Abstract
Glenoid inclination has been associated with rotator cuff tears and superior humeral translation, but the relationship between glenoid inclination and superior humeral translation has not been assessed in-vivo. The objective of this study was to compare glenoid inclination between repaired and contralateral shoulders of unilateral rotator cuff repair patients. As a secondary analysis, we assessed the relationship between glenoid inclination and in-vivo superior humeral translation. Glenoid inclination was measured from patient-specific, CT-based bone models. Glenohumeral joint motion was measured from biplane x-ray images collected during coronal-plane abduction of 21 rotator cuff repair patients. Glenoid inclination was significantly lower for the rotator cuff tear shoulders (90.7°) than the asymptomatic, contralateral shoulders (92.3°, p=0.04). There was no significant correlation between increased glenoid inclination and superior/inferior translation of the uninjured shoulder (p>0.30). This study failed to support the theory that glenoid inclination is responsible for superior humeral translation and the development of subacromial impingement.
Introduction
Rotator cuff injuries are very common, leading to pain, loss of function, and significant medical expense. The etiology of rotator cuff injuries is not well understood, but subacromial impingement has long been associated with rotator cuff disability.7-9 Subacromial impingement has been associated with superior translation of the humerus relative to the scapula10,15, and it is also believed that glenoid inclination, i.e., the degree to which the glenoid is tipped up relative to the scapula, may influence the amount of superior humeral translation. The belief that increased glenoid inclination leads to superior translation of the humerus and ultimately subacromial impingement is supported by previous data. Specifically, cadaveric studies have demonstrated that greater glenoid inclination is associated with higher superior translation of the humerus,6,13 and imaging studies have demonstrated greater glenoid inclination in the shoulders of patients or cadaver specimens with rotator cuff tears.4,12 In contrast, a study by Kandemir and colleagues failed to detect any significant difference in glenoid inclination between cadaver specimens with a rotator cuff injury and specimens with a normal, healthy rotator cuff. Furthermore, the relationship between glenoid inclination and superior humeral translation has been demonstrated only in cadaver studies, where it is extremely difficult to simulate the complex muscle forces and joint forces accurately that occur during in-vivo conditions. Thus, the relationship between glenoid inclination and glenohumeral joint translation under in-vivo conditions remains unknown. The primary objective of this study was to compare glenoid inclination between the repaired and contralateral shoulders of patients who had undergone unilateral rotator cuff repair. We hypothesized that there would be greater glenoid inclination in the repaired shoulder than in the contralateral shoulder. As a secondary analysis of these data, we assessed the relationship between glenoid inclination and in-vivo superior translation of the humerus relative to the scapula. We hypothesized that there would be a significant association between glenoid inclination and superior translation of the humerus during shoulder elevation.
Materials and Methods
Following IRB approval and informed consent, 21 subjects (14 male, 7 female, age 63.0 ± 11.4 years) were included in this study. The sample size of 21 patients was based on a standard deviation of 2.3° (from preliminary data collected as part of this study) and the desire to detect a difference in glenoid inclination of 1.5° with 80% power (α=0.05, β=0.2). Each subject underwent arthroscopic surgery on one shoulder 4 months prior to the study to repair a full-thickness supraspinatus tendon tear. The contralateral shoulder of each subject was asymptomatic and was deemed to be normal under clinical exam by an orthopaedic surgeon.
Glenoid inclination, i.e., superior/inferior tilt of the glenoid relative to the scapula, was measured in both shoulders of each subject using subject specific, CT-based, three-dimensional (3D) computer models. To achieve this, individual CT scans of the entire left and right scapula and humerus were acquired for each patient (GE Lightspeed16, Milwaukee, WI). Each CT scan had an in-plane resolution of approximately 0.6 by 0.6 mm and a slice spacing of 1.25 mm. The humerus and scapula were segmented from surrounding soft tissues (Mimics 11.11, Materialise, Leuven, Belgium) and then reconstructed into a 3D computer model.
Using custom software, anatomic landmarks were manually identified on each CT model and used to calculate glenoid inclination, as previously reported (Figure 1).4,5 These anatomic landmarks included: A) the intersection of the scapular spine and the scapula's medial border, B) the middle of the spinoglenoid notch, C) the superior-most point on the glenoid rim, and D) the inferior-most point on the glenoid rim. Glenoid inclination angle was defined as the 3D angle between a line connecting the intersection of the scapular spine and the medial border (Figure 1, point A) to the spinoglenoid notch (Figure 1, point B) and a line connecting the superior glenoid rim (Figure 1, point C) and inferior glenoid rim (Figure 1, point D). A greater inclination angle indicates a more superior facing glenoid relative to the scapula. One observer identified all landmarks for all subjects in the study. In addition, these landmarks were identified two more times on twelve of the CT models, with the observer masked to previous measurements. These data provided an assessment of intra-observer reliability.
Figure 1.
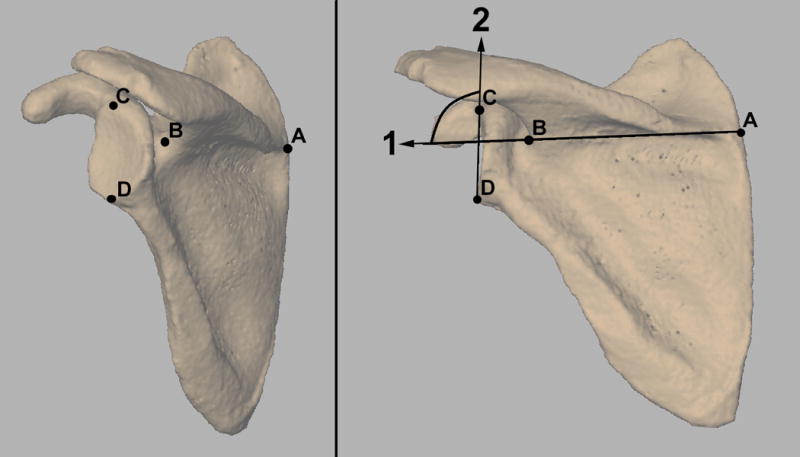
Glenoid inclination angle was calculated as the angle formed between lines 1 and line 2. Line 1 was defined as connecting (A) the intersection of the scapular spine with the scapula's medial border, and (B) the middle of the spinoglenoid notch. Line 2 was defined as connecting (C) the superior-most point on the glenoid rim, and (D) the inferior-most point on the glenoid rim.
Dynamic, in-vivo glenohumeral joint motion was determined by measuring the 3D position of the humerus and scapula from images acquired with a biplane x-ray system during shoulder abduction. To accomplish this, subjects were positioned with their shoulder centered within a biplane x-ray system.11 The system consisted of two 100 kW pulsed x-ray generators (EMD Technologies CPX 3100CV, Quebec) and two 30 cm image intensifiers (Shimadzu AI5765HVP), optically coupled to synchronized high-speed video cameras (Phantom IV, Vision Research, Wayne, NJ). Subjects wore a lead-lined thyroid shield and protective vest during testing to minimize x-ray exposure. Biplane x-ray images were acquired at 60 Hz, while each subject abducted his/her shoulder in the frontal plane from full adduction to approximately 120° of humerothoracic elevation. This motion was performed with each subject holding a 3-pound hand weight or a weight consistent with his/her stage of rehabilitation. Three trials were recorded for each shoulder, both shoulders were tested, and the testing order was randomized.
The 3D positions of the humerus and scapula throughout each trial were measured from the biplane x-ray images using an accurate (±0.4 mm, ±0.5°), model-based tracking technique.3 Using custom software, the 3D locations of major anatomic landmarks were identified on the humeral and scapular models and used to define standard coordinate system axes.14 Consistent with conventional techniques for measuring shoulder motion, translations were expressed in terms of the position of the center of the humeral head relative to the origin of the scapular coordinate system. Using these data, we calculated three specific outcome measures to characterize superior/inferior (S/I) translation of the center of the humeral head relative to the scapula. The outcome measures included humeral head center S/I translation range (HHC RANGE), S/I translation from the adducted starting position to full abduction (HHC ABD), and maximum superior translation relative to the adducted starting position (HHC MAX) (Figure 2). Although these three outcome measures are related, they were specifically chosen, since the S/I position of the humeral head center does not necessarily increase monotonically with shoulder abduction.2
Figure 2.
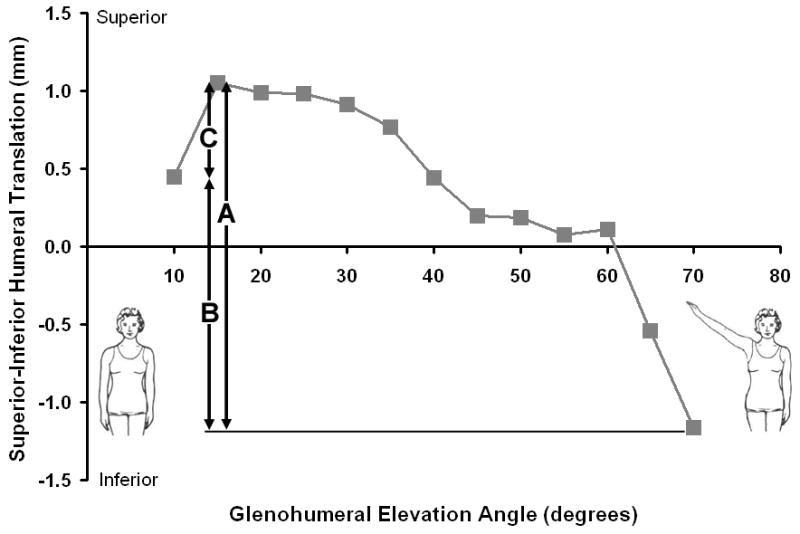
Data from a representative subject showing how the superior-inferior (S/I) position of the humeral head center changes relative to the scapula with elevation angle. S/I motion of the humeral head center was characterized for each subject in terms of: (A) S/I translation range, (B) S/I translation from the adducted starting position to full abduction, and (C) maximum superior translation relative to the adducted starting position.
As an alternative approach for quantifying in-vivo glenohumeral joint translation, we also calculated translation of the center of contact between the articulating surfaces of the humerus and glenoid. This was accomplished using a technique that estimates joint contact patterns by combining joint motion measured from the biplane x-ray images with the subject-specific bone models.1 Specifically, the glenohumeral joint contact center location was determined by first calculating the distance between the articulating surfaces of the humerus and glenoid and then calculating the centroid of the closest 200 mm2 region of contact between the humerus and glenoid. The 3D coordinates of this contact center location were expressed relative to the origin of the scapula coordinate system. These data were calculated for every frame of each trial, producing a contact center path whose position on the glenoid varied as the arm was abducted. Due to differences in glenoid size between subjects, these joint contact data were normalized relative the size of each subject's glenoid. Specifically, the 3D coordinate data were expressed as a percentage of the A/P glenoid dimension and the S/I glenoid dimension (i.e., the distance from point C to D in Figure 1). Using these data, we calculated three specific outcome measures to characterize superior/inferior (S/I) translation of the joint contact center relative to the glenoid. The outcome measures included the contact center S/I translation range (CC RANGE), contact center S/I translation from the adducted starting position to full abduction (CC ABD), and contact center maximum superior translation relative to the adducted starting position (CC MAX) (Figure 3). Although these three outcome measures are related, they were specifically chosen since the S/I position of the joint contact center does not necessarily increase monotonically with shoulder abduction.
Figure 3.
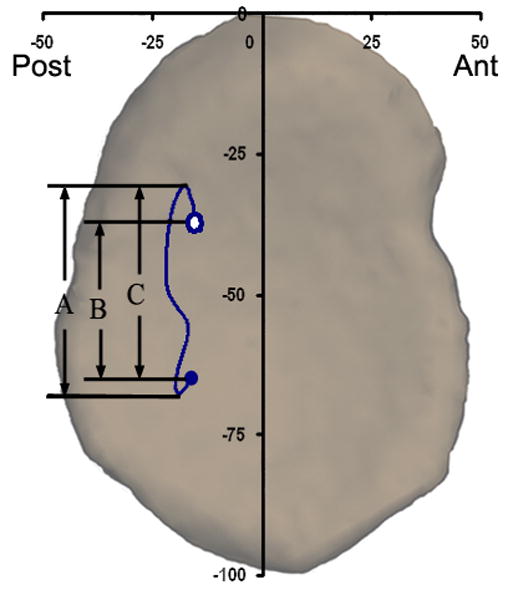
Data from a representative subject showing how the glenohumeral joint contact center position changed during elevation from the adducted starting position (closed circle) to approximately 120° of humerothoracic abduction (open circle). Superior-inferior (S/I) motion of the contact center was characterized for each subject in terms of: (A) S/I translation range, (B) S/I translation from the adducted starting position to full abduction, and (C) maximum superior translation relative to the adducted starting position.
Thus, a total of six measures of in-vivo glenohumeral joint translation were collected. Three of these outcome measures were based on the S/I translation of the center of the humeral head (i.e., HHC RANGE, HHC ABD and HHC MAX), and three of the outcome measures were based on the S/I translation of the glenohumeral joint contact center (i.e., CC RANGE, CC ABD, and CC MAX).
Statistical Analysis
The intraclass correlation coefficient was calculated to determine the reliability of the glenoid inclination measurement. The effect of shoulder condition (repaired vs. contralateral) on glenoid inclination was assessed with a paired t-test. The association between glenoid inclination and each of the six outcome measures of glenohumeral joint translation S/I translation was assessed for only the contralateral shoulder with linear regression and a correlation coefficient. Significance for all statistical tests was set at p < 0.05.
Results
The intraclass correlation coefficient of glenoid inclination angle measurements was 0.94. Glenoid inclination was an average of 1.6 ± 3.3° lower in the repaired shoulder than in the contralateral shoulder (p = 0.04, Figure 4). There was considerable variation across subjects in the difference in glenoid inclination between shoulders. Specifically, the individual results demonstrated that glenoid inclination in the asymptomatic shoulder ranged from 7.4° higher to 5.2° lower than the repaired shoulder (Figure 5). Fourteen subjects had greater glenoid inclination in their asymptomatic shoulder, six had greater glenoid inclination in their repaired shoulder, and one had no difference in glenoid inclination between his repaired and contralateral shoulders (Figure 5).
Figure 4.
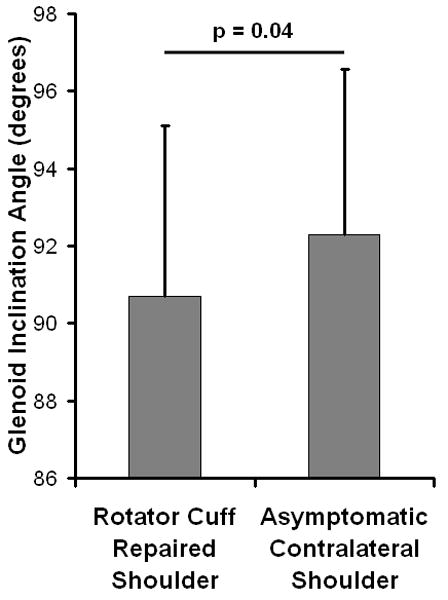
Average (±standard deviation) glenoid inclination in the rotator cuff repaired shoulder was significantly less than in the asymptomatic contralateral shoulder (p=0.04).
Figure 5.
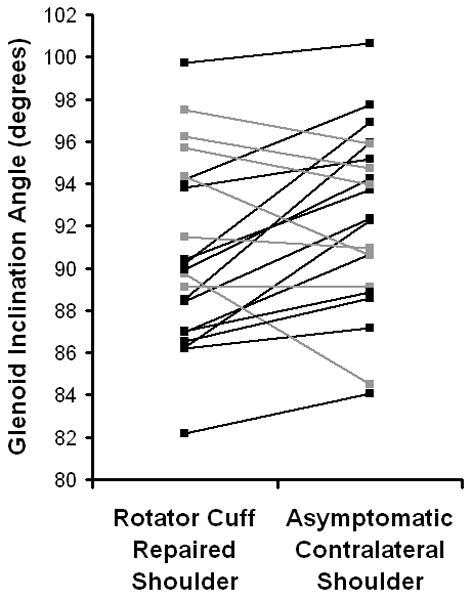
Individual glenoid inclination measurements for each of the 21 subjects. Subjects whose glenoid inclination was highest in the contralateral shoulder are shown in black. Subjects who glenoid inclination in the repaired shoulder was greater than or equal to their contralateral shoulder are shown in gray.
There was a weak association between glenoid inclination and the three measures of S/I translation based on the position of the center of the humeral head (Table 1). Specifically, no statistically significant association was detected between glenoid inclination and HHC RANGE (r = -0.25, p = 0.30), HHC MAX (r = 0.02, p = 0.95), or HHC ABD (r = -0.25, p = 0.30). Similarly, the association between glenoid inclination and the three measures of S/I translation based on the joint contact center data was also weak (Table 1). Specifically, no statistically significant association was detected between glenoid inclination and CC RANGE (r = -0.10, p = 0.67), CC MAX (r = -0.16, p = 0.50), or CC ABD (r = -0.22, p = 0.37).
Table 1.
Association between glenoid inclination and the six specific outcome measures of in-vivo superior/inferior humeral translation. The 95% confidence interval is reported in parentheses below each correlation coefficient. No statistically significant association was found between glenoid inclination and in-vivo superior/inferior humeral translation (p > 0.05).
| Outcome Measure of Superior/Inferior Humeral Translation | Correlation Coefficient (95% Confidence Interval) |
p-value |
|---|---|---|
| HHC RANGE | -0.25 (-0.63, 0.23) |
0.30 |
| HHC MAX | 0.01 (-0.44, 0.47) |
0.95 |
| HHC ABD | -0.25 (-0.63, 0.23) |
0.30 |
| CC RANGE | -0.10 (-0.53, 0.37) |
0.67 |
| CC MAX | -0.16 (-0.58, 0.31) |
0.50 |
| CC ABD | -0.22 (-0.61, 0.26) |
0.37 |
Discussion
The primary objective of this study was to compare glenoid inclination between the repaired and contralateral shoulders of patients who had a unilateral rotator cuff tear. As a secondary analysis, we assessed the association between glenoid inclination and in-vivo glenohumeral joint translation. There was a statistically significant difference in glenoid inclination between the repaired and contralateral shoulders (p = 0.04). However, none of the associations between glenoid inclination and the six measures of S/I glenohumeral translation were found to be statistically significant (p > 0.30).
The finding that glenoid inclination in the rotator cuff tear shoulder (90.7°) was lower than that of the asymptomatic, contralateral shoulder (92.3°) was somewhat surprising, particularly in light of previous research. Specifically, previous research has demonstrated the rotator cuff tears are associated with higher glenoid inclination. This finding has been supported by both cadaveric studies4 and imaging studies involving patients with rotator cuff tears.12 Furthermore, the reported differences in glenoid inclination between specimens or patients with rotator cuff tears and those without cuff tears were not trivial. Hughes and colleagues reported a difference in glenoid inclination of 7.6°,4 while Tetreault and colleagues reported a difference in glenoid inclination of 10°.12 However, in contrast to these findings, a study by Kandemir and colleagues failed to detect any significant difference in glenoid inclination between twelve cadaver specimens with a full-thickness rotator cuff tear and twelve specimens with no injury.5 Thus, there are conflicting results in the literature on the association between glenoid inclination and rotator cuff tears. To our knowledge, the current study is the first investigation to report lower glenoid inclination in patients with rotator cuff tears.
It is possible that the discrepancy in results between this and previous studies on the association between glenoid inclination and rotator cuff tears may be explained, at least in part, by differences in measurement techniques. In particular, two-dimensional (2D) measurement techniques, such as the radiographic images used by Hughes et al4 and the magnetic resonance images used by Tetreault et al12, are likely susceptible to subtle errors in alignment of the specimen or patient relative to the imaging plane. The study by Kandemir and colleagues lends further support to the influence of measurement technique. They found significant differences between measurement techniques when glenoid inclination angle was measured using both 2D (radiographs) and 3D (manual digitizing) techniques.5 The custom software used in the current study for identifying anatomic landmarks operated upon a 3D CT-based bone model, which could be resized (i.e., zoomed) and rotated in three dimensions as needed. Thus, the technique used in this study for calculating glenoid inclination is not susceptible to out-of-plane imaging errors that are inherent to 2D measurement techniques.
As previously mentioned, it has been theorized that glenoid inclination may have a significant impact on the extent to which the humerus translates superiorly relative to the scapula, as supported by cadaveric experiments. Wong and colleagues13 demonstrated that the amount of force required to produce superior humeral head motion decreased as glenoid inclination increased.13 Konrad et al showed a similar result, with superior translation of the humerus decreasing as glenoid inclination decreased.6 Contrary to these findings, our study failed to detect any statistically significant association between glenoid inclination and the six different measures of superior humeral translation. One potential explanation for this discrepancy is that the current study measured glenohumeral joint translation under in-vivo conditions, whereas previous studies were based on cadaveric studies that can not accurately simulate the muscle and joint forces associated with in-vivo conditions. Moreover, it seems overly simplistic to expect that that glenohumeral joint motion is dictated by a single anatomic factor such as glenoid inclination. Indeed, Michener and colleagues have summarized that a wide variety of factors (e.g., muscle activation patterns, muscle fatigue, scapular motion, posture, acromial shape, etc.) likely influence the development of subacromial impingement.7
There are several limitations associated with this study. First, we are assuming that motion of the contralateral shoulder of patients with a unilateral rotator cuff tear is characteristic of normal, healthy shoulders. However, previous research has demonstrated that only a small percentage (7.9% or 58 out of 731 patients) of patients with a unilateral rotator cuff tear have an asymptomatic tear in the contralateral shoulder.16 Furthermore, the contralateral shoulder of each subject was asymptomatic and was verified by an experienced shoulder surgeon to have normal function. Thus, we are comfortable in our assumption that the contralateral shoulder of this patient population provides a reasonable measure of normal shoulder function in a population of patients that is obviously susceptible to rotator cuff tears. Another limitation is that scapulothoracic motion was not quantified. This limitation is based on the biplane x-ray system's field of view, which is dictated by the size of the system's image intensifiers. It is anticipated that future upgrades of our biplane x-ray system will allow us to quantify both glenohumeral and scapulothoracic joint motion simultaneously. Last, we acknowledge that insufficient statistical power is one potential reason for the lack of association between glenoid inclination and superior/inferior glenohumeral joint translation.
In summary, this study detected a significant difference in glenoid inclination between the repaired and contralateral shoulders of patients who had surgical repair of a rotator cuff tear. Using an accurate motion measurement technique, the study failed to detect any significant association between glenoid inclination and in-vivo superior humeral translation during shoulder abduction. This study did not support the theory that glenoid inclination is responsible for superior humeral translation and the development of subacromial impingement.
Acknowledgments
The project was supported by grant number AR051912 from NIH/NIAMS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anderst WJ, Tashman S. A method to estimate in vivo dynamic articular surface interaction. J Biomech. 2003;36(9):1291–9. doi: 10.1016/s0021-9290(03)00157-x. [DOI] [PubMed] [Google Scholar]
- 2.Bey MJ, Kline SK, Zauel R, Lock TR, Kolowich PA. Measuring dynamic in-vivo glenohumeral joint kinematics: Technique and preliminary results. J Biomech. 2007 doi: 10.1016/j.jbiomech.2007.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128(4):604–9. doi: 10.1115/1.2206199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes RE, Bryant CR, Hall JM, Wening J, Huston LJ, Kuhn JE, Carpenter JE, Blasier RB. Glenoid Inclination is Associated With Full-Thickness Rotator Cuff Tears. Clin Orthop. 2003;(407):86–91. doi: 10.1097/00003086-200302000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Kandemir U, Allaire RB, Jolly JT, Debski RE, McMahon PJ. The relationship between the orientation of the glenoid and tears of the rotator cuff. J Bone Joint Surg Br. 2006;88(8):1105–9. doi: 10.1302/0301-620X.88B8.17732. [DOI] [PubMed] [Google Scholar]
- 6.Konrad GG, Markmiller M, Jolly JT, Ruter AE, Sudkamp NP, McMahon PJ, Debski RE. Decreasing glenoid inclination improves function in shoulders with simulated massive rotator cuff tears. Clin Biomech (Bristol, Avon) 2006;21(9):942–9. doi: 10.1016/j.clinbiomech.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon) 2003;18(5):369–79. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50. [PubMed] [Google Scholar]
- 9.Neer CS., 2nd Impingement lesions. Clin Orthop. 1983;(173):70–7. [PubMed] [Google Scholar]
- 10.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58(2):195–201. [PubMed] [Google Scholar]
- 11.Tashman S, Anderst W. In-vivo measurement of dynamic joint motion using high speed biplane radiography and CT: application to canine ACL deficiency. J Biomech Eng. 2003;125(2):238–45. doi: 10.1115/1.1559896. [DOI] [PubMed] [Google Scholar]
- 12.Tetreault P, Krueger A, Zurakowski D, Gerber C. Glenoid version and rotator cuff tears. J Orthop Res. 2004;22(1):202–7. doi: 10.1016/S0736-0266(03)00116-5. [DOI] [PubMed] [Google Scholar]
- 13.Wong AS, Gallo L, Kuhn JE, Carpenter JE, Hughes RE. The effect of glenoid inclination on superior humeral head migration. J Shoulder Elbow Surg. 2003;12(4):360–4. doi: 10.1016/s1058-2746(03)00026-0. [DOI] [PubMed] [Google Scholar]
- 14.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D'Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech. 2002;35(4):543–8. doi: 10.1016/s0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]
- 15.Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, Neviaser RJ. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9(1):6–11. doi: 10.1016/s1058-2746(00)90002-8. [DOI] [PubMed] [Google Scholar]
- 16.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]


