Abstract
Study Objective:
To determine the efficacy of melatonin on sleep problems in children with autistic spectrum disorder (ASD) and fragile X syndrome (FXS).
Methods:
A 4-week, randomized, double blind, placebo-controlled, crossover design was conducted following a 1-week baseline period. Either melatonin, 3 mg, or placebo was given to participants for 2 weeks and then alternated for another 2 weeks. Sleep variables, including sleep duration, sleep-onset time, sleep-onset latency time, and the number of night awakenings, were recorded using an Actiwatch and from sleep diaries completed by parents. All participants had been thoroughly assessed for ASD and also had DNA testing for the diagnosis of FXS.
Results:
Data were successfully obtained from the 12 of 18 subjects who completed the study (11 males, age range 2 to 15.25 years, mean 5.47, SD 3.6). Five participants met diagnostic criteria for ASD, 3 for FXS alone, 3 for FXS and ASD, and 1 for fragile X premutation. Eight out of 12 had melatonin first. The conclusions from a nonparametric repeated-measures technique indicate that mean night sleep duration was longer on melatonin than placebo by 21 minutes (p = .02), mean sleep-onset latency was shorter by 28 minutes (p = .0001), and mean sleep-onset time was earlier by 42 minutes (p = .02).
Conclusion:
The results of this study support the efficacy and tolerability of melatonin treatment for sleep problems in children with ASD and FXS.
Citation:
Wirojanan J; Jacquemont S; Diaz R; Bacalman S; Anders TF; Hagerman RJ; Goodlin-Jones BL. The Efficacy of Melatonin for Sleep Problems in Children with Autism, Fragile X Syndrome, or Autism and Fragile X Syndrome. J Clin Sleep Med 2009;5(2):145-150.
Keywords: Sleep problem, melatonin, autism, fragile X syndrome
Sleep disturbances are a common problem in childhood, with a prevalence of about 25% in typical preschool- and school-aged children.1 The problems have significant impact on not only children, but also their families. The association of sleep problems with emotional, behavioral, and cognitive problems has been well established.2,3 The prev2alence of sleep problems has been reported to be even higher in children with developmental disabilities,4,5 including autism6–8 and fragile X syndrome (FXS).9
Autism is a common developmental disorder characterized by impairments in social interaction, communication, and restrictive or repetitive behaviors.10 To date, the prevalence of autistic spectrum disorders (ASD) has been reported to be as high as 116 per 10,000 children.11 The etiology of ASD is generally thought to be related to heterogeneous genetic influences. In contrast, the most common known single-gene cause of a neurodevelopmental disorder is FXS.12 FXS is caused by a full mutation (> 200 CGG repeats) in the fragile X mental retardation 1 (FMR1) gene. The full mutation leads to methylation of the gene and subsequent deficiency or lack of the FMR1 protein (FMRP), an RNA- binding protein essential for normal brain development.13 The prevalence of FXS is about 1 in 3600 males.14
Sleep problems are reported in up to 89% of children with ASD6,8 and 77 % of children with FXS.9 Dyssomnias (i.e., difficulty falling asleep and frequent nighttime awakenings) are among the most commonly reported problems.9 Children with ASD and FXS are at risk of having cognitive impairment as well as emotional and behavior problems. Approximately 30% of children with full mutation FXS have symptoms that meet the diagnostic criteria for autism.15 The occurrence of sleep disturbances also may be associated with greater developmental, behavior, and psychological problems in these children.9 The reason why sleep problems commonly occur in children with ASD and FXS is elusive. One po.ssible explanation stems from reports of abnormal melatonin levels in these children.16–18
Melatonin, or N-acetyl-5-methoxytryptamine, is an endogenous hormone secreted mainly from the pineal gland. The secretion of melatonin occurs at night, with peak nocturnal plasma levels (approximately 60 pg/mL in young adults) at around 03:00, followed by a steady decline until morning. Secretion is suppressed by photic information transmitted through the suprachiasmatic nuclei of the hypothalamus and the sympathetic nervous system.19 In humans, one major role for melatonin is the regulation of sleep, including increasing the propensity for sleep and setting circadian rhythm control. There are a number of reports of sleep disturbances associated with melatonin deficiency resulting from pineal gland lesions or pinealectomy. In these conditions, some subjects show improvement with melatonin supplementation.20,21 In children with autism, Kulman et al16 reported abnormal melatonin circadian rhythm secretion with significantly lower blood melatonin levels at night in 14 children with autism, compared with healthy children. In 1986, O’Hare et al reported melatonin deficiency in 5 males with FXS.18 In contrast, a preliminary study of 13 boys with FXS showed aberrantly elevated levels of nighttime and minimal daytime mean melatonin levels compared with age-matched, typically developing children, even though the sleep problems were significantly higher in the FXS group.17 One possible explanation for this result might be a malfunctioning of melatonin receptors in these children. Overproduction of melatonin might occur as compensation for the overstimulation of the pineal gland due to increased activity of the sympathetic nervous system, typical of persons with FXS.22 Nevertheless, in our clinical experience, children with FXS have benefited from melatonin treatment for their sleep problems.23
Melatonin has been used as a pharmacologic treatment for insomnias associated with shift work, jet lag, and delayed sleep onset for decades. Subsequently, it has been increasingly used for the management of sleep disturbances in children with developmental disabilities.24,25 Melatonin is rapidly metabolized, mainly in the liver, and excreted in the urine. Orally administered 0.3 mg of melatonin increases serum melatonin levels to the nighttime peak physiologic range, whereas oral administration of melatonin at doses of 1 to 5 mg can elevate serum melatonin levels up to 100 times higher than the physiologic nocturnal peak within an hour. The level falls back to baseline within 4 to 8 hours after administration in adults. (See Brzezinski, 199719 for review)
To the best of our knowledge, no study of melatonin treatment in children with FXS has been reported. There have been only a few studies of melatonin treatment for sleep problems in children with ASD. In 2003, Paavonen et al reported on the effectiveness of melatonin in decreasing sleep-onset latency times and improvements in behavior problems in an open clinical trial in children with Asperger syndrome.26 However, their results showed no improvement in sleep duration and, in fact, showed a slight increase in th number of nighttime awakenings. Another open-label study of controlled-release melatonin in children with autism demonstrated an improvement in sleep pattern measured with the Children’s Sleep Habits Questionnaire.27 In 2006, Garstang and Wallis 28 reported on the effectiveness of melatonin for the treatment of sleep difficulties in 7 children with ASD who participated in a randomized, double-blind, crossover trial. This study aims to determine the efficacy of melatonin for sleep problems in children with ASD and FXS.
METHODS
Subjects
Eighteen subjects (16 boys, 2 girls) between 2 and 15.3 years of age (mean 6 years, SD 3.5) whose parents reported to physicians that their child had a sleep problem during a routine medical exam were recruited through the recruitment core of the Medical Investigation of Neurodevelopmental Disorders (M.I.N.D.) Institute clinic at the University of California, Davis. A University of California, Davis, institutional review board-approved consent form was completed by all of the participants’ parents or legal guardians. All children were enrolled due to the parent’s interest to improve the sleep problem, and no objective measure of sleep was required prior to enrollment. ASD (either autism or pervasive developmental disorder [PDD-NOS]) was diagnosed by a team of developmental pediatricians and psychologists using a comprehensive assessment battery including the Autism Diagnostic Observation Schedule (ADOS), the Autism Diagnostic Interview-Revised (ADI-R), or both.
The diagnosis of FXS was confirmed by FMR1 DNA testing from peripheral blood leucocytes using both southern blot and polymerase chain reaction analysis. Four of the participants had a diagnosis of FXS alone, 8 had a diagnosis of ASD, another 4 had a diagnosis of both FXS and ASD, and 2 participants had the premutation of the FMR1 gene. All participants were free of medication at the time of recruitment and were asked to inform investigators if any additional medications were added over the course of the study.
Study Design
A 4-week, randomized, double blind, placebo-controlled, crossover design was conducted following a 1-week baseline period. Participants were given instructions to take oral bedtime medication, which was either melatonin, 3 mg, or placebo, provided by the Twinlab corporation to look like the melatonin capsule, 30 minutes prior to bedtime over the 2-week trial. Participants were then crossed over to the alternate treatment for an additional 2 weeks. The participants’ families were given a 1-week supply of capsules each week and then seen at the end of the week to count the remaining capsules to document compliance. Compliance was good on both active and placebo drug in all children (12/18 or 67%) except for 1 participant who took the Actiwatch off and was lost at follow-up during the first block of intervention (which was placebo), and 5 others who did not complete data collection (see results).
Participants were assigned a study number based on the order in which they were enrolled. Assignment to treatment condition was concealed until the end of the 4-week study. The document linking their study number and their identifying data was locked in the investigator’s file until the conclusion of the study.
Outcome Measures
Sleep variables, including sleep-onset time (the clock time that the child fell asleep), total night sleep duration (the time from sleep onset to wake-up time minus the time awake during the night), sleep-onset latency time (the time from bedtime to sleep onset time), and the number of night awakenings were obtained from actigraphy and the daily sleep diary completed by the parents or caregivers.
The Actiwatch (Mini-Mitter, OR) is a small, light-weight, wrist-worn activity monitor. Subjects wore an Actiwatch on their nondominant wrist or ankle. The data, consisting of activity counts (frequency) for each 1-minute epoch, were extracted from the Actiwatch for a given child and analyzed with the ActiWare software. An activity count of 100 or above for two 2 consecutive minutes was considered the beginning of an awakening. Additionally, an awakening was scored as ending when the activity level returned to 0 for 3 consecutive minutes.
Parents or caregivers were responsible for completing the predated sleep diaries provided to them as a daily chart for recording the time their child went to bed in the evening, the time he or she fell asleep, the time(s) the child awakened during the night, the time(s) the child returned to sleep, and the time he or she woke up in the morning. A sleep diary is essential for interpretation of the Actiwatch data to know about bedtime, lights out, and other events. At the end of each week, data from Actiwatch were extracted, and sleep diaries were collected.
Statistical Analysis
All statistical analyses were computed using the Statistical Package for the Social Sciences (SPSS 14.0) and the Statistical Analysis System (SAS). Given the small number of subjects, the differences between days the children were administered a placebo and days that they were administered melatonin were tested using the analysis of variance-type statistic (ATS), a nonparametric technique that is valid for both continuous and discrete data.29 The assumptions of this test are that the vectors of 14 longitudinal observations in each of the 2 arms of the intervention corresponding to the 12 subjects are independent, although the components of each of these vectors can be arbitrarily dependent on one another. The probability distributions of these vectors are assumed to be identical, but these distributions do not need to be specified.
Given the small number of independent observations (12 patients), no likelihood imputation technique seemed appropriate. Therefore, 2 simple and practical methods to handle missing data were used: complete case analysis (CC), and last available observation carried forward (LOCF). The CC analysis includes only cases for which all observations are present; for the LOCF analysis, missing values were replaced with the last available observation.
Parametric paired t-tests were also used to compare the paired averages of all 12 participants over all 14 days in each treatment condition (ignoring missing values) for all of the variables. It was observed that the normality assumption for this test was violated due to highly skewed data and the presence of outliers especially in the sleep-duration variable. This pattern is commonly observed in data with small sample sizes as in the case of this study. However, as shown below the conclusions from this test match those of the more appropriate nonparametric test.
RESULTS
Data from 12 of the original 18 participants were useable and analyzed (11 boys, age range 2 to 15.25 years, mean 5.47, SD 3.6). Three participants (2 who had started on placebo) were excluded from analysis, although they completed the study, because their caregiver failed to complete the sleep diaries or the data from their Actiwatch were unreadable. One participant did not complete the study because the Actiwatch was not worn during his first block of treatment (melatonin). However, his parents reported a positive response during treatment. Another participant took the Actiwatch off during the first block of intervention (placebo). One family was excluded because they did not follow the study protocol and complete the sleep diary. No side effects for melatonin or placebo were reported by any parent.
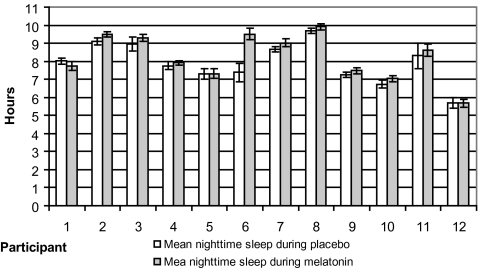
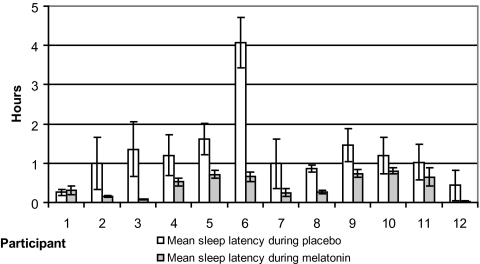
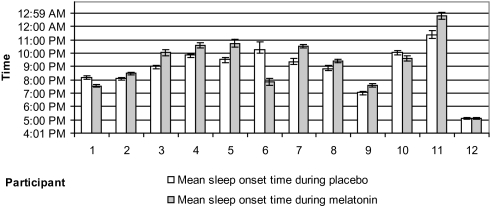
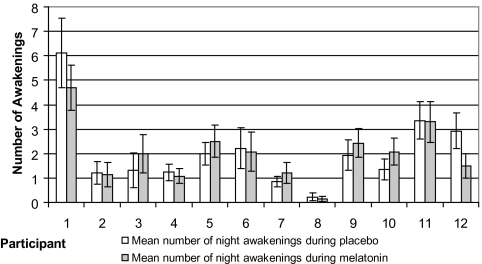
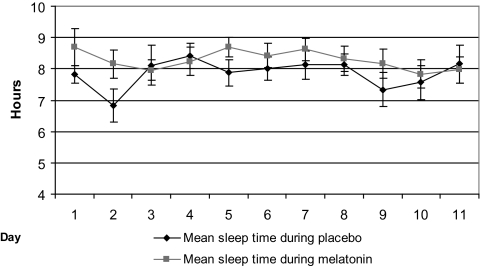
For the 12 participants included in the analysis, 8 had melatonin first. Age, sex, diagnosis, and treatment order for each participant are provided in Table 1. Total night sleep duration was longer in 10 participants (Figure 1), sleep latency time was shorter (Figure 2), and sleep-onset time (Figure 3) was earlier in 9 participants during melatonin treatment compared with placebo. These differences are statistically significant using a nonparametric analysis (Table 2). The number of night awakenings was also fewer during melatonin than placebo in 7 participants (Figure 4), but none of the tests produced a significant difference.
Table 1.
Demographic Data of Each Participant
| Participant number | Sex | Age, y | Block of firsttreatment | Diagnosis |
|---|---|---|---|---|
| 1 | Male | 2 | Placebo | FXS + ASD |
| 2 | Male | 3.5 | Melatonin | FXS |
| 3 | Male | 3.9 | Melatonin | ASD |
| 4 | Female | 7.7 | Melatonin | ASD |
| 5 | Male | 2.3 | Placebo | FXS |
| 6 | Male | 4.4 | Placebo | FXS premutation |
| 7 | Male | 5.1 | Melatonin | ASD |
| 8 | Male | 7.1 | Melatonin | ASD |
| 9 | Male | 3 | Placebo | FXS |
| 10 | Male | 4 | Melatonin | FXS + ASD |
| 11 | Male | 15.3 | Melatonin | ASD |
| 12 | Male | 7.4 | Melatonin | FXS + ASD |
FXS refers to fragile X syndrome; ASD, autism spectrum disorders.
Figure 1.
—Mean nighttime sleep duration with error bars during placebo (2 weeks) and melatonin (2weeks) in each patient.
Figure 2.
—Mean sleep-latency time with error bars during placebo (2 weeks) and melatonin (2 weeks) in each participant.
Figure 3.
Figure 3—Mean sleep-onset time with error bars during placebo (2 weeks) and melatonin (2 weeks) for each participant.
Table 2.
Nonparametric Analysis of the Sleep Variables for the CC Data Set and the LOCF Data Set
| Sleep variables | Data set | ATS χ2 | ˜ df | p Value |
|---|---|---|---|---|
| Night sleep duration | CC | 9.61 | 1 | 0.0019 |
| LOCF | 5.21 | 1 | 0.02 | |
| Sleep-latency time | CC | 15.07 | 1 | 0.0001 |
| LOCF | 14.48 | 1 | 0.0001 | |
| Sleep-onset time | CC | 7.87 | 1 | 0.005 |
| LOCF | 5.20 | 1 | 0.02 | |
| Number of night awakenings | CC | 0.0075 | 1 | 0.93 |
| LOCF | 0.61 | 1 | 0.44 |
ATS refers to analysis of variance-type test statistic; ˜ df, approximate degrees of freedom; CC, complete case analysis; LOCF, last available observation carried forward,.
Figure 4.
Figure 4—Mean number of night awakenings per night with error bars during placebo and melatonin for each participant.
Table 2 summarizes the nonparametric analyses performed on the CC and LOCF data sets. These analyses were performed using a SAS macro.29 The reported ATS is χ2 distributed under the null hypothesis with degrees of freedom obtained using the box-approximation for small sample size.29 The results from both CC and LOCF analyses suggest that there are no significant Treatment-x-Days interactions for any of the variables; however, both analyses are concordant for significant main-effects differences in treatment for sleep duration, sleep-onset latency, and sleep-onset time, as well as no significant differences for number of awakenings.
No significant differences were found for the main effect of Days, but both analyses indicated a tendency for the average sleep duration to be different in at least a pair of the days within either treatment (p = .056 for the CC data set, and p = .068 for the LOCF data set). Figure 5 shows the average sleep time over the 11 days (CC data set) in each of the treatment conditions for all participants. From this graph, it can be seen that these nearly significant p values at the .05 level can be attributed to the lower than average mean sleep times on the second day of placebo (6 hours 37 minutes). The data show that the lower than average value for this day is attributed to an unusually short sleep time (5 hours 13 minutes) for participant 5. Sleep times for this participant during the rest of the days do not indicate an unusual sleep pattern, and, thus, no further statistical analysis was deemed necessary to analyze mean sleep differences among days in each of the intervention arms.
Figure 5.
Figure 5—Mean night sleep duration for each day with error bars for the complete case analysis data.
Conclusions from the analysis performed with the parametric paired t-test, despite some violations of the assumptions of this test as mentioned above, coincide greatly with the conclusions of the nonparametric repeated-measure analysis. Table 3 presents a summary of the parametric analysis.
Table 3.
Comparison of Sleep Variables During Placebo and Melatonin
| Variables | Placebo | Melatonin | Differences | Effect size (da) | p Value b |
|---|---|---|---|---|---|
| Total night sleep duration, h:min | 7:54 (1:07) | 8:15 (1: 15) | + 0:21 | 2.1257 | 0.057 |
| Sleep-latency time, min:s | 53:35 (60:33) | 25:30 (16:53) | − 28:05 | 1.7959 | 0.10 |
| Sleep-onset, time of day | 21:25 (2:00) | 20:43 (1:39) | − 0:42 | 2.8090 | 0.017 |
| Awakenings, no./night | 2.07 (1.5) | 1.99 (1.2) | − 0.07 | 0.3540 | 0.73 |
Data are presented as mean (SD).
Paired t- test. Nondirectional 2-tail effect size (da refers to the number of standard error units between means)
DISCUSSION
The results of this study suggest that melatonin is an effective treatment for sleep problems in children with ASD and FXS, a finding that is consistent with previous studies of children with ASD and developmental disabilities.24,26–28 Overall, the mean sleep parameters were “better” while on melatonin compared with placebo. Significant improvements in total night sleep durations, sleep latency times, and sleep-onset time on melatonin were found with nonparametric analyses (from CC and LOCF data for repeated measures). These results confirm the effect of an increased propensity for sleep on melatonin. However, using a parametric test, only sleep-onset times showed a statistically significant difference. The effect sizes in Table 3 provide a unit-less comparison between each condition for the sleep variables, and, given the large variability, only more than 2.5 standard errors was large enough for significance. Perhaps, with a larger sample, the differences in other sleep variables would have been significant. Given that many parents have a problem with children settling in the beginning of the night, the significant improvement in sleep-onset time was received positively by families.
We designed this randomized, double blind, placebo-controlled, crossover trial following a 1-week baseline period without washout between treatment arms because of the short half-life of melatonin. Sleep data were collected using actigraphy along with sleep diaries to provide objective data. The diary information is needed to calculate such variables as sleep-latency duration. The Actiwatch is a reliable and useful tool for sleep studies in children.30 However, there are some limitations when attempting to distinguish sleep from quiet wakefulness and nighttime awakenings from active rapid eye movement sleep.31 We also experienced data loss and poor compliance in some participants.
No consensus on the dose of melatonin has been established, since there are variations in an individual's baseline melatonin level and orally administered preparations differ in their bioavailability. The most common treatment dose of melatonin in clinical studies of sleep problems in children with neurodevelopmental disorders is between 1 and 5 mg. Such a dose can raise blood melatonin levels higher than the physiologic nocturnal peak and has been shown to be effective because of its short half-life and because of poor responses at lower doses (0.5 to 1 mg).32 Jan et al25,33 suggested starting melatonin at a lower dose (1 to 3 mg for infants and toddlers and 2.5 to 5 mg for older children), then gradually adjusting the dose according to the response. In this study, we used 3 mg of melatonin with all of the participants, and the results suggest effectiveness. Practically, some participants may have needed higher dose for obtaining a significant response, whereas others might have benefited from lower doses.
The individual variability in response to treatment also may have resulted from wide variations in endogenous melatonin levels in each participant. Two studies of melatonin levels in children with FXS suggest such a possibility.17,18 Some medications have been reported to interfere with melatonin levels either by enhancing them (antidepressants34) or by diminishing them (β-adrenergic receptor-blocking agent and valproic acid35,36). None of our participants were taking other medications during the study. Another factor that might impact our results is the varying sleep hygiene practices in each of the families. Behavioral treatments focused on more structured sleep hygiene have proven to be effective in treating sleep disorders in children with autism and FXS.37
No significant adverse events or developmental impairments have been reported in pediatric studies of melatonin treatment24,25 except for 1 report of increasing seizure activity in 4 children with neurologic disabilities.38 The potential for neuroprotective and anticonvulsant properties of melatonin also has been reported.39 Seizures are common in children with ASD and FXS. Parents reported no side effects throughout this study.
In summary, the results of this study support the efficacy and tolerability of melatonin treatment for sleep problems in children with ASD and FXS. We conclude that melatonin can be considered a safe and effective pharmacologic treatment in addition to behavior therapies and sleep hygiene practices for the management of sleep problems in children with ASD and FXS.
ACKNOWLEDGMENTS
This study was supported, in part by NIH MH068232 (TFA) and the M.I.N.D. Institute. Melatonin and placebo were provided by the Twinlab corporation. We also wish to thank Anny Wu, Karen Tang, and Penelope Decle for research assistance and the members of families included in this study for their participation and assistance.
Disclosure Statement
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Owens JA, Witmans M. Sleep problems. Curr Probl Pediatr Adolesc Health Care. 2004;34:154–79. doi: 10.1016/j.cppeds.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Hiscock H, Canterford L, Ukoumunne OC, Wake M. Adverse associations of sleep problems in Australian preschoolers: national population study. Pediatrics. 2007;119:86–93. doi: 10.1542/peds.2006-1757. [DOI] [PubMed] [Google Scholar]
- 3.Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev. 2002;73:405–17. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- 4.Quine L. Sleep problems in primary school children: comparison between mainstream and special school children. Child Care Health Dev. 2001;27:201–21. doi: 10.1046/j.1365-2214.2001.00213.x. [DOI] [PubMed] [Google Scholar]
- 5.Piazza CC, Fisher WW, Kahng SW. Sleep patterns in children and young adults with mental retardation and severe behavior disorders. Dev Med Child Neurol. 1996;38:335–44. doi: 10.1111/j.1469-8749.1996.tb12099.x. [DOI] [PubMed] [Google Scholar]
- 6.Richdale AL. Sleep problems in autism: prevalence, cause, and intervention. Dev Med Child Neurol. 1999;41:60–6. doi: 10.1017/s0012162299000122. [DOI] [PubMed] [Google Scholar]
- 7.Gail Williams P, Sears LL, Allard A. Sleep problems in children with autism. J Sleep Res. 2004;13:265–8. doi: 10.1111/j.1365-2869.2004.00405.x. [DOI] [PubMed] [Google Scholar]
- 8.Wiggs L, Stores G. Sleep patterns and sleep disorders in children with autistic spectrum disorders: insights using parent report and actigraphy. Dev Med Child Neurol. 2004;46:372–80. doi: 10.1017/s0012162204000611. [DOI] [PubMed] [Google Scholar]
- 9.Richdale AL. A descriptive analysis of sleep behaviour in children with fragile X. J Intellect Dev Disabil. 2003;28:135–44. [Google Scholar]
- 10.American Psychiatric Association. 4th Edition-Text Revised. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 11.Baird G, Simonoff E, Pickles A, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006;368:210–5. doi: 10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- 12.Reddy KS. Cytogenetic abnormalities and fragile-X syndrome in autism spectrum disorder. BMC Med Genet. 2005;6:3. doi: 10.1186/1471-2350-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Irwin SA, Galvez R, Weiler IJ, Beckel-Mitchener A, Greenough WT. Brain structure and functions of FMR1 protein. In: Hagerman RJ, Hagerman PJ, editors. Fragile X Syndrome: Diagnosis, Treatment and Research. 3rd ed. Baltimore, MD: The Johns Hopkins University Press; 2002. pp. 192–205. [Google Scholar]
- 14.Crawford DC, Meadows KL, Newman JL, et al. Prevalence of the fragile X syndrome in African-Americans. Am J Med Genet. 2002;110:226–33. doi: 10.1002/ajmg.10427. [DOI] [PubMed] [Google Scholar]
- 15.Rogers SJ, Wehner DE, Hagerman R. The behavioral phenotype in fragile X: symptoms of autism in very young children with fragile X syndrome, idiopathic autism, and other developmental disorders. J Dev Behav Pediatr. 2001;22:409–17. doi: 10.1097/00004703-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Kulman G, Lissoni P, Rovelli F, Roselli MG, Brivio F, Sequeri P. Evidence of pineal endocrine hypofunction in autistic children. Neuroendocrinol Lett. 2000;21:31–4. [PubMed] [Google Scholar]
- 17.Gould EL, Loesch DZ, Martin MJ, Hagerman RJ, Armstrong SM, Huggins RM. Melatonin profiles and sleep characteristics in boys with fragile X syndrome: a preliminary study. Am J Med Genet. 2000;95:307–15. [PubMed] [Google Scholar]
- 18.O’Hare JP, O’Brien IA, Arendt J, et al. Does melatonin deficiency cause the enlarged genitalia of the fragile-X syndrome? Clin Endocrinol (Oxford) 1986;24:327–33. doi: 10.1111/j.1365-2265.1986.tb03274.x. [DOI] [PubMed] [Google Scholar]
- 19.Brzezinski A. Melatonin in humans. N Engl J Med. 1997;336:186–95. doi: 10.1056/NEJM199701163360306. [DOI] [PubMed] [Google Scholar]
- 20.Etzioni A, Luboshitzky R, Tiosano D, Ben-Harush M, Goldsher D, Lavie P. Melatonin replacement corrects sleep disturbances in a child with pineal tumor. Neurology. 1996;46:261–3. doi: 10.1212/wnl.46.1.261. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann ED, Cockerell OC, Rudge P. Somnolence associated with melatonin deficiency after pinealectomy. Lancet. 1996;347:323. doi: 10.1016/s0140-6736(96)90496-1. [DOI] [PubMed] [Google Scholar]
- 22.Miller LJ, McIntosh DN, McGrath J, et al. Electrodermal responses to sensory stimuli in individuals with fragile X syndrome: a preliminary report. Am J Med Genet. 1999;83:268–79. [PubMed] [Google Scholar]
- 23.Hagerman RJ. Medical follow-up and pharmacotherapy. In: Hagerman RJ, Hagerman PJ, editors. Fragile X Syndrome: Diagnosis, Treatment and Research. 3rd ed. Baltimore, MD: The Johns Hopkins University Press; 2002. pp. 287–338. [Google Scholar]
- 24.Dodge NN, Wilson GA. Melatonin for treatment of sleep disorders in children with developmental disabilities. J Child Neurol. 2001;16:581–4. doi: 10.1177/088307380101600808. [DOI] [PubMed] [Google Scholar]
- 25.Jan JE, Freeman RD, Fast DK. Melatonin treatment of sleep-wake cycle disorders in children and adolescents. Dev Med Child Neurol. 1999;41:491–500. [PubMed] [Google Scholar]
- 26.Paavonen EJ, Nieminen-von Wendt T, Vanhala R, Aronen ET, von Wendt L. Effectiveness of melatonin in the treatment of sleep disturbances in children with Asperger disorder. J Child Adolesc Psychopharmacol. 2003;13:83–95. doi: 10.1089/104454603321666225. [DOI] [PubMed] [Google Scholar]
- 27.Giannotti F, Cortesi F, Cerquiglini A, Bernabei P. An open-label study of controlled-release melatonin in treatment of sleep disorders in children with autism. J Autism Dev Disord. 2006 doi: 10.1007/s10803-006-0116-z. [DOI] [PubMed] [Google Scholar]
- 28.Garstang J, Wallis M. Randomized controlled trial of melatonin for children with autistic spectrum disorders and sleep problems. Child Care Health Dev. 2006;32:585–9. doi: 10.1111/j.1365-2214.2006.00616.x. [DOI] [PubMed] [Google Scholar]
- 29.Brunner E, Domhof S, Langer F. Nonparametric Analysis of Longitudinal Data in Factorial Experiments. New York, NY: John Wiley – Sons, Inc.; 2002. [Google Scholar]
- 30.Hyde M, O’Driscoll DM, Binette S, et al. Validation of actigraphy for determining sleep and wake in children with sleep disordered breathing. J Sleep Res. 2007;16:213–6. doi: 10.1111/j.1365-2869.2007.00588.x. [DOI] [PubMed] [Google Scholar]
- 31.Sitnick SL, Goodlin-Jones B, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31:395–401. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Camfield P, Gordon K, Dooley J, Camfield C. Melatonin appears ineffective in children with intellectual deficits and fragmented sleep: six “N of 1” trials. J Child Neurol. 1996;11:341–3. doi: 10.1177/088307389601100414. [DOI] [PubMed] [Google Scholar]
- 33.Jan JE, Freeman RD. Melatonin therapy for circadian rhythm sleep disorders in children with multiple disabilities: what have we learned in the last decade? Dev Med Child Neurol. 2004;46:776–82. doi: 10.1017/s0012162204001331. [DOI] [PubMed] [Google Scholar]
- 34.Murphy DL, Tamarkin L, Sunderland T, Garrick NA, Cohen RM. Human plasma melatonin is elevated during treatment with the monoamine oxidase inhibitors clorgyline and tranylcypromine but not deprenyl. Psychiatry Res. 1986;17:119–27. doi: 10.1016/0165-1781(86)90067-3. [DOI] [PubMed] [Google Scholar]
- 35.Stoschitzky K, Sakotnik A, Lercher P, et al. Influence of beta-blockers on melatonin release. Eur J Clin Pharmacol. 1999;55:111–5. doi: 10.1007/s002280050604. [DOI] [PubMed] [Google Scholar]
- 36.Monteleone P, Tortorella A, Borriello R, Natale M, Cassandro P, Maj M. Suppression of nocturnal plasma melatonin levels by evening administration of sodium valproate in healthy humans. Biol Psychiatry. 1997;41:336–41. doi: 10.1016/s0006-3223(96)00009-1. [DOI] [PubMed] [Google Scholar]
- 37.Weiskop S, Richdale A, Matthews J. Behavioural treatment to reduce sleep problems in children with autism or fragile X syndrome. Dev Med Child Neurol. 2005;47:94–104. doi: 10.1017/s0012162205000186. [DOI] [PubMed] [Google Scholar]
- 38.Sheldon SH. Pro-convulsant effects of oral melatonin in neurologically disabled children. Lancet. 1998;351:1254. doi: 10.1016/S0140-6736(05)79321-1. [DOI] [PubMed] [Google Scholar]
- 39.Molina-Carballo A, Munoz-Hoyos A, Reiter RJ, et al. Utility of high doses of melatonin as adjunctive anticonvulsant therapy in a child with severe myoclonic epilepsy: two years’ experience. J Pineal Res. 1997;23:97–105. doi: 10.1111/j.1600-079x.1997.tb00341.x. [DOI] [PubMed] [Google Scholar]