Abstract
Objective:
The aim of this study was to examine psychometric properties of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), diagnostics criteria for alcohol and marijuana dependences among 462 alcohol users and 311 marijuana users enrolled in two multisite trials of the National Drug Abuse Treatment Clinical Trials Network.
Method:
Diagnostic questions were assessed by the DSM-IV checklist. Data were analyzed by the item response theory and the multiple indicators–multiple causes method procedures.
Results:
Criterion symptoms of alcohol and marijuana dependences exhibited a high level of internal consistency. All individual symptoms showed good discrimination in distinguishing alcohol or marijuana users between high and low severity levels of the continuum. In both groups, “withdrawal” appeared to measure the most severe symptom of the dependence continuum. There was little evidence of measurement nonequivalence in assessing symptoms of dependence by gender, age, race/ethnicity, and educational level.
Conclusions:
These findings highlight the clinical utility of the DSM-IV checklist in assessing alcohol- and marijuana-dependence syndromes among treatment-seeking substance users.
In addiction treatment studies, investigators typically evaluate patients for the presence of addictive disorders, rely on self-reported diagnostic instruments for inclusion and exclusion criteria, and examine differences in treatment outcomes across diagnostic categories or key demographic groups (e.g., gender and race/ethnicity; Carroll, 1997). Hence it is imperative that the diagnostic instrument used to assess the presence of an addictive disorder measures the intended construct and that the instrument is equivalent for drug users with diverse demographic characteristics. In addition, there is a renewed focus on assessing the severity of addictions and other psychiatric disorders because, like other medical problems (e.g., asthma, cancer, and hypertension), these disorders present with varying levels of severity that have a growing number of treatment implications. For example, the Patient Placement Criteria of the American Society of Addiction Medicine provide guidelines for assigning patients to varying treatment intensities as a function of clinical judgments about severity and associated comorbidities. The present study seeks to inform the conceptualization of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 2000), and emerging DSM Fifth Edition (DSM-V) diagnostic criteria for alcohol and marijuana dependences and assesses item-response bias in the endorsement of these symptoms in a diverse sample of treatment-seeking stimulant users who participated in multisite randomized trials of the Clinical Trials Network (Peirce et al., 2006; Petry et al., 2005).
The dependence syndrome concept was introduced by Edwards and Gross (1976), who emphasized the coherence and unidimensionality of a set of behavioral, cognitive, and physiological components constituting a clinical syndrome for alcoholism. This syndrome concept provides the theoretical framework for diagnostic criteria used for alcohol- and drug-dependence disorders in the DSM, Third Edition, Revised (DSM-III-R; American Psychiatric Association, 1987; Bryant et al., 1991; Kosten et al., 1987); the DSM-IV (American Psychiatric Association, 2000; Feingold and Rounsaville, 1995); the International Classification of Diseases-10 (World Health Organization, 1992); and criteria that will be a focus of attention for DSM-V. This concept fundamentally suggests that elements of a dependence syndrome exist in degree and form a single factor.
Investigators have generally reported that a single factor captures the criteria of alcohol- and marijuana-dependence disorders (Feingold and Rounsaville, 1995; Rounsaville et al., 1993; Swift et al., 2001). However, most of these studies employ factor analysis to examine factor structures underlying the diagnostic criteria. Comparatively few reports have used item response theory (IRT) modeling (see Baker, 2001; Embretson and Reise, 2000; Hambleton et al., 1991; Saha et al., 2006) to evaluate and guide the conceptualization of DSM-IV criteria for alcohol and other drug dependences. IRT analyses can evaluate how well each diagnostic criteria performs and how much information each contributes to a disorder, as well as evaluate symptom-endorsing equivalence between demographic groups. For example, Saha et al. (2006) used IRT analyses to characterize the construct of alcohol-use disorders in a sample of the general population and showed how IRT can be used to evaluate symptom-endorsing equivalence between demographic groups (i.e., item severity estimates). This approach provides very relevant information for evaluating specific criteria employed to define the underlying construct of a given disorder.
Furthermore, measurement equivalence concerns whether the differences between groups in a latent construct such as dependence reflect true differences or item response bias (Teresi and Fleishman, 2007). Measurement nonequivalence or bias occurs when individuals with equivalent levels of a latent construct respond differently to a given instrument as a function of group membership (Chen and Anthony, 2003; Teresi and Fleishman, 2007). Measurement nonequivalence in a diagnostic instrument can lead to inaccurate comparisons across groups involving screening or diagnosing individuals, as well as assessing prevalence rates, risk factors, and severity (Chen and Anthony, 2003; McHorney and Fleishman, 2006). Because self-report instruments are prone to measurement bias (DeVellis, 2003), assessing measurement equivalence is fundamental to the development of measures for making unbiased diagnoses.
Multiple indicators-multiple causes (MIMIC) modeling can be used to detect measurement nonequivalence of the criteria for multiple demographic variables and, importantly, to compensate for them in the analysis of predictors of the latent construct within a regression framework and thereby reduce distortion of the risk factor assessment (e.g., Chen and Anthony, 2003; Grant et al., 2007). It improves recognition of the impact of item response bias detected on the latent dependence risk because it allows statistical adjustment for the effects of multiple background variables on the latent dependence risk. This latter feature represents a clear advantage over IRT methods. Because it is essential to demonstrate that the dependence construct assessed by a given instrument is adequate for use in different population subgroups, the present evaluation uses both IRT and MIMIC methods to study this issue.
Alcohol and marijuana dependences are among the most prevalent substance dependences (Grant et al., 2004b). Psychometric properties associated with their assessment and measurement equivalence among treatment-seeking patients are much less known than those among population-based participants (Agrawal and Lynskey, 2007; Gillespie et al., 2007; Saha et al., 2006). At present, a generic set of DSM-IV dependence criteria is applied to alcohol and all separate drug classes (American Psychiatric Association, 2000). For both research and clinical reasons, it is important to assess whether different substances with variations in pharmacological effects produce the same clinical dependence profile, whether specific dependence criteria are necessary for different substances, and which features are associated with more severe forms of dependence across substances (Hughes, 2006). Importantly, withdrawal symptoms from marijuana use are not officially recognized by DSM-IV (American Psychiatric Association, 2000), despite mounting evidence that they exist (Budney, 2006). A potentially valuable source of data to address these questions is available in the multisite Clinical Trials Network, because it provides a unique opportunity to evaluate the psychometric properties of current alcohol- and marijuana-dependence criteria (including marijuana withdrawal) in a geographically and clinically diverse group of drug users seeking treatment for substance-use problems across the United States.
Recent IRT studies of population-based participants (Gillespie et al., 2007; Lynskey and Agrawal, 2007) and addiction patients (Langenbucher et al., 2004) have found that lifetime abuse/dependence symptoms for alcohol or drug use form a single underlying continuum of risk and that item performance of the criteria varies across substances. For example, marijuana users are unlikely to endorse abuse/ dependence symptoms unless they are at relatively higher levels of severity as compared with users of other drugs (Gillespie et al., 2007). “Lifetime symptoms of withdrawal” appear to measure high levels of severity for an IRT-defined marijuana-use-disorder risk (Gillespie et al., 2007; Lynskey and Agrawal, 2007), whereas “giving up activities” captures high levels of severity for an IRT-defined alcohol-use-disorder risk (Langenbucher et al., 2004). Although these results are highly informative, the studies are somewhat limited because they focus on lifetime abuse/dependence symptoms, whereas DSM-IV requires the occurrence and clustering of at least three criteria within a 12-month period for a current diagnosis (American Psychiatric Association, 2000). On the other hand, Saha et al. (2006) examined directly current DSM-IV abuse/dependence criteria for alcohol-use disorders in a national sample of American adults. They found that cognitive-behavioral symptoms such as “time spent” and “taking larger amounts” were more discriminative than other criteria in measuring the latent construct and that “giving up activities” appeared to tap the most severe end on the continuum.
The present study investigates the psychometric properties and relationships of the DSM-IV diagnostic criteria for alcohol and marijuana with differing severities of the dependence disorder, as well as measurement equivalence and demographic predictors of the dependence risk, in a combined sample of treatment-seeking patients from two national multisite studies conducted within the Clinical Trials Network (Peirce et al., 2006; Petry et al., 2005). The large and diverse sample used in this study helps identify possible subgroups with a high severe level of dependence that might be targeted for more intensive or otherwise specific clinical interventions. The diversity of the sample and treatment programs represented in the study also enables us to replicate aspects of earlier work done in smaller or less diverse samples and settings, and to meaningfully extend that work by using psychometric modeling to address additional measurement questions not considered in those reports (Feingold and Rounsaville, 1995; Morgenstern et al., 1994; Rounsaville et al., 1993).
The specific questions tested in the study are (1) Do the criteria for current dependence form a single continuum of severity (i.e., one factor), and if they do, where along this continuum does each criterion rest?; (2) How well does each of these criteria perform, or discriminate, relative to the others?; (3) Does the probability of endorsing the criteria of dependence at the equivalent level of severity differ across gender, age group, racial/ethnic backgrounds, and treatment settings?; and (4) What demographic subgroups manifest the high level of severity on the dependence continuum?
Method
Data source
Statistical analyses were performed on data from the public-use files of two multisite studies of the Clinical Trials Network, which evaluated stimulant-use outcomes of an abstinence-based contingency management intervention as an addition to usual care in non-methadone maintenance treatment (non-MMT) (Petry et al., 2005) and in methadone maintenance treatment (MMT) (Peirce et al., 2006). All programs were outpatient community-based treatment providers associated with the Clinical Trials Network in their geographic regions. Non-MMT participants were recruited from eight treatment programs that did not administer methadone or other opioid agonists (Petry et al., 2005). Six of these programs were located in eastern, southeastern, or southwestern urban regions of the United States; one was located in the suburban southeast and one in the rural southwest. Eligible participants included patients who (1) reported stimulant use within 2 weeks of study entry, (2) used stimulants within 2 weeks of entering a controlled environment (a detoxification unit, hospital, or correctional facility) and exited the controlled environment within 2 weeks of study entry, or (3) submitted a stimulant-positive urine sample at treatment entry.
MMT participants were recruited from six programs located in urban areas in the northeastern, eastern, or southwestern United States (Peirce et al., 2006). Eligible participants included opioid-dependent patients who had (1) been enrolled in methadone maintenance for a minimum of 30 days but not longer than 3 years; (2) submitted a stimulant-positive (cocaine or amphetamines) urine sample in treatment or within 2 weeks of study enrollment based on clinic records; (3) reported that they were not in recovery from a gambling problem; and (4) demonstrated an understanding of study procedures by correctly answering 80% or more of the questions on a quiz covering the requirements, risks, and benefits of participation in the parent study.
Study variables
Social and demographic variables were collected at study intake: age, gender, race/ethnicity, and years of education. Specific substance-use disorders were assessed by the DSM-IV checklist (Hudziak et al., 1993; Wu et al., 2008). All participants were asked about past-year use of five classes of substances: amphetamines/methamphetamine, cocaine, opioids, alcohol, and marijuana. If participants reported use of a substance in the past year, they were asked about each of the seven DSM-IV dependence criteria associated with that substance (American Psychiatric Association, 2000). All seven dependence criteria were assessed by DSM-IV checklist: (1) tolerance, (2) withdrawal (e.g., manifesting two or more symptoms of withdrawal from alcohol use or taking alcohol to relieve or avoid withdrawal symptoms), (3) substance often taken in large amounts or for longer periods, persistent desire or unsuccessful attempt to cut down or control use, (5) a great deal of time spent in activities necessary to get the substance, (6) important activities given up, and (7) continued substance use despite knowledge of having persistent or recurrent physical or psychological problems. The parent studies from which these data are drawn coded participants who reported two or more of the following five symptoms as having marijuana withdrawal: (1) unable to sleep or sleeping too much, (2) eating much less, (3) poor concentration, (4) extreme tiredness/lack of energy, and headaches (unpublished Clinical Trials Network training documents: provided by coauthor R.K.B.). Consistent with DSM-IV (American Psychiatric Association, 2000), participants who reported three or more criterion symptoms of dependence from alcohol use were classified as having dependence. The same logic was applied to each of the other substances.
Data analyses
We first examined the distributions of study variables. Factor analysis of binary data was then conducted using Mplus (Muthén and Muthén, 2007) to examine the IRT's assumption of unidimensionality (Hambleton et al., 1991), which is established by demonstrating that a one-factor model provides the most parsimonious fit to the data. We assessed the number of factors to be retained with the scree test (Cattell, 1966), the ratio of the first eigenvalue to the second eigenvalue, and variance explained by the first eigenvector. A two-parameter normal ogive IRT modeling was then conducted with BILOG-MG3 (Zimowski et al., 2005). The two-parameter model allowed us to examine the relationship between the participants’ item performance and the traits underlying item performance, which is described by a monotonically increasing S-shaped item characteristic curve (Embretson and Reise, 2000). An item characteristic curve is characterized by item severity and discrimination parameters. An item severity (threshold) parameter indicates the position of the item characteristic curve in relation to the latent continuum (Embretson and Reise, 2000). It represents the latent trait z score in which the probability of a criterion symptom being present is 0.5 and measures the severity of a specific criterion on the IRT-defined latent trait continuum. The item discrimination parameter measures the degree of precision with which an item distinguishes between participants with levels of the latent trait above versus those with levels below the item's severity.
Test information curves (Baker, 2001) were also created. A test information curve describes where along the latent severity continuum the dependence items as a whole provide the greatest amount of information. The more information a test provides at a particular trait level, the smaller the standard errors in that range. Measurement equivalence was then examined using the differential criterion (item) functioning to determine whether severity estimates of each item functioned differently across groups by gender (male vs female), race/ethnicity (nonwhite vs white), age (<40 years vs ≥40 years), educational level (<high school vs ≥high school), and treatment setting (non-MMT vs MMT). The selection of these variables was based on their previously reported associations with alcohol- or marijuana-dependence syndromes (Agrawal and Lynskey, 2007; Anthony et al., 1994; Blanco et al., 2007; Grant et al., 2004a) and on the differences in substance use and treatment settings (non-MMT vs MMT). The presence of differential criterion functioning indicates measurement nonequivalence or item response bias across groups (i.e., differential item severity).
Finally, MIMIC modeling using Mplus (Muthén and Muthén, 2007) was conducted to examine further the presence of differential criterion functioning by demographic characteristics and treatment settings as well as to identify subgroups with higher levels of the dependence risk (i.e., the continuous latent liability to dependence measured by the seven criteria). The Tucker-Lewis index (TLI), comparative fit index (CFI), and the root mean square error of approximation (RMSEA) were used to assess the model fit. Values of TLI and CFI ≥ .95 (1 = perfect fit) and values of RMSEA ≤.06 (the lower the better) indicate an excellent fit to the data (Browne and Cudeck, 1993; Hu and Bentler, 1999).
Study sample
All participants reported past-year use of stimulants. Analyses were based on the subsample who also reported past-year use of alcohol (n = 462) or marijuana (n = 311). Psychometric properties of cocaine and opioid dependences are reported elsewhere (Wu et al., in press-b). The sample size of amphetamine users was too small for separate analyses. Consistent with prior IRT research (e.g., Langenbucher et al., 2004; Lynskey and Agrawal, 2007), groups were not mutually exclusive. Among alcohol users, 48% also used marijuana; among marijuana users, 72% also used alcohol. More than half (59%) of the participants in both groups were non-MMT patients (Table 1). Among alcohol users, 58% were ages 18–39, 52% were female, and 53% were black. Among marijuana users, 65% were ages 18–39, 49% were female, and 41% were black. Cocaine was the primary stimulant used by most alcohol (93%) or marijuana (87%) users.
Table 1.
Selected characteristics of outpatient stimulant users, by alcohol- and marijuana-use status
| Selected characteristics | Past-year alcohol users (n = 462), % | Past-year marijuana users (n = 311), % |
| Treatment setting | ||
| Non-methadone-maintenance treatment program | 59.3 | 58.5 |
| Methadone-maintenance treatment program | 40.7 | 41.5 |
| Age, years | ||
| 18–39 | 58.0 | 65.3 |
| ≥40 | 42.0 | 34.7 |
| Gender | ||
| Male | 48.3 | 51.1 |
| Female | 51.7 | 48.9 |
| Race/ethnicity | ||
| Black | 53.2 | 41.2 |
| White | 27.3 | 36.0 |
| Hispanic | 13.9 | 17.7 |
| Other | 5.6 | 5.1 |
| Education, years | ||
| <12 | 34.2 | 36.3 |
| ≥12 | 65.8 | 63.7 |
| Types of stimulants used | ||
| Amphetamines/methamphetamine | 14.3 | 24.4 |
| Cocaine | 93.1 | 86.5 |
| Past year DSM-IV substance abuse | ||
| Alcohol | 13.0 | 12.9 |
| Marijuana | 4.5 | 10.3 |
| Amphetamines | 0.9 | 1.3 |
| Cocaine | 4.1 | 3.5 |
| Opioids | 1.7 | 0.6 |
| Past year DSM-IV substance dependence | ||
| Alcohol | 40.9 | 30.2 |
| Marijuana | 17.3 | 35.0 |
| Amphetamines | 10.6 | 20.3 |
| Cocaine | 75.8 | 73.3 |
| Opioids | 38.1 | 43.4 |
| No. of DSM-IV dependence symptoms among users | ||
| 0 | 42.6 | 45.3 |
| 1 | 10.0 | 8.4 |
| 2 | 6.5 | 11.3 |
| 3 | 7.1 | 8.4 |
| 4 | 6.3 | 8.7 |
| 5 | 6.5 | 5.8 |
| 6 | 6.1 | 7.1 |
| 7 criterion symptoms | 14.9 | 5.1 |
Note: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Results
Prevalence of past year (current) DSM-IV substance-use disorders
Approximately 41% of alcohol users met criteria for DSM-IV alcohol dependence, and 35% of marijuana users met criteria for DSM-IV marijuana dependence. In both groups, the great majority also met criteria for cocaine dependence: 76% among alcohol users and 73% among marijuana users. Among alcohol users (n = 462), a higher prevalence of alcohol dependence was noted among women relative to men (47% vs 34%; χ2 test, p < .01), those without a high school diploma relative to those with more years of education (49% vs 37%; χ2 test, p = .02), and non-MMT patients relative to MMT patients (53% vs 24%; χ2 test, p < .01). Age group and race/ethnicity were not associated with alcohol dependence. Among marijuana users (n = 311), a higher prevalence of marijuana dependence was noted among patients younger than age 40 relative to those age 40 years or older (42% vs 21%; χ2 test, p < .01) and non-MMT patients relative to MMT patients (43% vs 24%; χ2 test, p < .01). gender, race/ethnicity, and educational level were not associated with alcohol dependence.
Unidimensionality of dependence criterion symptoms
The scree plot indicated that a one-factor model fit the data for alcohol- and marijuana-dependence criteria, respectively. The first eigenvalue and the first:second eigenvalue ratio were high for both substances (6.01/0.28 = 21.5 for alcohol dependence; 5.27/0.64 = 8.2 for marijuana dependence). The first eigenvector explained 86% of the variance for alcohol-dependence criteria and 75% for marijuana-dependence criteria. Both sets of the criteria also exhibited a high level of internal consistency (Cronbach's α coefficient ≥ 0.86). Results from a one-factor model further supported the unidimensionality (fit indexes: CFI = 0.996, TLI = 0.997, RMSEA = 0.067 for alcohol; CFI = 0.985, TLI = 0.987, RMSEA = 0.085 for marijuana).
Item characteristic curve: Symptom discrimination and severity
Alcohol.
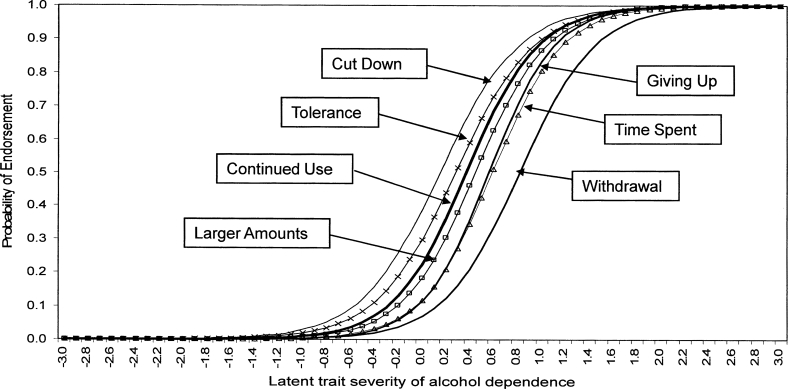
As shown in Table 2, all alcohol-dependence items exhibited good discrimination (1.8–2.2) in distinguishing between alcohol users along the dependence continuum. Several items had particularly good discrimination: “giving up activities,” “time spent using alcohol,” “taking larger amounts,” and “continued use despite having problems” (steeper lines in Figure 1). Of all the severity parameters (.2–.8), “withdrawal” represented a more severe symptom (estimate = .8) that was endorsed at higher severity levels or shifted to the right end of the item characteristic curve; “time spent using alcohol” and “giving up activities” measured the next most severe levels (Figure 1).
Table 2.
The item response theory analysis of past-year DSM-IV alcohol- and marijuana-dependence symptoms
| Symptoms of dependence | Alcohol users (n = 462) |
Marijuana users (n = 311) |
||||||
| Prev.% | Factor loadings | Item discrim. (SE) | Item severity (SE) | Prev. % | Factor loadings | Item discrim. (SE) | Item severity (SE) | |
| D1: Tolerance | 40.3 | .89 | 1.80 (0.14) | 0.28 (0.07) | 34.1 | .80 | 1.51 (0.12) | 0.52 (0.09) |
| D2: Withdrawal | 24.5 | .90 | 1.88 (0.16) | 0.82 (0.07) | 16.7 | .78 | 1.61 (0.13) | 1.17 (0.10) |
| D3: Taking larger amounts | 34.8 | .93 | 1.98 (0.17) | 0.45 (0.07) | 31.8 | .91 | 1.79 (0.16) | 0.58 (0.09) |
| D4: Unable to cut down | 44.4 | .87 | 1.79 (0.13) | 0.15 (0.06) | 39.9 | .82 | 1.60 (0.13) | 0.33 (0.09) |
| D5: Time spent using or recovering | 30.5 | .95 | 2.03 (0.18) | 0.59 (0.07) | 32.2 | .92 | 1.84 (0.17) | 0.56 (0.09) |
| D6: Giving up activities | 31.2 | .97 | 2.16 (0.21) | 0.56 (0.07) | 21.9 | .90 | 1.80 (0.17) | 0.92 (0.10) |
| D7: Continued use despite having problems | 37.2 | .92 | 1.97 (0.17) | 0.37 (0.07) | 21.5 | .84 | 1.66 (0.14) | 0.95 (0.10) |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; prev. = prevalence; discrim. = discrimination; D = dependence symptoms.
Figure 1.
Item characteristic curves for alcohol-dependence criteria. An item characteristic curve is characterized by item severity and discrimination parameters. It relates the probability of endorsing symptoms to the dependence continuum.
Marijuana.
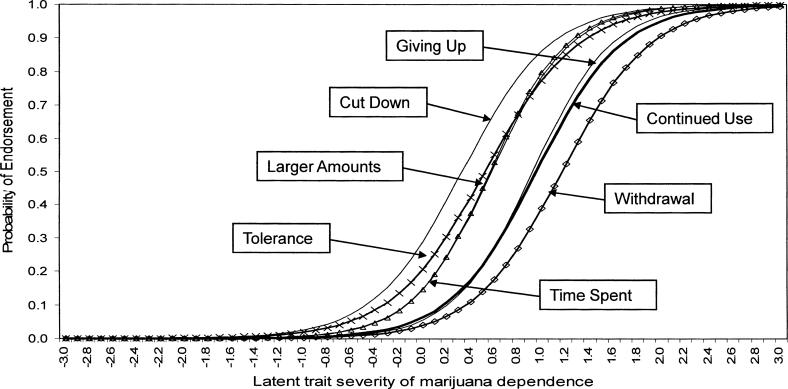
All marijuana-dependence items revealed moderately high values of discrimination (1.5–1.8), and the items found to have greater discrimination than the others were similar to the alcohol-dependence items. Of all severity parameters (0.3–1.2), “withdrawal” (estimate = 1.2) also represented the most severe symptom on the IRT-defined latent trait continuum; “continued use despite having problems” and “giving up activities” captured the next most severe levels (Figure 2).
Figure 2.
Item characteristic curves for marijuana-dependence criteria. An item characteristic curve is characterized by item severity and discrimination parameters. It relates the probability of endorsing symptoms to the dependence continuum.
Test information curve: Test information and measurement precision
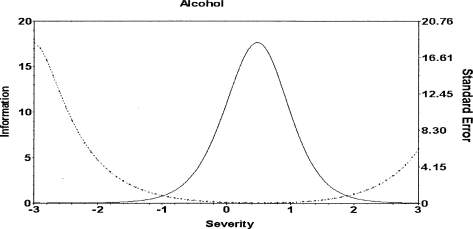
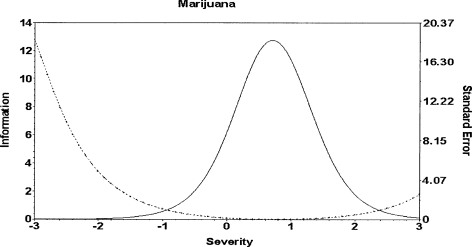
Test information curves and their aggregated standard errors of measurement were examined to better assess the amount of information yielded by the criteria across the dependence continuum (Figures 3 and 4). The alcohol-dependence criteria as a whole provided a good measure for a slightly narrow range of moderately severe levels on the continuum (i.e., low values of standard errors on both sides). The marijuana-dependence criteria provided a high level of information and precision in capturing a wider range of moderately severe levels on the continuum.
Figure 3.
Test information curve for alcohol-dependence criteria. The test information curve indicates where along the latent severity continuum the dependence items as a whole provide the most information. Solid line = the total test information; dotted line = standard error.
Figure 4.
Test information curve for marijuana-dependence criteria. The test information curve indicates where along the latent severity continuum the dependence items as a whole provide the most information. Solid line = the total test information; dotted line = standard error.
Differential criterion functioning: Item equivalence across groups
Results of differential criterion functioning from BILOG-MG3 indicated measurement equivalence in severity parameters of each criterion of alcohol and marijuana dependences by gender, race/ethnicity, age group, educational level, and treatment setting except for “alcohol tolerance” by treatment setting. The mean (SE) severity threshold of tolerance was significantly lower among MMT patients (−.27 [.087]) than among non-MMT patients (.12 [.069]). Thus, at the equivalent dependence level, MMT patients (with a lower severity threshold) were more likely than non-MMT patients to endorse “tolerance.”
Multiple indicators-multiple causes modeling
MIMIC modeling provided a further check on item response bias by allowing the inclusion of statistical adjustment for demographic and treatment setting variables in the same model. This information is not provided by IRT modeling because it examines item response bias one variable at a time (e.g., splitting into two groups). In addition, MIMIC modeling helps generate “less biased” estimates for subgroups at risk for dependence, while adjusting for the identified item response bias in a risk factor analysis. The MIMIC model of alcohol (CFI = 0.991, TLI = 0.995, RMSEA = 0.053) and marijuana dependence (CFI = 0.985, TLI = 0.989, RMSEA = 0.048) fit the data very well.
Measurement equivalence.
The results were consistent with differential criterion functioning findings from BILOG-MG3. MMT patients were more likely than non-MMT patients to endorse symptoms of tolerance from alcohol use (regression coefficient = .49, p < .001) even after holding constant the level of the latent dependence risk, key demographics, and treatment setting. In contrast, there was no differential criterion functioning for marijuana-dependence items.
Predictors of higher levels of the alcohol-dependence risk.
To explore the impact of item response bias on associations between each predictor and the dependence risk, we compared the model excluding differential criterion functioning (i.e., treatment setting on tolerance) with the model including it. The presence of differential criterion functioning was found to have no impact on associations for each demographic predictor, only a modest change in the association for treatment setting (from −.71 to −.80 after adjusting differential criterion functioning), and no change in the p values for each predictor. Using MIMIC modeling to hold constant item response bias (i.e., treatment setting on tolerance), women were much more likely than men to have higher levels of alcohol-dependence risk (regression coefficient = .21, p < .05). Patients with versus without a high school diploma (−.30, p < .01) and MMT patients compared with non-MMT patients (−.80, p < .01) had lower levels of alcohol-dependence risk. Race/ethnicity and age were not associated with alcohol-dependence risk.
Predictors of higher levels of marijuana-dependence risk.
MIMIC modeling showed that patients age 40 or older versus those younger than age 40 (−.28, p < .03) and MMT patients compared with non-MMT patients (−.40, p < .01) had lower levels of marijuana-dependence risk. gender, race/ethnicity, and education were not associated with marijuana-dependence risk.
Discussion
Within this diverse sample of MMT and non-MMT outpatients who reported recent stimulant use, 41% of participants who also used alcohol met DSM-IV criteria for alcohol dependence, and 35% of those who also used marijuana met criteria for marijuana dependence. The IRT analysis indicated that dependence on alcohol or marijuana as assessed by the DSM-IV checklist was arrayed along a continuum of severity. All individual diagnostic criteria also showed good discrimination in distinguishing substance users who were higher versus lower on the dependence severity continuum. The MIMIC modeling further revealed item severity equivalence in the endorsement of alcohol- or marijuana-dependence symptoms by gender, age group, race/ethnicity, and education level.
These findings provide both new and impressive evidence of a single-dimensional construct for alcohol- and marijuana-dependence syndromes and replicate prior studies reporting on smaller or less geographically diverse samples (e.g., Feingold and Rounsaville, 1995; Kosten et al., 1987; Morgenstern et al., 1994; Rounsaville et al., 1993). They also extend earlier work by demonstrating minimal item response biases in the endorsement of dependence symptoms by key demographic characteristics in a diverse sample. Although we found item response biases related to reporting of tolerance of alcohol use by treatment setting, this had no appreciable impact on estimates of associations between predictors and dependence risk in the MIMIC model. This suggests that the effect of item response bias may be minimal. It does suggest, however, that the alcohol-using MMT participants have a lower threshold for reporting tolerance to alcohol compared with alcohol-using non-MMT participants. Alcohol-use disorder is prevalent among MMT patients (Disney et al., 2005), and there is a possible pharmacokinetic interaction between alcohol and methadone, with alcohol altering the steady-state disposition kinetics of methadone (Tommasello and Adir, 1984). One possible future direction would be to examine whether co-use of alcohol and opioids decreases patients’ threshold for perceiving the need for increased amounts of alcohol to achieve the desired effect.
Item discrimination
Consistent with the study of cocaine and opioid dependence among MMT patients (Wu et al., in press-b) and of alcohol-use disorders among alcohol users in the community (Saha et al., 2006), symptoms indicative of compulsive substance use provided good discrimination between patients with varying levels of dependence. “Taking larger amounts,” “time spent using the substance,” “giving up other activities,” and “continued use despite problems” all showed good discrimination and precision in measuring the alcohol- and marijuana-dependence continuum. Additional research might be able to show that these items may have good clinical utility as rapid screens to identify problematic users that may benefit from additional monitoring or more focused interventions. As noted by Edwards (2008), the dependence syndrome is a very personal experience, and these results support his recommendation that cognitive components of compulsive substance use should be evaluated in patients.
Item severity
According to DSM-IV (American Psychiatric Association, 2000), the presence of either tolerance or withdrawal constitutes a physiological subtype of dependence that is widely regarded as a severity indicator. Irrespective of alcohol or marijuana use, we found that “withdrawal” measured a high level of severity on the dependence continuum as defined by IRT modeling, whereas “tolerance” indicated a lower severity level. Prior studies have found that alcohol withdrawal symptoms, but not tolerance, predicted poorer treatment outcomes for alcohol-dependence disorder (Hasin et al., 2000) and a greater number of substance use-related problems (Schuckit et al., 2003). The present findings replicate earlier findings and do so in a more diverse sample of patients and treatment programs and modalities. Also, similar to other studies (Hasin et al., 2000; Schuckit et al., 2003), the present findings do not favor the value of tolerance alone in determining physiological dependence in DSM-IV. One reasonable direction for future work would be to determine whether the item of higher dependence risk (i.e., withdrawal) from IRT modeling can be used as an indicator of the need for medical detoxification or for more intensive inpatient or outpatient management, as suggested by current American Society of Addiction Medicine guidelines.
It is noteworthy that the marijuana withdrawal symptoms reported by participants indicated severe levels on the IRT-defined dependence continuum given that DSM-IV does not recognize the presence of withdrawal for this drug class (American Psychiatric Association, 2000). Nonetheless, a laboratory model for marijuana withdrawal has been reported (Lichtman and Martin, 2005). Other recent studies both support and extend the laboratory work by providing further evidence for a marijuana withdrawal syndrome and its association with higher levels of continuous use (Budney, 2006) and a more severe dependence syndrome (Gillespie et al., 2007; Lynskey and Agrawal, 2007). Likewise, the present study dovetails with some earlier findings showing that adults with versus without a self-reported history of marijuana withdrawal had a more severe spectrum of drug-use problems (Schuckit et al., 1999).
Budney (2006) recently proposed six symptoms of marijuana withdrawal for consideration in DSM-V (i.e., anger or aggression, decreased appetite or weight loss, irritability, nervousness or anxiety, restlessness, and sleep difficulties). Several of the withdrawal symptoms listed in the present study resemble those suggested by Budney (2006): unable to sleep/sleeping too much and eating much less); the remaining three have been reported by marijuana users as withdrawal symptoms (Budney, 2006; Budney et al., 2003; Crowley et al., 1998). Because specific withdrawal symptoms were not individually recorded in the public-use data files in the present study, a further analysis of individual withdrawal symptoms was not possible. Additional investigations applying IRT modeling to marijuana users would help to determine the discrimination and precision of each observed symptoms of withdrawal in relation to the marijuana-dependence construct.
Predictors of the dependence risk
Finally, MIMIC modeling indicated that alcohol users who were female, less educated, or in non-MMT programs had higher levels of alcohol-dependence risk and that marijuana users younger than age 40 or in non-MMT programs had higher levels of marijuana-dependence risk. Hence, treatment-seeking substance users who are using these drugs, especially if they are female, younger, and less educated, may require extra clinical monitoring because of their elevated risk for substance dependence. Results also suggest that female stimulant users who consume alcohol may be at heightened risk for problem use given their increased risk for alcohol dependence and that substance dependence in non-MMT patients may be equally severe in MMT patients. This heightened risk for alcohol dependence among female stimulant users in the present study has some important implications for clinical interventions and research because the association was robust and was not distorted by item response bias in relation to the other key demographic variables examined. This finding may be related to heightened risk for stimulant dependence among women compared with men (Wu et al., in press-a; Wu and Schlenger, 2003). For instance, our study of latent class analysis of cocaine dependence among treatment-seeking cocaine users found that women were significantly more likely than men to be classified into the most severe subtype, characterized by exhibiting almost all of the dependence criteria (Wu et al., in press-a). Because cocaine- and alcohol-dependence disorders are frequently comorbid (Higgins et al., 1994; Brooner et al., 1997) and alcohol is often used by cocaine users to moderate the agitation and general discomfort associated with postcocaine use (Magura and Rosenblum, 2000), increased levels of alcohol dependence may occur in combination with cocaine dependence as noted in this sample.
Limitations and strengths
These results are based on a clinically diverse sample of substance abusers who were in treatment for abuse of stimulants or other substances (e.g., opioids, alcohol, and marijuana) and may not generalize well to treatment-seeking substance users or the general population who do not use stimulants. The study sample may represent a group of more problematic users of alcohol or marijuana than those in the general population. Although this is a limitation of the study, it is also one of its strengths. The data were collected from patients in 14 outpatient programs across the United States, stimulant use is commonly reported in these and similar settings, and stimulant use (cocaine or amphetamines) constitutes more than 70% of illicit drug-related visits to hospital emergency departments nationally (Substance Abuse and Mental Health Services Administration, 2007). Findings from the present report are likely to generalize to these settings. In addition, this study showed that patient-reported dependence on alcohol or marijuana can be assessed appropriately, a finding that favors the use of patient-reported outcome measures in addiction treatment trials (Babor et al., 2000).
Another limitation of the study is the possibility of inaccurate reporting or recall errors because of reliance on self-reported symptoms without other informant information. This problem is common in the field and one that limits most studies in this area. The fact that our present findings replicate and extend those of earlier studies, however, does provide some assurance of the validity of these data (Babor et al., 2000). Comparisons of our findings concerning marijuana withdrawal with others are also limited by a lack of agreement on the presence or characteristics of its symptoms in the literature. Nonetheless, the symptoms that were assessed, although not comprehensive, were consistent with reports (Budney, 2006; Budney et al., 2003; Crowley et al., 1998) and with other studies reporting marijuana withdrawal symptoms as a significant correlate of continuing use and a more severe problem profile (Budney, 2006; Schuckit et al., 1999). Lastly, because of resource constraints, abuse was not assessed among subjects who met the criteria for dependence on the substance in question because a diagnosis of dependence excludes a diagnosis of abuse (American Psychiatric Association, 2000) and because having the abuse data for participants who met the criterion for dependence on a given drug class was deemed unnecessary for the purposes of the primary studies. Thus the psychometric properties of DSM-IV abuse criteria were not examined.
Conclusions and implications
Results from this psychometric modeling study favor the clinical utility of the DSM-IV checklist in assessing alcohol and marijuana dependences among substance abusers in methadone and nonmethadone treatment programs who also use stimulants. They clearly support the construct of a dependence syndrome with varying levels of severity for both marijuana and alcohol in this diverse sample. The generic set of dependence criteria employed in DSM-IV that consist of components of neuroadaptation (tolerance and withdrawal), maladaptive cognitions, and impaired control of substance use (American Psychiatric Association, 2000) appears to be applicable to either alcohol or marijuana dependence. If no biological marker or better construct for dependence emerges (Koob, 2006), this study suggests that, when moving to DSM-V, there is little reason for changing these criteria for alcohol and marijuana. These data also show that withdrawal symptoms identify a relatively high severity level of dependence on the IRT-defined continuum across alcohol and marijuana users. Thus, withdrawal symptoms for marijuana use should be studied further for consideration of including in the DSM-V. The presence of withdrawal symptoms in patients reporting marijuana use suggests that it is important to more clearly define them and to emphasize the importance of discussions between clinicians and patients about their marijuana use and the process of stopping. The consistent association between severity of dependence and withdrawal supports the DSM-IV subtyping of “with or without physiological features” and that this item should continue to have a significant role in treatment planning and patient placement criteria.
Acknowledgments
The authors wish to thank the participants, staff, investigators, and others who made the original studies and this work possible. We thank Amanda McMillan for editorial assistance.
Footnotes
This research was supported by National Institute on Drug Abuse contract HHSN271200522071C (principal investigator: Dan G. Blazer) to the Duke University Medical Center. The Duke University Institutional Review Board exempted the present study from review because it used existing de-identified and public-use data. The opinions expressed in this article are solely those of the authors and do not necessarily reflect those of the sponsoring agency.
References
- Agrawal A, Lynskey MT. Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the National Epidemiological Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;88:300–307. doi: 10.1016/j.drugalcdep.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR) Washington, DC: 2000. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Exp. Clin. Psychopharmacol. 1994;2:244–268. [Google Scholar]
- Babor T, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. J. Stud. Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Baker F. The Basics of Item Response Theory. College Park, MD: ERIC Clearinghouse on Assessment and Evaluation, University of Maryland; 2001. [Google Scholar]
- Blanco C, Harford TC, Nunes E, Grant B, Hasin D. The latent structure of marijuana and cocaine use disorders: Results from the National Longitudinal Alcohol Epidemiologic Survey (NLAES) Drug Alcohol Depend. 2007;91:91–96. doi: 10.1016/j.drugalcdep.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooner RK, King VL, Kidorf M, Schmidt CW, Jr, Bigelow GE. Psychiatric and substance use comorbidity in treatment-seeking opioid abusers. Arch. Gen. Psychiat. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Thousand Oaks, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Bryant KJ, Rounsaville BJ, Babor TF. Coherence of the dependence syndrome in cocaine users. Brit. J. Addict. 1991;86:1299–1310. doi: 10.1111/j.1360-0443.1991.tb01705.x. [DOI] [PubMed] [Google Scholar]
- Budney AJ. Are specific dependence criteria necessary for different substances: How can research on cannabis inform this issue? Addiction. 2006;101(Suppl.No. 1):125–133. doi: 10.1111/j.1360-0443.2006.01582.x. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Vandrey RG. The time course and significance of cannabis withdrawal. J. Abnorm. Psychol. 2003;112:393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- Carroll KM. New methods of treatment efficacy research: Bridging clinical research and clinical practice. Alcohol Hlth Res. World. 1997;21:352–359. [PMC free article] [PubMed] [Google Scholar]
- Cattell RB. The scree test for the number of factors. Multivar. Behav. Res. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Chen CY, Anthony JC. Possible age-associated bias in reporting of clinical features of drug dependence: Epidemiological evidence on adolescent-onset marijuana use. Addiction. 2003;98:71–82. doi: 10.1046/j.1360-0443.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, MacDonald MJ, Whitmore EA, Mikulich SK. Cannabis dependence, withdrawal, and reinforcing effects among adolescents with conduct symptoms and substance use disorders. Drug Alcohol Depend. 1998;50:27–37. doi: 10.1016/s0376-8716(98)00003-9. [DOI] [PubMed] [Google Scholar]
- DeVellis RF. Scale Development: Theory and Applications. 2nd Edition. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- Disney ER, Kidorf M, King VL, Neufeld K, Kolodner K, Brooner RK. Prevalence and correlates of cocaine physical dependence subtypes using the DSM-IV in outpatients receiving opioid agonist medication. Drug Alcohol Depend. 2005;79:23–32. doi: 10.1016/j.drugalcdep.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Edwards G. Substance dependence and substance-related problems: An agenda-setting debate. A further commentary on Li et al. Addiction. 2008;103:179–180. doi: 10.1111/j.1360-0443.2007.02107.x. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: Provisional description of a clinical syndrome. BMJ. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item Response Theory for Psychologists. Mahwah, NJ: Lawrence Erlbaum; 2000. [Google Scholar]
- Feingold A, Rounsaville B. Construct validity of the dependence syndrome as measured by DSM-IV for different psychoactive substances. Addiction. 1995;90:1661–1669. doi: 10.1046/j.1360-0443.1995.901216618.x. [DOI] [PubMed] [Google Scholar]
- Gillespie NA, Neale MC, Prescott CA, Aggen SH, Kendler KS. Factor and item-response analysis DSM-IV criteria for abuse of and dependence on cannabis, cocaine, hallucinogens, sedatives, stimulants and opioids. Addiction. 2007;102:920–930. doi: 10.1111/j.1360-0443.2007.01804.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004a;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthén BO, Yi HY, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: Further evidence of validity in the general population. Drug Alcohol Depend. 2007;86:154–166. doi: 10.1016/j.drugalcdep.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiat. 2004b;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of Item Response Theory. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Hasin D, Paykin A, Meydan J, Grant B. Withdrawal and tolerance: Prognostic significance in DSM-IV alcohol dependence. J. Stud. Alcohol. 2000;61:431–438. doi: 10.15288/jsa.2000.61.431. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Badger GJ. Alcohol dependence and simultaneous cocaine and alcohol use in cocaine-dependent patients. J. Addict. Dis. 1994;13(4):177–189. doi: 10.1300/j069v13n04_06. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equat. Model. 1999;61:1–55. [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, Przybeck T. The use of the DSM-III-R checklist for initial diagnostic assessment. Comprehen. Psychiat. 1993;134:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Should criteria for drug dependence differ across drugs? Addiction. 2006;101(Suppl. No. 1):134–141. doi: 10.1111/j.1360-0443.2006.01588.x. [DOI] [PubMed] [Google Scholar]
- Koob GF. The neurobiology of addiction: A neuroadaptational view relevant for diagnosis. Addiction. 2006;101(Suppl. No. 1):23–30. doi: 10.1111/j.1360-0443.2006.01586.x. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Babor TF, Spitzer RL, Williams JB. Substance-use disorders in DSM-III-R: Evidence for the dependence syndrome across different psychoactive substances. Brit. J. Psychiat. 1987;151:834–843. doi: 10.1192/bjp.151.6.834. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Labouvie E, Martin CS, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. J. Abnorm. Psychol. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Lichtman AH, Martin BR. Cannabinoid tolerance and dependence. Handbook Exp. Pharmacol. 2005;168:691–717. doi: 10.1007/3-540-26573-2_24. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Agrawal A. Psychometric properties of DSM assessments of illicit drug abuse and dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Psychol. Med. 2007;37:1345–1355. doi: 10.1017/S0033291707000396. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Fleishman JA. Assessing and understanding measurement equivalence in health outcome measures: Issues for further quantitative and qualitative inquiry. Med. Care. 2006;44(11 Suppl. 3):S205–S210. doi: 10.1097/01.mlr.0000245451.67862.57. [DOI] [PubMed] [Google Scholar]
- Magura S, Rosenblum A. Modulating effect of alcohol use on cocaine use. Addict. Behav. 2000;25:117–122. doi: 10.1016/s0306-4603(98)00128-2. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Langenbucher J, Labouvie EW. The generalizability of the dependence syndrome across substances: An examination of some properties of the proposed DSM-IV dependence criteria. Addiction. 1994;89:1105–1113. doi: 10.1111/j.1360-0443.1994.tb02787.x. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Mplus: Statistical Analysis with Latent Variables, Version 4.2.1. Los Angeles, CA: Muthén and Muthén; 2007. [Google Scholar]
- Peirce JM, Petry NM, Stitzer ML, Blaine J, Kellogg S, Satterfield F, Schwartz M, Krasnansky J, Pencer E, Silva-Vazquez L, Kirby KC, Royer-Malvestuto C, Roll JM, Cohen A, Copersino ML, Kolodner K, Li R. Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: A National Drug Abuse Treatment Clinical Trials Network study. Arch. Gen. Psychiat. 2006;63:201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, Obert J, Killeen T, Saladin ME, Cowell M, Kirby KC, Sterling R, Royer-Malvestuto C, Hamilton J, Booth RE, Macdonald M, Liebert M, Rader L, Burns R, DiMaria J, Copersino M, Stabile PQ, Kolodner K, Li R. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: A National Drug Abuse Treatment Clinical Trials Network study. Arch. Gen. Psychiat. 2005;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Bryant K, Babor T, Kranzler H, Kadden R. Cross system agreement for substance use disorders: DSM-III-R, DSM-IV and ICD-10. Addiction. 1993;88:337–348. doi: 10.1111/j.1360-0443.1993.tb00821.x. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Daeppen JB, Danko GP, Tripp ML, Smith TL, Li TK, Hesselbrock VM, Bucholz KK. Clinical implications for four drugs of the DSM-IV distinction between substance dependence with and without a physiological component. Amer. J Psychiat. 1999;156:41–49. doi: 10.1176/ajp.156.1.41. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Danko GP, Smith TL, Hesselbrock V, Kramer J, Bucholz K. A 5-year prospective evaluation of DSM-IV alcohol dependence with and without a physiological component. Alcsm Clin. Exp. Res. 2003;27:818–825. doi: 10.1097/01.ALC.0000067980.18461.33. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (Office of Applied Studies) Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. Drug Abuse Warning Network, 2005: National Estimates of Drug-Related Emergency Department Visits, DAWN Series D-29, DHHS Publication No. (SMA) 07–4256. [Google Scholar]
- Swift W, Hall W, Teesson M. Characteristics of DSM-IV and ICD-10 cannabis dependence among Australian adults: Results from the National Survey of Mental Health and Wellbeing. Drug Alcohol Depend. 2001;63:147–153. doi: 10.1016/s0376-8716(00)00197-6. [DOI] [PubMed] [Google Scholar]
- Teresi JA, Fleishman JA. Differential item functioning and health assessment. Qual. Life Res. 2007;16(Suppl. No. 1):33–42. doi: 10.1007/s11136-007-9184-6. [DOI] [PubMed] [Google Scholar]
- Tommasello AC, Adir J. Alcohol and the steady-state disposition kinetics of methadone in rats. J. Stud. Alcohol. 1984;45:155–159. doi: 10.15288/jsa.1984.45.155. [DOI] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Patkar AA, Stitzer ML, Wakim PG, Brooner RK. Heterogeneity of stimulant dependence: A National Drug Abuse Treatment Clinical Trials Network (CTN) study. Amer. J. Addict. in press-a doi: 10.1080/10550490902787031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Stitzer ML, Patkar AA, Blaine JD. Infrequent illicit methadone use among stimulant-using patients in methadone maintenance treatment programs: A National Drug Abuse Treatment Clinical Trials Network Study. Amer. J. Addict. 2008;17:304–311. doi: 10.1080/10550490802138913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Pan JJ, Blazer DG, Tai B, Brooner RK, Stitzer ML, Patkar AA, Blaine JD. The construct and measurement equivalence of cocaine and opioid dependences: A National Drug Abuse Treatment Clinical Trials Network (CTN) study. Drug Alcohol Depend. in press-b doi: 10.1016/j.drugalcdep.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Schlenger WE. Psychostimulant dependence in a community sample. Subst. Use Misuse. 2003;38:221–248. doi: 10.1081/JA-120017246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- Zimowski M, Muraki E, Mislevy R, Bock D. The BILOG-MG3 Statistical Program. Lincolnwood, IL: Scientific Software International; 2005. [Google Scholar]