Abstract
OBJECTIVE
To study which perinatal factors affect the risk of childhood overweight in offspring with a first-degree relative (FDR) with type 1 diabetes and to determine whether maternal diabetes is an independent contributor to overweight risk.
RESEARCH DESIGN AND METHODS
Data on a child's weight and height were collected at age 2, 5, and 8 years from 1,214 children participating in the prospective BABYDIAB study. All children had an FDR with type 1 diabetes, including 783 whose mothers had type 1 diabetes. Overweight was defined as BMI percentile ≥90. Data on birth size, breast-feeding, maternal age, and smoking during pregnancy were collected by questionnaires. Risk estimates were calculated by logistic regression analyses.
RESULTS
Breastfeeding duration and birth size both contributed significantly to overweight risk at all age intervals. Full breast-feeding >4 months or any breast-feeding >6 months reduced risk of overweight (aged 8 years: odds ratio 0.3 [95% CI 0.2–0.7], P = 0.004; and 0.3 [0.1–0.6], P = 0.001). Large-for-gestational-age status increased risk of overweight (aged 8 years: 2.4 [1.4–4.3], P = 0.002). Importantly, no evidence was found for an independent contribution of maternal type 1 diabetes to childhood overweight.
CONCLUSIONS
Our findings indicate that maternal type 1 diabetes is not an independent risk factor for overweight during childhood in offspring of type 1 diabetic mothers but that factors associated with maternal type 1 diabetes, such as short breast-feeding duration and high birth size, predispose children to overweight during childhood.
The increasing prevalence of overweight and obesity in children is a major health problem, as obesity-related medical conditions affect almost every organ system in the body (1). Gestational and perinatal factors have been shown to influence weight in childhood. Among these, maternal diabetes during pregnancy has been associated with an increased prevalence of childhood obesity (2–6). This has led to the hypothesis that in utero exposure to increased concentrations of glucose and insulin leads to increased risk of obesity and insulin resistance later in life (2). Previous studies (3–5) have been small or retrospective in design. Moreover, it is not clear whether maternal diabetes as such, or factors such as birth size and breast-feeding, which are affected by maternal diabetes, modify obesity risk.
Here, we have examined weight and BMI during childhood in a cohort of 1,214 children whose mothers or fathers have type 1 diabetes and who were followed from age ≤3 months. The aim of the analysis was to determine which gestational and perinatal factors may increase the risk of childhood obesity and whether maternal diabetes is an independent contributor to obesity risk.
RESEARCH DESIGN AND METHODS
Risk of overweight was assessed in 1,214 children who were enrolled in the prospective BABYDIAB study (7) between 1989 and 2000. All children had a mother and/or father with type 1 diabetes, including 783 children whose mothers had type 1 diabetes. All children were recruited throughout Germany, were entered into the studies before age 3 months, and were followed for >2 years. In families with more than one offspring participating in the study, the oldest one was included in the analyses. Twins and children who developed type 1 diabetes during follow-up were excluded from analyses.
Data on a child's weight and height at ages 2, 5, and 8 years were recorded by physicians in that child's pediatric record at regular clinical visits. From these data the BMI was calculated and expressed as percentiles adjusted for age and sex according to the German reference system established by Kromeyer-Hauschild et al. (8). Overweight was defined as BMI percentile ≥90. Data on children's weight and height were available for 1,155 children at 2 (age range 1.5–2.5), 1,031 children at 5 (4.5–5.5), and 665 children at 8 (7.5–8.5) years of age.
Birth weight and gestational age were collected from each child's pediatric record at birth. Pediatric records were completed by trained staff at delivery. Gestational age was determined on the basis of the last menstrual period and expressed in weeks. Birth weight was adjusted for sex and gestational age and expressed as a percentile of the reference German population as determined by the German Perinatal Registry (9). Offspring below the 10th percentile were defined as small for gestational age (SGA) and those ≥90th percentile as large for gestational age (LGA). Appropriate for gestational age (AGA) was defined as >10th and <90th percentile and served as the reference category in our analyses.
Data on breast-feeding (yes/no) and the duration of full and any breast-feeding (weeks) were obtained from questionnaires completed by the child's mother when the child was aged 9 months and aged 2 years. Breast-feeding was defined according to World Health Organization criteria (10) as “full breast-feeding” if the infant received breast milk with or without supplements of water, water-based drinks, vitamins, and medicines but without formula or other milk or solids. It was defined as “any breast-feeding” if the infant received breast milk, irrespective of any other types of food including full breast-feeding. To analyze the effect of breast-feeding on overweight, children who were never breast-fed were used as a reference category. Categories of full-breast-feeding duration were defined according to the national recommendations at the time of the children's enrollment (at least 4 months). Categories of any breast-feeding were defined as <1, 1.1–3.0, 3.1–6.0, and ≥6 months. Additional data used in the current analysis were obtained at birth either from the child's pediatric record (sex of the child) or from a questionnaire (parental type 1 diabetes status, smoking during pregnancy [defined as ≥1 cigarette/day], yes versus no). Written informed consent was obtained from the parents. The study was approved by the ethics committee of Bavaria (Bayerische Landesärztekammer [Bavarian Medical Council] no. 95357).
Statistical analyses
Continuous variables are given as means ± SD or median (interquartile range [IQR]). To test the effect of the factors under investigation on overweight, univariate logistic regression analyses were performed, giving the unadjusted odds ratio (OR) and 95% CI for overweight for each of the covariates. Variables that were significantly associated with overweight in offspring in the univariate analyses (P < 0.05) were included in a multivariate analysis by a multiple logistic regression model. The results of the logistic regression analyses are expressed as ORs (95% CI). The influence of breast-feeding duration and birth size on the prevalence of overweight was analyzed by a χ2 test. For all analyses, a two-tailed P value of 0.05 was considered significant. All statistical analyses were performed using the Statistical Package for Social Science (version 15.0; SPSS, Chicago, IL).
RESULTS
Factors affecting overweight in childhood: univariate analysis
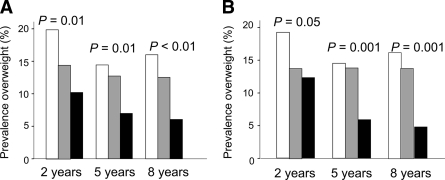
We examined whether factors such as maternal diabetes, breast-feeding duration, birth size, maternal age, sex, or maternal smoking during pregnancy increased the risk of childhood obesity at 2, 5, and 8 years of age. Details of the study cohort are shown in Table 1. In the univariate analysis, maternal diabetes was significantly associated with increased risk of overweight in offspring at 2 and 5 years of age. Full breast-feeding for >4 months or any breast-feeding for >6 months protected against the development of overweight (Table 2) (Fig. 1).
Table 1.
Characteristics of the cohort
| Variables used for analysis | n | |
|---|---|---|
| Female:male | 1,214 | 578:636 |
| Maternal diabetes (%) | 1,214 | 64.5 |
| Breast-feeding | ||
| Any breast-feeding (%) | 1,125 | 79.4 |
| Breast-feeding duration (weeks) (median [IQR]) | ||
| Full | 9 (0–21) | |
| Any | 16 (3–32) | |
| Birth size | ||
| SGA (%) | 1,137 | 10.2 |
| AGA (%) | 1,137 | 71.6 |
| LGA (%) | 1,137 | 18.2 |
| Maternal age at birth (years, median [IQR]) | 1,203 | 29.8 (27.2–32.3) |
| Maternal smoking during pregnancy (%) | 1,210 | 12.1 |
Table 2.
Risk of overweight in children at 2, 5, and 8 years of age: univariate analysis
| 2 years of age |
5 years of age |
8 years of age |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | OR (95% CI) | P | n | OR (95% CI) | P | n | OR (95% CI) | P | |
| Maternal diabetes | |||||||||
| No diabetes | 414 | 1.0 | 375 | 1.0 | 1.0 | ||||
| Type 1 diabetes | 741 | 1.5 (1.02–2.1) | 0.04 | 670 | 1.9 (1.2–3.1) | 0.004 | 1.1 (0.7–1.9) | 0.6 | |
| Breast-feeding | |||||||||
| Never breast-fed | 213 | 1.0 | 192 | 1.0 | 112 | 1.0 | |||
| Full breast-fed ≤4 months | 480 | 0.7 (0.5–1.08) | 0.1 | 434 | 0.9 (0.5–1.4) | 0.6 | 294 | 0.8 (0.4–1.4) | 0.4 |
| Full breast-fed >4 months | 382 | 0.5 (0.3–0.8) | 0.004 | 338 | 0.4 (0.3–0.8) | 0.006 | 230 | 0.3 (0.2–0.7) | 0.004 |
| Any breast-feeding | |||||||||
| ≤1 month | 54 | 1.0 (0.5–2.2) | 0.9 | 52 | 1.8 (0.8–3.8) | 0.1 | 32 | 0.7 (0.2–2.4) | 0.6 |
| 1.1–3.0 months | 167 | 0.7 (0.4–1.1) | 0.1 | 146 | 0.6 (0.3–1.2) | 0.2 | 101 | 0.5 (0.2–1.2) | 0.1 |
| 3.1–6.0 months | 245 | 0.6 (0.4–0.9) | 0.02 | 221 | 1.0 (0.6–1.7) | 1.0 | 152 | 1.1 (0.6–2.1) | 0.8 |
| >6 months | 377 | 0.6 (0.4–0.9) | 0.02 | 335 | 0.4 (0.2–0.7) | 0.001 | 230 | 0.3 (0.1–0.6) | 0.001 |
| Birth size | |||||||||
| AGA | 780 | 1.0 | 691 | 1.0 | 445 | 1.0 | |||
| SGA | 111 | 0.5 (0.2–1.05) | 0.07 | 96 | 0.6 (0.2–1.6) | 0.3 | 73 | 0.8 (0.3–2.0) | 0.7 |
| LGA | 198 | 2.3 (1.5–3.3) | <0.0001 | 178 | 4.0 (2.5–6.2) | <0.0001 | 107 | 2.4 (1.4–4.3) | 0.002 |
| Maternal age | |||||||||
| ≤30.1 years | 604 | 1.0 | 540 | 1.0 | 340 | 1.0 | |||
| >30.1 years | 543 | 1.2 (0.9–1.7) | 0.3 | 482 | 0.7 (0.4–0.99) | 0.04 | 323 | 0.9 (0.5–1.4) | 0.5 |
| Sex | |||||||||
| Male | 606 | 1.0 | 543 | 1.0 | 347 | 1.0 | |||
| Female | 549 | 0.7 (0.5–1.01) | 0.05 | 488 | 1.0 (0.7–1.5) | 0.9 | 318 | 0.7 (0.4–1.2) | 0.2 |
| Smoking during pregnancy | |||||||||
| No | 1019 | 1.0 | 909 | 1.0 | 581 | 1.0 | |||
| One or more cigarettes per day | 134 | 1.4 (0.9–2.2) | 0.2 | 122 | 1.6 (0.9–2.7) | 0.1 | 81 | 1.5 (0.8–2.9) | 0.2 |
| HLA DR4 genotype | |||||||||
| No | 564 | 1.0 | 509 | 1.0 | 1.0 | ||||
| Yes | 531 | 0.9 (0.6–1.2) | 0.4 | 481 | 1.2 (0.8–1.8) | 0.4 | 0.6 (0.5–1.4) | 0.6 | |
Figure 1.
Prevalence of overweight at 2, 5, and 8 years of age in children with a first-degree relative with type 1 diabetes, depicted in relation to full (A) and any (B) breast-feeding duration. □, children who were not breast-fed;  , children with short breast-feeding duration (≤4 months full breast-feeding and ≤6 months full breast-feeding); ■, children with long breast-feeding duration (>4 months full and >6 months any breast-feeding).
, children with short breast-feeding duration (≤4 months full breast-feeding and ≤6 months full breast-feeding); ■, children with long breast-feeding duration (>4 months full and >6 months any breast-feeding).
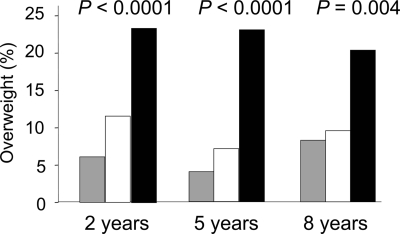
LGA status in the newborn was associated with an increased risk of overweight at all ages (OR 2.3 [95% CI 1.5–3.3], P < 0.0001; 4.0 [2.5–6.2], P < 0.0001; and 2.4 [1.4–4.3], P = 0.002 for ages 2, 5, and 8 years, respectively) (Table 2) (Fig. 2). We further observed that LGA was also an important factor for becoming overweight during infancy. Among children who moved from normal weight at age 2 years to overweight at age 5 years, 38.2% were born LGA and 1.8% were born SGA. In contrast, 14.5% and 11.1% of the children who remained normal weight between 2 and 5 years of age were LGA and SGA, respectively (P < 0.0001). A higher maternal age (>30.1 years) was slightly associated with lower risk of overweight in offspring at 5 years of age (0.7 [0.4–0.99], P = 0.04) but did not affect risk at 2 and 8 years of age. Sex of the child, maternal smoking during pregnancy, and HLA-DR4 genotype in the child did not influence risk of overweight at any age.
Figure 2.
Prevalence of overweight at 2, 5, and 8 years of age in children with a first-degree relative with type 1 diabetes, depicted in relation to birth size.  , children born SGA; □, children born AGA; ■, children born LGA.
, children born SGA; □, children born AGA; ■, children born LGA.
Factors affecting overweight in childhood: multivariate analysis
Maternal diabetes, breast-feeding duration, birth size, and maternal age were included as variables in a multivariate analysis of the whole cohort using a multiple logistic regression model (Table 3). Neither maternal diabetes nor maternal age affected risk of overweight in the multivariate model. However, breast-feeding duration and birth size both contributed significantly to overweight risk at all age intervals (Table 3). OR at 2 years of age was 0.6 (95% CI 0.3–0.9) (P = 0.02), and that at 8 years of age was 0.3 (0.1–0.6) (P = 0.002) for full breast-feeding duration of ≥4 months. Finally, an effect of breast-feeding duration and birth size on overweight risk could be observed when analyzing offspring of mothers with type 1 diabetes separately (online appendix Table A1 [available at http://care.diabetesjournals.org/cgi/content/full/dc08–1943/DC1]).
Table 3.
Risk of overweight in children at 2, 5, and 8 years of age: multivariate analysis*
| 2 years of age |
5 years of age |
8 years of age |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| n | 1,009 | 896 | 598 | |||
| Maternal diabetes | ||||||
| No diabetes | 1.0 | 1.0 | 1.0 | |||
| Type 1 diabetes | 1.1 (0.7–1.6) | 0.7 | 1.1 (0.7–1.8) | 0.7 | 0.8 (0.5–1.4) | 0.4 |
| Breast-feeding | ||||||
| Never breast-fed | 1.0 | 1.0 | 1.0 | |||
| Full breast-fed ≤4 months | 0.8 (0.5–1.2) | 0.3 | 0.8 (0.5–1.5) | 0.6 | 0.7 (0.4–1.3) | 0.2 |
| Full breast-fed >4 months | 0.6 (0.3–0.9) | 0.02 | 0.5 (0.3–0.9) | 0.03 | 0.3 (0.1–0.6) | 0.002 |
| Any breast-feeding | ||||||
| ≤1 month | 1.1 (0.5–2.4) | 0.8 | 1.7 (0.7–4.0) | 0.2 | 0.7 (0.2–2.3) | 0.7 |
| 1.1–3.0 months | 0.7 (0.4–1.3) | 0.3 | 0.6 (0.3–1.3) | 0.2 | 0.5 (0.2–1.1) | 0.07 |
| 3.1–6.0 months | 0.6 (0.3–1.0) | 0.05 | 1.0 (0.5–1.8) | 0.9 | 0.9 (0.5–1.9) | 0.9 |
| >6 months | 0.7 (0.4–1.1) | 0.1 | 0.4 (0.2–0.8) | 0.007 | 0.2 (0.1–0.5) | 0.001 |
| Birth size | ||||||
| AGA | 1.0 | 1.0 | 1.0 | |||
| SGA | 0.5 (0.2–1.2) | 0.1 | 0.6 (0.2–1.7) | 0.3 | 0.7 (0.2–1.8) | 0.4 |
| LGA | 2.3 (1.5–3.4) | <0.0001 | 3.9 (2.4–6.4) | <0.0001 | 2.5 (1.4–4.5) | 0.003 |
| Maternal age | ||||||
| ≤30.1 years | 1.0 | 1.0 | 1.0 | |||
| >30.1 years | 1.3 (0.9–1.9) | 0.1 | 0.8 (0.5–1.2) | 0.2 | 1.0 (0.6–1.8) | 0.9 |
*Variables that were included in the multiple logistic regression model were maternal diabetes, breast-feeding duration, birth size, and maternal age.
CONCLUSIONS
This study shows associations between childhood overweight and both high birth weight and breast-feeding habits but found no evidence for an independent contribution of maternal type 1 diabetes to childhood overweight up to age 8 years.
Children participating in the BABYDIAB study were followed from birth, and all had a father and/or mother with type 1 diabetes. This provided the opportunity to study the impact of both maternal type 1 diabetes and other gestational and perinatal factors on the risk of overweight. Due to the study design, recall bias in questionnaires addressing breast-feeding duration and smoking behavior during pregnancy was avoided or limited. Weight and height were measured by a pediatrician according to standardized methods, and, therefore, we can rule out the over- or underestimating that may occur when data are reported by parents. Of the enrolled children, 98% have German parents, allowing us to rule out the possibility that results have been influenced by race or ethnicity. A limitation of the current analysis is that other confounding variables that may influence risk of overweight, such as socioeconomic status, educational level of the mother, and maternal BMI, were not available for this analysis. Therefore, we cannot exclude the possibility that the associations observed could in some cases be secondary to other variables.
Our finding that maternal diabetes is not an independant predictor of overweight during childhood is in contrast to a number of previous studies. These other studies reported an increased prevalence of overweight and/or obesity in children of mothers with type 1 diabetes at ages 5.9–9.0 (5), 5–15 (3), and 5–9 (6) years. One study (11) showed no effect of maternal diabetes status on the risk of overweight in breast-fed children. We found that maternal type 1 diabetes did not affect the risk of overweight but that factors previously reported to be linked with maternal type 1 diabetes, such as shorter duration of breast-feeding (12) and greater birth weight (13,14), impacted significantly on risk of overweight in childhood. The reason for the discrepancies between studies could lie in the small number of cases analyzed previously and the lack of confounder variable analysis in some studies.
The multivariate analysis showed that children born LGA were at increased risk of overweight throughout childhood. Our study thus confirms results from previous studies in children of the general population, as well as in offspring of mothers with diabetes, which have shown that being born LGA is an important risk factor for overweight during childhood (6,15,16). Previous studies (17) reported that the age between 2 and 6 years is a critical period for the development of obesity. We could show that children born LGA contributed more than a third of new overweight cases at age 5 years. In contrast, children with an SGA status seemed to be protected from developing overweight between 2 and 5 years of age.
Several studies (18–20) in the general population have demonstrated an inverse association between breast-feeding and obesity at different ages. However, both a meta-analysis and another study (21,22) performed in the general population have shown that the protective effect of breast-feeding on overweight was weakened by adjusting for confounding factors such as birth weight and parental obesity. Separate studies (11,23,24) have reported the risk for overweight in breast-fed offspring of mothers with type 1 or gestational diabetes. Studies in offspring of mothers with type 1 diabetes have provided inconsistent results. Like our study, the Growing Up Today Study (11) found a decreased risk of overweight in breast-fed children of mothers with diabetes. In our multivariate analysis, long duration of breast-feeding protected children who had a first-degree relative with type 1 diabetes from overweight throughout childhood. Moreover, the protective effect of breast-feeding on risk of overweight appeared to increase with age. This protective effect was comparable in children who received full breast-feeding for >4 months and in those with any breast-feeding for a period of >6 months, suggesting that the protective effect can also be achieved by any breast-feeding over a longer time span. This is particularly important for mothers with type 1 diabetes, as they often find it difficult to fully breast-feed their children for several months (12).
In conclusion, our findings indicate that maternal type 1 diabetes is not an independent risk factor for overweight during childhood but that factors associated with maternal type 1 diabetes, such as short breast-feeding duration and high birth size, predispose children to overweight during childhood. Although future research will be needed to investigate factors associated with overweight risk after puberty, our results indicate that mothers with type 1 diabetes should be encouraged to breast-feed and that blood glucose management during pregnancy should be optimized with a view to preventing overweight during early childhood.
Supplementary Material
Acknowledgments
This study was supported by grants from the Juvenile Diabetes Research Foundation (JDRF no. 1-2006-665), the Foundation for Children with Type 1 Diabetes (Stiftung Das Zuckerkranke Kind), and the German Competence Net for Diabetes Mellitus.
No potential conflicts of interest relevant to this article were reported.
This work forms part of the dissertation of M. Pflüger at the Technical University, Munich, Germany.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Barlow SE: Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2001; 120( Suppl. 4): S164– S192 [DOI] [PubMed] [Google Scholar]
- 2. Dabelea D: The predisposition to obesity and diabetes in offspring of diabetic mothers. Diabetes Care 2007; 30( Suppl. 2): S160– S174 [DOI] [PubMed] [Google Scholar]
- 3. Weiss PA, Scholz HS, Haas J, Tamussino KF, Seissler J, Borkenstein MH: Long-term follow-up of infants of mothers with type 1 diabetes: evidence for hereditary and nonhereditary transmission of diabetes and precursors. Diabetes Care 2000; 23: 905– 911 [DOI] [PubMed] [Google Scholar]
- 4. Hunter WA, Cundy T, Rabone D, Hofman PL, Harris M, Regan F, Robinson E, Cutfield WS: Insulin sensitivity in the offspring of women with type 1 and type 2 diabetes. Diabetes Care 2004; 27: 1148– 1152 [DOI] [PubMed] [Google Scholar]
- 5. Rodrigues S, Ferris AM, Perez-Escamilla R, Backstrand JR: Obesity among offspring of women with type 1 diabetes. Clin Invest Med 1998; 21: 258– 266 [PubMed] [Google Scholar]
- 6. Plagemann A, Harder T, Kohlhoff R, Rohde W, Dörner G: Overweight and obesity in infants of mothers with long-term insulin-dependent diabetes or gestational diabetes. Int J Obes Relat Metab Disord 1997; 21: 451– 456 [DOI] [PubMed] [Google Scholar]
- 7. Ziegler AG, Hummel M, Schenker M, Bonifacio E: Autoantibody appearance and risk for the development of childhood diabetes in offspring of parents with type 1 diabetes: the German BABYDIAB study. Diabetes 1999; 48: 460– 468 [DOI] [PubMed] [Google Scholar]
- 8. Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V, Hippel v. A, Jaeger U, Johnsen D, Korte W, Menner K, Müller G, Müller JM, Müller M, Niemann-Pilatus A, Remer T, Schaefer F, Wittchen HU, Zabransky S, Zellner K, Ziegler A, Hebebra J: Perzentile für den Body-mass-Index für das Kinder- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschr Kinderheilkd 2001; 8: 807– 818 [article in German] [Google Scholar]
- 9. Voigt M, Schneider KTM, Stillger R, Pildner von Steinburg S, Fusch C, Hesse V: Analyse des Neugeborenenkollektivs der Jahre 1995–1997 der Bundesrepublik Deutschland. Geburtshilfe Frauenheilkd 2005; 65: 474– 481 ( article in German) [Google Scholar]
- 10. World Health Organization. Indicators for Assessing Breast-Feeding Practices. Report of an Informal Meeting, 11–12 June 1991. WHO/CDD/SER/9114. World Health Org., Geneva, 1991 [Google Scholar]
- 11. Mayer-Davis EJ, Rifas-Shiman SL, Zhou L, Hu FB, Colditz GA, Gillman MW: Breast-feeding and risk for childhood obesity: does maternal diabetes or obesity status matter? Diabetes Care 2006; 29: 2231– 2237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hummel S, Winkler C, Schoen S, Knopff A, Marienfeld S, Bonifacio E, Ziegler AG: Breast feeding habits in families with type 1 diabetes. Diabet Med 2007; 24: 671– 676 [DOI] [PubMed] [Google Scholar]
- 13. Kerssen A, deValk HW, Visser GHA: Increased second trimester maternal glucose levels are related to extremely large-for-gestational-age infants in women with type 1 diabetes. Diabetes Care 2007; 30: 1069– 1074 [DOI] [PubMed] [Google Scholar]
- 14. Mello G, Parretti E, Mecacci F, La Torre P, Cioni R, Cianciulli D, Scarselli G: What degree of maternal metabolic control in women with type 1 diabetes is associated with normal body size and proportions in full-term infants? Diabetes Care 2000; 23: 1494– 1498 [DOI] [PubMed] [Google Scholar]
- 15. Boney CM, Verma A, Tucker R, Vohr BR: Metabolic syndrome in childhood: association with birth weight, maternal obesity and gestational diabetes mellitus. Pediatrics 2005; 115: e290– e296 [DOI] [PubMed] [Google Scholar]
- 16. Moschonis G, Grammatikaki E, Manio Y: Perinatal predictors of overweight at infancy and preschool childhood: the GENESIS study. Int J Obes 2008; 32: 39– 47 [DOI] [PubMed] [Google Scholar]
- 17. Rolland-Cachera MF, Deheeger M, Bellisle F, Sempé M, Guilloud-Bataille M, Patois E: Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr 1984; 39: 129– 135 [DOI] [PubMed] [Google Scholar]
- 18. Arenz S, Rückerl R, Koletzko B, von Kries R: Breast-feeding and childhood obesity: systematic review. Int J Obes Relat Metab Disord 2004; 28: 1247– 1256 [DOI] [PubMed] [Google Scholar]
- 19. Harder T, Bergmann R, Kallischnigg G, Plagemann A: Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol 2005; 162: 397– 403 [DOI] [PubMed] [Google Scholar]
- 20. Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG: The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. Am J Clin Nutr 2005; 82: 1298– 1307 [DOI] [PubMed] [Google Scholar]
- 21. Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG: Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics 2005; 115: 1367– 1377 [DOI] [PubMed] [Google Scholar]
- 22. Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, Steer C, Sheriff A: the Avon Longitudinal Study of Parents and Children Study Team. Early life risk factors for obesity in childhood: cohort study. BMJ 2005; 330: 1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Plagemann A, Harder T, Franke K, Kohlhoff R: Long-term impact of neonatal breast-feeding on body weight and glucose tolerance in children of diabetic mothers. Diabetes Care 2002; 25: 16– 22 [DOI] [PubMed] [Google Scholar]
- 24. Kerssen A, Evers IM, de Valk HW, Visser GH: Effect of breast milk of diabetic mothers on bodyweight of the offspring in the first year of life. Eur J Clin Nutr 2004; 58: 1429– 1431 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.