Abstract
Objective
To examine the association between smoking and changes in cognitive function over time in the elderly persons without dementia.
Methods
The results of neuropsychological tests grouped into domains of memory, abstract-visuospatial and language, from several intervals over a five-year-period in 791 elderly without dementia or cognitive impairment. Smoking history was categorized as never, current or past smokers and related to the slope of performance in each cognitive domain using generalized estimating equations.
Results
Performance in all cognitive domains declined over time. Memory performance declined more rapidly among current smokers over age 75 years than in non-smokers similar in age, including those who never smoked or had quit smoking. The effect was stronger among those without an APOE-e4 allele. There was no association between smoking and performance in any cognitive domain in persons under age 75 years, and there was no association between past smoking and performance on any of the three cognitive factors at any time interval in either age group.
Conclusion
Current smokers over age 75 years perform more poorly on cognitive tests and appear to decline in memory more rapidly than their peers who do not smoke, especially if they lack the APOE-e4 allele. Smoking does not effect cognitive performance in those persons under age 75 years.
INTRODUCTION
Cognitive decline is a major public health concern in aging societies. About 1 percent of people aged 65-69 years have dementia, and this proportion increases with age to approximately 60 percent for people over the age of 95 1. There are inconclusive data relating smoking, a modifiable risk factor associated with many age-related diseases such as atherosclerosis or cerebrovascular disease 2,3, to cognitive decline and dementia 4-6. While case-control studies suggest that smoking lowers the risk of Alzheimer's Disease (AD) 6, prospective studies have shown an increased risk 4,5,7, or no association with AD 8-10. The effects of nicotine-induced increases in nicotinic acetylcholine receptors (nAChR) and protection against age-related nAChR decline are inconsistent because studies have also shown a reduction in nAChR in AD 11.
Whether or not smoking affects cognitive function in elderly without dementia or cognitive impairment, remains unclear. Most of the evidence derives from retrospective or cross-sectional studies using only a single time-point for the analysis 12,13. Longitudinal studies have provided only global neuropsychological assessments, did not have the ability to detect early stages of cognitive decline 14-16 or provided only short-follow-up periods 8,9,16. The objective in this study was to determine whether or not smoking is associated with decline in memory and other cognitive functions in elderly persons without dementia or cognitive impairment without dementia (CIND) at baseline.
METHODS
Subjects and Setting
Participants were part of a longitudinal study of Medicare recipients 65 years or older residing in northern Manhattan (Washington Heights, Hamilton Heights, Inwood) that has been described elsewhere 17. Each participant underwent an in-person interview of general health and function at the time of study entry followed by a standard assessment, including medical history, physical and neurological examination as well as a neuropsychological battery 18. Baseline data were collected from 1992 through 1994. Follow-up data were collected during evaluations at sequential intervals of approximately 18 months, performed from 1994 to 1996, 1996 to 1997, and 1997 to 1999. In this elderly population, some participants did not complete follow up at all intervals due to refusal to participate further, relocation or death. About one half of participants were evaluated at the third follow-up visit. This study was approved by the institutional review board of the Columbia-Presbyterian Medical Center.
The participants selected for this study were without dementia or cognitive impairment, complete smoking information, and with at least 3 follow-up intervals.
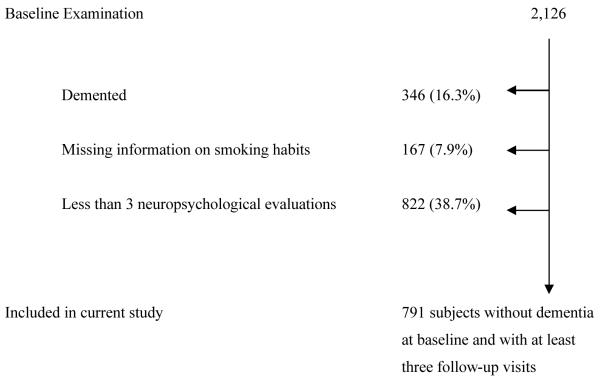
Of the 2126 individuals who underwent clinical assessment at baseline, 346 (16.3%) individuals were excluded due to dementia or CIND at baseline. Information on smoking habit was unavailable in 167 (7.9%) cases and 822 (38.7%) subjects had less than three follow-up visits with neuropsychological evaluation (Figure 1). The study focused on 791 individuals without dementia or cognitive impairment followed over a 5 year interval.
Figure 1.
Description of sample size.
Clinical assessments
Data included medical, neurological, and neuropsychological evaluations 18,19. All participants underwent a standardized neuropsychological test battery in either English or Spanish 18. Orientation was evaluated using parts of the modified Mini-Mental State Examination 20. Language was assessed using the Boston Naming Test 21, the Controlled Word Association Test 22, category naming, and the Complex Ideational Material and Phrase Repetition subtests from the Boston Diagnostic Aphasia Evaluation 23. Abstract Reasoning was evaluated using WAIS-R Similarities subtest 24, and the non-verbal Identities and Oddities subtest of the Mattis Dementia Rating Scale 25. Visuospatial ability was examined using the Rosen Drawing Test 26, and a matching version of the Benton Visual Retention Test 27. Memory was evaluated using the multiple choice version of the Benton Visual Retention Test 27 and the seven subtests of the Selective Reminding Test 28: total recall, long-term recall, long-term storage, continuous long-term storage, words recalled on last trial, delayed recall, and delayed recognition. This neuropsychological test battery has established norms for the same community 29.
Definition of dementia and cognitive impairment
Results from the neurological, psychiatric and neuropsychological examinations were reviewed in a consensus conference comprised of physicians, neurologists, neuropsychologists and psychiatrists. Based on this review all participants were assigned to one of three categories: normal cognitive function, CIND, or dementia. A diagnosis of CIND required a) a memory complaint b) objective impairment in at least one cognitive domain based on the average of the scores on the neuropsychological measures within that domain and a 1.5 SD cutoff using normative corrections for age, years of education, ethnicity and sex, c) essentially preserved activities of daily living, d) no evidence for dementia. Dementia was defined as the presence of abnormalities in several cognitive domains in neuropsychiatric testing accompanied by significant functional impairment (Clinical Dementia Rating (CDR) ≥ 1).
Smoking
A structured risk factor questionnaire, given in English and Spanish, was developed for the assessment of exposures to putative risk factors related to dementia 30. A trigger question asked whether or not the individual ever smoked at least one cigarette per day for a period of one year or more. If the answer to the trigger question was no, the subject was classified as non-smoker and no further questions were asked. Participants who answered the question affirmatively were classified as current smokers when they were still smoking, or past smokers when they had quit smoking. Current and past smokers were additionally asked at what age they began smoking and how many cigarettes on average they had smoked or still smoked per day. Past smokers were also asked at what age they had stopped smoking.
APOE Genotyping
APOE genotypes were determined as described by Hixson and Vernier 31 with slight modification 32. We classified persons as homozygeous or heterozygeous for the APOE ε4 allele or not having any ε4 allele.
Other covariates
Diabetes mellitus and hypertension were defined by self-report at baseline and at each follow-up interval or by the use of disease specific medications. Blood pressure measurements were also considered in the definition of hypertension. Body mass index (BMI) was calculated by the formula BMI = weight (Kg)/height (m)2.
Statistical Methods
A factor analysis was performed using data from the entire cohort with the 15 neuropsychological measures using a principal component analysis with varimax rotation and Kaiser normalization 33. This analysis resulted in three factors: 1) a memory factor, in which the seven subtests of the Selective Reminding Test were the main contributors; 2) a abstract/visuospatial factor, where visuospatial and tests of reasoning were the main contributors; and 3) a language factor, in which language measures from the Boston Naming Test 21, Controlled Oral Word Association Test 22, and the WAIS-R Similarities 24 were the main contributors. We calculated cognitive scores for each participant at each visit by adding the scores of the measures that contributed most to each factor (tests with correlations of 0.5 or higher). Each factor score was normally distributed.
GEE 34 were used to examine changes in each cognitive domain over time. The dependent variables were the factor scores, and the independent variables were current smoking, past smoking, time (included as a continuous variable), and the interaction of smoking and time. Gender, age, education, ethnic group, APOEε4 allele, hypertension and heart disease were included as covariates in subsequent analyses.
The GEE analysis yielded coefficient values that represent the associations between a factor score and variables included in the model. There were three main coefficients of interest in each model: one comparing the smoking groups at baseline, one relating the change in cognitive scores with time, and an interaction term for current or past smoking and time. A significant p value for the coefficient comparing smoking groups at baseline indicates a difference between two groups at baseline. A significant p value for the coefficient of time indicates a statistically significant change in a cognitive score over the total duration of follow-up. A significant p value for the interaction coefficient indicates a difference in the rate of change in a factor score depending on the smoking group; this is the main variable of interest for the interpretation of the analyses. All analyses were repeated after stratifying for median of age.
RESULTS
The mean age of the sample was 75.6 ± 5.4 years, 70.5% were women, 48.6% were Hispanic, 19.2% were White, and 31.6% were Black (Table 1). The mean of years of education was 8.7 ± 4.6, and 29.4% were homozygous or heterozygous for the APOE-ε4 allele. The mean BMI was 27.1 ± 5.1, and 16.9% of the subjects reported having diabetes, 56.8% hypertension and 14.6% heart disease. 48.9% were never smokers, 35.1% past smokers and 15.9% current smokers.
Table 1.
Demographic characteristics of study population
| Healthy elderly (n=791) | |
|---|---|
| Men | 233 (29.5) |
| Women | 558 (70.5) |
| Education, mean (SD), year | 8.7 (4.6) |
| Age, mean (SD), year | 75.6 (5.4) |
| Body mass index, mean (SD) | 27.1 (5.1) |
| Ethnic group ‡ | |
| White/Non-Hispanic | 152(19.2) |
| Black/Non-Hispanic | 250(31.6) |
| Hispanic | 384 (48.6) |
| APOE genotype 4/4 | 13 (1.6) |
| APOE genotype 4/- | 220 (27.8) |
| APOE genotype -/- | 549 (69.4) |
| Smoking Habit | |
| Never smoker | 387 (48.9%) |
| Past smoker | 278 (35.1%) |
| Current smoker | 126(15.9%) |
| No Diabetes | 652 (82.4) |
| Diabetes, not treated | 29 (3.7) |
| Diabetes, treated | 104 (13.2) |
| No heart disease | 670 (84.7) |
| Heart disease, not treated | 22 (2.8) |
| Heart disease, treated | 93 (11.8) |
| No hypertension | 338 (42.7) |
| Hypertension, not treated | 127 (16.6) |
| Hypertension, treated | 318 (40.2) |
Values are expressed as number (percentage) unless otherwise indicated. Some percentages are based on an incomplete sample due to small amounts of missing data.
Classified by self-report using the format of the 1990 US census49.
Men were more often current or past smokers than women (Table 2). Blacks were significantly less often never smokers but more often current smokers than Whites and Hispanics.
Table 2.
Comparison of smoking status by demographics in 791 subjects
| Never Smoking | Past Smoking | Current Smoking | |
|---|---|---|---|
| Men | 61 (26.2) | 113 (48.5)* | 59 (25.3)* |
| Women | 326 (58.4)* | 165 (29.6) | 67 (12.0) |
| Ethnic group† | |||
| White/Non-Hispanic | 78 (51.3)* | 59 (38.8) | 15 (9.9) |
| Black/Non-Hispanic | 104 (41.6) | 86 (34.4) | 60 (24.0)** |
| Hispanic | 203 (52.9)* | 133 (34.6) | 48 (12.5) |
Values are expressed as number (SD) unless otherwise indicated. Some percentages are based on an incomplete sample due to small amounts of missing data.
Significant at a 0.05 level versus lowest value within smoking group, based on χ2 test for categorical data.
Significant at a 0.05 level versus all lower values within smoking group, based on χ2 test for categorical data.
Classified by self-report using the format of the 1990 US census49.
In the GEE analysis memory, abstract/visuospatial and language performance declined significantly over time. Increased age at baseline was related to lower scores in all three cognitive domains at each interval, while higher education and White ethnicity were associated with higher scores in all domains at each interval. Current or past smoking was not associated with more rapid cognitive decline in analyses for the whole sample (p for interaction of smoking and time = 0.2).
These analyses were repeated stratifying by median of age (75.6 years). Current smokers over 75 years showed significantly lower scores in abstract/visuospatial performance at baseline than never or past smokers (Table 3), and they showed a significant decline over the follow-up in memory (p = 0.05). Thus, memory performance declined at a faster rate among current smokers older than 75 years than in subjects of similar age who never smoked or quit smoking (Table 4). These associations remained significant after adjusting for age, gender, ethnic group, education, APOEε4 allele and potential vascular risk factors such as hypertension and heart disease. In participants without the APOEε4 allele being over 75 years smoking substantially increased the risk of cognitive and memory decline, while carriers of APOEε4 showed no relation between smoking and memory or abstract/visuospatial performance (Table 5).
Table 3.
Impact of Current Smoking and Follow-up time on Abstract/visuospatial Performance in Elderly Persons Stratified by Age Group.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | Estimated ß (SE) | p-value | Estimated ß (SE) | p-value |
| Persons ≤ 75 years old | ||||
| Time | -0.7 (0.2) | 0.001* | -0.7 (0.2) | 0.001* |
| Current Smoking | 1.2 (2.7) | 0.7 | 0.2 (2.9) | 0.9 |
| Time*current smoking | 0.1 (0.5) | 0.9 | 0.1 (0.5) | 0.9 |
| Persons > 75 years old | ||||
| Time | -0.9 (0.2) | 0.002* | -1.0(0.2) | 0.002* |
| Current Smoking | -7.4 (2.3) | 0.001* | -7.9 (2.4) | 0.001* |
| Time*current smoking | -0.5 (0.6) | 0.4 | -0.4 (0.5) | 0.5 |
Model 1 is adjusted for age and gender, Model 2 is adjusted for age, gender, education, ethnic group and APOEε4, hypertension, heart disease and diabetes
significant at a 0.05 level
Table 4.
Relationship of Current Smoking and Time of Follow-up to Memory Performance in Elderly Persons Over 5 years of Follow-up Stratified by Age Group.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | Estimated ß (SE) | p-value | Estimated ß (SE) | p-value |
| Persons ≤ 75 years old | ||||
| Time | -5.9 (0.6) | 0.001* | -5.8 (0.6) | 0.001* |
| Current Smoking | -1.0 (5.8) | 0.8 | -3.6 (5.8) | 0.9 |
| Time*current smoking | -1.2 (1.6) | 0.4 | -1.1 (1.6) | 0.5 |
| Persons > 75 years old | ||||
| Time | -7.7 (0.6) | 0.002* | -7.9 (0.7) | 0.002* |
| Current Smoking | -1.8 (1.2) | 0.1 | -3.9 (6.6) | 0.5 |
| Time*current smoking | -0.7 (0.3) | 0.05* | -4.0 (1.8) | 0.02* |
Model 1 is adjusted for age and gender, Model 2 is adjusted for age, gender, education, ethnic group and APOEε4, hypertension, heart disease and diabetes
significant at a 0.05 level
Table 5.
Relationship of Current Smoking and Time of Follow-up to Memory and Abstract/visuospatial Performance by APOEε4 genotype
| -/- APOEε4 genotype | -/4 or 4/4 APOEε4 genotype | |||
|---|---|---|---|---|
| Variable | Estimated ß (SE) | p-value | Estimated ß (SE) | p-value |
| Memory Performance | ||||
| Persons ≤ 75 years old | ||||
| Time | -5.5 (0.7) | 0.001* | -6.9 (1.2) | 0.002* |
| Current Smoking | -5.7 (6.6) | 0.4 | 8.9 (11.2) | 0.4 |
| Time*current smoking | -1.3 (1.9) | 0.5 | -0.1 (2.7) | 0.9 |
| Persons > 75 years old | ||||
| Time | -7.1 (0.7) | 0.001* | -9.7 (1.2) | 0.002* |
| Current Smoking | -4.8 (7.7) | 0.5 | 0.4 (10.7) | 0.9 |
| Time*current smoking | -5.5 (2.3) | 0.016* | -0.9 (2.8) | 0.7 |
| Abstract/visuospatial Performance | ||||
| Persons ≤ 75 years old | ||||
| Time | -0.7 (0.2) | 0.003* | -0.8 (0.4) | 0.08 |
| Current Smoking | -1.8 (3.4) | 0.6 | 5.1 (5.2) | 0.3 |
| Time*current smoking | 0.4 (0.6) | 0.5 | -0.6 (1.0) | 0.5 |
| Persons > 75 years old | ||||
| Time | -0.9 (0.3) | 0.001* | -1.2 (0.4) | 0.006* |
| Current Smoking | -8.9 (3.1) | 0.005* | -4.7 (4.0) | 0.3 |
| Time*current smoking | -0.3 (0.7) | 0.7 | -0.4 (1.2) | 0.7 |
All models adjusted for age, gender, education, ethnic group, hypertension, heart disease and diabetes
significant at a 0.05 level
There was no association between smoking and decline in language or abstract-visuospatial test (Tables 3 and 6). Scores of both factors were normally distributed at each time interval indicating that the lack of a total current smoking*time interaction was not the result of a ceiling or floor effect.
Table 6.
Relationship of Current Smoking and Time of Follow-up to Language Performance in Healthy Elderly Over 5 years of Follow-up Stratified by Age Group.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | Estimated ß (SE) | p-value | Estimated ß (SE) | p-value |
| Persons ≤ 75 years old | ||||
| Time | -0.2 (0.1) | 0.002* | -0.2 (0.1) | 0.001* |
| Current Smoking | 0.7 (0.4) | 0.1 | 0.6 (0.4) | 0.2 |
| Time*current smoking | -0.1 (0.1) | 0.4 | -0.1 (0.1) | 0.5 |
| Persons > 75 years old | ||||
| Time | -0.3 (0.1) | 0.003* | -0.3 (0.1) | 0.004* |
| Current Smoking | -0.5 (0.6) | 0.5 | -0.7 (0.7) | 0.3 |
| Time*current smoking | -0.1 (0.2) | 0.5 | -0.1 (0.2) | 0.5 |
Model 1 is adjusted for age and gender, Model 2 is adjusted for age, gender, education, ethnic group and APOEε4, hypertension, heart disease and diabetes
significant at a 0.05 level
DISCUSSION
In this study the performance in memory, abstract-visuospatial and language domains over time declined in individuals free of dementia or cognitive impairment at baseline, and increased age was associated with lower scores in all cognitive domains. Current smoking was associated with faster cognitive decline only in memory among subjects older than 75 years without the APOE-ε4 allele. Past smoking was not associated with poor performance in any cognitive domain at any specific time interval, or decline in any domain over time.
The mechanisms by which smoking affects cognitive performance remain unclear. It has been proposed that smoking may increase the risk of dementia through cerebrovascular disease 35, or that it augments cholinergic metabolism by upregulation of cholinergic nicotinic receptors in the brain 36. Cholinergic deficits, characterized by reduced levels of acetylcholine and nicotinic receptors, are found in AD 37. However, nicotine increases acetylcholine release, elevates the number of nicotinic receptors, and improves attention and information processing 38. These actions may be opposed by high oxidative stress caused by smoking, which is a putative mechanism in AD 39,40, through generation of free radicals and affecting inflammatory-immune systems, which activate phagocytes that generate further oxidative damage 41. There is also evidence that smokers have a lower dietary intake of antioxidants compared with nonsmokers 42.
Studies examining the role of smoking in cognitive function reported inconsistent results. Several case-control studies suggested that smoking might be related to a lower risk of AD 6, but prospective studies reported an increased risk of AD 4,5,7 or no association 8-10.
Our results are consistent with studies showing an increased risk of AD in current smokers. The main cognitive domain affected in AD is memory 43,44 and it seems reasonable to postulate that if smoking is related to a higher risk of AD, it must be related to decline in memory.
We found that the association between current smoking and AD was restricted to persons older than 75 years of age. The risk of AD increases with age 43, and our finding may indicate that smoking increases the risk of memory decline in those who are more likely to develop memory decline. We also found that the association between current smoking and faster cognitive decline was confined to subjects without the APOE-ε4 allele. This is in agreement with two previous studies reporting an increased risk of AD in participants without the APOEε4 allele. The presence of the APOE-ε4 allele increases the risk of AD 45. Older individuals with the APOE-ε4 may have an increased risk of memory decline 46 in a such a way that other risk factors may not increase the risk further. Another potential explanation for the lack of association of smoking to memory decline in APOEε-4 carriers is that smoking may be harmful through vascular mechanisms, but also partly beneficial in APOEε4 carriers. This hypothesis is supported by previous findings that persons with AD who are APOEε4 carriers have fewer nicotinic receptor binding sites and lower activity of choline acetyltransferase than non-carriers 47. Smoking could counterbalance the APOEε4 associated impairment by facilitating the release of acetylcholine or increasing the density of nicotine receptors.
There are several potential alternative explanations for our findings. One is chance, particularly in the context of multiple comparisons. However, our findings were not unexpected, are consistent with our previous findings relating current smoking to a higher risk of AD 5, and consistent with other studies as described in the previous paragraph; these facts make chance due to multiple comparisons an unlikely explanation for our findings 48. Another potential explanation is bias. For example, that only subjects with preclinical AD reported smoking while subjects that would not develop AD did not. This type of reporting bias seems unlikely and we excluded cases of incipient dementia or cognitive impairment that could have influenced our results. Another potential explanation is confounding. For example, if lower education is related to current smoking, and persons with lower education are more likely to be diagnosed with AD, then it is possible that a relation between smoking and cognitive decline could be due to confounding by socioeconomic factors. We adjusted for years of education and ethnicity as markers of socioeconomic status to account for this possibility. Finally, another explanation is genetic confounding. It may be that smoking propensity is associated with a gene or combination of genes (but not APOE) which in turn is associated with the risk of AD. Therefore, it is possible that smoking is related to other behaviors related to poor health or genetic factors, that in turn may increase the risk of AD, that we could not adjust for, and we cannot eliminate the possibility of lack of control for unknown confounders as a potential explanation for our findings.
This study has several strengths. We had a comprehensive and sensitive neuropsychological battery validated for use in the communities of northern Manhattan 18. We also excluded from our analyses persons with dementia and cognitive impairment without dementia at baseline that may have biased the analyses, and had several evaluation time points that allowed prospective analyses.
The main limitation of this study is the ascertainment of smoking status. We relied on self-report by participants, and did not have information on quantity or duration of smoking. Assuming random misclassification of smoking, this would have resulted in the underestimation of the association between smoking and cognitive impairment. Given that we excluded subjects with dementia and with cognitive impairment without dementia at baseline from the analyses, it seems unlikely that the report of smoking status was influenced by cognitive status.
It is important to point out that this study was conducted in an elderly multiethnic community in an urban setting with a high prevalence of risk factors for morbidity and mortality, such as diabetes and hypertension. Persons who dropped out of the study before completing at least three follow-up visits were at baseline older, less educated and had a higher prevalence of vascular risk factors than those who remained in the study. Also, smoking is related to higher mortality from various causes, and it is possible that many smokers would have demonstrated cognitive decline had they not died prior to inclusion in this cohort. Thus, there are important biases related to the sample of this study that should be taken into account in the interpretation and generalization of these findings.
References
- (1).Fratiglioni L, De Ronchi D, Aguero-Torres H. Worldwide prevalence and incidence of dementia. Drugs Aging. 1999;15(5) doi: 10.2165/00002512-199915050-00004. [DOI] [PubMed] [Google Scholar]
- (2).Howard G, Wagenknecht LE, Burke GL, et al. Cigarette smoking and progression of atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Study. Jama. 1998;279(2) doi: 10.1001/jama.279.2.119. 1914. [DOI] [PubMed] [Google Scholar]
- (3).McGill HC., Jr. Smoking and the pathogenesis of atherosclerosis. Adv Exp Med Biol. 1990;273 doi: 10.1007/978-1-4684-5829-9_2. [DOI] [PubMed] [Google Scholar]
- (4).Launer LJ, Andersen K, Dewey ME, et al. Rates and risk factors for dementia and Alzheimer's disease: results from EURODEM pooled analyses. EURODEM Incidence Research Group and Work Groups. European Studies of Dementia. Neurology. 1999;52(1) doi: 10.1212/wnl.52.1.78. 1901. [DOI] [PubMed] [Google Scholar]
- (5).Merchant C, Tang MX, Albert S, Manly J, Stern Y, Mayeux R. The influence of smoking on the risk of Alzheimer's disease. Neurology. 1999;52(7) doi: 10.1212/wnl.52.7.1408. 1922. [DOI] [PubMed] [Google Scholar]
- (6).Tyas SL. Are tobacco and alcohol use related to Alzheimer's disease? A critical assessment of the evidence and its implications. Addict Biol. 1996;1(3) doi: 10.1080/1355621961000124856. [DOI] [PubMed] [Google Scholar]
- (7).Ott A, Slooter AJ, Hofman A, et al. Smoking and risk of dementia and Alzheimer's disease in a population-based cohort study: the Rotterdam Study. Lancet. 1998;351(9119) doi: 10.1016/s0140-6736(97)07541-7. 1920. [DOI] [PubMed] [Google Scholar]
- (8).Brayne C, Gill C, Huppert FA, et al. Vascular risks and incident dementia: results from a cohort study of the very old. Dement Geriatr Cogn Disord. 1998;9(3) doi: 10.1159/000017043. [DOI] [PubMed] [Google Scholar]
- (9).Broe GA, Creasey H, Jorm AF, et al. Health habits and risk of cognitive impairment and dementia in old age: a prospective study on the effects of exercise, smoking and alcohol consumption. Aust N Z J Public Health. 1998;22(5) doi: 10.1111/j.1467-842x.1998.tb01449.x. [DOI] [PubMed] [Google Scholar]
- (10).Doll R, Peto R, Boreham J, Sutherland I. Smoking and dementia in male British doctors: prospective study. Bmj. 2000;320(7242) doi: 10.1136/bmj.320.7242.1097. 1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Sabbagh MN, Lukas RJ, Sparks DL, Reid RT. The nicotinic acetylcholine receptor, smoking, and Alzheimer's disease. J Alzheimers Dis. 2002;4(4) doi: 10.3233/jad-2002-4407. [DOI] [PubMed] [Google Scholar]
- (12).Elwood PC, Gallacher JE, Hopkinson CA, et al. Smoking, drinking, and other life style factors and cognitive function in men in the Caerphilly cohort. J Epidemiol Community Health. 1999;53(1) doi: 10.1136/jech.53.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Hill RD, Nilsson LG, Nyberg L, Backman L. Cigarette smoking and cognitive performance in healthy Swedish adults. Age Ageing. 2003;32(5) doi: 10.1093/ageing/afg067. [DOI] [PubMed] [Google Scholar]
- (14).Ford AB, Mefrouche Z, Friedland RP, Debanne SM. Smoking and cognitive impairment: a population-based study. J Am Geriatr Soc. 1996;44(8) doi: 10.1111/j.1532-5415.1996.tb01858.x. [DOI] [PubMed] [Google Scholar]
- (15).Herbert LE, Scherr PA, Beckett LA, et al. Relation of smoking and low-to-moderate alcohol consumption to change in cognitive function: a longitudinal study in a defined community of older persons. Am J Epidemiol. 1993;137(8) doi: 10.1093/oxfordjournals.aje.a116749. 1915. [DOI] [PubMed] [Google Scholar]
- (16).Launer LJ, Feskens EJ, Kalmijn S, Kromhout D. Smoking, drinking, and thinking. The Zutphen Elderly Study. Am J Epidemiol. 1996;143(3) doi: 10.1093/oxfordjournals.aje.a008732. 1901. [DOI] [PubMed] [Google Scholar]
- (17).Tang MX, Stern Y, Marder K, et al. The APOE-epsilon4 allele and the risk of Alzheimer disease among African Americans, whites, and Hispanics. Jama. 1998;279(10) doi: 10.1001/jama.279.10.751. 1911. [DOI] [PubMed] [Google Scholar]
- (18).Stern Y, Andrews H, Pittman J, et al. Diagnosis of dementia in a heterogeneous population. Development of a neuropsychological paradigm-based diagnosis of dementia and quantified correction for the effects of education. Arch Neurol. 1992;49(5) doi: 10.1001/archneur.1992.00530290035009. [DOI] [PubMed] [Google Scholar]
- (19).Pittman J, Andrews H, Tatemichi T, et al. Diagnosis of dementia in a heterogeneous population. A comparison of paradigm-based diagnosis and physician's diagnosis. Arch Neurol. 1992;49(5) doi: 10.1001/archneur.1992.00530290043010. [DOI] [PubMed] [Google Scholar]
- (20).Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3) doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- (21).Kaplan E, Goodglass H, Weintraub S. Boston Naming Test. Lea & Febiger; Philadelphia, PA: 1983. [Google Scholar]
- (22).Benton A. FAS Test. University of Victoria; Viactoria, B.C.: 1967. [Google Scholar]
- (23).Goodglass H, Kaplan E. The Assessment of Aphasia and Related Disorders. 2.ed. Lea & Febiger; Philadelphia, PA: 1983. [Google Scholar]
- (24).Wechsler D. Wechsler Adult Intelligence Scale-Revised. The Psychological Corporation; New York, NY: 1981. [Google Scholar]
- (25).Mattis S. Mental status examination for organic mental syndrome in the elderly patient. In: Bellak L, Karasu TB, editors. Geriatric Psychiatry. Grune & Stratton; New York, NY: 1976. pp. 77–121. [Google Scholar]
- (26).Rosen W. The Rosen Drawing Test. Veterans Administration Medical Center; Bronx, NY: 1981. [Google Scholar]
- (27).Benton A. The Benton Visal Retention Test. The Psychological Corporation; New York: 1955. [Google Scholar]
- (28).Buschke H, Fuld PA. Evaluating storage, retention, and retrieval in disordered memory and learning. Neurology. 1974;24(11) doi: 10.1212/wnl.24.11.1019. [DOI] [PubMed] [Google Scholar]
- (29).Stricks L, Pittman J, Jacobs DM, Sano M, Stern Y. Normative data for a brief neuropsychological battery administered to English- and Spanish-speaking community-dwelling elders. J Int Neuropsychol Soc. 1998;4(4) [PubMed] [Google Scholar]
- (30).Mayeux R, Ottman R, Tang MX, et al. Genetic susceptibility and head injury as risk factors for Alzheimer's disease among community-dwelling elderly persons and their first-degree relatives. Ann Neurol. 1993;33(5) doi: 10.1002/ana.410330513. [DOI] [PubMed] [Google Scholar]
- (31).Hixson JE, Vernier DT. Restriction isotyping of human apolipoprotein E by gene amplification and cleavage with HhaI. J Lipid Res. 1990;31(3) [PubMed] [Google Scholar]
- (32).Mayeux R, Ottman R, Maestre G, et al. Synergistic effects of traumatic head injury and apolipoprotein-epsilon 4 in patients with Alzheimer's disease. Neurology. 1995;45(3 Pt 1) doi: 10.1212/wnl.45.3.555. [DOI] [PubMed] [Google Scholar]
- (33).Kleinbaum D, Klipper L, Muller K. Applied regression analysis and other multivariable methods. 2nd ed. PWS-Kent; Boston: p. 631. [Google Scholar]
- (34).Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4) [PubMed] [Google Scholar]
- (35).Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. Jama. 1999;282(22) doi: 10.1001/jama.282.22.2149. 1908. [DOI] [PubMed] [Google Scholar]
- (36).Whitehouse PJ, Martino AM, Wagster MV, et al. Reductions in [3H]nicotinic acetylcholine binding in Alzheimer's disease and Parkinson's disease: an autoradiographic study. Neurology. 1988;38(5) doi: 10.1212/wnl.38.5.720. [DOI] [PubMed] [Google Scholar]
- (37).Nordberg A. Biological markers and the cholinergic hypothesis in Alzheimer's disease. Acta Neurol Scand Suppl. 1992;139 doi: 10.1111/j.1600-0404.1992.tb04455.x. [DOI] [PubMed] [Google Scholar]
- (38).Kellar KJ, Wonnacott S. In: Nicotinic cholinergic receptors in Alzheimer's Disease, in nicotine psychopharmacology: molecular, cellular, and behavioral aspects. Wonnacott S, Russell MAH, Stolerman P, editors. Oxford University Press; Oxford: 1990. [Google Scholar]
- (39).Perry G, Cash AD, Smith MA. Alzheimer Disease and Oxidative Stress. J Biomed Biotechnol. 2002;2(3) doi: 10.1155/S1110724302203010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Rottkamp CA, Nunomura A, Raina AK, Sayre LM, Perry G, Smith MA. Oxidative stress, antioxidants, and Alzheimer disease. Alzheimer Dis Assoc Disord. 2000;14(Suppl 1) doi: 10.1097/00002093-200000001-00010. [DOI] [PubMed] [Google Scholar]
- (41).Traber MG, van der Vliet A, Reznick AZ, Cross CE. Tobacco-related diseases. Is there a role for antioxidant micronutrient supplementation? Clin Chest Med. 2000;21(1) doi: 10.1016/s0272-5231(05)70016-2. [DOI] [PubMed] [Google Scholar]
- (42).Dallongeville J, Marecaux N, Fruchart JC, Amouyel P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: a meta-analysis. J Nutr. 1998;128(9) doi: 10.1093/jn/128.9.1450. [DOI] [PubMed] [Google Scholar]
- (43).Ritchie K, Lovestone S. The dementias. Lancet. 2002;360(9347) doi: 10.1016/S0140-6736(02)11667-9. 1930. [DOI] [PubMed] [Google Scholar]
- (44).Small SA, Stern Y, Tang M, Mayeux R. Selective decline in memory function among healthy elderly. Neurology. 1999;52(7) doi: 10.1212/wnl.52.7.1392. 1922. [DOI] [PubMed] [Google Scholar]
- (45).Selkoe DJ. Alzheimer's disease: genotypes, phenotypes, and treatments. Science. 1997;275(5300) doi: 10.1126/science.275.5300.630. 1931. [DOI] [PubMed] [Google Scholar]
- (46).Mayeux R, Small SA, Tang M, Tycko B, Stern Y. Memory performance in healthy elderly without Alzheimer's disease: effects of time and apolipoprotein-E. Neurobiol Aging. 2001;22(4) doi: 10.1016/s0197-4580(01)00223-8. [DOI] [PubMed] [Google Scholar]
- (47).Poirier J, Delisle MC, Quirion R, et al. Apolipoprotein E4 allele as a predictor of cholinergic deficits and treatment outcome in Alzheimer disease. Proc Natl Acad Sci U S A. 1995;92(26) doi: 10.1073/pnas.92.26.12260. 1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (48).Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1) [PubMed] [Google Scholar]
- (49).STF 1A database. Bureau of Census; Washington DC: 1991. Census of Population and Housing. Summary Tape File1, Technical Documentation (computer program) 1990. [Google Scholar]