childhood deaths age 0 to 13 years at a rural district hospital in Kenya 1998-2002 and the potential effect of low blood culture sensitivity (source data: Berkley 2005).42.
A further consideration is that results of studies at referral centers may differ because deaths from bacterial sepsis occur rapidly, before referral. For all these reasons, it is conceivable that involvement of bacterial sepsis among severely ill children with a positive malaria slide is commoner than has been identified from existing blood culture studies. We believe that routine treatment with parenteral antibiotics is warranted because of an association with mortality and the uncertainty that malaria parasitemia is the sole cause of illness, especially so where false positive malaria microscopy may occur.
Where blood and CSF culture are not available, treating with parenteral antibiotics until the child is no longer severely ill then completing a short (5 day) antibiotic course is a practical approach, with relatively low risk of promoting antibiotic resistance. Although not evaluated by prospective studies in this context, short course treatment for pneumonia does appear to be as effective as longer courses (reviewed by Qazi).56 Lumbar puncture is reported to be infrequently undertaken among children in East African hospitals18,19 but is essential for detecting meningitis which cannot be reliably distinguished from cerebral malaria clinically.10,46,57,58 Most cases of meningitis can be identified from simple tests of CSF: inspection of turbidity, leukocyte count by microscopy and CSF: blood glucose ratio.59
SEVERE MALARIA AND HIV
More than 90% of the 3 million HIV-1-infected children worldwide live in sub-Saharan Africa.60,61 The widespread co-existence of HIV and malaria makes any interaction of considerable public health importance.62-64 Whilst data from adults suggest a clear association between declining CD4 counts and malaria attacks, 62,65-68 current data from children in malaria endemic areas are so far limited and inconclusive.62
Early data from Kinshasa suggested the incidence of malaria (odds ratio 2.1) and parasite density were (non-significantly) higher among children with AIDS than uninfected children.69 However, the overall incidence of fever was higher suggesting that some of the effect could be due to detection of co-incidental parasitemia. Conversely, in Kampala, HIV uninfected infants more commonly had a positive malaria slide (risk ratio 1.6) and no difference in febrile episodes between HIV infected and uninfected infants70 The authors hypothesized a protective effect of HIV and/or chloroquine use. In Dar es Salaam, lower parasite prevalence was found in HIV infected children participating in a vitamin A trial (prevalence ratio 0.56), but cotrimoxazole use was not examined.71
More recent data suggest some association with severity. In Kwa-Zulu Natal, an area of unstable malaria transmission, severe disease was associated with HIV (odds ratio, 3.0) among children presenting to hospital with malaria.72 The duration and pattern of symptoms, and parasite densities were similar. There were too few deaths to examine effects on mortality and co-morbidity with invasive bacterial disease was not examined. Among Malawian children with severe malaria and Kenyan children with acute malaria, HIV was associated with increased severe anemia but again there was no association with parasite density or death.53,73 It may be that effects of HIV are limited among children who have not yet acquired immunity to malaria. There is an urgent need for detailed epidemiological, clinical and immunological studies in children.
Cotrimoxazole prophylaxis is highly effective in preventing malaria. Cotrimoxazole prophylaxis resulted in an incidence rate ratio for malaria of 0.28 among Ugandan adults,74 and a protective efficacy of 99.5% among HIV-uninfected Malian children.75 However, there are no published data on the effects of cotrimoxazole or antiretroviral treatment on malaria among HIV-infected children. There is some evidence from adults of an increased risk of clinical treatment failure, mainly due to new infections rather than to recrudescence (hazard ratio 3.28).76 There was no increased risk of treatment failure among 1,802 HIV infected children.
On the basis of the current data, the clinical approach to HIV infected children with severe malaria should be that outlined above. The need for investigation and treatment for other causes of severe illness such as bacterial and opportunistic infections is likely to be greater among HIV infected children. Admission with severe malaria is a valuable opportunity for diagnostic testing and counseling (DTC).
SEVERE MALARIA AND MALNUTRITION
Malnutrition is thought to contribute to 53% of under-fives mortality in the developing world.77 The global distribution of malnutrition overlaps with that of malaria. The relationship between malnutrition and malaria is unclear. Under nutrition is widely believed to be protective for malaria, 78-80 largely from hospital rather than community-based studies and no single study has convincingly refuted this view.
Caulfield et al. have applied risk data from two cohort studies in Gambia81 and Vanuatu82 to the global distribution of malnutrition.83,84 The studies yielded a non-significant pooled risk estimate for clinical malaria of 1.31for underweight. However, the Vanuatu study, which contributed most cases, principally reported the effect on malnutrition after P. vivax infection, making the direction of association unclear. For the malaria mortality risk associated with underweight, Caulfield et al. examined data from studies in Ghana, Guinea Bissau and Senegal.85-88 They found statistically significant pooled relative risks for death from malaria of 9.49, 4.48 and 2.12 for children with weight for age z-scores of <-3, -3 to -1 and -1 to -2 compared with a z score of > -1.
Two recent cross sectional surveys89,90 have reported stunting to be associated with clinical malaria (odds ratio 1.77 89 and incidence rate ratio 1.9190). Additionally, a cohort study in Gambia reported a relative risk for malaria episodes of 1.35 for stunting.91 However, clinical malaria (i.e. fever) was mainly diagnosed by verbal autopsy and not confirmed by microscopy. In none of these studies were microbiological investigations performed to exclude bacterial infection.
Among hospital admissions in the Gambia, there was a clear association between low weight for age and mortality: 92 Case fatality among children at <-4 z scores was 20% compared to 6.8% at >-2 z scores. Data from Nigeria93 and other African data reviewed by Rice et al.94 support these findings and suggest a convincing relationship between nutritional status and the outcome of malaria in hospitalized children.
Malnutrition is commonly under-diagnosed by health workers, especially if focused on another disease process.95,96 Measuring weight and height and looking up a Z score or percentile on tables is cumbersome and error prone, especially among severely ill children. Simpler methods such as mid-upper arm circumference (MUAC) are probably more appropriate.96,97
There are few data on clinical features, optimal management among children with severe malaria and malnutrition. Altered fluid homeostasis may influence the pathophysiology of acidosis and make safe fluid resuscitation difficult.43 When intravenous fluids are given, severely malnourished children should be monitored closely with frequent observation as suggested in the WHO referral care guidelines.43 Replacement of electrolytes and micronutrients such as potassium and zinc are an essential component of management of hospitalized malnourished children, despite not being specifically indicated for severe malaria.43,98 Children with severe malnutrition are susceptible to invasive bacterial infections13 and severe malnutrition should itself be regarded as a syndromic indication for parenteral antibiotics in a seriously ill, febrile child. Further clinical studies of management of undernourished children with malaria, especially of glucose, fluid replacement and bacterial infections, are awaited.
CONCLUSIONS
Malaria is frequently over-diagnosed and results in failure to treat other life-threatening conditions, invasive bacterial infection being the most commonly identified. Importantly, there are worryingly few data on the relationships and consequences of HIV or malnutrition among children with severe malaria. Survival in severely ill children with or without malaria depends on structured, early assessment and supportive management with resuscitation, oxygen, fluids, blood, glucose and anticonvulsants (Box). These are largely independent of underlying etiology. We have previously proposed that decisions regarding antibiotic and antimalarial treatment among severely ill children should be made entirely separately, according to the clinical syndromes present, the available laboratory resources and knowledge of local epidemiology.13 The approach outlined will be familiar to practitioners in the United States and Europe where highly structured approaches to managing the critically ill child have evolved from clinical research over the last 15 years. Examples include the modern approaches to management of meningococcal sepsis or resuscitation procedures. Several recent studies of paediatric practice in East Africa demonstrate that such structured assessment and treatment are rarely used in this setting.7,18,19 Further research and the development of guidelines and training programs should therefore reflect these approaches in the context of a high case fatality of severely ill children in this setting and the likely uncertainty of the causes of disease.
ACKNOWLEDGEMENTS
We thank the clinical and nursing staff of Kilifi District Hospital and the KEMRI-Wellcome Trust Programme for their support. This paper is published with the permission of the director of KEMRI.
FUNDING
This study was supported by the Wellcome Trust, UK. Dr Berkley was a Wellcome Trust Training Fellow in Clinical Tropical Medicine (053439) and Prof Newton is a Wellcome Trust Senior Clinical Fellow (070114).
Footnotes
CONFLICT OF INTEREST
All authors declare no conflict of interest.
Contributor Information
SAMSON GWER, Centre for Geographic Medicine Research (coast), Kenya Medical Research Institute, PO Box 230, Kilifi 80108, Kenya, Tel.: +254 415 22063, Fax: +254 415 22390.
CHARLES RJC NEWTON, Prof, Centre for Geographic Medicine Research (coast), Kenya Medical Research Institute, PO Box 230, Kilifi 80108, Kenya, Tel.: +254 415 22063, Fax: +254 415 22390 & Neurosciences Unit, Institute of Child Health, London, WC1N 2AP, UK.
JAMES A BERKLEY, Dr, Centre for Geographic Medicine Research (coast), Kenya Medical Research Institute, PO Box 230, Kilifi 80108, Kenya, Tel.: +254 415 22063, Fax: +254 415 22390 & Centre for Clinical Vaccinology and Tropical Medicine, University of Oxford, Churchill Hospital, Oxford, OX3 7LJ, UK.
REFERENCES
- 1.RBM . Global Strategic Plan: Roll Back Malaria 2005-2015. Geneva: Roll Back Malaria Partnership, World Health Organization; 2005. [Google Scholar]
- 2.Breman JG. The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001;64:1–11. doi: 10.4269/ajtmh.2001.64.1. [DOI] [PubMed] [Google Scholar]
- 3.Snow RW, Craig M, Deichmann U, Marsh K. Estimating mortality, morbidity and disability due to malaria among Africa’s non-pregnant population. Bull World Health Organ. 1999;77:624–40. [PMC free article] [PubMed] [Google Scholar]
- 4.Mung’ala VO, Snow RW. Death registration on the Kenyan Coast. East Afr Med J. 1994;71:747–50. [PubMed] [Google Scholar]
- 5.Greenwood BM, Bradley AK, Greenwood AM, Byass P, Jammeh K, Marsh K, Tulloch S, Oldfield FS, Hayes R. Mortality and morbidity from malaria among children in a rural area of The Gambia, West Africa. Trans R Soc Trop Med Hyg. 1987;81:478–86. doi: 10.1016/0035-9203(87)90170-2. [DOI] [PubMed] [Google Scholar]
- 6.Snow RW, Armstrong JR, Forster D, Winstanley MT, Marsh VM, Newton CR, Waruiru C, Mwangi I, Winstanley PA, Marsh K. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet. 1992;340:351–5. doi: 10.1016/0140-6736(92)91414-4. [DOI] [PubMed] [Google Scholar]
- 7.Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O, Saganda K, Shao J, Kitua A, Olomi R, Greenwood BM, Whitty CJ. Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. Bmj. 2004;329:1212. doi: 10.1136/bmj.38251.658229.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005;434:214–7. doi: 10.1038/nature03342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.English M, Punt J, Mwangi I, McHugh K, Marsh K. Clinical overlap between malaria and severe pneumonia in Africa children in hospital. Trans R Soc Trop Med Hyg. 1996;90:658–62. doi: 10.1016/s0035-9203(96)90423-x. [DOI] [PubMed] [Google Scholar]
- 10.Molyneux E, Walsh A, Phiri A, Molyneux M. Acute bacterial meningitis in children admitted to the Queen Elizabeth Central Hospital, Blantyre, Malawi in 1996-97. Trop Med Int Health. 1998;3:610–8. doi: 10.1046/j.1365-3156.1998.00278.x. [DOI] [PubMed] [Google Scholar]
- 11.Akpede GO, Sykes RM. Malaria with bacteraemia in acutely febrile preschool children without localizing signs: coincidence or association/complication? J Trop Med Hyg. 1993;96:146–50. [PubMed] [Google Scholar]
- 12.Berkley J, Mwarumba S, Bramham K, Lowe B, Marsh K. Bacteraemia complicating severe malaria in children. Trans R Soc Trop Med Hyg. 1999;93:283–6. doi: 10.1016/s0035-9203(99)90024-x. [DOI] [PubMed] [Google Scholar]
- 13.Berkley JA, Maitland K, Mwangi I, Ngetsa C, Mwarumba S, Lowe BS, Newton CR, Marsh K, Scott JA, English M. Use of clinical syndromes to target antibiotic prescribing in seriously ill children in malaria endemic area: observational study. Bmj. 2005;330:995. doi: 10.1136/bmj.38408.471991.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evans JA, Adusei A, Timmann C, May J, Mack D, Agbenyega T, Horstmann RD, Frimpong E. High mortality of infant bacteraemia clinically indistinguishable from severe malaria. Qjm. 2004;97:591–7. doi: 10.1093/qjmed/hch093. [DOI] [PubMed] [Google Scholar]
- 15.Kallander K, Nsungwa-Sabiiti J, Peterson S. Symptom overlap for malaria and pneumonia--policy implications for home management strategies. Acta Trop. 2004;90:211–4. doi: 10.1016/j.actatropica.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 16.English M, Berkley J, Mwangi I, Mohammed S, Ahmed M, Osier F, Muturi N, Ogutu B, Marsh K, Newton CR. Hypothetical performance of syndrome-based management of acute paediatric admissions of children aged more than 60 days in a Kenyan district hospital. Bull World Health Organ. 2003;81:166–73. [PMC free article] [PubMed] [Google Scholar]
- 17.Jakka SR, Veena S, Atmakuri RM, Eisenhut M. Characteristic abnormalities in cerebrospinal fluid biochemistry in children with cerebral malaria compared to viral encephalitis. Cerebrospinal Fluid Res. 2006;3:8. doi: 10.1186/1743-8454-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.English M, Esamai F, Wasunna A, Were F, Ogutu B, Wamae A, Snow RW, Peshu N. Assessment of inpatient paediatric care in first referral level hospitals in 13 districts in Kenya. Lancet. 2004;363:1948–53. doi: 10.1016/S0140-6736(04)16408-8. [DOI] [PubMed] [Google Scholar]
- 19.Reyburn H, Mwangi R, Mwakasungula E, Chonya S, Mtei F. Assessment of paediatric care in district and Regional hospitals in Tanga and Kilimanjaro Regions, North East Tanzania. 2006. http://www.lshtm.ac.uk/malaria/MC%20website/Assessment%20of%20paediatric%20inpatient%20care%20in%20Tanzania.pdf.
- 20.Nolan T, Angos P, Cunha AJ, Muhe L, Qazi S, Simoes EA, Tamburlini G, Weber M, Pierce NF. Quality of hospital care for seriously ill children in less-developed countries. Lancet. 2001;357:106–10. doi: 10.1016/S0140-6736(00)03542-X. [DOI] [PubMed] [Google Scholar]
- 21.Makani J, Matuja W, Liyombo E, Snow RW, Marsh K, Warrell DA. Admission diagnosis of cerebral malaria in adults in an endemic area of Tanzania: implications and clinical description. Qjm. 2003;96:355–62. doi: 10.1093/qjmed/hcg059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oster N, Krause E, Hatz C. Towards a rational malaria management at district hospital level: exploratory case series of febrile adult patients in a holoendemic area of Tanzania. Trop Doct. 2000;30:203–7. doi: 10.1177/004947550003000407. [DOI] [PubMed] [Google Scholar]
- 23.Petti CA, Polage CR, Quinn TC, Ronald AR, Sande MA. Laboratory medicine in Africa: a barrier to effective health care. Clin Infect Dis. 2006;42:377–82. doi: 10.1086/499363. [DOI] [PubMed] [Google Scholar]
- 24.Zurovac D, Midia B, Ochola SA, English M, Snow RW. Microscopy and outpatient malaria case management among older children and adults in Kenya. Trop Med Int Health. 2006;11:432–40. doi: 10.1111/j.1365-3156.2006.01587.x. [DOI] [PubMed] [Google Scholar]
- 25.Berkley JA, Ross A, Mwangi I, Osier FH, Mohammed M, Shebbe M, Lowe BS, Marsh K, Newton CR. Prognostic indicators of early and late death in children admitted to district hospital in Kenya: cohort study. Bmj. 2003;326:361. doi: 10.1136/bmj.326.7385.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marsh K, Forster D, Waruiru C, Mwangi I, Winstanley M, Marsh V, Newton C, Winstanley P, Warn P, Peshu N, et al. Indicators of life-threatening malaria in African children. N Engl J Med. 1995;332:1399–404. doi: 10.1056/NEJM199505253322102. [DOI] [PubMed] [Google Scholar]
- 27.Barat L, Chipipa J, Kolczak M, Sukwa T. Does the availability of blood slide microscopy for malaria at health centers improve the management of persons with fever in Zambia? Am J Trop Med Hyg. 1999;60:1024–30. doi: 10.4269/ajtmh.1999.60.1024. [DOI] [PubMed] [Google Scholar]
- 28.Bodker R, Msangeni HA, Kisinza W, Lindsay SW. Relationship between the intensity of exposure to malaria parasites and infection in the Usambara Mountains, Tanzania. Am J Trop Med Hyg. 2006;74:716–23. [PubMed] [Google Scholar]
- 29.Ehrhardt S, Burchard GD, Mantel C, Cramer JP, Kaiser S, Kubo M, Otchwemah RN, Bienzle U, Mockenhaupt FP. Malaria, anemia, and malnutrition in african children--defining intervention priorities. J Infect Dis. 2006;194:108–14. doi: 10.1086/504688. [DOI] [PubMed] [Google Scholar]
- 30.Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JS, Fosiko NG, Lewallen S, Liomba NG, Molyneux ME. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med. 2004;10:143–5. doi: 10.1038/nm986. [DOI] [PubMed] [Google Scholar]
- 31.Schubart CD, Mturi N, Beld MG, Wertheim PM, Newton CR. Role of viruses in Kenyan children presenting with acute encephalopathy in a malaria-endemic area. Am J Trop Med Hyg. 2006;75:1148–50. [PubMed] [Google Scholar]
- 32.Smith T, Schellenberg JA, Hayes R. Attributable fraction estimates and case definitions for malaria in endemic areas. Stat Med. 1994;13:2345–58. doi: 10.1002/sim.4780132206. [DOI] [PubMed] [Google Scholar]
- 33.Beare NA, Southern C, Chalira C, Taylor TE, Molyneux ME, Harding SP. Prognostic significance and course of retinopathy in children with severe malaria. Arch Ophthalmol. 2004;122:1141–7. doi: 10.1001/archopht.122.8.1141. [DOI] [PubMed] [Google Scholar]
- 34.Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME. Malarial retinopathy: a newly established diagnostic sign in severe malaria. Am J Trop Med Hyg. 2006;75:790–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar S. Overdiagnosis of cerebral malaria in patients admitted with neurological dysfunction. Qjm. 2003;96:688. doi: 10.1093/qjmed/hcg117. [DOI] [PubMed] [Google Scholar]
- 36.Fenn B, Morris SS, Black RE. Comorbidity in childhood in northern Ghana: magnitude, associated factors, and impact on mortality. Int J Epidemiol. 2005;34:368–75. doi: 10.1093/ije/dyh335. [DOI] [PubMed] [Google Scholar]
- 37.Okubadejo NU, Danesi MA. Diagnostic issues in cerebral malaria: a study of 112 adolescents and adults in Lagos, Nigeria. Niger Postgrad Med J. 2004;11:10–4. [PubMed] [Google Scholar]
- 38.Sasi P, English M, Berkley J, Lowe B, Shebe M, Mwakesi R, Kokwaro G. Characterisation of metabolic acidosis in Kenyan children admitted to hospital for acute non-surgical conditions. Trans R Soc Trop Med Hyg. 2006;100:401–9. doi: 10.1016/j.trstmh.2005.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zakai HA. Methods used in the diagnosis of malaria: where do we stand? J Egypt Soc Parasitol. 2003;33:979–90. [PubMed] [Google Scholar]
- 40.Ochola LB, Vounatsou P, Smith T, Mabaso ML, Newton CR. The reliability of diagnostic techniques in the diagnosis and management of malaria in the absence of a gold standard. Lancet Infect Dis. 2006;6:582–8. doi: 10.1016/S1473-3099(06)70579-5. [DOI] [PubMed] [Google Scholar]
- 41.Reyburn H, Mbakilwa H, Mwangi R, Mwerinde O, Olomi R, Drakeley C, Whitty CJ. Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: randomised trial. Bmj. 2007;334:403. doi: 10.1136/bmj.39073.496829.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berkley JA, Lowe BS, Mwangi I, Williams T, Bauni E, Mwarumba S, Ngetsa C, Slack MP, Njenga S, Hart CA, Maitland K, English M, Marsh K, Scott JA. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med. 2005;352:39–47. doi: 10.1056/NEJMoa040275. [DOI] [PubMed] [Google Scholar]
- 43.WHO . Pocket book of hospital care for children - guidelines for the management of common illnesses with limited resources. Geneva: WHO; 2005. [PubMed] [Google Scholar]
- 44.Ryan M, McCracken GH., Jr. Evidence behind the WHO guidelines: hospital care for children. J Trop Pediatr. 2006;52:46–8. doi: 10.1093/tropej/fmk007. [DOI] [PubMed] [Google Scholar]
- 45.Ayoola OO, Adeyemo AA, Osinusi K. Concurrent bacteraemia and malaria in febrile Nigerian infants. Trop Doct. 2005;35:34–6. doi: 10.1258/0049475053001840. [DOI] [PubMed] [Google Scholar]
- 46.Berkley JA, Mwangi I, Mellington F, Mwarumba S, Marsh K. Cerebral malaria versus bacterial meningitis in children with impaired consciousness. Qjm. 1999;92:151–7. doi: 10.1093/qjmed/92.3.151. [DOI] [PubMed] [Google Scholar]
- 47.Burdon J. Meningococcal meningitis in patients with falciparum malaria. Trop Doct. 1998;28:184–5. doi: 10.1177/004947559802800327. [DOI] [PubMed] [Google Scholar]
- 48.Enwere G, Van Hensbroek MB, Adegbola R, Palmer A, Onyiora E, Weber M, Greenwood BM. Bacteremia in Cerebral Malaria. Annals of Tropical Paediatrics. 1998;18:275–278. doi: 10.1080/02724936.1998.11747959. [DOI] [PubMed] [Google Scholar]
- 49.Graham SM, Walsh AL, Molyneux EM, Phiri AJ, Molyneux ME. Clinical presentation of non-typhoidal Salmonella bacteraemia in Malawian children. Trans R Soc Trop Med Hyg. 2000;94:310–4. doi: 10.1016/s0035-9203(00)90337-7. [DOI] [PubMed] [Google Scholar]
- 50.Okwara FN, Obimbo EM, Wafula EM, Murila FV. Bacteraemia, urinary tract infection and malaria in hospitalised febrile children in Nairobi: is there an association? East Afr Med J. 2004;81:47–51. doi: 10.4314/eamj.v81i1.8795. [DOI] [PubMed] [Google Scholar]
- 51.Walsh AL, Phiri AJ, Graham SM, Molyneux EM, Molyneux ME. Bacteremia in febrile Malawian children: clinical and microbiologic features. Pediatr Infect Dis J. 2000;19:312–8. doi: 10.1097/00006454-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 52.Wolday D, Kibreab T, Bukenya D, Hodes R. Meningococcal meningitis in patients with falciparum malaria. Trop Doct. 1996;26:157–9. doi: 10.1177/004947559602600405. [DOI] [PubMed] [Google Scholar]
- 53.Bronzan RN, Taylor TE, Mwenechanya J, Tembo M, Kayira K, Bwanaisa L, Njobvu A, Kondowe W, Chalira C, Walsh AL, Phiri A, Wilson LK, Molyneux ME, Graham SM. Bacteremia in Malawian children with severe malaria: prevalence, etiology, HIV coinfection, and outcome. J Infect Dis. 2007;195:895–904. doi: 10.1086/511437. [DOI] [PubMed] [Google Scholar]
- 54.Saez-Llorens X, Vargas S, Guerra F, Coronado L. Application of new sepsis definitions to evaluate outcome of pediatric patients with severe systemic infections. Pediatr Infect Dis J. 1995;14:557–61. doi: 10.1097/00006454-199507000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Falade AG, Mulholland EK, Adegbola RA, Greenwood BM. Bacterial isolates from blood and lung aspirate cultures in Gambian children with lobar pneumonia. Ann Trop Paediatr. 1997;17:315–9. doi: 10.1080/02724936.1997.11747904. [DOI] [PubMed] [Google Scholar]
- 56.Qazi S. Short-course therapy for community-acquired pneumonia in paediatric patients. Drugs. 2005;65:1179–92. doi: 10.2165/00003495-200565090-00001. [DOI] [PubMed] [Google Scholar]
- 57.Berkley JA, Versteeg AC, Mwangi I, Lowe BS, Newton CR. Indicators of acute bacterial meningitis in children at a rural Kenyan district hospital. Pediatrics. 2004;114:e713–9. doi: 10.1542/peds.2004-0007. [DOI] [PubMed] [Google Scholar]
- 58.Wright PW, Avery WG, Ardill WD, McLarty JW. Initial clinical assessment of the comatose patient: cerebral malaria vs. meningitis. Pediatr Infect Dis J. 1993;12:37–41. doi: 10.1097/00006454-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 59.Berkley JA, Mwangi I, Ngetsa CJ, Mwarumba S, Lowe BS, Marsh K, Newton CR. Diagnosis of acute bacterial meningitis in children at a district hospital in sub-Saharan Africa. Lancet. 2001;357:1753–7. doi: 10.1016/S0140-6736(00)04897-2. [DOI] [PubMed] [Google Scholar]
- 60.Dabis F, Ekpini ER. HIV-1/AIDS and Maternal and Child Health in Africa. Lancet. 2002;359:2097–2104. doi: 10.1016/S0140-6736(02)08909-2. [DOI] [PubMed] [Google Scholar]
- 61.UNAIDS UNAIDS Fact Sheet. 2005. http://data.unaids.org/pub/GlobalReport/2006/200605-FS_SubSaharanAfrica_en.pdf.
- 62.Korenromp EL. Malaria attributable to the HIV-1 epidemic, sub-Saharan Africa. Emerging Infectious Diseases. 2005;11:1410–1419. doi: 10.3201/eid1109.050337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abu-Raddad LJ, Patnaik P, Kublin JG. Dual infection with HIV and malaria fuels the spread of both diseases in sub-Saharan Africa. Science. 2006;314:1603–6. doi: 10.1126/science.1132338. [DOI] [PubMed] [Google Scholar]
- 64.Laufer MK, Plowe CV. The Interaction between HIV and Malaria in Africa. Curr Infect Dis Rep. 2007;9:47–54. doi: 10.1007/s11908-007-0022-3. [DOI] [PubMed] [Google Scholar]
- 65.Whitworth J, Morgan D, Quigley M, Smith A, Mayanja B, Eotu H, Omoding N, Okongo M, Malamba S, Ojwiya A. Effect of HIV-1 and increasing immunosuppression on malaria parasitaemia and clinical episodes in adults in rural Uganda: a cohort study. Lancet. 2000;356:1051–6. doi: 10.1016/S0140-6736(00)02727-6. [DOI] [PubMed] [Google Scholar]
- 66.Patnaik P, Jere CS, Miller WC, Hoffman IF, Wirima J, Pendame R, Meshnick SR, Taylor TE, Molyneux ME, Kublin JG. Effects of HIV-1 serostatus, HIV-1 RNA concentration, and CD4 cell count on the incidence of malaria infection in a cohort of adults in rural Malawi. J Infect Dis. 2005;192:984–91. doi: 10.1086/432730. [DOI] [PubMed] [Google Scholar]
- 67.Laufer MK, van Oosterhout JJ, Thesing PC, Thumba F, Zijlstra EE, Graham SM, Taylor TE, Plowe CV. Impact of HIV-Associated Immunosuppression on Malaria Infection and Disease in Malawi. J Infect Dis. 2006;193:872–8. doi: 10.1086/500245. [DOI] [PubMed] [Google Scholar]
- 68.Cohen C, Karstaedt A, Frean J, Thomas J, Govender N, Prentice E, Dini L, Galpin J, Crewe-Brown H. Increased prevalence of severe malaria in HIV-infected adults in South Africa. Clin Infect Dis. 2005;41:1631–7. doi: 10.1086/498023. [DOI] [PubMed] [Google Scholar]
- 69.Greenberg AE, Nsa W, Ryder RW, Medi M, Nzeza M, Kitadi N, Baangi M, Malanda N, Davachi F, Hassig SE. Plasmodium Falciparum malaria and perinatally acquired human immunodeficiency virus type 1 infection in Kinshasa, Zaire. A prospective, longitudinal cohort study of 587 children. N Engl J Med. 1991;325:105–9. doi: 10.1056/NEJM199107113250206. [DOI] [PubMed] [Google Scholar]
- 70.Kalyesubula I, Musoke-Mudido P, Marum L, Bagenda D, Aceng E, Ndugwa C, Olness K. Effects of malaria infection in human immunodeficiency virus type 1-infected Ugandan children. Pediatr Infect Dis J. 1997;16:876–81. doi: 10.1097/00006454-199709000-00011. [DOI] [PubMed] [Google Scholar]
- 71.Villamor E, Fataki MR, Mbise RL, Fawzi WW. Malaria parasitaemia in relation to HIV status and vitamin A supplementation among pre-school children. Trop Med Int Health. 2003;8:1051–61. doi: 10.1046/j.1360-2276.2003.01134.x. [DOI] [PubMed] [Google Scholar]
- 72.Grimwade K, French N, Mbatha DD, Zungu DD, Dedicoat M, Gilks CF. Childhood malaria in a region of unstable transmission and high human immunodeficiency virus prevalence. Pediatr Infect Dis J. 2003;22:1057–63. doi: 10.1097/01.inf.0000101188.95433.60. [DOI] [PubMed] [Google Scholar]
- 73.Otieno RO, Ouma C, Ong’echa JM, Keller CC, Were T, Waindi EN, Michaels MG, Day RD, Vulule JM, Perkins DJ. Increased severe anemia in HIV-1-exposed and HIV-1-positive infants and children during acute malaria. Aids. 2006;20:275–280. doi: 10.1097/01.aids.0000200533.56490.b7. [DOI] [PubMed] [Google Scholar]
- 74.Mermin J, Ekwaru JP, Liechty CA, Were W, Downing R, Ransom R, Weidle P, Lule J, Coutinho A, Solberg P. Effect of co-trimoxazole prophylaxis, antiretroviral therapy, and insecticide-treated bednets on the frequency of malaria in HIV-1-infected adults in Uganda: a prospective cohort study. Lancet. 2006;367:1256–61. doi: 10.1016/S0140-6736(06)68541-3. [DOI] [PubMed] [Google Scholar]
- 75.Thera MA, Sehdev PS, Coulibaly D, Traore K, Garba MN, Cissoko Y, Kone A, Guindo A, Dicko A, Beavogui AH, Djimde AA, Lyke KE, Diallo DA, Doumbo OK, Plowe CV. Impact of trimethoprim-sulfamethoxazole prophylaxis on falciparum malaria infection and disease. J Infect Dis. 2005;192:1823–9. doi: 10.1086/498249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kamya MR, Gasasira AF, Yeka A, Bakyaita N, Nsobya SL, Francis D, Rosenthal PJ, Dorsey G, Havlir D. Effect of HIV-1 infection on antimalarial treatment outcomes in Uganda: a population-based study. J Infect Dis. 2006;193:9–15. doi: 10.1086/498577. [DOI] [PubMed] [Google Scholar]
- 77.WHO World Health Report 2005. 2005. http://www.who.int/whr/2005/whr2005_en.pdf.
- 78.Murray MJ. Diet and cerebral malaria: The effect of Famine and Refeeding. American Journal of Clinical Nutrition. 1978;37:57–61. doi: 10.1093/ajcn/31.1.57. [DOI] [PubMed] [Google Scholar]
- 79.Edington MJ. Pathology of Malaria in West Africa. Bmj. 1967;1:715. doi: 10.1136/bmj.1.5542.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Genton B, Al-Yaman F, Ginny M, Taraika J, Alpers MP. Relation of anthropometry to malaria morbidity and immunity in Papua New Guinean children. Am J Clin Nutr. 1998;68:734–41. doi: 10.1093/ajcn/68.3.734. [DOI] [PubMed] [Google Scholar]
- 81.Snow RW, Byass P, Shenton FC, Greenwood BM. The relationship between anthropometric measurements and measurements of iron status and susceptibility to malaria in Gambian children. Trans R Soc Trop Med Hyg. 1991;85:584–9. doi: 10.1016/0035-9203(91)90351-x. [DOI] [PubMed] [Google Scholar]
- 82.Williams TN, Maitland K, Phelps L, Bennett S, Peto TE, Viji J, Timothy R, Clegg JB, Weatherall DJ, Bowden DK. Plasmodium vivax: a cause of malnutrition in young children. Qjm. 1997;90:751–7. doi: 10.1093/qjmed/90.12.751. [DOI] [PubMed] [Google Scholar]
- 83.Caulfield LE, Richard SA, Black RE. Undernutrition as an underlying cause of malaria morbidity and mortality in children less than five years old. Am J Trop Med Hyg. 2004;71:55–63. [PubMed] [Google Scholar]
- 84.Fishman S, Caulfield LE, de Onis M, Blossner M, Hyder A, Mullany L, Black RE. Comparative Quantification of Health Risks: The Global and Regional Burden of Disease due to 25 Selected Major Risk Factors. Cambridge: World Health Organization/Harvard University Press; 2004. Malnutrition and the global burden of disease: underweight. [Google Scholar]
- 85.WHO/CHD Immunisation-Linked Vitamin A Supplementation Study Group Randomised trial to assess benefits and safety of vitamin A supplementation linked to immunisation in early infancy. Lancet. 1998;352:1257–63. [PubMed] [Google Scholar]
- 86.Andersen M. Anthropometric Measurements in Health Programmes: Epidemiological and Statistical Aspects. Copenhagen, Denmark: University of Copenhagen; 1997. [Google Scholar]
- 87.Garenne M, Garenne M, Maire B, Fontaine O, Dieng K, Briend A. Risks of Dying Associated with Different Nutritional Status in Pre-School Aged Children. Dakar: 2000. [Google Scholar]
- 88.Ghana VAST Study Team Vitamin A supplementation in northern Ghana: effects on clinic attendances, hospital admissions, and child mortality. Lancet. 1993;342:7–12. [PubMed] [Google Scholar]
- 89.Friedman JF, Kwena AM, Mirel LB, Kariuki SK, Terlouw DJ, Phillips-Howard PA, Hawley WA, Nahlen BL, Shi YP, ter Kuile FO. Malaria and nutritional status among pre-school children: results from cross-sectional surveys in western Kenya. Am J Trop Med Hyg. 2005;73:698–704. [PubMed] [Google Scholar]
- 90.Nyakeriga AM, Troye-Blomberg M, Chemtai AK, Marsh K, Williams TN. Malaria and nutritional status in children living on the coast of Kenya. Am J Clin Nutr. 2004;80:1604–10. doi: 10.1093/ajcn/80.6.1604. [DOI] [PubMed] [Google Scholar]
- 91.Deen JL, Walraven GE, von Seidlein L. Increased risk for malaria in chronically malnourished children under 5 years of age in rural Gambia. J Trop Pediatr. 2002;48:78–83. doi: 10.1093/tropej/48.2.78. [DOI] [PubMed] [Google Scholar]
- 92.Man WD, Weber M, Palmer A, Schneider G, Wadda R, Jaffar S, Mulholland EK, Greenwood BM. Nutritional status of children admitted to hospital with different diseases and its relationship to outcome in The Gambia, West Africa. Trop Med Int Health. 1998;3:678–86. doi: 10.1046/j.1365-3156.1998.00283.x. [DOI] [PubMed] [Google Scholar]
- 93.Olumese PE, Sodeinde O, Ademowo OG, Walker O. Protein energy malnutrition and cerebral malaria in Nigerian children. J Trop Pediatr. 1997;43:217–9. doi: 10.1093/tropej/43.4.217. [DOI] [PubMed] [Google Scholar]
- 94.Rice AL, Sacco L, Hyder A, Black RE. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull World Health Organ. 2000;78:1207–21. [PMC free article] [PubMed] [Google Scholar]
- 95.Hamer C, Kvatum K, Jeffries D, Allen S. Detection of severe protein-energy malnutrition by nurses in The Gambia. Arch Dis Child. 2004;89:181–4. doi: 10.1136/adc.2002.022715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community based therapeutic care programs. 2005. http://www.unsystem.org/scn/Publications/community_based_mgmt/A%20review%20of%20methods%20to%20detect%20cases%20of%20severely%20malnourished%20children%20in%20the%20community.pdf. [DOI] [PubMed]
- 97.Berkley J, Mwangi I, Griffiths K, Ahmed I, Mithwani S, English M, Newton C, Maitland K. Assessment of severe malnutrition among hospitalized children in rural Kenya: comparison of weight for height and mid upper arm circumference. Jama. 2005;294:591–7. doi: 10.1001/jama.294.5.591. [DOI] [PubMed] [Google Scholar]
- 98.Group ZAPS Effect of zinc on the treatment of Plasmodium falciparum malaria in children: a randomized controlled trial. Am J Clin Nutr. 2002;76:805–12. doi: 10.1093/ajcn/76.4.805. [DOI] [PubMed] [Google Scholar]