Abstract
OBJECTIVE
Phosphorylation of two members of the TBC1 domain family of proteins, Akt substrate of 160 kDa (AS160, also known as TBC1D4) and TBC1D1, has been implicated in the regulation of glucose transport in skeletal muscle. Insulin-stimulated phosphorylation (measured using the phospho-Akt substrate [PAS] antibody) of AS160 and TBC1D1 appears to occur in an Akt-dependent manner, but the kinases responsible for contraction-stimulated PAS-AS160 and PAS-TBC1D1 remain unclear. AMP-activated protein kinase (AMPK) and Akt, both activated by contraction, can each phosphorylate AS160 and TBC1D1 in cell-free assays.
RESEARCH DESIGN AND METHODS
To evaluate the roles of AMPK and Akt on insulin- or contraction-stimulated PAS-AS160, PAS-TBC1D1, and glucose transport, rat epitrochlearis was incubated with and without compound C (inhibitor of AMPK) or Wortmannin (inhibitor of phosphatidylinositol [PI] 3-kinase, which is upstream of Akt) before and during insulin stimulation or contraction.
RESULTS
Insulin-stimulated glucose transport and phosphorylation of both AS160 and TBC1D1 were completely inhibited by Wortmannin. Wortmannin eliminated contraction stimulation of phospho-Ser21/9glycogen synthase kinase 3α/β (pGSK3; Akt substrate) and PAS-AS160 but did not significantly alter pAMPK, phospho-Ser79acetyl CoA carboxylase (pACC; AMPK substrate), PAS-TBC1D1, or glucose transport in contraction-stimulated muscle. Compound C completely inhibited contraction-stimulated pACC and PAS-TBC1D1 and partially blocked glucose transport, but it did not significantly alter pAkt, pGSK3, or PAS-AS160.
CONCLUSIONS
These data suggest that 1) insulin stimulates glucose transport and phosphorylation of AS160 and TBC1D1 in a PI 3-kinase/Akt–dependent manner, 2) contraction stimulates PAS-AS160 (but not PAS-TBC1D1 or glucose transport) in a PI 3-kinase/Akt–dependent manner, and 3) contraction stimulates PAS-TBC1D1 and glucose transport (but not PAS-AS160) in an AMPK-dependent manner.
Insulin and contractile activity, the two most important physiological stimuli that increase glucose transport in skeletal muscle, can each induce the translocation of GLUT4 glucose transporters from the cell's interior to its surface membranes (1,2). However, they regulate glucose transport via distinct signaling pathways (3). Insulin-stimulated glucose transport requires phosphatidylinositol (PI) 3-kinase activation, which leads to Akt activation without stimulating AMP-activated protein kinase (AMPK) (3–6). A great deal of evidence suggests that contraction stimulates glucose transport by a mechanism independent of PI 3-kinase/Akt (7–10) and attributable to the effects of multiple inputs, with AMPK- and calcium-mediated processes being major factors (11,12).
In 3T3-L1 adipocytes, insulin stimulates phosphorylation of Akt substrate of 160 kDa (AS160; also called TBC1D4) in an Akt-dependent manner on sites identifiable by the phospho-Akt substrate (PAS) antibody (13,14). AS160 includes a Rab GTPase-activating protein domain (RabGAP) that inhibits Rab proteins involved in regulating vesicular traffic (15). The insulin-mediated increase in PAS phosphorylation of AS160 (PAS-AS160) appears to inhibit RabGAP activity, thereby allowing GLUT4 to be recruited to surface membranes and elevate glucose transport (14–17). In skeletal muscle, insulin or contraction results in elevated PAS-AS160 (18,19), and AS160 phosphorylation appears to regulate glucose transport (20).
Recently, TBC1D1, a RabGAP protein paralog to AS160, was also shown to become PAS-phosphorylated (PAS-TBC1D1) in response to insulin in an Akt-dependent manner (21). However, whereas AS160 knockdown in 3T3-L1 adipocytes resulted in elevated basal cell-surface GLUT4 (17,22), TBC1D1 knockdown had no effect on basal cell-surface GLUT4 in 3T3-L1 cells (23). TBC1D1 protein is only ∼5% as abundant as AS160 protein in 3T3-L1 adipocytes, which may explain why TBC1D1 does not appear to play a major role in regulating glucose transport in these cells (23). TBC1D1 protein abundance is much greater in skeletal muscle versus adipose tissue (24), and silencing TBC1D1 in L6 myotubes resulted in increased basal cell-surface GLUT4 (25), supporting the idea that TBC1D1 inhibits GLUT4 translocation in the basal state. However, in contrast to the results for L6 cells with AS160 knockdown (which did not alter the insulin-stimulated net increase in cell-surface GLUT4), silencing TBC1D1 in L6 cells resulted in greater insulin-induced GLUT4 translocation versus control cells (25). In other words, TBC1D1 knockdown allowed insulin to induce a greater amount of GLUT4 translocation than in cells that express TBC1D1. These findings suggest that at least a portion of the inhibitory effects of TBC1D1 on GLUT4 may not be restrained by insulin. However, they do not eliminate the possibility that TBC1D1 can regulate an insulin-independent increase in glucose transport (e.g., with contraction). PAS-TBC1D1 is elevated in response to contraction in rodent skeletal muscle (19,24). Therefore, it seems possible that PAS-TBC1D1 may play a role in mediating contraction-stimulated glucose transport.
Experiments using purified Akt or AMPK demonstrated that each kinase can phosphorylate both AS160 and TBC1D1 in cell-free assays (26,27). Considerable evidence indicates that the insulin-stimulated increase in PAS-AS160 is Akt dependent in skeletal muscle (18,28), and increased AS160 phosphorylation appears to be important for the full effect of insulin on glucose transport (20). However, the specific kinases responsible for contraction-stimulated PAS-AS160 need to be clarified because: 1) Wortmannin can completely inhibit the contraction-stimulated increase in PAS-AS160 in rat skeletal muscle, suggesting that Akt is responsible for the increased PAS-phosphorylation of AS160 during contraction (18), but 2) muscles from mice with genetically disrupted AMPK versus wild-type littermates had reduced contraction-stimulated increase in immunoreactivity toward PAS antibody at ∼160 kDa (PAS-160) (28,29).
The primary aim of this study was to elucidate the contributions of Akt and AMPK on increases in PAS-AS160 and PAS-TBC1D1 in skeletal muscle stimulated by insulin or contraction. The PI 3-kinase inhibitor Wortmannin was used to prevent Akt activation (without altering AMPK activation), and compound C, a potent AMPK inhibitor (30), was used to prevent AMPK activation (without altering Akt activation). A secondary aim was to determine whether inhibition of insulin- or contraction-stimulated increases in PAS-AS160 or PAS-TBC1D1 was accompanied by attenuated insulin- or contraction-stimulated glucose transport. We hypothesized that in isolated rat epitrochlearis muscle: 1) Akt-dependent mechanisms are essential for the insulin-stimulated increases in glucose transport and phosphorylation of AS160 and TBC1D1; 2) Akt-dependent (but not AMPK-dependent) mechanisms are essential for contraction-stimulated increases in PAS-AS160, but not glucose transport; and 3) AMPK-dependent (but not Akt-dependent) mechanisms are essential for contraction-stimulated increases in PAS-TBC1D1 (but not PAS-AS160) and glucose transport.
RESEARCH DESIGN AND METHODS
Human recombinant insulin was obtained from Eli Lilly (Indianapolis, IN). Wortmannin was purchased from Sigma-Aldrich (St. Louis, MO). Compound C was from EMD Chemicals (San Diego, CA). Reagents for SDS-PAGE and immunoblotting, including Precision Plus Protein dual-color standards, were from Bio-Rad (Hercules, CA). Bicinchoninic acid protein assay reagent, T-PER tissue protein extraction reagent, and West Dura extended duration substrate were from Pierce Biotechnology (Rockford, IL). Anti–phospho-Thr308Akt (pAkt), anti–phospho-Ser21/9glycogen synthase kinase 3α/β (pGSK3), anti-GSK3α, anti–phospho-Thr172AMPK (pAMPK), anti-AMPK, anti–phospho-Ser79acetyl CoA carboxylase (pACC), anti-ACC, anti–phospho-Thr286Ca2+/calmodulin-dependent kinase II (pCaMKII), anti-CaMKII, anti–phospho-(Ser/Thr) Akt substrate (PAS; which was designed to recognize Akt phosphorylation motif peptide sequences [RXRXXpT/S]), and goat anti-rabbit IgG HRP conjugate were from Cell Signaling Technology (Danvers, MA). TBC1D1 polyclonal antibody was provided by Dr. Jianxin Xie (Cell Signaling Technology). AS160 antibody was from Millipore (Billerica, MA). Anti-Akt1/2/3, Preclearing Matrix F, and ExactaCruz F-HRP were from Santa Cruz Biotechnology (Santa Cruz, CA). 3-O-methyl-[3H]glucose ([3H]3-MG) was from Sigma-Aldrich, and [14C]mannitol was from Perkin Elmer (Waltham, MA). Other reagents were from Sigma-Aldrich or Fisher Scientific (Pittsburgh, PA).
Animal treatment.
Procedures for animal care were approved by the University of Michigan committee on use and care of animals. Male Wistar rats (∼150–200 g; Harlan, Indianapolis, IN) were provided with rodent chow (Lab Diet; PMI Nutritional International, Brentwood, MO) and water ad libitum until 1700 the night before the experiment, when their food was removed. The next day, between 1000 and 1300, rats were anesthetized (intraperitoneal injection of sodium pentobarbital, 60 mg/kg wt). While rats were deeply anesthetized, both epitrochlearis muscles were rapidly extracted.
Muscle treatment.
Isolated epitrochlearis muscles were preincubated in Krebs-Henseleit buffer (KHB) + 0.1% BSA + 8 mmol/l glucose (solution 1) in a water bath at 35°C with continuous gassing (95% O2/5% CO2). During this step, one muscle per rat was incubated in solution 1 with either 500 nmol/l Wortmannin (30 min) or 40 μmol/l compound C (60 min); stock solutions of each inhibitor were dissolved in vehicle (DMSO), and the contralateral muscle was incubated in solution 1 containing vehicle (Wortmannin, 0.05% DMSO; compound C, 0.4% DMSO). Inhibitors or vehicle remained at the same concentration throughout subsequent incubations. Some muscles were transferred to vials containing identical media for 20 min (basal). Other muscles were attached to a glass rod and force transducer (Radnoti, Litchfield, CT) as previously described (31). Mounted muscles were incubated in solution 1 with gassing (95% O2/5% CO2) and stimulated to contract as previously described (20 min, 2 ms pulse, 120 pulses/min, 25V; Grass S48 stimulator; Grass Instruments, Quincy, MA) (19). Immediately afterward, muscles were either freeze-clamped or transferred to vials containing KHB + 2 mmol/l pyruvate + 36 mmol/l mannitol (solution 2; 30°C, 10 min) before 3-MG transport measurement.
In separate experiments, muscles preincubated with inhibitors or vehicle were transferred to vials with solution 1 supplemented with either insulin (2,000 μU/ml, 20 min) or 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR; 2 mmol/l, 40 min). Muscles were then either freeze-clamped or transferred to vials with solution 2 for 10 min before 3-MG transport measurement.
Measurement of 3-MG transport.
After 10-min incubation in solution 2, muscles were transferred to flasks containing KHB, 0.1% BSA with 8 mmol/l 3-MG (including [3H]3-MG at a final specific activity of 0.25 mCi/mmol), and 2 mmol/l mannitol (including [14C]mannitol at a final specific activity of 6.25 μCi/mmol) (32). After 10 min, muscles were rapidly blotted, trimmed, freeze-clamped, and stored (−80°C) until processed.
Homogenization.
Muscles used for glucose transport and immunoblotting were homogenized in 1 ml ice-cold homogenization buffer (20 mmol/l Tris-HCl, pH 7.4, 150 mmol/l NaCl, 1% Igepal CA-639, 2 mmol/l Na3VO4, 2 mmol/l EDTA, 2 mmol/l EGTA, 2.5 mmol/l sodium pyrophosphate, 20 mmol/l β-glycerophosphate, 2 mmol/l phenylmethanesulphonylfluoride, and 1 μg/ml leupeptin) using glass-on-glass tubes (Kontes, Vineland, NJ). Homogenates were rotated (4°C, 1 h) before being centrifuged (12,000g, 10 min, 4°C). Aliquots of supernatant used for 3-MG transport measurement were pipetted into vials for scintillation counting, and 3-MG transport was determined (32). A portion of supernatant was used to determine protein concentration per the manufacturer's instructions (catalog no. 23227; Pierce Biotechnology). Remaining supernatant was stored at −80°C until further analysis.
Immunoprecipitation.
Muscles to be immunoprecipitated by anti-PAS or anti-TBC1D1 were homogenized in T-PER–supplemented homogenization buffer (2 mmol/l Na3VO4, 2 mmol/l EDTA, 2 mmol/l EGTA, 2.5 mmol/l sodium pyrophosphate, 1 mmol/l β-glycerophosphate, 1 mmol/l phenylmethanesulphonylfluoride, and 1 μg/ml leupeptin in T-PER). Homogenate (300–500 μg protein) was mixed with Preclearing Matrix F (30 min), and the supernatant was immunoprecipitated with 1.5–2 μg of anti-PAS, anti-AS160, or anti-TBC1D1 (4°C) using ExactaCruz F-HRP. After gentle rotation overnight, the immunoprecipitation mix was centrifuged (4,000g), and supernatant was aspirated. After washing (four times with 500 μl PBS), protein bound to beads was eluted with 2× Laemmli sample buffer, boiled, and loaded on a polyacrylamide gel.
Immunoblotting.
Immunoprecipitates or lysate, boiled with SDS loading buffer, were separated and electrophoretically transferred to nitrocellulose. Samples were rinsed with Tris-buffered saline plus Tween (TBST; 0.14 mol/l NaCl, 0.02 mol/l Tris base, pH 7.6, and 0.1% Tween 20), blocked with 5% nonfat dry milk in TBST (1 h, room temperature), washed 3 × 5 min (room temperature), and treated with primary antibodies (1:1,000 in TBST + 5% BSA) overnight (4°C). Blots were washed 3 × 5 min with TBST, incubated with the secondary antibody (goat anti-rabbit IgG HRP conjugate, 1:20,000 in TBST + 5% milk, 1 h at room temperature), washed again 3 × 5 min with TBST, and developed with West Dura extended duration substrate reagent. Protein bands were quantitated by densitometry (Alpha Innotech, San Leandro, CA). Mean values for basal muscles incubated without inhibitors on each blot were normalized to equal 1.0. All values were expressed relative to the normalized basal value.
Statistical analysis.
Statistical analyses used Sigma Stat version 2.0 (San Rafael, CA). Data are expressed as the mean ± SE, and P ≤ 0.05 was considered statistically significant. One-way ANOVA and the Student-Newman-Keuls post hoc test were used. When data failed the Levene Median test for equal variance, the Kruskal-Wallis nonparametric ANOVA on ranks was used with Dunn's post hoc test.
RESULTS
Tension development.
Neither Wortmannin nor compound C affected peak force or total force (data not shown).
Total protein abundance.
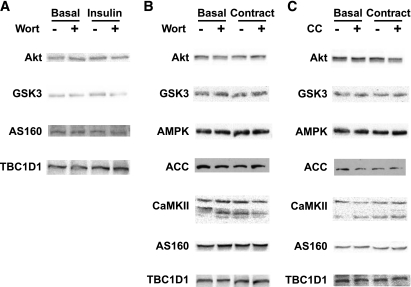
For all comparisons of immunoblot band intensities, equal amounts of total protein or of immunoprecipitate derived from equal amounts of total protein were loaded in each lane. Abundance of total proteins (Akt, GSK3, AMPK, ACC, CaMKII, AS160, and TBC1D1) was unaltered by insulin, contraction, Wortmannin, and/or compound C (Fig. 1).
FIG. 1.
Abundance of total proteins (Akt, GSK3, AMPK, ACC, CaMKII, AS160, and TBC1D1). There were no statistically significant differences among groups (n = 4 per group) for total protein abundance in muscles with or without insulin and/or Wortmannin (A), contraction and/or Wortmannin (B), and contraction and/or compound C (C). CC, compound C; Wort, Wortmannin.
AS160 and TBC1D1 phosphorylation.
As previously shown (19), the anti-PAS immunoblot of muscle samples (basal, insulin, or contraction) without prior immunoprecipitation contained multiple PAS bands, including the following: 1) an anti-PAS band migrating at a location above the 150 kDa molecular marker (PAS-160) that corresponded to the location of the anti-AS160 band from an AS160 immunoblot and 2) an anti-PAS band migrating at a location similar to the 150 kDa molecular marker (PAS-150) and corresponding with the location of the anti-TBC1D1 band from a TBC1D1 immunoblot (data not shown). When samples were immunoprecipitated with anti-PAS and immunoblotted with anti-AS160, the location of the band (PAS-AS160) corresponded to the location of the PAS-160 band. When samples were immunoprecipitated with anti-TBC1D1 and immunoblotted with anti-PAS, the location of the band (PAS-TBC1D1) corresponded to the location of the PAS-150 band. Throughout this report, when samples were directly immunoblotted with anti-PAS, the bands are referred to as PAS-160 or PAS-150, respectively, whereas when samples are immunoprecipitated before immunoblotting, the respective bands are referred to as PAS-AS160 or PAS-TBC1D1.
Wortmannin.
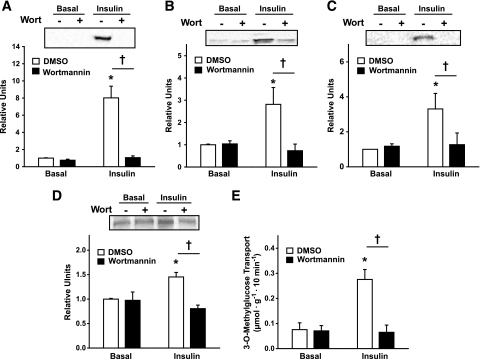
Incubation of skeletal muscle with Wortmannin for 30 min completely inhibited the insulin-stimulated increases in pAkt and pGSK3 (P < 0.001) (Fig. 2A and B). Insulin (with or without Wortmannin) did not alter pAMPK, pACC, or pCaMKII (data not shown). Insulin-stimulated increases in PAS-160 (Fig. 2C), PAS-150 (Fig. 2D), and glucose transport (Fig. 2E) were completely inhibited by Wortmannin (P < 0.001).
FIG. 2.
Effects of Wortmannin on insulin-stimulated phosphorylation of AktThr308 (A), GSK3Ser21/9 (B), PAS-160 (C), PAS-150 (D), and glucose transport (E). Paired isolated rat epitrochlearis muscles were incubated with or without 500 nmol/l of Wortmannin for 30 min. Muscles were then either incubated in identical media (basal) or in solution that contained 2,000 μU/ml of insulin for 20 min, freeze-clamped immediately, and used for immunoblotting or for 3-MG transport measurement. Data are the means ± SE, n = 5–9 per group. Post hoc analysis: *P < 0.05 (effect of insulin); †P < 0.05 (effect of Wortmannin). □, DMSO; ■, Wortmannin. Wort, Wortmannin.
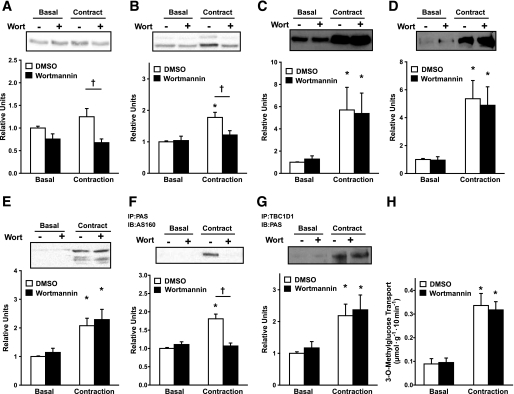
Contraction resulted in a significant increase in glucose transport, pGSK3, pAMPK, pACC, and pCaMKII (P < 0.05) (Figs. 3 and 4) as well as PAS-160 and PAS-150 (data not shown). PAS-AS160 and PAS-TBC1D1 were also significantly (P < 0.05) elevated after contraction compared with basal muscles (Fig. 3F and G). Consistent with previous results using this contraction protocol (19), there was a nonsignificant trend for a small contraction-stimulated increase in pAkt (Fig. 3A and 4A). There were no contraction effects on pAkt and pGSK3 in Wortmannin-treated muscles (Fig. 3A and B) (P < 0.05). Wortmannin did not affect contraction-stimulated pAMPK, pACC, or pCaMKII (Fig. 3C–E). Increases in PAS-AS160 (P < 0.01) (Fig. 3F) and PAS-160 (data not shown) in contraction-stimulated muscles were eliminated with Wortmannin treatment. In contrast, increases in PAS-TBC1D1 (Fig. 3G) and PAS-150 (data not shown) in contraction-stimulated muscles were not significantly affected by Wortmannin treatment. As expected, glucose transport in contraction-stimulated muscles was unaltered by Wortmannin (Fig. 3H).
FIG. 3.
Effects of Wortmannin on contraction-stimulated phosphorylation of AktThr308 (A), GSK3Ser21/9 (B), AMPKThr172 (C), ACCSer79 (D), CaMKIIThr286 (E), PAS-AS160 (F), PAS-TBC1D1 (G), and glucose transport (H). Paired isolated rat epitrochlearis muscles were incubated with or without 500 nmol/l of Wortmannin for 30 min. Muscles were then either rested (basal) or stimulated to contract for 20 min, freeze-clamped immediately for immunoprecipitation (IP) and/or immunoblotting (IB), or used for 3-MG transport measurement. Data are the means ± SE, n = 9–17 per group. Post hoc analysis: *P < 0.05 (effect of contraction); †P < 0.05 (effect of Wortmannin). □, DMSO; ■, Wortmannin. Wort, Wortmannin.
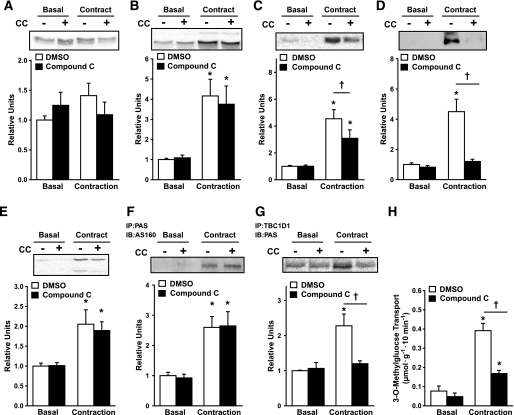
FIG. 4.
Effects of compound C on contraction-stimulated phosphorylation of AktThr308 (A), GSK3Ser21/9 (B), AMPKThr172 (C), ACCSer79 (D), CaMKIIThr286 (E), PAS-AS160 (F), PAS-TBC1D1 (G), and glucose transport (H). Paired isolated rat epitrochlearis muscles were incubated with or without 40 μmol/l of compound C for 60 min. Muscles were then either rested (basal) or stimulated to contract for 20 min, freeze-clamped immediately for immunoprecipitation (IP) and/or immunoblotting (IB), or used for 3-MG transport measurement. Data are the means ± SE, n = 6–14 per group. Post hoc analysis: *P < 0.05 (effect of contraction); †P < 0.05 (effect of compound C). □, DMSO; ■, compound C. CC, compound C.
Compound C.
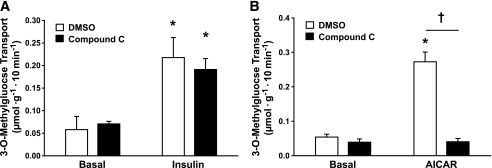
Compound C caused complete inhibition of the contraction-stimulated increase in pACC (P < 0.001) (Fig. 4D) without affecting pAkt, pGSK3, and pCaMKII (Fig. 4A, B, and E). Compound C did not significantly alter the increased PAS-AS160 (Fig. 4F) or PAS-160 (data not shown) in contraction-stimulated muscles. In contrast, compound C significantly reduced the increases in PAS-TBC1D1 (P < 0.05) (Fig. 4G) and PAS-150 (data not shown) in contraction-stimulated muscles. The increase in glucose transport in contraction-stimulated muscles was partially reduced by compound C (P < 0.001) (Fig. 4H). Insulin-stimulated glucose transport was unaffected by compound C (Fig. 5A), and the increase in glucose transport in AICAR-stimulated muscles was completely eliminated by compound C (P < 0.01) (Fig. 5B).
FIG. 5.
Effects of compound C on insulin-stimulated (A) and AICAR-stimulated (B) glucose transport. Paired isolated rat epitrochlearis muscles were incubated with or without 40 μmol/l of compound C for 60 min. Muscles were then either incubated in identical media (basal) or in solution that contained 2,000 μU/ml of insulin (A) for 20 min or in solution that contained 2 mmol/l of AICAR (B) for 40 min and used for 3-MG transport measurement. Data are the means ± SE, n = 6–14 per group. Post hoc analysis: *P < 0.05 (effect of insulin or AICAR); †P < 0.05 (effect of compound C). □, DMSO; ■, compound C.
DISCUSSION
This study provides new information about the regulation and function of AS160 and TBC1D1, two related RabGAP proteins expressed by skeletal muscle, each of which has been implicated to modulate glucose transport. The results demonstrate that it is possible to separate contraction's ability to increase AS160 phosphorylation from TBC1D1 phosphorylation, as identified using the PAS antibody, and reveal novel insights regarding their respective roles in the activation of glucose transport. The data suggest that in isolated rat epitrochlearis muscle: 1) PI 3-kinase–dependent (and presumably Akt-dependent) mechanisms are essential for the insulin-stimulated increases in glucose transport and phosphorylation of AS160 and TBC1D1, 2) PI 3-kinase/Akt–dependent (but not AMPK-dependent) mechanisms are essential for the contraction-stimulated increase in PAS-AS160 (but not PAS-TBC1D1 or glucose transport), and 3) AMPK-dependent (but not PI 3-kinase/Akt–dependent) mechanisms are essential for the contraction-stimulated increases in PAS-TBC1D1 (but not PAS-AS160) and glucose transport. The findings support the idea that elevated PAS-TBC1D1, via an AMPK-dependent mechanism, may participate in contraction-mediated glucose transport.
Regarding insulin stimulation, the data are consistent with earlier research in 3T3-L1 adipocytes (13,16,33), human primary myocytes (34), and rodent skeletal muscle (18,28), which indicated that the insulin stimulation of PAS-AS160 is Akt dependent. Our results confirm that insulin can induce increased PAS-TBC1D1 in skeletal muscle (24). Wortmannin has been shown to reduce PAS-TBC1D1 in insulin-stimulated HEK-293 cells (21), but the current data are apparently the first demonstration in an authentic insulin target tissue that Wortmannin-induced inhibition of Akt eliminates the insulin-stimulated increase in PAS-150, which corresponds to PAS-TBC1D1.
Contraction for 20 min caused an increase in phosphorylation of GSK3, an Akt substrate, despite only a trend for increased Akt phosphorylation. These results are consistent with previous observations indicating that contractile activity can transiently activate Akt, achieving peak activity and phosphorylation at ∼2–5 min with reversal at ∼15–20 min, despite continued stimulation (19,35). In rat epitrochlearis, contraction-stimulated PAS-AS160 was completely Wortmannin inhibitable, suggesting that contraction-stimulated AS160 Pas phosphorylation is PI 3-kinase/Akt–dependent, as previously reported (18). The current results confirm recent studies that found contraction causes an increase in skeletal muscle PAS-TBC1D1 (19,24). In striking contrast to AS160, Wortmannin did not attenuate the contraction-stimulated increase in PAS-TBC1D1, suggesting that contraction's effect on PAS-TBC1D1 was not PI 3-kinase/Akt–dependent. Furthermore, the AMPK inhibitor compound C completely suppressed contraction-stimulated PAS-TBC1D1 without inhibiting contraction's effect on PAS-AS160. Notably, Wortmannin did not alter phosphorylation of AMPK or ACC (an AMPK substrate), and compound C did not alter phosphorylation of Akt or GSK3 (an Akt substrate). These experiments reveal fundamental differences in mechanisms whereby contraction regulates phosphorylation of two closely related RabGAP proteins.
The data provide new evidence that increased PAS-TBC1D1 in skeletal muscle with contraction is AMPK dependent. Supporting this interpretation, incubating skeletal muscle with AICAR induced an increase in PAS-TBC1D1, and incubation of recombinant AMPK with immunoprecipitated TBC1D1 caused increased PAS-TBC1D1 (24). Earlier studies that found that muscle from mice with genetically disrupted AMPK had reduced contraction-stimulated phosphorylation at ∼160 kDa had not performed immunoprecipitation of samples before immunoblotting with the PAS antibody (28,29). Perhaps in these studies, the PAS immunoreactivity included both TBC1D1 and AS160, with TBC1D1 accounting for at least a portion of the apparently AMPK-dependent phosphorylation.
A secondary aim was to determine whether inhibition of insulin- or contraction-stimulated increases in PAS-AS160 or PAS-TBC1D1 were accompanied by attenuation of glucose transport. A great deal of evidence supports the idea that the insulin-stimulated increase in AS160 phosphorylation, via a PI 3-kinase/Akt–dependent mechanism, is important for increased GLUT4 translocation and glucose transport (13–18,33). The current data are consistent with this role of AS160. Few studies have evaluated TBC1D1's possible role in insulin-stimulated glucose transport. In 3T3-L1 adipocytes, knockdown of TBC1D1 did not alter basal or insulin-stimulated GLUT4 in surface membranes (23). However, these results are not necessarily predictive of skeletal muscle, which, compared with 3T3-L1 cells, expresses TBC1D1 at much greater levels (23). In L6 myotubes, knockdown of TBC1D1 resulted in elevated basal surface GLUT4 and a ∼1.5-fold elevation in insulin-stimulated GLUT4 translocation (25). The authors' interpretation was that TBC1D1 can modulate GLUT4 traffic, but insulin may not regulate TBC1D1's RabGAP activity. The current data demonstrate that insulin regulates TBC1D1 phosphorylation in skeletal muscle via a PI 3-kinase/Akt–dependent mechanism, but the functional consequences of TBC1D1 phosphorylation on glucose transport remain uncertain.
Because contraction-stimulated glucose transport was unaltered by Wortmannin, despite elimination of the increase in PAS-AS160, it is evident that increased PAS-AS160 is not essential for contraction-mediated glucose transport. The lack of a Wortmannin effect on contraction-stimulated increases in PAS-TBC1D1 and glucose transport, together with compound C inducing full inhibition of contraction's effect on PAS-TBC1D1 and partial inhibition of glucose transport, is consistent with the possibility that PAS-TBC1D1 participates in the contraction-stimulated increase in glucose transport. However, the current results do not establish causality, and although compound C did not alter tension development, pCaMKII, pAkt, pGSK3, or PAS-AS160, these results do not prove that compound C's effects are exclusively attributable to inhibiting AMPK.
Wortmannin can completely inhibit contraction's activation of Akt in skeletal muscle without reducing contraction-stimulated glucose transport (7,8,36). Another PI 3-kinase inhibitor, LY294002, also inhibits contraction-activated Akt (35). These results with two distinct PI 3-kinase inhibitors suggest that PI 3-kinase is upstream of contraction-stimulated Akt. However, muscle contraction does not increase class Ia PI 3-kinase activity associated with insulin receptor substrate proteins (10) or class II PI 3-kinase activity (37). Sakamoto et al. (35) proposed that contraction may activate class Ib PI 3-kinase, but this possibility remains to be experimentally confirmed. Nevertheless, Wortmannin can clearly eliminate contraction-stimulated increases in pAkt and PAS-AS160 in rat epitrochlearis muscle, which begs the question: How can activation of Akt and PAS-AS160 be important for insulin-stimulated glucose transport, but not contraction-stimulated glucose transport? A similar paradox is that either insulin or contraction can individually lead to increased glucose transport in skeletal muscle by increasing GLUT4 translocation, but the combined stimulation of muscle with maximally effective insulin and contraction can increase glucose transport (38,39) and cell-surface GLUT4 (39) more than either stimulus alone. There is evidence suggesting that insulin and contraction recruit different intracellular pools of GLUT4 vesicles (1,2). Little is known about subcellular localization of AS160 or TBC1D1, but it has been reported that in 3T3-L1 adipocytes, AS160 appears to be associated with GLUT4 vesicles under basal conditions, and insulin treatment can cause an increase in cytosolic AS160 (40). A speculative scenario is that insulin-recruitable GLUT4 vesicles may associate with AS160, whereas contraction-associated GLUT4 vesicles may associate with TBC1D1. In addition, AS160 and TBC1D1 function are likely also regulated by other mechanisms, including 1) phosphorylation on sites undetectable with anti-PAS, 2) Ca2+-calmodulin interaction with each protein's calmodulin binding domain, 3) binding to 14-3-3 proteins, and 4) changes in subcellular localization (21,26,27,40–43). Evaluation of these and alternative mechanisms will be necessary to fully understand the regulation and roles of AS160 and TBC1D1.
We also determined whether acute inhibition of the contraction-stimulated activation of AMPK would result in attenuated glucose transport. AMPK was originally recognized as a potential participant in contraction-stimulated glucose transport by Winder and colleagues (44–46). They found that exercise or contraction can activate AMPK (44,45), and AICAR, which also leads to AMPK activation, can stimulate glucose uptake (46). Many studies have supported a role for AMPK in contraction-stimulated glucose transport (4,11,12,47), but research using mice with genetic modification of AMPK suggests that AMPK may not be essential for contraction-stimulated glucose transport (48,49). With genetic modifications, there may be compensatory responses. Compound C, which offers a useful alternative approach for rapid inhibition of AMPK, resulted in reduced contraction-stimulated glucose transport, providing novel evidence that AMPK may be important for this contraction effect.
The partial reduction in contraction-stimulated glucose transport by compound C supports earlier studies that indicated that AMPK-independent mechanisms can account for a portion of the contraction-stimulated glucose transport (11,12). Multiple lines of evidence suggest that increased cytosolic calcium contributes to contraction-stimulated glucose transport (12,41). For example, calmodulin binding to AS160 has been implicated in contraction-stimulated glucose transport (41). TBC1D1 also contains a calmodulin binding domain (21). Unaltered contraction-stimulated increases in pCaMKII and tension in compound C–treated muscles suggest that cytosolic Ca2+ was not reduced, which may account, at least in part, for the residual effect of contraction on glucose transport. AICAR can activate AMPK without altering cytosolic Ca2+ concentration in isolated rat epitrochlearis (50). In this context, it is notable that, in contrast to the partial inhibition of contraction-stimulated glucose transport, compound C completely inhibited AICAR-stimulated glucose transport. Furthermore, compound C had no effect on insulin-stimulated glucose transport, indicating that compound C's ability to reduce glucose transport activated by contraction or AICAR is not because of a nonspecific effect on glucose transport, regardless of the stimulation pathway.
The contraction-stimulated increases in PAS-TBC1D1 and glucose transport with 20 min of contractile activity in the current study are similar to earlier results using the same contraction protocol (19). The previous study, which included assessment for up to 60 min of contraction, found that the glucose transport rate achieved with 20 min of contraction was sustained with contraction lasting 60 min, even though contraction-stimulated PAS-TBC1D1 had returned to basal levels at 60 min (19). These results suggest PAS-TBC1D1 may trigger the initial increase in contraction-stimulated glucose transport. It remains unclear whether the initial increase in PAS-TBC1D1 is sufficient to cause a sustained increase in contraction-stimulated glucose transport or whether another mechanism is required for a sustained increase.
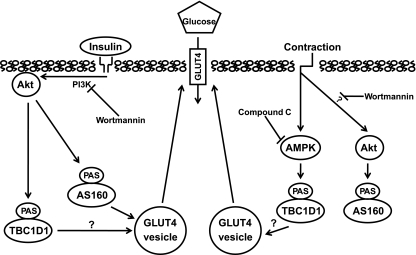
In conclusion, Fig. 6 represents our Working model for increasing PAS-AS160 and PAS-TBC1D1 with insulin or contraction, and for the roles that insulin- or contraction-stimulated PAS-AS160 and PAS-TBC1D1 may play in the regulation of glucose transport. We found that: 1) insulin stimulates Pas phosphorylation of AS160 and TBC1D1 in an Akt-dependent manner, and PAS-AS160 appears to be important for the regulation of insulin-stimulated glucose transport with the functional role of insulin-stimulated PAS-TBC1D1 currently uncertain; 2) contraction stimulates PAS-phosphorylation of AS160, but not TBC1D1, in an Akt-dependent manner, and the contraction-stimulated PAS-AS160 does not contribute to contraction-stimulated glucose transport; and 3) contraction stimulates Pas phosphorylation of TBC1D1 in an AMPK-dependent manner, consistent with the idea that contraction-stimulated PAS-TBC1D1 may regulate contraction-stimulated glucose transport. Additional research with specific manipulation of TBC1D1 expression and/or activation will be needed to further elucidate TBC1D1's role in glucose transport of skeletal muscle.
FIG. 6.
Working model for the roles of PAS-AS160 and PAS-TBC1D1 in insulin- and contraction-stimulated glucose transport. For clarity, the figure focuses on PAS-AS160 and PAS-TBC1D1 and does not depict other possible mechanisms that may influence glucose transport (e.g., calcium-mediated processes with contraction, binding of AS160 or TBC1D1 to 14-3-3 proteins, and/or phosphorylation on sites not recognized by anti-PAS with insulin or contraction). Insulin, by a PI 3-kinase (PI3K)-dependent mechanism, activates Akt, which phosphorylates AS160 (TBC1D4) and TBC1D1 on sites identified using the PAS antibody. The PI 3-kinase inhibitor Wortmannin completely eliminates insulin-stimulated glucose transport and PAS-phosphorylation of AS160 and TBC1D1. Increased PAS-AS160 is required for insulin's full effect on GLUT4 translocation and glucose transport. TBC1D1's role in insulin-stimulated glucose transport is uncertain. Contraction leads to increased phosphorylation of AMPK and Akt; although the ability of Wortmannin to inhibit Akt activation by contraction suggests at PI 3-kinase–dependent process, the precise mechanism is unknown. AMPK inhibition (by compound C) completely eliminates the increased PAS-TBC1D1 without altering PAS-AS160, and Wortmannin completely eliminates the increased PAS-AS160 without altering PAS-TBC1D1. Compound C partially inhibits contraction-stimulated glucose transport, consistent with AMPK-related mechanisms accounting for a portion of contraction-mediated glucose transport. The concomitant AMPK-dependent inhibition of PAS-TBC1D1 suggests it may play a role in contraction-stimulated glucose transport.
ACKNOWLEDGMENTS
This research was supported by National Institutes of Health Grants AG-010026 and DK-071771 (to G.D.C.).
No potential conflicts of interest relevant to this article were reported.
This work was accepted at the 68th Scientific Session of the American Diabetes Association, San Francisco, California, 6–10 June 2008.
We thank James G. MacKrell and David R. Blair for assistance in muscle tension measurements.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Douen AG, Ramlal T, Rastogi S, Bilan PJ, Cartee GD, Vranic M, Holloszy JO, Klip A: Exercise induces recruitment of the “insulin-responsive glucose transporter”: evidence for distinct intracellular insulin- and exercise-recruitable transporter pools in skeletal muscle. J Biol Chem 1990; 265: 13427– 13430 [PubMed] [Google Scholar]
- 2.Coderre L, Kandror KV, Vallega G, Pilch PF: Identification and characterization of an exercise-sensitive pool of glucose transporters in skeletal muscle. J Biol Chem 1995; 270: 27584– 27588 [DOI] [PubMed] [Google Scholar]
- 3.Cartee GD, Wojtaszewski JF: Role of Akt substrate of 160 kDa in insulin-stimulated and contraction-stimulated glucose transport. Appl Physiol Nutr Metab 2007; 32: 557– 566 [DOI] [PubMed] [Google Scholar]
- 4.Hayashi T, Hirshman MF, Kurth EJ, Winder WW, Goodyear LJ: Evidence for 5′ AMP-activated protein kinase mediation of the effect of muscle contraction on glucose transport. Diabetes 1998; 47: 1369– 1373 [DOI] [PubMed] [Google Scholar]
- 5.Cho H, Mu J, Kim JK, Thorvaldsen JL, Chu Q, Crenshaw EB, 3rd, Kaestner KH, Bartolomei MS, Shulman GI, Birnbaum MJ: Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB beta). Science 2001; 292: 1728– 1731 [DOI] [PubMed] [Google Scholar]
- 6.McCurdy CE, Cartee GD: Akt2 is essential for the full effect of calorie restriction on insulin-stimulated glucose uptake in skeletal muscle. Diabetes 2005; 54: 1349– 1356 [DOI] [PubMed] [Google Scholar]
- 7.Yeh JI, Gulve EA, Rameh L, Birnbaum MJ: The effects of Wortmannin on rat skeletal muscle: dissociation of signaling pathways for insulin- and contraction-activated hexose transport. J Biol Chem 1995; 270: 2107– 2111 [DOI] [PubMed] [Google Scholar]
- 8.Lee AD, Hansen PA, Holloszy JO: Wortmannin inhibits insulin-stimulated but not contraction-stimulated glucose transport activity in skeletal muscle. FEBS Lett 1995; 361: 51– 54 [DOI] [PubMed] [Google Scholar]
- 9.Sakamoto K, Arnolds DE, Fujii N, Kramer HF, Hirshman MF, Goodyear LJ: Role of Akt2 in contraction-stimulated cell signaling and glucose uptake in skeletal muscle. Am J Physiol Endocrinol Metab 2006; 291: E1031– E1037 [DOI] [PubMed] [Google Scholar]
- 10.Goodyear LJ, Giorgino F, Balon TW, Condorelli G, Smith RJ: Effects of contractile activity on tyrosine phosphoproteins and PI 3-kinase activity in rat skeletal muscle. Am J Physiol 1995; 268: E987– E995 [DOI] [PubMed] [Google Scholar]
- 11.Mu J, Brozinick JT, Jr, Valladares O, Bucan M, Birnbaum MJ: A role for AMP-activated protein kinase in contraction- and hypoxia-regulated glucose transport in skeletal muscle. Mol Cell 2001; 7: 1085– 1094 [DOI] [PubMed] [Google Scholar]
- 12.Wright DC, Hucker KA, Holloszy JO, Han DH: Ca(2+) and AMPK both mediate stimulation of glucose transport by muscle contractions. Diabetes 2004; 53: 330– 335 [DOI] [PubMed] [Google Scholar]
- 13.Kane S, Sano H, Liu SC, Asara JM, Lane WS, Garner CC, Lienhard GE: A method to identify serine kinase substrates: Akt phosphorylates a novel adipocyte protein with a Rab GTPase-activating protein (GAP) domain. J Biol Chem 2002; 277: 22115– 22118 [DOI] [PubMed] [Google Scholar]
- 14.Sano H, Kane S, Sano E, Miinea CP, Asara JM, Lane WS, Garner CW, Lienhard GE: Insulin-stimulated phosphorylation of a Rab GTPase-activating protein regulates GLUT4 translocation. J Biol Chem 2003; 278: 14599– 14602 [DOI] [PubMed] [Google Scholar]
- 15.Miinea CP, Sano H, Kane S, Sano E, Fukuda M, Peranen J, Lane WS, Lienhard GE: AS160, the Akt substrate regulating GLUT4 translocation, has a functional Rab GTPase-activating protein domain. Biochem J 2005; 391: 87– 93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeigerer A, McBrayer MK, McGraw TE: Insulin stimulation of GLUT4 exocytosis, but not its inhibition of endocytosis, is dependent on RabGAP AS160. Mol Biol Cell 2004; 15: 4406– 4415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eguez L, Lee A, Chavez JA, Miinea CP, Kane S, Lienhard GE, McGraw TE: Full intracellular retention of GLUT4 requires AS160 Rab GTPase activating protein. Cell Metab 2005; 2: 263– 272 [DOI] [PubMed] [Google Scholar]
- 18.Bruss MD, Arias EB, Lienhard GE, Cartee GD: Increased phosphorylation of Akt substrate of 160 kDa (AS160) in rat skeletal muscle in response to insulin or contractile activity. Diabetes 2005; 54: 41– 50 [DOI] [PubMed] [Google Scholar]
- 19.Funai K, Cartee GD: Contraction-stimulated glucose transport in rat skeletal muscle is sustained despite reversal of increased Pas phosphorylation of AS160 and TBC1D1. J Appl Physiol 2008; 105: 1788– 1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kramer HF, Witczak CA, Taylor EB, Fujii N, Hirshman MF, Goodyear LJ: AS160 regulates insulin- and contraction-stimulated glucose uptake in mouse skeletal muscle. J Biol Chem 2006; 281: 31478– 31485 [DOI] [PubMed] [Google Scholar]
- 21.Roach WG, Chavez JA, Miinea CP, Lienhard GE: Substrate specificity and effect on GLUT4 translocation of the Rab GTPase-activating protein Tbc1d1. Biochem J 2007; 403: 353– 358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blot V, McGraw TE: Molecular mechanisms controlling GLUT4 intracellular retention. Mol Biol Cell 2008; 19: 3477– 3487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chavez JA, Roach WG, Keller SR, Lane WS, Lienhard GE: Inhibition of GLUT4 translocation by Tbc1d1, a Rab GTPase-activating protein abundant in skeletal muscle, is partially relieved by AMP-activated protein kinase activation. J Biol Chem 2008; 283: 9187– 9195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor EB, An D, Kramer HF, Yu H, Fujii NL, Roeckl KS, Bowles N, Hirshman MF, Xie J, Feener EP, Goodyear LJ: Discovery of TBC1D1 as an insulin-, AICAR-, and contraction-stimulated signaling nexus in mouse skeletal muscle. J Biol Chem 2008; 283: 9787– 9796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ishikura S, Klip A: Muscle cells engage Rab8A and myosin Vb in insulin-dependent GLUT4 translocation. Am J Physiol Cell Physiol 2008; 295: C1016– C1025 [DOI] [PubMed] [Google Scholar]
- 26.Geraghty KM, Chen S, Harthill JE, Ibrahim AF, Toth R, Morrice NA, Vandermoere F, Moorhead GB, Hardie DG, MacKintosh C: Regulation of multisite phosphorylation and 14-3-3 binding of AS160 in response to IGF-1, EGF, PMA and AICAR. Biochem J 2007; 407: 231– 241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen S, Murphy J, Toth R, Campbell DG, Morrice NA, Mackintosh C: Complementary regulation of TBC1D1 and AS160 by growth factors, insulin and AMPK activators. Biochem J 2008; 409: 449– 459 [DOI] [PubMed] [Google Scholar]
- 28.Kramer HF, Witczak CA, Fujii N, Jessen N, Taylor EB, Arnolds DE, Sakamoto K, Hirshman MF, Goodyear LJ: Distinct signals regulate AS160 phosphorylation in response to insulin, AICAR, and contraction in mouse skeletal muscle. Diabetes 2006; 55: 2067– 2076 [DOI] [PubMed] [Google Scholar]
- 29.Treebak JT, Glund S, Deshmukh A, Klein DK, Long YC, Jensen TE, Jorgensen SB, Viollet B, Andersson L, Neumann D, Wallimann T, Richter EA, Chibalin AV, Zierath JR, Wojtaszewski JF: AMPK-mediated AS160 phosphorylation in skeletal muscle is dependent on AMPK catalytic and regulatory subunits. Diabetes 2006; 55: 2051– 2058 [DOI] [PubMed] [Google Scholar]
- 30.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE: Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 2001; 108: 1167– 1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dumke CL, Kim J, Arias EB, Cartee GD: Role of kallikrein-kininogen system in insulin-stimulated glucose transport after muscle contractions. J Appl Physiol 2002; 92: 657– 664 [DOI] [PubMed] [Google Scholar]
- 32.Cartee GD, Bohn EE: Growth hormone reduces glucose transport but not GLUT-1 or GLUT-4 in adult and old rats. Am J Physiol 1995; 268: E902– E909 [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez E, McGraw TE: Insulin signaling diverges into Akt-dependent and -independent signals to regulate the recruitment/docking and the fusion of GLUT4 vesicles to the plasma membrane. Mol Biol Cell 2006; 17: 4484– 4493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouzakri K, Zachrisson A, Al-Khalili L, Zhang BB, Koistinen HA, Krook A, Zierath JR: siRNA-based gene silencing reveals specialized roles of IRS-1/Akt2 and IRS-2/Akt1 in glucose and lipid metabolism in human skeletal muscle. Cell Metab 2006; 4: 89– 96 [DOI] [PubMed] [Google Scholar]
- 35.Sakamoto K, Hirshman MF, Aschenbach WG, Goodyear LJ: Contraction regulation of Akt in rat skeletal muscle. J Biol Chem 2002; 277: 11910– 11917 [DOI] [PubMed] [Google Scholar]
- 36.Nolte LA, Han DH, Hansen PA, Hucker KA, Holloszy JO: A peroxovanadium compound stimulates muscle glucose transport as powerfully as insulin and contractions combined. Diabetes 2003; 52: 1918– 1925 [DOI] [PubMed] [Google Scholar]
- 37.Soos MA, Jensen J, Brown RA, O'Rahilly S, Shepherd PR, Whitehead JP: Class II phosphoinositide 3-kinase is activated by insulin but not by contraction in skeletal muscle. Arch Biochem Biophys 2001; 396: 244– 248 [DOI] [PubMed] [Google Scholar]
- 38.Constable SH, Favier RJ, Cartee GD, Young DA, Holloszy JO: Muscle glucose transport: interactions of in vitro contractions, insulin, and exercise. J Appl Physiol 1988; 64: 2329– 2332 [DOI] [PubMed] [Google Scholar]
- 39.Gao J, Ren J, Gulve EA, Holloszy JO: Additive effect of contractions and insulin on GLUT-4 translocation into the sarcolemma. J Appl Physiol 1994; 77: 1597– 1601 [DOI] [PubMed] [Google Scholar]
- 40.Larance M, Ramm G, Stockli J, van Dam EM, Winata S, Wasinger V, Simpson F, Graham M, Junutula JR, Guilhaus M, James DE: Characterization of the role of the Rab GTPase-activating protein AS160 in insulin-regulated GLUT4 trafficking. J Biol Chem 2005; 280: 37803– 37813 [DOI] [PubMed] [Google Scholar]
- 41.Kramer HF, Taylor EB, Witczak CA, Fujii N, Hirshman MF, Goodyear LJ: Calmodulin-binding domain of AS160 regulates contraction- but not insulin-stimulated glucose uptake in skeletal muscle. Diabetes 2007; 56: 2854– 2862 [DOI] [PubMed] [Google Scholar]
- 42.Kane S, Lienhard GE: Calmodulin binds to the Rab GTPase activating protein required for insulin-stimulated GLUT4 translocation. Biochem Biophys Res Commun 2005; 335: 175– 180 [DOI] [PubMed] [Google Scholar]
- 43.Ramm G, Larance M, Guilhaus M, James DE: A role for 14-3-3 in insulin-stimulated GLUT4 translocation through its interaction with the RabGAP AS160. J Biol Chem 2006; 281: 29174– 29180 [DOI] [PubMed] [Google Scholar]
- 44.Winder WW, Hardie DG: Inactivation of acetyl-CoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol 1996; 270: E299– E304 [DOI] [PubMed] [Google Scholar]
- 45.Hutber CA, Hardie DG, Winder WW: Electrical stimulation inactivates muscle acetyl-CoA carboxylase and increases AMP-activated protein kinase. Am J Physiol 1997; 272: E262– E266 [DOI] [PubMed] [Google Scholar]
- 46.Merrill GF, Kurth EJ, Hardie DG, Winder WW: AICA riboside increases AMP-activated protein kinase, fatty acid oxidation, and glucose uptake in rat muscle. Am J Physiol 1997; 273: E1107– E1112 [DOI] [PubMed] [Google Scholar]
- 47.Sakamoto K, McCarthy A, Smith D, Green KA, Grahame Hardie D, Ashworth A, Messi DR: Deficiency of LKB1 in skeletal muscle prevents Ampk activation and glucose uptake during contraction. EMBO J 2005; 24: 1810– 1820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jorgensen SB, Viollet B, Andreelli F, Frosig C, Birk JB, Schjerling P, Vaulont S, Richter EA, Wojtaszewski JF: Knockout of the alpha2 but not alpha1 5′-AMP-activated protein kinase isoform abolishes 5-aminoimidazole-4-carboxamide-1-beta-4-ribofuranosidebut not contraction-induced glucose uptake in skeletal muscle. J Biol Chem 2004; 279: 1070– 1079 [DOI] [PubMed] [Google Scholar]
- 49.Fujii N, Hirshman MF, Kane EM, Ho RC, Peter LE, Seifert MM, Goodyear LJ: AMP-activated protein kinase alpha2 activity is not essential for contraction- and hyperosmolarity-induced glucose transport in skeletal muscle. J Biol Chem 2005; 280: 39033– 39041 [DOI] [PubMed] [Google Scholar]
- 50.Terada S, Muraoka I, Tabata I: Changes in [Ca2+]i induced by several glucose transport-enhancing stimuli in rat epitrochlearis muscle. J Appl Physiol 2003; 94: 1813– 1820 [DOI] [PubMed] [Google Scholar]