Abstract
Objectives
We examine whether multiple health-related quality of life (HRQoL) measures are stratified by socioeconomic status (SES) and age in the United States.
Methods
Data are from the 2005/2006 National Health Measurement Study, a telephone survey of a nationally representative sample of U.S. adults. We plot mean HRQoL scores by SES within age groups. Regression analyses test whether education, income, and assets each have independent associations with three “preference-based” HRQoL measures and self-rated health (SRH). We test whether these associations vary by age.
Results
There are SES disparities in HRQoL and SRH among adults in the United States at all age groups. Income differentials in HRQoL are strong across current adult age cohorts, except the 75–89 age cohort. Education and assets have statistically significant but weaker associations with HRQoL. All three SES measures are associated with SRH (net of each other) at every age group. Those in the lowest income and education groups in the 35–44 age cohort have worse HRQoL and SRH than those in higher SES groups in the 65+ age cohort.
Discussion
Significant improvements in HRQoL at the population level will only be possible if we improve the HRQoL of people at the lowest end of the socioeconomic distribution.
Keywords: Health disparities, Health-related quality of life, Health status, Socioeconomic status
SINCE the 1980s, rates of functional limitations and disabilities have declined among older adults (Crimmins & Saito, 2001; Freedman, Martin, & Schoeni, 2002; Manton & Gu, 2001), and self-reported health has improved as well (Martin, Schoeni, Freedman, & Andreski, 2007; Soldo, Mitchell, Tfaily, & McCabe, 2006). Although reports of these trends have painted an increasingly optimistic picture of health at older ages, research also demonstrates that not all older adults are postponing significant morbidity and disability. Indeed, people with lower socioeconomic status (SES) have worse health in all adult age groups, including at older ages (House et al., 1994; House, Lantz, & Herd, 2005). Research reports and media attention that summarize only overall or mean trends in improved health among older adults mask important SES disparities in health that persist at older ages.
Although research has documented socioeconomic disparities in various measures of morbidity and mortality, there has been little attention paid to the socioeconomic stratification of health-related quality of life (HRQoL). However, “preference-based” HRQoL measures are increasingly used in both clinical studies and cost-effectiveness studies, nationally and internationally, though they have only recently appeared in population-based studies that examine health disparities in the United States (Fryback et al., 2007). Preference-based HRQoL measures were originally created to measure overall health states and were weighted by an average community or societal valuation of how good or bad it would be to have given health states. If there is great socioeconomic stratification in HRQoL, as there is with other measures of morbidity and mortality, it would suggest that future research on HRQoL in clinical, cost-effectiveness, and population studies should attend to not only examining mean levels of HRQoL but also disparities in HRQoL.
The current study uses a recent, large national data set to describe how SES is related to HRQoL and how this relationship varies by age among U.S. adults. This study extends prior work in a number of ways. First, the data were collected in 2005/2006, allowing us to examine SES and age variations in HRQoL using current data. Second, we use three SES measures (income, education, and assets) to examine how patterns vary by each of these measures separately and simultaneously. Third, we include three preference-based HRQoL measures, along with the commonly used self-rated health (SRH) item, to examine similarities and differences in patterns of stratification across these measures.
BACKGROUND
Stratification of Health by SES and Age
Our research is informed by social stratification and life course theories. One contemporary social stratification theory, the “fundamental cause theory” (Link & Phelan, 1995), aims to address why there are strong, consistent associations between SES and health in the United States (Adler & Rehkopf, 2008), why these associations persist across time and measure, and why these associations persist despite attempts to improve health in the United States. Fundamental cause theory suggests that SES shapes exposures to a variety of psychosocial and material conditions that more directly impact health (House et al., 2005; Link & Phelan). This theory emphasizes, however, that SES-related resources, such as knowledge, money, power, and prestige, are flexible resources that allow people to avoid risks and adopt protective strategies no matter which psychosocial and material risk and protective factors are closely aligned with health at a given time (House et al., 2005; Link & Phelan). Therefore, addressing the particular risk and protective factors that currently link SES to health will not eliminate the association between SES and health because those at the top of the socioeconomic hierarchy will find new ways to use their flexible resources to gain advantages that result in better relative health status.
Life course theories have been combined with social stratification theories in a variety of ways to conceptualize how relationships between SES and health vary, change, and accumulate over time. Cumulative advantage/disadvantage hypotheses would predict that we should see larger SES disparities in health at older than at younger ages. Consistent with a fundamental cause theory, this hypothesis suggests that experiences of advantage/disadvantage shape both short- and long-term health, and the accumulation of advantage/disadvantage over the life course ultimately leads to increasing heterogeneity at older ages (Dannefer, 2003; Hatch, 2005; Lauderdale, 2001; O'Rand, 1996; Ross & Wu, 1996).
In contrast, the “age-as-leveler” hypothesis suggests that the relationship between SES and health should look smaller at older ages. This hypothesis reflects a number of both theoretically and methodologically based ideas. From a theoretical standpoint, House and colleagues (1994) describe a theory of social stratification of aging and health that posits that social and biological factors affect both exposure to and impact of material and psychosocial conditions over the life course. Consistent with a fundamental cause theory, socioeconomic differences in exposure to risk factors may increase through adulthood and accumulate to affect health particularly through middle and older ages. However, in later older ages, biological frailty may become strong enough to level the playing field. Age-associated biological frailty may make older adults particularly vulnerable to exposure to risk factors, reducing socioeconomic differentiation in health in later old age. Data consistent with the age-as-leveler hypothesis show that SES disparities in health are smallest at younger ages, widest at middle and early older ages, and smaller again at later old ages in national surveys conducted in the mid 1980s (Deaton & Paxson, 1998; House et al., 1994, 2005; Robert & House, 1996).
In a recent study, Dupre (2007) combined the cumulative advantage/disadvantage hypothesis and the age-as-leveler hypothesis, suggesting that they are not contradictory. Although cumulative advantage/disadvantage processes on an individual level produce disparate onset and survival over time, this individual process ultimately results in aggregate-level findings of smaller SES disparities in health at later old ages. Accumulated disadvantage over the life course produces selective mortality, leaving many robust low SES survivors in the population at later old ages. The age-as-leveler phenomenon also may be partly due to improved social, economic, and health policies at older ages that buffer the effects of low SES on health (House et al., 2005). Moreover, methodological explanations may contribute to the age-as-leveler phenomenon because of weak measurement of SES and health (Robert & House, 1996) or the exclusion of nursing home residents from surveys, which essentially exclude the sickest and lowest SES older adults.
Understanding the relationships between SES and health over the life course is further complicated by the fact that different dimensions of SES are theorized to affect health in both overlapping and separate ways and at different points in the life course (Luo & Waite, 2005). In adulthood, one's own education and income are theorized to have both joint and separate effects on health. Although one of the pathways linking education to health is through its impact on income, education also has independent effects on health through shaping knowledge of health behaviors, sense of control, and greater preferences for health (Grossman, 1972; Ross & Wu, 1996). Education may be most important in affecting the onset of disease and disability (Herd, Goesling, & House, 2007; House et al., 2005; Melzer, Izmirlian, Leveille, & Guralnik, 2001; Ross & Wu, 1996), whereas income may most strongly affect the progression of disease (Feinglass et al., 2007; Herd et al., 2007; House et al., 2005).
Most U.S. research examines income and education as separate measures of SES but does not address wealth (Pollack et al., 2007), despite the potential importance of wealth to health (Baum, 2007; Pollack et al., 2007), and evidence that it may be strongly associated with health among older adults (Robert & House, 1996). Indeed, wealth may be a good marker for cumulative advantage over the life course. People making it into older age with high levels of wealth likely had (a) a trajectory of financial accumulation positively associated with health throughout adulthood and (b) no major health or economic shock that significantly depleted assets (Kim & Lee, 2006; Lee & Kim, 2003).
The current study describes associations among multiple measures of SES and HRQoL and examines how these relationships vary by age group in the United States. From a fundamental causes perspective, we expect to see that multiple measures of SES are associated with HRQoL, just as they have been shown to be associated with unidimensional measures of health. We also expect that SES will be associated with HRQoL at all ages but that the size of this association may vary by age. Although we do not have the longitudinal data to test cumulative advantage/disadvantage versus age-as-leveler hypotheses, we will examine whether there is more support for one hypothesis over the other. Prior research has not looked at how preference-based HRQoL measures are stratified by both age and SES in the United States, so it is important to see if these patterns look similar or different from patterns noted using unidimensional health measures.
Most of the social gerontology literature, and indeed most of the research on social stratification and health in the United States more generally, have not used multidimensional measures of health (Alwin & Wray, 2005), let alone preference-based HRQoL measures. Therefore, one goal of this study is to more generally introduce preference-based HRQoL measures to a readership that has not extensively employed these measures. We believe that social gerontologists need to contribute to important discourse over strengths and weaknesses of employing preference-based HRQoL measures in future clinical, cost-effectiveness, and population-based studies. Therefore, we first provide a general introduction to preference-based HRQoL measures before describing our study.
Background of Preference-Based HRQoL Measures
Health is a complex concept to define and measure. Although there are various separate measures of disease states and disability, HRQoL measures were originally established to quantify overall health by combining observations of various domains of health (e.g., pain, physical function, social function, and mental health) into one summary index. However, this is a difficult task, as it is hard to determine how to weight different health domains in relation to each other because individuals have different preferences regarding trade-offs among health domains. For example, who should be considered worse off—someone with a functional disability and significant pain or someone with depression and inability to perform social roles? Therefore, preference-based HRQoL measures were originally created to go beyond existing HRQoL measures. Preference-based HRQoL measures not only capture multiple domains of health, but also take the next step to combine them in an index that weights more heavily some domains over others, as measured by community or societal valuation of health domain trade-offs.
Creating preference-based HRQoL measures is a three-step process (Feeny et al., 2002; Fryback et al., 2007). First, data are gathered to identify important functional (e.g., physical function, mobility, social function) and experiential (e.g., pain) domains and to create categorical scales for each domain ranging from extremely bad health to full health. A specific combination of one level from each measured domain defines a health state. The second step is to create a scoring system for health states such that full or perfect health is scored at 1.0, and states judged equivalent to being dead are scored at 0.0. This is done by having a representative sample of people evaluate and rate a selected set of unique health states and then using econometric models to derive a scoring function that represents the sample's average valuations of these health states. Once this scoring function is established, the third step is to collect data from individuals to determine their health states and then to assign them each a preference-based HRQoL score that weights their health states by the scoring function. Preference-based HRQoL measures provide a summary score anchored at 0 (as bad as being dead) and 1 (perfect health) (Feeny et al.; Fryback et al.).
One strength of preference-based HRQoL measures is that they can be used both in clinical studies to track health outcomes and in large, population-based surveys to track trends in the HRQoL of populations. This includes the ability to track not just poor health but exceptionally good health as well (Kaplan et al., 2008). Moreover, preference-based HRQoL measures are the outcome measure of choice for cost-effectiveness analyses in clinical and policy-based studies (e.g., McHorney, 1999; Miller, Robinson, & Lawrence, 2006). Given their increased use, we need to understand how HRQoL varies for subgroups of the population, such as by age and SES.
In the United States, research has shown that preference-based HRQoL scores are lower in older versus younger age groups (e.g., Hanmer, Lawrence, Anderson, Kaplan, & Fryback, 2006; Lubetkin, Jia, Franks, & Gold, 2005). Research also shows that higher SES is associated with higher HRQoL in the United States (Lubetkin et al.). However, we know of no population-based U.S. research that has examined the stratification of HRQoL by both SES and age. In one Canadian study, education, income, and occupation were associated with one measure of HRQoL, and this association was larger at late middle ages than at either younger or older ages (Roberge, Berthelot, & Wolfson, 1995). We extend this work by using a national rather than regional sample, a U.S. sample, and multiple measures of HRQoL.
Our study examines age variations in the relationships among multiple measures of SES and three commonly used preference-based HRQoL measures: the SF-6D (Brazier, Roberts, & Deverill, 2002), the European Quality of Life (EuroQol) 5-domain survey (EQ-5D) (Johnson, Luo, Shaw, Kind, & Coons, 2005; Kind, 2007), and the Health Utilities Index Mark 3 (HUI3) (Feeny et al., 2002; Horsman, Furlong, Feeny, & Torrance, 2003). Although the three preference-based HRQoL indexes are each designed to measure the value of a given health state, research has found that these measures vary somewhat in the same population (Fryback et al., 2007). Therefore, we use and compare three measures of preference-based HRQoL as well as the traditional SRH item (Idler, Russell, & Davis, 2000) so that (a) we can examine consistency of patterns and (b) our results can be compared with future research using other data sets that may have only one of these measures.
Study Aims
Our first aim is to examine whether multiple HRQoL measures are stratified by SES among adults in the United States. We also examine whether the relationship between SES and HRQoL varies by measure of SES and whether multiple measures of SES each contribute independently to explaining variation in HRQoL. Our second aim is to examine whether there are age variations in the relationship between SES and HRQoL and whether such patterns are consistent with cumulative advantage/disadvantage versus age-as-leveler hypotheses.
METHODS
Data
Data are from the National Health Measurement Study, a random-digit–dial telephone survey of a nationally representative sample of 3,844 noninstitutionalized U.S. adults in the 48 contiguous states, aged 35–89 years, with over-samples of telephone exchanges with high percentages of African Americans and of people older than 65 years (Fryback et al., 2007). The survey was conducted between June 2005 and August 2006, with a simple response rate of 46%. SRH was asked early in the survey, followed by randomly ordered questionnaire sets used to compute scores for different preference-based HRQoL measures. Sampling weights were computed based on the sample selection algorithm and adjusted by poststratification to reflect the targeted 2000 Census population by age, gender, and race. We excluded from analyses 181 respondents (4.7%) reporting their race as neither White nor Black (people reporting Hispanic ethnicity were included if their race was reported as White or Black). The weighted results are generalizable to the U.S. noninstitutionalized adult population aged 35–89 years in the 48 contiguous states for people reporting their race as White or Black.
Measures
We categorize age groups as 35–44, 45–54, 55–64, 65–74, and 75–89 years. Self-reported race is categorized as either Caucasian/White (White) or Black/African American (Black). Income reflects household income over the previous year and was grouped into four categories: <$20,000, $20,000–34,999, $35,000–74,999, and $75,000 or more. Education was grouped into four categories: less than high school, high school graduate, some postsecondary education, and a college degree or higher. Our measure of wealth is referred to as household assets, measured by asking people: “Suppose you needed money quickly, and you (and your spouse) cashed in all of your checking and savings accounts, any stocks and bonds, and real estate other than your home. If you added up what you got, would this be . . . (provided dollar ranges)?” We coded household assets as <$25,000, $25,000–99,999, and $100,000 or more. Although this is a crude measure of assets, there are no additional wealth variables available, and we argue that having some measure of wealth (or virtual lack of any wealth) is important to examine. Similar crude assets measures have demonstrated associations with health in prior studies (Robert & House, 1996), but we will be cautious about interpretations using this measure. Table 1 describes the sample and independent variables.
Table 1.
Distributions of Variables From the National Health Measurement Study Among Respondents Reporting Their Race as White or Black (n = 3,663)
| Unweighted |
Weighted |
||
| Variables | N | % | % |
| Gender | |||
| Male | 1,554 | 42.4 | 46.4 |
| Female | 2,109 | 57.6 | 53.6 |
| Age group (years) | |||
| 35–44 | 593 | 16.2 | 30.8 |
| 45–54 | 785 | 21.4 | 23.8 |
| 55–64 | 664 | 18.1 | 20.4 |
| 65–74 | 922 | 25.2 | 14.4 |
| 75+ | 699 | 19.1 | 10.7 |
| Race | |||
| White | 2,569 | 70.1 | 88.5 |
| Black | 1,095 | 29.9 | 11.5 |
| Education (highest level) | |||
| <High school | 432 | 11.8 | 8.0 |
| High school graduate | 1,121 | 30.6 | 28.7 |
| Some post–high school | 825 | 22.5 | 22.3 |
| 4-Year college degree or more | 1,285 | 35.1 | 41.0 |
| Household income | |||
| <$20,000 | 882 | 24.1 | 12.1 |
| $20,000–$34,999 | 752 | 20.5 | 15.9 |
| $35,000–$74,999 | 1,184 | 32.3 | 35.8 |
| $75,000+ | 845 | 23.1 | 36.2 |
| Household assets | |||
| <$25,000 | 1,428 | 39.0 | 33.6 |
| $25,000–$99,999 | 1,211 | 33.1 | 32.6 |
| $100,000+ | 1,024 | 28.0 | 33.9 |
Note: Percentages may not sum to 100 due to rounding.
The EQ-5D is a widely used measure of HRQoL (Kind, 2007), particularly in Europe, but increasingly in the United States (Johnson et al., 2005). The EQ-5D instrument involves five questions about respondent's health today in five domains: mobility, self-care, usual activities, pain, and anxiety/depression, with each question having three possible responses: no, moderate, and severe problem (Rabin & de Charro, 2001). The unique combinations of these five components define 243 health states, which were then transformed to summary scores (ranging from −0.11 to 1.00) by applying population-based preference weights created by Shaw, Johnson, and Coons (2005) using a population sample of about 4,000 U.S. adults.
The SF-6D is a preference-based measure of HRQoL derived from the proprietary SF-36v2™, a widely used multipurpose health survey. The SF-6D comes from a subset of 11 of the 36 questions asked in the SF-36v2 (Brazier et al., 2002). The SF-6D includes six domains (physical function, role limitation, social function, pain, mental health, and vitality), each having between four and six levels, resulting in a total of 18,000 unique health states. The scoring algorithm for the summary score comes from a U.K. population sample, as distributed by the SF-36v2 vendor, and ranges from 0.30 to 1.0.
The HUI3 is a preference-based HRQoL measure that has been widely used as an outcome measure in clinical studies and population health surveys and in economic evaluations (e.g., Feeny et al., 2002; Horsman et al., 2003). The interviewer-administered version involves 40 questions regarding respondents’ health over the last week in eight domains: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain. Each domain has either five or six levels, resulting in 972,000 unique health states. The summary score was created using a scoring algorithm (Feeny et al., 2002), including health states valued as worse than dead (<0), ranging from −0.36 to 1.0.
The SRH question was phrased: “In general, would you say your health is: Excellent, very good, good, fair, or poor?” We use it as an ordinal scale ranging from 1 (poor health) to 5 (excellent health). This measure has been included in a number of large national surveys, and despite this question's simplicity, it is usually a robust predictor of later health outcomes (Idler et al., 2000), including disability and mortality (Idler & Benyamini, 1997; Idler & Kasl, 1995; Kaplan, Berthelot, Feeny, McFarland, & Khan, 2007).
Analyses
In order to examine age variations in the relationship between SES and HRQoL, we first graphed mean values of each of the HRQoL and SRH variables within SES and age groups. Analyses of variance (ANOVAs) were performed to test SES differences in HRQoL and SRH scores, both for the full sample and within each age group, with no control variables. Analyses were performed using SAS System for Windows (Version 9.1) procedures that incorporate survey weights, PROC SURVEYMEANS and PROC SURVEYREG (SAS Institute Inc., 2002–2003).
We conducted multivariate weighted least squares (WLS) regressions to examine the associations between each SES and HRQoL variable (and SRH), first net of gender, age, and race and subsequently net of the other SES variables as well. Partial F-tests were conducted to test whether each SES variable significantly explained variation in HRQoL or SRH. We also tested age-by-SES interaction terms, added to the WLS models that included all the SES variables simultaneously (testing one interaction at a time).
There were missing data on seven items (percent missing in parentheses): education (0.5%), income (8.3%), assets (9.9%), EQ-5D (1.2%), SF-6D (3.0%), HUI3 (7.2%), and SRH (0.5%). We therefore conducted multiple imputation, creating five multiply imputed data sets. Results across the five imputed data sets demonstrated little variation. The partial F-tests and ANOVAs were performed with the first imputed data set. All other analyses were performed by combining all five data sets via PROC MIANALYZE.
RESULTS
HRQoL Stratification by SES
We first examine whether multiple measures of SES (income, education, and assets) are separately and simultaneously associated with multiple measures of HRQoL and SRH. Table 2 summarizes results of regressing each of the three HRQoL and SRH measures on each of the SES measures separately, controlling for age, race, and gender. Table 2 demonstrates that each measure of SES is associated with all HRQoL and SRH measures. At each lower level compared with the highest level of education, income, and assets, people report worse HRQoL and SRH. Partial F-tests confirm that each SES measure significantly contributes to explaining variance in every HRQoL and SRH measure.
Table 2.
Health-Related Quality of Life and Self-Rated Health (SRH) Measures Regressed (Weighted Least Squares) on Each Socioeconomic Status (SES) Variable Separately (Controlling for Age, Race, and Gender) (2005/2006 National Health Measurement Study, n = 3,663)
| EQ-5D |
SF-6D |
HUI3 |
SRH |
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Education | ||||||||
| <High school | −0.106*** | 0.018 | −0.096*** | 0.015 | −0.201*** | 0.031 | −1.047*** | 0.107 |
| High school | −0.044*** | 0.008 | −0.030*** | 0.008 | −0.046*** | 0.013 | −0.430*** | 0.068 |
| Some post–high school | −0.042*** | 0.011 | −0.031*** | 0.009 | −0.062*** | 0.018 | −0.366*** | 0.067 |
| 4-Year college degree or more | Reference group | Reference group | Reference group | Reference group | ||||
| R2 | 8.1% | 7.1% | 7.6% | 14.3% | ||||
| Partial F-statistic(3, 3,654) | 53.2*** | 49.4*** | 58.6*** | 112.8*** | ||||
| Household income | ||||||||
| <$20,000 | −0.149*** | 0.019 | −0.140*** | 0.015 | −0.260*** | 0.029 | −1.110*** | 0.076 |
| $20,000–$34,999 | −0.065*** | 0.013 | −0.065*** | 0.010 | −0.119*** | 0.022 | −0.534*** | 0.087 |
| $35,000–$74,999 | −0.029*** | 0.008 | −0.021** | 0.007 | −0.037** | 0.013 | −0.230*** | 0.065 |
| $75,000+ | Reference group | Reference group | Reference group | Reference group | ||||
| R2 | 12.3% | 13.3% | 12.9% | 16.2% | ||||
| Partial F-statistic(3, 3,654) | 112*** | 141.1*** | 134.7*** | 145.9*** | ||||
| Household assets | ||||||||
| <$25,000 | −0.068*** | 0.010 | −0.079*** | 0.009 | −0.121*** | 0.018 | −0.706*** | 0.072 |
| $25,000–$99,999 | −0.028** | 0.008 | −0.031*** | 0.008 | −0.030* | 0.014 | −0.311*** | 0.063 |
| $100,000+ | Reference group | Reference group | Reference group | Reference group | ||||
| R2 | 7.4% | 9.1% | 7.1% | 13.6% | ||||
| Partial F-statistic(2, 3,655) | 66.7*** | 118.1*** | 85.9*** | 155.0*** | ||||
Notes: All models control for gender, age, and race; partial F-test is for the given SES variable added to a base model of gender, age, and race. HUI3, Health Utilities Index Mark 3; EQ-5D, EuroQol EQ-5D.
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
In Table 3, we present results of regressing each HRQoL and SRH measure on the three SES measures simultaneously, controlling for age, race, and gender. Partial F-tests (not shown) indicated that each SES variable (each block of SES dummy variables) is significantly associated with each HRQoL and SRH measure (p < .05), while controlling for gender, age, race, and other SES variables. This means that although some of the coefficients representing pairwise comparisons between the highest versus lower SES groups are not statistically significant in Table 3, each overall measure of SES does contribute as a whole to HRQoL and SRH, net of other SES variables.
Table 3.
Health-Related Quality of Life and Self-Rated Health (SRH) Measures Regressed (Weighted Least Squares) on Gender, Race, and Socioeconomic Status (Education, Income, and Assets), for the Full Sample (2005/2006 National Health Measurement Study, n = 3,663)
| EQ-5D |
SF-6D |
HUI3 |
SRH |
|||||
| Variables | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE |
| Intercept | 0.951 | 0.010 | 0.856 | 0.009 | 0.900 | 0.018 | 4.225 | 0.070 |
| Gender (Female) | −0.009 | 0.008 | −0.010 | 0.007 | −0.009 | 0.012 | 0.169*** | 0.051 |
| Age group (years) | ||||||||
| 35–44 | Reference group | Reference group | Reference group | Reference group | ||||
| 45–54 | −0.026* | 0.011 | −0.013 | 0.010 | −0.019 | 0.017 | −0.215** | 0.069 |
| 55–64 | −0.053*** | 0.012 | −0.034*** | 0.010 | −0.055** | 0.021 | −0.425*** | 0.084 |
| 65–74 | −0.023 | 0.013 | −0.013 | 0.011 | −0.003 | 0.021 | −0.426*** | 0.075 |
| 75–89 | −0.035* | 0.014 | −0.030** | 0.012 | −0.034 | 0.024 | −0.472*** | 0.083 |
| Race | ||||||||
| Black | −0.022 | 0.012 | −0.006 | 0.010 | −0.026 | 0.021 | −0.142* | 0.065 |
| White | Reference group | Reference group | Reference group | Reference group | ||||
| Education | ||||||||
| <High school | −0.043* | 0.019 | −0.028 | 0.016 | −0.081* | 0.033 | −0.595*** | 0.111 |
| High school degree | −0.017 | 0.009 | −0.002 | 0.009 | 0.002 | 0.013 | −0.239*** | 0.069 |
| Some post–high school | −0.025* | 0.010 | −0.012 | 0.009 | −0.032* | 0.016 | −0.229*** | 0.066 |
| 4-Year college degree or more | Reference group | Reference group | Reference group | Reference group | ||||
| Household income | ||||||||
| <$20,000 | −0.122*** | 0.022 | −0.107*** | 0.016 | −0.216*** | 0.034 | −0.635*** | 0.104 |
| $20K–34,999 | −0.045** | 0.015 | −0.041*** | 0.012 | −0.089*** | 0.025 | −0.201* | 0.092 |
| $35K–74,999 | −0.019* | 0.009 | −0.009 | 0.009 | −0.027 | 0.015 | −0.064 | 0.071 |
| $75,000+ | Reference group | Reference group | Reference group | Reference group | ||||
| Household assets | ||||||||
| <$25,000 | −0.014 | 0.011 | −0.036*** | 0.010 | −0.029 | 0.020 | −0.348*** | 0.085 |
| $25K–99,999 | −0.008 | 0.008 | −0.017* | 0.008 | 0.001 | 0.015 | −0.186** | 0.067 |
| $100,000+ | Reference group | Reference group | Reference group | Reference group | ||||
| R2 | 13.1% | 14.7% | 14.2% | 20.0% | ||||
Notes: HUI3, Health Utilities Index Mark 3; EQ-5D, EuroQol EQ-5D.
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
Summarizing the results from Table 3 by SES measure and focusing first on the three preference-based HRQoL measures, we note that education has statistically significant pairwise comparisons between lower and highest education categories with two of the preference-based HRQoL measures. In terms of the magnitude of the associations, using the cutoff of 0.03 as a coefficient size that is commonly considered substantively important for preference-based HRQoL measures (Lubetkin et al., 2005; Sullivan, Lawrence, & Ghushchyan, 2005; Wyrwich et al., 2005), we find that education has both statistically significant and substantively important differences between lowest and highest education categories predicting EQ-5D and HUI3 scores. For example, those with less than a high school education have an EQ-5D score that is 0.043 worse (on a scale of 0–1) than those with a college degree or greater. Although those with some post–high school education have worse EQ-5D scores (−0.025) than those with a college degree, this coefficient is statistically significant but not of sufficient magnitude (because the coefficient is <0.03) to be considered substantively significant.
Income consistently shows statistically and substantively significant associations with all three preference-based HRQoL measures. Level of assets has only one substantively significant association for the SF-6D when comparing respondents with the lowest and highest asset levels. Analyses regarding multicollinearity (not shown) suggest that although the SES measures are related, there is not a substantial multicollinearity problem with these additive analyses.
We cannot directly compare the regression coefficients for SRH (scaled from 1 to 5) with those for the three preference-based HRQoL indexes because the scales differ numerically and in interpretation. Those in the lowest education group have, on average, a 0.60 worse SRH score (over one half a category) than those in the highest education group. Those in the lowest income group have a 0.64 worse SRH score than those in the highest income group. Finally, those with the lowest asset levels have a 0.35 lower SRH score than those with the highest asset levels.
Among the SES variables, income has the strongest and most consistent association with the HRQoL and SRH measures. Education makes modest additional contributions to explaining variation in HRQoL, and the assets measure does not consistently contribute much. However, all three SES measures have independent associations with SRH. In sum, these results demonstrate that all three SES measures have independent associations with both HRQoL and SRH.
HRQoL Stratification by SES and Age
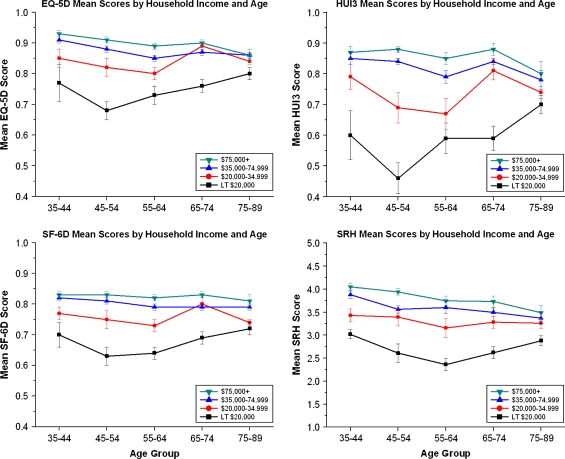
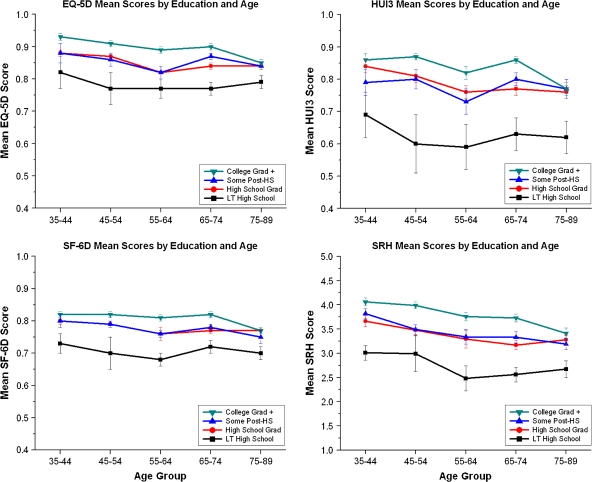
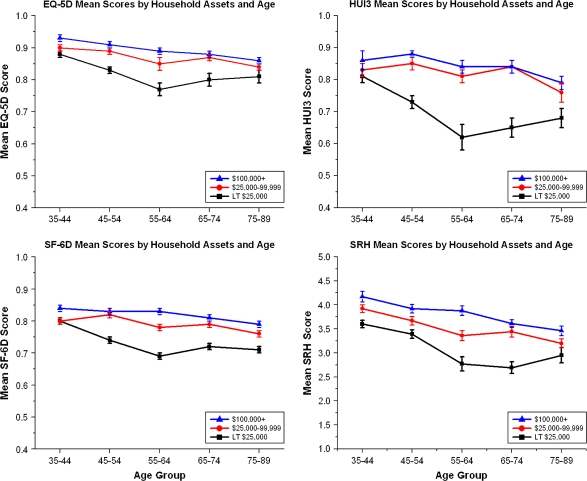
Our second aim is to examine whether there are age variations in the relationship between SES and HRQoL. We begin by plotting simple means of the three HRQoL and SRH measures within age groups and by SES categories. Figures 1–3 show the unadjusted means of the HRQoL and SRH measures within age groups and by income, education, and assets categories, respectively. The three preference-based HRQoL indexes can be compared with each other, as they have similar scales anchored at 0 and 1. Although the SRH measure is not on the same metric, we can at least observe similarities and differences in general patterns.
Figure 1.
Income-by-age interactions for each health-related quality of life measure.
Figure 2.
Education-by-age interactions for each health-related quality of life measure.
Figure 3.
Assets-by-age interactions for each health-related quality of life measure.
Figure 1 shows that income is associated with all measures of HRQoL and SRH. ANOVAs (not shown) confirm that income has a statistically significant association (p < .05) with all four HRQoL measures within each age group. People in the lowest income group (<$20,000) have worse HRQoL than those with greater income at every age group. In fact, those in the lowest income group have worse HRQoL at ages 35–44 years than do those in the next highest income group at ages 75–89 years. Income disparities appear wider for the HUI3 measure than for either the SF-6D or EQ-5D. Income disparities in SRH appear wide as well. Income disparities appear widest at ages 45–54 years, and although they are smaller at ages 75–89 years, they are still statistically significant at this age group. F-tests of age-by-income interactions with no other controls (results not shown) confirm statistically significant (p < .01) age variations in the associations between income and all three preference-based HRQoL and SRH measures.
Figure 2 shows that education disparities in HRQoL and SRH are fairly consistent across age groups (confirmed by statistically nonsignificant [p > .05] age-by-education interactions). Those with less than a high school education have much worse HRQoL than those with higher levels of education at all ages. ANOVAs (not shown) find that education has a statistically significant association with all HRQoL and SRH measures within each age group (p < .01). Again, the HUI3 and SRH outcomes appear to reflect a greater gap than do the SF-6D and EQ-5D.
Figure 3 shows that asset differentials in HRQoL are generally smaller at young adulthood (35–44), largest at ages 55–64 years, and smaller again at later old age (75–89). F-tests of age-by-asset interactions were statistically significant (p < .001) for all HRQoL and SRH measures, with no other controls in the model. Despite the fact that the gap is smaller at later old age, ANOVAs (not shown) confirm that there are still asset disparities in HRQoL at each age (p < .05), including at older ages (except at ages 35–44 years with the HUI3). Of note is that the average HRQoL is slightly higher at later old ages than at middle ages for the groups with the lowest income and assets, which we address in the Discussion section.
As results in Figures 1–3 do not adjust for other variables, we also performed WLS regressions including blocks of age-by-SES interaction terms to the models in Table 3 to examine whether age-by-SES interactions were statistically significant once other SES variables were controlled. These results (not shown) confirm that the association between education and HRQoL and SRH does not vary by age group. In addition, income disparities in HRQoL and SRH no longer vary by age group in multivariate models. There were statistically significant interactions between age and assets for both the SF-6D and HUI3 indicating that having <$25,000 in assets is particularly associated with worse SF-6D and HUI3 scores among those aged 45–54 and 55–64 years, net of all other SES variables and race and gender. In additional sensitivity analyses, age-specific analyses were also conducted (not shown) and demonstrated general consistency with the results reported here.
DISCUSSION
Our study demonstrates that preference-based HRQoL measures are significantly stratified by SES among U.S. adults. Income, education, and assets are each associated with multiple preference-based HRQoL measures and SRH, with income being the strongest, most consistent predictor. We also show that although there is some age variation in the size of the relationship between SES and HRQoL, SES disparities in HRQoL exist at all adult age groups—even at older ages. In particular, we find that those at the bottom of the socioeconomic distribution (with the lowest income, education, and assets) have much worse HRQoL and SRH than those with higher levels of SES. Indeed, those in the lowest income and education groups currently have worse HRQoL at ages 35–44 years than do those in the current 65+ age cohort in any of the higher income and education groups. Our results of persisting SES disparities at older ages are consistent with a recent Canadian prospective study that similarly found strong income differences in older adults’ ability to maintain exceptional health over a 10-year follow-up period (using the HUI3 HRQoL measure) (Kaplan et al., 2008).
One of the goals of our research was to introduce several preference-based HRQoL measures to the literature on socioeconomic and age stratification and health. Our results are relatively consistent with previous work focusing on age differences in SES disparities in unidimensional measures of health. For example, our results show that income differentials in HRQoL and SRH exist at all ages, but the widest differentials are noted at about ages 45–54 years and the smallest at later old age. These results are generally consistent with research by House and colleagues (1994, 2005), who found similar age patterns in the relationship between income and functional health and chronic conditions in a national study in the 1980s. Our multivariate results demonstrated that among all SES variables, income is the strongest predictor of HRQoL and SRH, with income strongly associated with HRQoL and SRH at all ages except at 75–89 years, net of other SES variables.
Our results indicated that education disparities in HRQoL and SRH are fairly constant across all current age cohorts, consistent with research demonstrating that education matters to health throughout the life course (Lynch, 2006), including at older ages (Martin et al., 2007; Schoeni, Martin, Andreski, & Freedman, 2005). However, education was a weaker predictor than income and indeed appeared to be particularly weak at later old age (75–89 years). This is consistent with research suggesting that education may be more important earlier in life (affecting the onset of disease), whereas income may be more important in later life (affecting the progression of disease) (Herd et al., 2007; House et al., 2005; Melzer et al., 2001; Ross &Wu, 1996). Our results suggest that asset differentials in HRQoL exist net of other measures of SES for some HRQoL measures, particularly in middle age, consistent with previous research focusing on specific measures of morbidity (Robert & House, 1996). However, our measure of assets was crude and likely underestimated asset effects—further research should employ more detailed measures of wealth.
Our analyses were cross-sectional, and therefore we did not aim to rigorously test cumulative advantage/disadvantage versus age-as-leveler hypotheses. However, our results are not consistent with a cumulative advantage/disadvantage hypothesis. Because the relationship between SES and health is generally much smaller at older ages in these data, our results are more consistent with an age-as-leveler hypothesis. In fact, our bivariate figures showed that those with the lowest income and asset levels actually had higher mean HRQoL in the later old age cohort than did those in the middle age cohorts. These results may be due to methodological issues (sampling and response bias), or they may be real and due to either age or cohort effects and/or availability of Medicare-supported health care to those older than 65 years.
As this research is based on a community sample, we do not have data on people who are most likely to be the sickest—those in nursing homes or other institutions. Therefore, it may be that our sample reflects the hardy survivors who lived to older ages who are physically and mentally healthy enough to participate in a phone survey. Indeed, Kaplan and colleagues (2008) found that baseline income was strongly linked to maintaining exceptionally good health more than 10 years among Canadian elders, particularly when these “thrivers” were compared with older adults who were in institutions after 10 years. Future U.S. research needs to examine the health of all older adults, no matter where they reside, in order to fully understand age variations in health, and particularly if we want to well test cumulative advantage/disadvantage versus age-as-leveler hypotheses.
When comparing the results for the three preference-based HRQoL measures with the single SRH measure, we found that SRH appeared most strongly associated with or sensitive to SES. Whereas the preference-based HRQoL measures embody self-reported health status valued using community preferences, SRH embodies self-reported health implicitly valued by an individual's own rating. Perhaps lower SES individuals experiencing poor health are more likely to evaluate this health state much lower than the valuation of the general public. Our results suggest that this simple SRH measure remains useful in research aimed at understanding SES and health, particularly because it is much easier to measure than the preference-based HRQoL measures. However, because the preference-based HRQoL measures may increasingly be used in clinical, cost-effectiveness, and population-based studies, gerontologists should contribute to the discourse both over the use of these measures more generally (whether or when they are appropriate/inappropriate) and about the importance of examining their stratification by SES and age when they are used.
For researchers interested primarily in HRQoL, our results demonstrate whether and how social stratification by SES and age needs to be considered in future research and provides estimates across three common HRQoL measures that can be used for comparative purposes. Comparing the three preference-based HRQoL measures, we note larger SES disparities for the HUI3 than for the SF-6D and the EQ-5D in both bivariate and multivariate analyses. The HUI3 indicates much lower levels of HRQoL among those in the lowest income group in particular. It might be that the HUI3 is more able to discriminate among severe poor health states, as it includes eight attributes with five or six levels each. Alternately, it may be that these results reflect the fact that the preference values assigned to the same poor health states are given lower value weights in the HUI3. Future research should examine whether the HUI3 indeed captures more nuanced aspects of poor health that are more likely to be seen among low SES groups or whether differences in the assigned preference values are solely responsible for the different results. In any case, researchers with data without multiple measures of HRQoL should be aware that the values for lower SES groups may differ by HRQoL measure.
Another limitation to this study is that we excluded 4.7% of respondents reporting their race as neither White nor Black, meaning that our results are generalizable only to U.S. community-residing adults who report their race as either White or Black. Future research will need to examine the relationship between race and HRQoL more closely, including how it may vary by hard-to-reach racial subgroups of the population. Strengths of this study include that we use a recent national study on health among U.S. adults, using multiple preference-based measures of HRQoL and an SRH measure, and examine three SES measures (education, income, and assets). Our results provide an excellent basis of comparison for future studies that have more limited data on either SES or HRQoL measures.
In conclusion, given that people in the highest SES groups already have very high HRQoL and SRH in all age groups, we cannot expect overall mean population health to significantly improve in the United States unless it improves for people who currently have the lowest SES levels and the lowest HRQoL and SRH. Moreover, although the overall economic status of older adults has improved in recent decades, it has not improved for all older adults. Our results show that these SES disparities are associated with HRQoL and SRH disparities among all adult age groups. Policy and program efforts to improve population health might most effectively focus on those at the bottom of the SES distribution. Although this might involve efforts to buffer the health effects of having low SES, a fundamental cause theory would suggest that a more efficient policy effort might be to address educational attainment and income and asset security directly rather than to temporarily buffer their effects.
FUNDING
This study was funded by a grant from the National Institute on Aging (P01AG020679).
Acknowledgments
A previous version of this study was presented at the 14th Annual Scientific Meeting of the International Society of Quality of Life Research, October 2007. We acknowledge Jenny Buechner for contributions to organizing the data and the editor and anonymous reviewers for their helpful comments. It should be noted that David Feeny has a proprietary interest in Health Utilities Incorporated, Dundas, Ontario, Canada. HUInc. distributes copyrighted HUI materials and provides methodological advice on the use of HUI. Author contributions: S. A. Robert planned the study and was primarily responsible for writing the paper. D. Cherepanov conducted the analyses and contributed to writing. M. Palta supervised the analyses and contributed to study conceptualization and manuscript revision. N. C. Dunham, D. Feeny, and D. G. Fryback contributed to study conceptualization and manuscript revision.
References
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Alwin DF, Wray LA. A life-span developmental perspective on social status and health. Journals of Gerontology: Social Sciences. 2005;60B(Special Issue II):7–14. doi: 10.1093/geronb/60.special_issue_2.s7. [DOI] [PubMed] [Google Scholar]
- Baum F. Wealth and health: The need for more strategic public health research. Journal of Epidemiology and Community Health. 2007;59:542–545. doi: 10.1136/jech.2004.021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics. 2002;21:271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y. Trends in health life expectancy in the United States, 1970–1990: Gender, racial, and educational differences. Social Science and Medicine. 2001;52:1629–1641. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- Dannefer D. Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. Journals of Gerontology: Social Sciences. 2003;58B:S327–S337. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Deaton AS, Paxson CH. Aging and inequality in income and health. American Economic Review. 1998;88:248–253. [Google Scholar]
- Dupre ME. Educational differences in age-related patterns of disease: Reconsidering the cumulative disadvantage and age-as-leveler hypotheses. Journal of Health and Social Behavior. 2007;48:1–15. doi: 10.1177/002214650704800101. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong WJ, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Denton M, Boyle M. Multiattribute and single-attribute utility functions for the Health Utilities Index Mark 3 system. Medical Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- Feinglass J, Lin S, Thompson J, Sudano J, Dunlop D, Song J, Baker DW. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: Findings from the Health and Retirement Study, 1992–2002. Journals of Gerontology: Social Sciences. 2007;62B:S209–S217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: A systematic review. Journal of the American Medical Association. 2002;288:3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Fryback DG, Cross Dunham N, Palta M, Hanmer J, Buechner J, Cherepanov, et al. U.S. norms for six generic health-related quality-of-life indexes from the National Health Measurement Study. Medical Care. 2007;45:1162–1170. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M. On the concept of health capital and the demand for health. Journal of Political Economy. 1972;80:223–255. [Google Scholar]
- Hanmer J, Lawrence WF, Anderson JP, Kaplan RM, Fryback DG. Report of nationally representative values for the non-institutionalized US adult population for 7 health-related quality-of-life scores. Medical Decision Making. 2006;26:391–400. doi: 10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- Hatch SL. Conceptualizing and identifying cumulative adversity and protective resources: Implications for understanding health inequalities. Journals of Gerontology: Social Sciences. 2005;60B:130–134. doi: 10.1093/geronb/60.special_issue_2.s130. [DOI] [PubMed] [Google Scholar]
- Herd P, Goesling B, House JS. Socioeconomic position and health: The differential effects of education versus income on the onset versus progression of health problems. Journal of Health and Social Behavior. 2007;48:223–238. doi: 10.1177/002214650704800302. [DOI] [PubMed] [Google Scholar]
- Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI©): Concepts, measurement properties and applications. Health and Quality of Life Outcomes. 2003;1:54–66. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JA, Lantz PM, Herd P. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study) Journals of Gerontology: Social Sciences. 2005;60B(Special Issue II):15–26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Herzog AR. The social stratification of aging and health. Journal of Health and Social Behavior. 1994;35:213–234. [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler EL, Kasl S. Self-ratings of health: Do they also predict change in functional ability? Journals of Gerontology: Social Sciences. 1995;50B(Suppl):S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I epidemiological follow-up study, 1992. American Journal of Epidemiology. 2000;152:874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Johnson JA, Luo N, Shaw JW, Kind P, Coons SJ. Valuations of EQ-5D health states: Are the United States and the United Kingdom different? Medical Care. 2005;43:221–228. doi: 10.1097/00005650-200503000-00004. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Berthelot JM, Feeny DH, McFarland BH, Khan S. The predictive validity of two measures of health-related quality of life: Mortality in a longitudinal population-based study. Quality of Life Research. 2007;16:1539–1546. doi: 10.1007/s11136-007-9256-7. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Orpana H, Feeny D, McFarland BH, Ross N. Prevalence and factors associated with thriving in older adulthood: A 10-year population-based study. Journals of Gerontology: Medical Sciences. 2008;63:M1097–M1104. doi: 10.1093/gerona/63.10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Lee J. The impact of comorbidity on wealth changes in later life. Journals of Gerontology: Social Sciences. 2006;61:S307–S314. doi: 10.1093/geronb/61.6.s307. [DOI] [PubMed] [Google Scholar]
- Kind P. Size matters: EQ-5D in transition. Medical Care. 2007;45:809–810. doi: 10.1097/MLR.0b013e318074ceac. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS. Education and survival: Birth cohort, period, and age effects. Demography. 2001;38:551–561. doi: 10.1353/dem.2001.0035. [DOI] [PubMed] [Google Scholar]
- Lee J, Kim H. An examination of the impact of health on wealth depletion in elderly individuals. Journals of Gerontology: Social Sciences. 2003;58:S120–S126. doi: 10.1093/geronb/58.2.s120. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;37(Extra issue):80–94. [PubMed] [Google Scholar]
- Lubetkin EI, Jia H, Franks P, Gold MR. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Quality of Life Research. 2005;14:2187–2196. doi: 10.1007/s11136-005-8028-5. [DOI] [PubMed] [Google Scholar]
- Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. Journals of Gerontology: Social Sciences. 2005;60B:S93–S101. doi: 10.1093/geronb/60.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch SM. Explaining life course and cohort variation in the relationship between education and health: The role of income. Journal of Health and Social Behavior. 2006;47:324–338. doi: 10.1177/002214650604700402. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X. Changes in the prevalence of chronic disability in the United States Black and non-Black population above age 65 from 1982 to 1999. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:6354–6359. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Schoeni RF, Freedman VA, Andreski P. Feeling better? Trends in general health status. Journals of Gerontology: Social Sciences. 2007;62:S11–S21. doi: 10.1093/geronb/62.1.s11. [DOI] [PubMed] [Google Scholar]
- McHorney CA. Health status assessment methods for adults: Past accomplishments and future challenges. Annual Review of Public Health. 1999;20:309–325. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]
- Melzer D, Izmirlian G, Leveille SG, Guralnik JM. Educational differences in the prevalence of mobility disability in old age: The dynamics of incidence, mortality, and recovery. Journals of Gerontology: Social Sciences. 2001;56:S294–S301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- Miller W, Robinsin LA, Lawrence RS, editors. Valuing health for regulatory cost-effectiveness analysis. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- O'Rand A. The precious and the precocious: Understanding cumulative disadvantage and cumulative advantage over the life course. The Gerontologist. 1996;36:230–238. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. American Journal of Preventive Medicine. 2007;33:250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- Rabin R, de Charro F. EQ-5D: A measure of health status from the EuroQol Group. Annals of Medicine. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Roberge R, Berthelot JM, Wolfson M. The Health Utility Index: Measuring health differences in Ontario by socioeconomic status. Health Reports. 1995;7:25–32. [PubMed] [Google Scholar]
- Robert SA, House JS. SES differentials in health by age and alternative indicators of SES. Journal of Aging and Health. 1996;8:359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- Ross CE, Wu CL. Education, age, and the cumulative advantage in health. Journal of Health and Social Behavior. 1996;37:104–120. [PubMed] [Google Scholar]
- SAS Institute Inc. Version 9.1 of the SAS System for Windows. Cary, NC: SAS Institute Inc.; 2002–2003. [Google Scholar]
- Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. American Journal of Public Health. 2005;95:2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw JW, Johnson JA, Coons SJ. U.S. valuation of the EQ-5D health states: Development and testing of the D1 valuation model. Medical Care. 2005;43:203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- Soldo BJ, Mitchell OS, Tfaily R, McCabe JF. Cross-cohort differences in health on the verge of retirement. Cambridge, MA: National Bureau of Economic Research; 2006. Working paper 12762. [Google Scholar]
- Sullivan PW, Lawrence WF, Ghushchyan V. A national catalogue of preference-based scores for chronic conditions in the U.S. Medical Care. 2005;43:736–749. doi: 10.1097/01.mlr.0000172050.67085.4f. [DOI] [PubMed] [Google Scholar]
- Wyrwich KW, Bullinger M, Aaronson N, Hays RD, Patrick DL, Symonds T the Clinical Significance Consensus Meeting Group. Estimating clinically significant differences in quality of life outcomes. Quality of Life Research. 2005;14:285–295. doi: 10.1007/s11136-004-0705-2. [DOI] [PubMed] [Google Scholar]