Abstract
The objective of this study was to investigate screening performance measures in the English screening units that began inviting women aged 65–70 between 1 April 2001 and 1 April 2004. We analysed results after each unit commenced inviting women aged 65–70. In addition, we analysed data from units that invited this age group for a second time between 1 April 2004 and 31 March 2007. Results for women aged 65–70 were compared to women aged 50–64 and 60–64. Average uptake was 72.8% for women aged 65–70 and 76.7% for women aged 50–64. For women screened within the last 5 years, uptake was 88.7% for older women and 89.1% for younger women. For women previously screened within 5 years the invasive cancer detection rate was 17% higher in the 65–70 age group than in the 60–64 age group. The rates of recall to assessment and PPV were 3.5 and 27.6% in women aged 65–70 and 3.4 and 24.6% in women aged 50–64 respectively. These results suggest that, as in the earlier demonstration studies, uptake rates remain high in older women, and many more older women attend following an invitation than had previously self-referred. The cancer detection rate is higher in this older age group, whereas rates of recall are generally similar to those in younger women; consequently the PPV is also higher in older women.
Keywords: breast cancer, screening, older women
When the UK NHS Breast Screening Programme (NHSBSP) began in 1988, women aged between 50 and 64 years were invited to three yearly screening, whereas older women were able to self-refer. (Forrest, 1986). A survey in 1995 showed that in many countries women aged up to 69 or 70 are invited to screening (Shapiro et al, 1998). Although breast screening is acknowledged as efficacious for women aged 50–69, when the UK programme commenced there was concern regarding possible lower uptake and reduced cost-effectiveness in older women (Moss et al, 2001). More recently, results from three demonstration studies in England, in which invitations were extended to women aged 65–69, suggested that older women who have previously been routinely screened by the programme had similar uptake patterns to younger women, and screening these women was estimated to be as cost-effective as for the 50–64 age group (Moss et al, 2001). As a result of these studies, the expansion of the programme to invite women up to the age of 70 was announced in the NHS Cancer Plan in 2000 (Department of Health, 2000). The publication also announced the introduction of two-view mammography at the incident screen. English units were expected to have begun this by 2003 and to have started including women aged 65–70 into the routine invitation system by the end of 2004.
The aim of this study was to investigate if the implementation of this policy change gave similar results to those from the demonstration studies. We analysed results from those units that began inviting the 65–70 age group between 1 April 2001 and 1 April 2004 and therefore had completed at least a full 3-year screening round by 31 March 2007.
METHODS
Between April 2001 and April 2004, 36 units in England began inviting women aged between 65 and 70, in addition to women aged 50–64, to screening. These units were distributed throughout England and represented approximately 40% of both the total number of units and of the target population of the screening programme.
Aggregated information on activity and outcomes is reported annually by screening units on statutory KC62 returns, which report on specific cohorts of women; for example data for 2002 relate to women screened between 1 April 2001 and 31 March 2002.
As the majority of women aged 65–70 will have been previously screened, performance measures (rates of recall, cancer detection, benign biopsy and non-operative diagnosis of cancer) were calculated for women who had previously been screened by the programme both within the last 5 years and more than 5 years previously. Uptake of invitation was calculated for all women according to previous screening history. Results for the 65–70 age group were compared with those for both the previous target age range (50–64) and the oldest age group in that range (60–64). The statistical significance of these comparisons was tested using a two-sample test of proportions in Stata version 9.2.
We examined data for each unit for the first 3 complete years after they commenced inviting the 50–70 age group. For example, in a unit beginning to invite the 65–70 age group in August 2003, we used data for the period 1 April 2004 to 31 March 2007. To estimate the increase in the number of older women being screened due to the expansion of invitation to the 65–70 age group, we compared the number of women aged 65–70 screened in this 3-year period with the number of women who self-referred in the 65–69 age group (because data for age 70 were not available before 2003) in the 3 complete years prior to each unit inviting older women.
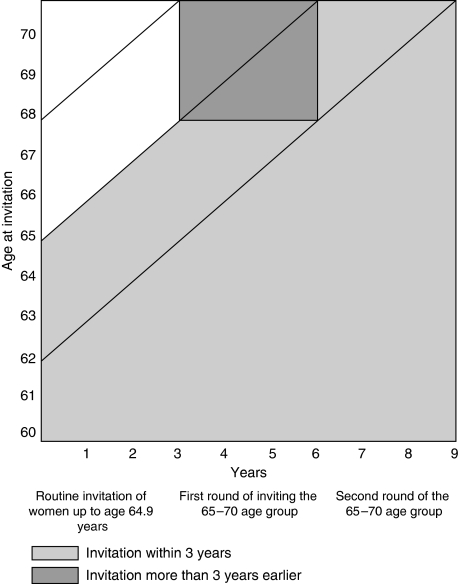
During initial invitation of older women (round 1), those aged between 65 and 67 will have been invited to screening 3 years previously, and are likely to form the majority of women screened within the last 5 years, whereas those aged 68–70 are likely not to have been invited for 6 years and will form the majority of women last screened more than 5 years previously. In addition, for the 23 units that began the expansion between April 2001 and April 2003, we examined data as they began the re-invitation of the 65–70 age group (round 2) to screening, when all women will have been invited to screening within the last 3 years. Figure 1 shows the previous screening history of women aged 65–70 at both rounds 1 and 2 assuming that before the policy change women had received their last invitation between ages 62 and 64.9 years.
Figure 1.
Age at invitation and previous screening history of older women in units commencing invitation of 65–70 age group.
In 2004, an annex was added to the data return providing anonymised individual-based pathology data for all screen-detected cancers. The quality of these data was poor in the first year, and we therefore used data from 2005 onwards. Data on all cancers detected by the screening units during the 3-year period between 1 April 2004 and 31 March 2007 (KC62 year, 2005–2007) were used to calculate the Nottingham Prognostic Index (NPI) in order to compare the prognosis for the 65–70 age group with that of younger women. The index was derived from a series of women with primary breast cancer and uses lymph node status, tumour size and pathological grade. From this series three subsets of patients were identified; those with a good prognosis, a moderate prognosis and a poor prognosis (survival at 10 years after diagnosis was 88, 60 and 18% respectively) (Blamey, 2002).
RESULTS
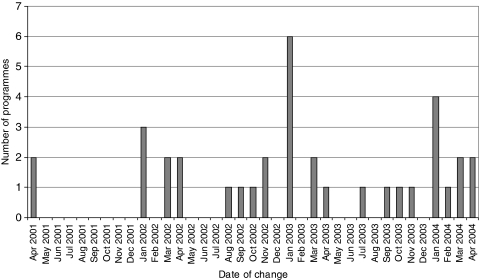
The dates when the 36 units began inviting women up to the age of 70 are shown in Figure 2. Units commencing between April 2001 and April 2003 began re-inviting the 65–70 age group between April 2004 and April 2006. Although two units commenced inviting the 65–70 age group in April 2001, the majority of the units began in 2003. By this time approximately 60% of the units had already started taking two views at the incident screen, and a further third started at the same time; therefore most women invited by the units would have had two mammographic views taken.
Figure 2.
Start date for programmes commencing to invite 65–70 age group between April 2001 and April 2004.
A total of 516 213 women aged 65–70 were invited to screening in the first round, and 201 589 in the second round. Uptake for this age group was 72.8% at both rounds. Average uptake in the two rounds was 76.7%, and 76.8% for the 50–64 and 60–64 age groups respectively. The number of older women screened in the first round was more than five times the number (67 546, aged 65–69) who self-referred in these units in the 3 years prior to them beginning to invite older women.
Table 1 shows the uptake rates by age group, invitation type and round. A percentage of women aged 65–70 were invited for the first time. (Reasons for this may include women moving to the UK, previously screened women moving to a new area whose screening history was not forwarded from their old area and women previously recorded as ineligible now being invited). At the first round, the 65–70 age group demonstrated similar patterns of uptake to women aged 60–64, except for those women whose last screen was more than 5 years ago, whose uptake was higher (66.6 vs 46.0%). The results may reflect the fact that the older women in the 65–70 age group would not have been invited for 6 years. A proportion of older women in this age group will have been screened more recently as a result of self-referral, and this may explain why more than half of the 65–70 age group had been screened within the last 5 years. At the second round, for women screened more than 5 years previously, the older age group showed a similar pattern of uptake to the 60–64 age group; all these women will have been non-attenders at their last invitation.
Table 1. Uptake of screening according to invitation type and screening round.
| First round of inviting 65–70 age group | Second round of inviting 65–70 age group | Overall | ||||
|---|---|---|---|---|---|---|
| Invitation type | Invited | Uptake (%) | Invited | Uptake (%) | Invited | Uptake (%) |
| First invitation | ||||||
| 50–64 | 360 432 | 74.0 | 130 075 | 73.0 | 490 507 | 73.7 |
| 60–64 | 7836 | 35.3 | 2713 | 36.8 | 10 549 | 35.7 |
| 65–70 | 8209 | 31.7 | 2269 | 30.1 | 10 478 | 31.4 |
| Previously invited never screened | ||||||
| 50–64 | 194 771 | 21.0 | 77 044 | 19.7 | 271 815 | 20.6 |
| 60–64 | 50 689 | 10.1 | 20 590 | 9.6 | 71 279 | 9.9 |
| 65–70 | 50 349 | 8.5 | 18 599 | 6.6 | 68 948 | 8.0 |
| Previous screen ⩽5 years | ||||||
| 50–64 | 1 244 889 | 89.3 | 471 812 | 88.6 | 1 716 701 | 89.1 |
| 60–64 | 434 364 | 89.8 | 175 411 | 89.5 | 609 775 | 89.7 |
| 65–70 | 288 718 | 88.9 | 147 893 | 88.3 | 436 611 | 88.7 |
| Previous screen >5 years | ||||||
| 50–64 | 128 460 | 51.5 | 50 399 | 49.9 | 178 859 | 51.1 |
| 60–64 | 61 404 | 46.0 | 25 054 | 44.9 | 86 458 | 45.7 |
| 65–70 | 168 937 | 66.6 | 32 828 | 43.7 | 201 765 | 62.8 |
The overall recall to assessment rate in the 65–70 age group was 3.4% for women screened within the last 5 years and was similar to the 60–64 age group at both rounds (Table 2). For women screened more than 5 years previously the rate was 5.2% in the older age group. This was similar to rates in the younger age groups at the first round but at the second round rates decreased in both the 50–64 and 60–64 age groups but remained higher in the 65–70 age group.
Table 2. Rates of recall to assessment and cancer detection by screening round, previous screening history and age group.
|
Cancer detection rate per 1000 women screened
|
|||||
|---|---|---|---|---|---|
| No of women screened | Recalled to assessment (%) | Invasive cancers | In situ cancers | Small (<15 mm) cancers | |
| First round of inviting 65–70 age group | |||||
| Women previously screened ⩽5 years ago | |||||
| 50–64 | 1 111 069 | 3.4 | 5.3 | 1.4 | 2.9 |
| 60–64 | 390 198 | 3.4 | 6.6 | 1.6 | 3.7 |
| 65–70 | 256 671 | 3.5 | 7.8 | 1.7 | 4.4 |
| Women previously screened >5 years ago | |||||
| 50–64 | 66 172 | 5.2 | 8.1 | 2.1 | 4.4 |
| 60–64 | 28 220 | 5.4 | 9.0 | 2.3 | 5.0 |
| 65–70 | 112 432 | 5.2 | 12.0 | 2.6 | 6.2 |
| Second round of inviting 65–70 age group | |||||
| Women previously screened ⩽5 years ago | |||||
| 50–64 | 417 983 | 3.1 | 5.1 | 1.4 | 2.9 |
| 60–64 | 156 971 | 3.1 | 6.2 | 1.5 | 3.6 |
| 65–70 | 130 594 | 3.1 | 7.2 | 1.6 | 4.4 |
| Women previously screened >5 years ago | |||||
| 50–64 | 25 146 | 4.8 | 7.7 | 2.2 | 3.8 |
| 60–64 | 11 255 | 4.5 | 8.5 | 2.0 | 3.9 |
| 65–70 | 14 339 | 5.3 | 11.6 | 2.4 | 5.4 |
The average invasive cancer detection rate in the 65–70 age group was 7.6 per 1000 in women screened within the last 5 years and 12.0 per 1000 in women screened at a longer screening interval (Table 2). Both were significantly (P<0.001) higher than rates in the 60–64 age group (6.5 per 1000 women screened and 8.9 per 1000 women screened respectively).
The in situ cancer detection rate was similar in the 60–64 and 65–70 age groups; 1.6 per 1000 women screened versus 1.7 per 1000 women screened for women screened within 5 years and 2.2 per 1000 women screened versus 2.6 per 1000 women screened in women screened more than 5 years ago (Table 2).
In women screened within the last 5 years the small (<15 mm) invasive cancer detection rate was significantly (P<0.001) higher in the 65–70 age group than the 60–64 age group (4.4 per 1000 women screened vs 3.7 per 1000 women screened) (Table 2). Rates were also higher in older women screened more than 5 years ago but the rates decreased from the first to the second round in all age groups (unlike in women screened within the last 5 years where they remained stable).
The percentage of small (<15 mm) invasive cancers was 55% in the 50–64 age group, 57% in the 60–64 age group and 58% in the 65–70 age group for women screened within the last 5 years. For women screened more than 5 years previously the percentages were 53, 52 and 51% respectively.
The positive predictive value of recall to assessment (PPV) was significantly (P<0.001) higher in the 65–70 age group than the 60–64 age group for women screened both within the last 5 years (27.6 vs 24.6%) and those with a longer screening interval (28.3 vs 21.8%).
Rates of benign surgical biopsies for the 65–70 age group were 0.06% in women screened within 5 years and 0.10% for women screened more than 5 years previously. These were similar to those in the 50–64 and 60–64 age groups. The overall percentages of cancers with a non-operative diagnosis of cancer were also similar between the 60–64 and 65–70 age groups with 95.1% of older women screened within 5 years receiving a non-operative diagnosis of cancer and 94.8% who were screened more than 5 year previously.
Table 3 shows the proportion of cancers (including those with an unknown lymph node status) falling into each of the diagnostic categories of the NPI. The proportion of cancers in older women with a good prognosis was similar to that in the 60–64 age group.
Table 3. NPI (prevalent and incident screens combined) by age group.
|
Good
|
Moderate
|
Poor
|
Not known
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | No | % | Total | |
| 50–54 | 1313 | 55 | 891 | 37 | 136 | 6 | 65 | 3 | 2405 |
| 55–59 | 1503 | 53 | 1058 | 37 | 192 | 7 | 89 | 3 | 2842 |
| 60–64 | 1715 | 58 | 1007 | 34 | 147 | 5 | 112 | 4 | 2981 |
| 65–70 | 2023 | 59 | 1110 | 32 | 165 | 5 | 128 | 4 | 3426 |
DISCUSSION
Although units included in this study began including women aged 65–70 in the invitation system between April 2001 and April 2004, most began inviting older women after December 2002; results from the first invitation of the 65–70 age group therefore mainly represented activity between 1 April 2003 and 31 March 2007, whereas the results for the re-invitation of the 65–70 age group were based on units that began earlier and represent activity mainly between 1 April 2005 and 31 March 2007. The re-invitation of the age group only represents a full 3-year screening round for 2 out of the 23 units. However, average performance measures in England between April 2003 and March 2007 were stable apart from recall rate which has decreased.
The results of this study showed that although uptake was lower in women aged 65–70 than in women aged both 50–64 and 60–64 for all age groups, it was more than the 70% minimum target set by the programme (NHS Breast Screening Programme, 2005). The results are similar to those from the English demonstration studies and results from screening programmes in both Denmark and the Netherlands, which also invite women aged 65–69 and report more than 70% of women accepting an invitation to screening (Sarkeala et al, 2004).
The invasive cancer detection rate in women screened both within 5 years and more than 5 years previously and the small invasive cancer detection rate in women screened more than 5 years ago both decreased between the first and second rounds. At the first round, in the 50–64 age group, these rates were higher than the English average and thus results at the second round, although based on fewer data, may better reflect rates as units continue to invite women aged 65–70.
As in the demonstration studies, the rise in breast cancer incidence with age was reflected in the increased invasive cancer detection rate in the 65–70 age group. However rates of both small and overall invasive cancers in all age groups were higher in this study than in the demonstration studies, probably as a result of units now using two-view mammography at all incident screens. However, a slower rate of tumour growth is suggested by an increased mean sojourn time in the older age group (Tabar et al, 2000), this may suggest an increasing chance of overdiagnosis in the older age group due to increasing all-cause mortality.
As a result of the increased invasive cancer detection rate in the 65–70 age group, and low rates of recall to assessment, the PPV increased in older women. However, results from further units will be watched with interest. The demonstration studies showed a lower rate of recall in the older age group, although the Netherlands, which has always invited the 50–70 age group, has shown an increase in recall rate, as well as PPV and cancer detection, with increasing age (National Evaluation Team for Breast Cancer Screening, 2005).
In 2002, an IARC working group concluded, given the evidence from randomised controlled trials, that breast screening programmes should target women aged 50–69 (IARC Working Group on the Evaluation of Cancer-Preventive Strategies, 2002). Some countries now routinely invite women aged over 70; women are invited up to 74 years in Sweden and 75 years in the Netherlands. In England, the recent publication of the Cancer Reform Strategy announced the further expansion of the NHSBSP to women aged 47–73 years (Department of Health, 2007). The results from this observational study of extending the upper age limit to 70 have shown that although women above the age of invitation are able to self-refer, the number doing so is far fewer than the number of women in the same age group who attend following an invitation. Consequently, current rates of self-referral in women aged 71–73 should not be used to predict future uptake in this age group. The effect on resources of the further extension of the programme is likely to be considerable if uptake for both the 71–73 and 47–49 age groups is similar to the 50–70 age group.
Calculation of the NPI
The index was calculated using the formula: size (cm) × 0.2+lymph node status (1–3)+grade (Haybittle et al, 1982). An index using a revised formula (size (cm) × 0.42+grade × 0.78) was calculated for cancers with unknown lymph node status (The Breast Screening Frequency Trial Group, 2002).
Acknowledgments
We are grateful to the NHS Cancer Screening Programmes for providing data for this study. This work forms part of a programme of independent research by the CSEU, which is funded by the Policy Research Programme of the Department of Health. The views are those of the authors and not necessarily those of the Department of Health.
References
- Blamey RW (2002) Estimation of prognosis of the individual with primary breast cancer and its applications. Scand J Surg 91: 273–278 [DOI] [PubMed] [Google Scholar]
- Department of Health (2000) The NHS Cancer Plan. A Plan for Investment. A Plan for Reform. Department of Health: London [Google Scholar]
- Department of Health (2007) Cancer Reform Strategy. Department of Health: London [Google Scholar]
- Forrest APM (1986) Breast Cancer Screening: Report to the Health Ministers of England, Wales, Scotland and Northern Ireland. HMSO: London [Google Scholar]
- Haybittle JL, Blamey RW, Elston CW, Johnson J, Doyle PJ, Campbell FC, Nicholson RI, Griffiths K (1982) A prognostic index in primary breast cancer. Br J Cancer 45: 361–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC Working Group on the Evaluation of Cancer-Preventive Strategies (2002) IARC Handbooks of Cancer Prevention: Breast Cancer Screening. IARC: Lyon [Google Scholar]
- Moss SM, Brown J, Garvican L, Coleman DA, Johns LE, Blanks RG, Rubin G, Oswald J, Page A, Evans A, Gamble P, Wilson R, Lee L, Liston J, Sturdy L, Sutton G, Wardman G, Patnick J, Winder R (2001) Routine breast screening for women aged 65–69: results from evaluation of the demonstration sites. Br J Cancer 85: 1289–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Evaluation Team for Breast Cancer Screening (2005) Landelijke evaluatie van bevolkingsonderzoek naar borstkanker in Nederland. Erasmus MC: Rotterdam [Google Scholar]
- NHS Breast Screening Programme (2005) Consolidated Guidance on Standards for the NHS Breast Screening Programme. NHSBSP Publications: Sheffield [Google Scholar]
- Sarkeala T, Anttila A, Forsman H, Luostarinen T, Saarenmaa I, Hakama M (2004) Process indicators from ten centres in the Finnish breast cancer screening programme from 1991 to 2000. Eur J Cancer 40: 2116–2125 [DOI] [PubMed] [Google Scholar]
- Shapiro S, Coleman EA, Broeders M, Codd M, de Koning H, Fracheboud J, Moss S, Paci E, Stachenko S, Ballard-Barbash R (1998) Breast cancer screening programmes in 22 countries: current policies, administration and guidelines. International Breast Cancer Screening Network (IBSN) and the European Network of Pilot Projects for Breast Cancer Screening. Int J Epidemiol 27: 735–742 [DOI] [PubMed] [Google Scholar]
- Tabar L, Vitak B, Chen HH, Duffy SW, Yen MF, Chiang CF, Krusemo UB, Tot T, Smith RA (2000) The Swedish Two-County Trial twenty years later. Updated mortality results and new insights from long-term follow-up. Radiol Clin North Am 38: 625–651 [DOI] [PubMed] [Google Scholar]
- The Breast Screening Frequency Trial Group (2002) The frequency of breast cancer screening: results from the UKCCCR Randomised Trial. Eur J Cancer 38: 1458–1464 [DOI] [PubMed] [Google Scholar]