Abstract
Aims
Patients with Alzheimer’s disease need assistance and supervision of their daily activities. They survive for protracted periods of time, placing an extensive burden of care on the caregiver prior to the patient’s death. The present study addressed the predictive value of behavior-related burden on Alzheimer’s disease caregivers.
Participants
82 patients with probable Alzheimer’s (73.7 ± 8.1 years), and their primary caregivers (59.6 ± 14.8 years, 81.5% women), were assessed.
Methods
Cognitive impairment, neuropsychiatric symptoms, and dementia severity were assessed with Mini Mental State Examination (MMSE), Neuropsychiatric Inventory (NPI), and Clinical Dementia Rating (CDR), respectively. Caregivers were given Zarit’s Burden Interview and Carer Activity Inventory.
Results
Neuropsychiatric symptoms like delusions, hallucinations, restlessness, anxiety, euphoria, disinhibition, unusual motor behavior, sleep disturbances, and appetite alterations were the best caregiver burden predictors (NPI r = 0.482, p < 0.001). No correlation with cognition, disease stage, or negative neuropsychiatric symptoms (depression and apathy) was found.
Conclusion
Increased caregiver burden was related to increased levels of patient behavioral disturbance. Of these symptoms, hallucinations, unusual (motor) behavior, and abnormal behavior at nighttime were the most significant. No correlation with neuropsychiatric symptoms such as apathy and depression was found. This may have relevance to appropriate interventions for caregivers.
Keywords: caregivers, caregiver burden, Alzheimer’s, behavior, neuropsychiatric
Introduction
The prevalence of dementia in developed countries ranges from 1.4% in 65- to 69-year-old subjects to 38.6% in individuals aged 90–94 years (Jorm 1990). The gradual progressive impairment and behavioral symptoms that may emerge in the course of Alzheimer’s disease produce a requirement for care and supervision of daily activities. This usually falls upon relatives acting as informal caregivers, causing them great burden and stress. The term caregiver burden refers to the consequences derived from caring for demented patients. These consequences may be psychological, physical, and economic (Garre-Olmo et al 2002). Caregiver burden is not only present in Alzheimer’s disease. This syndrome has also been noted in other illnesses like stroke, Parkinson’s disease (Thommessen et al 2002), and vascular dementia (Annerstedt et al 2000).
Behavioral disturbances are a common feature in dementia and cause significant caregiver burden (Mangone et al 1993; Absher and Cummings 1994). The symptoms that more frequently caused caregiver burden are aggression, wandering, and delusions (Nagaratnam et al 1998). This demand on the caregiver has been associated with adverse psychological reactions and has been identified as a risk factor for caregiver mortality (Zarit et al 1980; Schulz and Beach 1999). These results have even been confirmed in studies performed with caregivers from different cultural backgrounds (Pang et al 2002). Other studies have tried to describe the differences in the impact of the symptoms according to the sex of the caregivers (Shanks-McElroy et al 2001).
The present study aimed to assess the predictors of burden in caregivers of Alzheimer’s patients in Argentina.
Methods
The studied patients came from the Memory Clinic of the Zubizarreta Hospital and the CEMIC University Institute at Buenos Aires City. The assessment was part of a “Dementia Training Program” sponsored by the City of Buenos Aires Health Secretariat. From September 1 2001 to March 1 2002, a sample of 82 consecutively referred noninstitutionalized patients with probable Alzheimer’s disease according to National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and related Disorders Association (NINCDS-ADRDA) criteria (McKhann et al 1984) and their primary informal caregivers (defined as the persons responsible for the day-to-day decisions and providing care) were studied. Patients who had paid caregivers were not included in this study.
Patient variables
All patients had to go through extensive neurological, neuropsychological, neuropsychiatric, laboratory, and neuroim-aging assessments to fulfil all dementia criteria according to DSM-IV (APA 1994) and probable Alzheimer’s as per NINCDS-ADRDA (McKhann et al 1984).
Cognitive functioning level was assessed by means of the Mini Mental State Examination (MMSE) (Folstein et al 1975), a Buenos Aires version (Spanish translation and norms) (Allegri et al 1999; Butman et al 2001); severity range was determined through Clinical Dementia Rating (CDR) (Hughes et al 1982). For the neuropsychiatric assessment a local Spanish version of the Neuropsychiatric Inventory (NPI) (Cummings et al 1994) was used, which takes into account the following subitems: delusions, hallucinations, restlessness–aggressiveness, depression, anxiety, euphoria–denial, apathy, disinhibition, irritability, unusual (motor) behavior, unusual behavior (at nighttime), and changes in appetite and food intake. Dementia duration and family income were also considered.
Carer variables
A series of variables identified in the literature as being important for understanding caregivers’ burden, health, and emotional well-being was evaluated by means of a semistructured questionnaire. Evaluated demographic–situational items included age, gender, marital status, relationship with the patient, duration of the patient’s disease, hours per week spent with the patient (questionnaire by Gilleard et al 1984), and time spent in patient-related activities (eg, communication, feeding, dressing, transportation, supervision) (questionnaire by Davis et al 1997). The degree of burden experienced by caregivers was evaluated by means of Zarit’s Burden Interview (Zarit et al 1985), consisting of 22 questions evaluated by means of a 5-point scale, ranging from nil = 0 to overburdened = 4.
Because depression influences negatively the caregiver’s evaluation of the patient (Arguelles et al 2001), we defined the following exclusion criteria for the caregivers:
Presence of dementia, depression, or psychosis.
Contact with the patient for less than 10 hours per week.
Statistical analysis
Data were analyzed using the statistical package SPSS® 11.0.0 for Windows® (2001) (SPSS Inc, Chicago, IL, USA). Demographic variables in both populations (patients and caregivers) as well as MMSE, CDR, and NPI general results were expressed by medians and standard deviation. Neuropsychiatric symptoms evaluated by means of NPI were considered globally and partially for each of the areas under study, using the severity by disturbance presence frequency estimate. Influence of cognitive factors on caregiver burden (MMSE), duration stage (CDR), behavioral factors (NPI), time of disease duration, as well as economic level were analyzed by a linear regression model, applying burden level as a dependent variable. Correlations between global burden and different behavioral areas (NPI) were evaluated by means of Spearman’s correlation coefficient.
Results
Eighty-two patients with probable Alzheimer’s disease (NINCDS-ADRDA criteria) and their primary caregivers were assessed. There were 38 men and 44 women in the patient sample with a mean age of 73.7 years (range 50–90). The severity of dementia ranged from very mild to severe on all measures. The duration of illness was 38.7 ± 32.1 months. The mean age of the primary caregivers was 59.6 ± 14.8 years. Most were female (81.5%) and had finished primary school (mean 9.3 years of education). Most were either spouses (54.6%) or children (36%) of the patients. More demographic data for both groups are described in Table 1.
Table 1.
Patient and caregiver demographic data
| Patients with Alzheimer’s | Primary caregivers | |
|---|---|---|
| Age (years) | 73.7 ± 8.1a (range 50–90) | 59.6 ± 14.8 |
| Education (years) | 8.1 ± 3.9 | 9.3 ± 3.3 |
| Gender (m/f) | 38/44 | 15/67 |
| MMSE | 18.3 ± 7 | |
| CDR | 1.6 ± 0.8 (range 0.5–3) | |
| NPI | 24.0 ± 20.2 | |
| Duration of illness (months) | 38.7 ± 32.1 | |
| Income (family group) $/month | 612 ± 729 | |
| Caregiver burden (Zarit et al 1985) | 29.2 ± 18.0 | |
| Relationship to patient | ||
| Spouse | 54.6% | |
| Children | 36.0% | |
| Son/daughter in law | 0% | |
| Other | 9.4% | |
Values expressed are median ± standard deviation (except for gender and caregiver relationship to patient).
The proportion of caregivers who resided with the patients varied with the severity of the pathology (Table 2).
Table 2.
Number of caregivers residing with patients
| MMSE | Total patients | Living with caregiver | Institutionalized |
|---|---|---|---|
| >20 | 21 | 12 | 0 |
| 11–20 | 24 | 16 | 4 |
| <11 | 24 | 8 | 15 |
Abbreviation: MMSE, Mini Mental State Examination.
Caregiver burden ranged from minimal to severe (Zarit’s scale = mean 29.2, range 4–72). The influence on caregiver burden of cognitive impairment (MMSE), disease stage (CDR), behavioral disturbances (NPI), evolution time, family income, and hours per week spent with patient was studied. Using Zarit’s burden scale as the dependent variable, we found the NPI to be the best predictor of caregiver burden (p < 0.001) (Table 3).
Table 3.
Results of regression analysis using Zarit’s (Zarit et al 1985) burden scale score as the dependent variable
| Independent primary variable | Regression B coefficient | p |
|---|---|---|
| MMSE | −0.106 | 0.382 |
| CDR | 0.115 | 0.340 |
| NPI (total score) | 0.482 | <0.001 |
| Income | −0.037 | 0.751 |
| Evolution (months) | 0.081 | 0.525 |
Abbreviations: CDR, Clinical Dementia Rating; MMSE, Mini Mental State Examination; NPI, Neuropsychiatric Inventory.
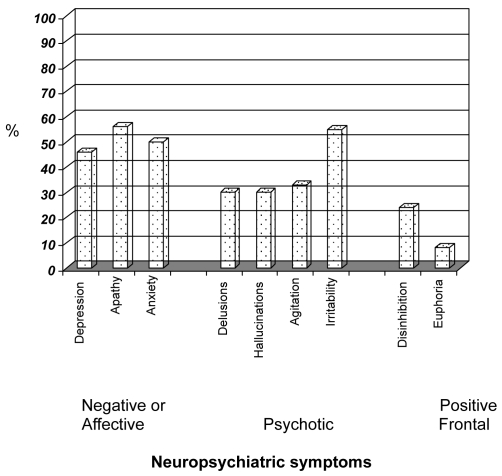
To study which behavioral disturbances caused the burden, a correlation with the different areas of the NPI was performed. The elements of the NPI that correlated better were: hallucinations, anxiety, unusual (motor) behavior, and sleep disturbance (p < 0.01), and delusions, restlessness, disinhibition, and appetite alterations (p < 0.05) (Figure 1 and Table 4)
Figure 1.
Patient’s neuropsychiatric symptoms (percentage of subjects with symptoms).
Table 4.
Correlationa between caregiver burden (Zarit’s Burden Interview [Zarit et al 1985]) and patient’s neuropsychiatric symptoms (NPI)
| Zarit’s Burden Interview
|
||
|---|---|---|
| r | P | |
| NPI total score | 0.482 | < 0.01 |
| Affective symptoms | ||
| Depression | 0.179 | ns |
| Apathy | 0.227 | ns |
| Anxiety | 0.570 | < 0.01 |
| Psychotic symptoms | ||
| Delusions | 0.289 | < 0.05 |
| Hallucinations | 0.398 | < 0.01 |
| Restlessness | 0.297 | < 0.05 |
| Irritability | 0.235 | ns |
| Frontal symptoms | ||
| Euphoria | 0.229 | ns |
| Disinhibition | 0.288 | < 0.05 |
| Other | ||
| Unusual (motor) behavior | 0.392 | < 0.01 |
| Sleep disturbances | 0.477 | < 0.01 |
| Appetite alterations | 0.30 | < 0.05 |
Correlation coefficient for nonparametric Spearman’s test; ns, no significant values.
Abbreviation: NPI, Neuropsychiatric Inventory.
Family burden level showed significant correlation with positive neuropsychiatric symptoms such as hallucinations, unusual (motor) behavior, and abnormal behavior at nighttime. Correlation was also found, but to a lesser degree, with delusions, restlessness, anxiety, disinhibition, and alterations in eating habits. No correlation with negative neuropsychiatric symptoms such as apathy and depression was found. It should be noted that the symptoms having the highest correlation with caregiver burden were not the most frequent.
The only demographic caregiver variable correlating with burden was education. Age, gender, marital status, and family relationship were not significant. Thus, a lower educational level shows a higher burden index (p < 0.01) (Table 5).
Table 5.
Correlationa between caregiver burden level (Zarit’s Burend Interview [Zarit et al 1985]) and demographic carer data
| Zarit’s Burden Interview
|
||
|---|---|---|
| r | P | |
| Age | 0.016 | ns |
| Gender | 0.191 | ns |
| Education | −0.249 | < 0.01 |
| Marital Status | 0.003 | ns |
| Family relationship | −0.062 | ns |
Correlation coefficient for nonparametric Spearman’s test.
Discussion
Alzheimer’s disease patients need assistance and supervision of their daily activities. This frequently falls upon informal caregivers (family members), causing them significant burden and stress. A high prevalence of psychiatric disorders has been detected in caregivers, including a higher intake of psychotropic drugs compared with the general population (Clipp and George 1990). Despite the fact that studies have shown contradictory results (Irwin et al 1997), caregivers are also a target for several stress-related conditions affecting the immune system.
Caregiver burden as a term refers to the consequences of caring for demented patients, and such consequences can be psychological, physical, and economic (Garre-Olmo et al 2002). The term not only applies to caregivers of Alzheimer’s disease patients, but also to caregivers of patients with other chronic or disabling conditions such as vascular dementia or Parkinson’s disease (Thommessen et al 2002).
In our sample, 81.7% of the informal caregivers were women, while 54.6% were spouses and 36% were children of patients. Such percentages are similar to those reported in other studies (Cohen et al 1997). Although several studies have not related gender to caregiver burden, others indicate that this index could be even higher among female caregivers (Gallicchio et al 2002).
In the present study, burden was not related to cognitive impairment (MMSE), or to disease stage (CDR). This lack of association is consistent with findings in the literature (Mangone et al 1993; Cohen et al 1997). Family group income level or duration of illness were also not related to burden.
Conversely, caregiver burden was positively related to behavioral disturbances in patients, as reported in other studies (Mangone et al 1993; Cohen et al 1997; Clyburn et al 2000), and negatively to caregiver’s educational level. The influence of neuropsychiatric symptoms on burden becomes important if we consider that in different samples, the prevalence of these symptoms in Alzheimer’s disease is over 50% (Lyketsos et al 2000). Within the spectrum of these symptoms, not all correlated similarly. Psychiatric symptoms that correlated positively (p < 0.01) with caregiver distress were hallucinations, abnormal behavior (eg, wandering), and sleep disturbances. Delusions, restlessness, anxiety, disinhibition, and appetite alterations also correlated with burden (p < 0.05). All of these symptoms are the so-called “positive symptoms”. Most of the published papers showed similar findings for this group of symptoms, and some have even reported that such symptoms can trigger temporary or permanent institutionalization (Annerstedt et al 2000). Contrary to other papers that correlated patient’s depression to caregiver burden (Teri 1997), no correlation with “negative” affective psychiatric symptoms such as depression or apathy was found in our sample.
In addition to the symptoms described above, another factor has been found to contribute to burden: the patient’s awareness of his/her own deficit influences burden in the early stages of the disease (Selzter et al 1997). This was not studied in our assessment.
Caregiver quality of life and how it is affected in the course of caring for a dementia patient represents a central issue relevant to the environment of the patients. There may be a need for measures to reduce or control behavioral disturbances, particularly positive psychiatric symptoms. This is significant not only for the quality of life of the caregiver and the patient but also for the influence these symptoms have on the caregiver’s judgment of the patient’s functional abilities (Arguelles et al 2001). In fact, caregiver burden is associated with an increased risk of nursing home placement for patients with dementia (Yaffe et al 2002).
Although this study was performed with patients having probable Alzheimer’s disease, caregiver burden, as already mentioned, is not only found when this condition is present, but also among caregivers of vascular dementia patients. At mild stages of disease, the burden even seems to be higher in the caregivers of patients with vascular dementia (Vetter et al 1999).
Strategies, for example education and information, designed to ease caregiver distress have shown their effectiveness on the syndrome’s features (Patterson et al 1999). When caregivers were informed of the disease’s features and prognosis, their burden levels decreased compared with those who had not been informed (Hepburn et al 2001). The same happened following institutionalization of the patient. However, a year after institutionalization, a feeling of frustration still persisted in the caregivers (Elmstahl et al 1998).
Treatment of behavioral disorders helps to diminish caregiver burden (Shigenobu et al 2002). At present, there is clear evidence that pharmacological intervention with cholinesterase inhibitors reduces the prevalence and severity of psychiatric disturbances in Alzheimer’s disease. Several studies have directly tested caregiver burden decrease after anticholinesterase treatment (Fillit et al 2000; Shikiar et al 2000). Correct management of these disturbances, together with adequate educational intervention for caregivers, significantly reduces distress, improving quality of life for both caregiver and patient.
Finally, the time devoted to caring has been related to burden level. It could not be determined, however, if a longer time was caused by loss of efficiency due to the burden or by the fact that patients with psychiatric symptoms demanded more caring time.
Our study limitation has been the lack of caregiver psychological profile, and its relationship to burden and the decision to institutionalize the patient (Colerick and George 1986).
Acknowledgments
The authors thank Dr Jeffrey Cummings (UCLA) for his helpful comments on this article. This research was jointly supported by grants from the Rene Baron Foundation, CEMIC, the Research Council of the Health Secretariat, Government of Buenos Aires City (Dr RF Allegri), the Carrillo-Oñativia Grants (Dr J Butman), and Novartis Argentina.
References
- Absher JR, Cummings JL. Cognitive and noncognitive aspects of dementia syndromes: an overview. In: Burns A, Levy R, editors. Dementia . London: Chapman & Hall Medical; 1994. [Google Scholar]
- Allegri RF, Ollari JA, Mangone CA, et al. El “Mini Mental State Examination” en la Argentina: Instrucciones para su administración. [“Mini Mental State Examination” in Argentina. Instructions for its use] Rev Neurol Argent. 1999;24:31–5. [Google Scholar]
- [APA] American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: APA; 1994. [Google Scholar]
- Annerstedt L, Elmstahl S, Ingvad B, et al. Family caregiving in dementia, an analysis of the caregiver’s burden and the “breaking-point” when home care becomes inadequate. Scand J Public Health. 2000;28:23–31. doi: 10.1177/140349480002800106. [DOI] [PubMed] [Google Scholar]
- Arguelles S, Loewenstein DA, Eisdorfer C, et al. Caregivers’ judgments of the functional abilities of the Alzheimer‘s disease patient: impact of caregivers’ depression and perceived burden. J Geriatr Psychiatry Neurol. 2001;14:91–8. doi: 10.1177/089198870101400209. [DOI] [PubMed] [Google Scholar]
- Butman J, Arizaga RL, Harris P, et al. El “Mini Mental State Examination”en Español. Normas para Buenos Aires. [“Mini Mental State Examination” in Spanish. Buenos Aires Standards] Rev Neurol Argent. 2001;26:11–15. [Google Scholar]
- Clipp EC, George LK. Psychotropic drug use among caregivers of patients with dementia. J Am Geriatr Soc. 1990;38:227–35. doi: 10.1111/j.1532-5415.1990.tb03496.x. [DOI] [PubMed] [Google Scholar]
- Clyburn LD, Stones MJ, Hadjistavropoulos T, et al. Predicting caregiver burden and depression in Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. 2000;55:S2–13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- Cohen RF, Swanwick GRJ, O’Boyle CA, et al. Behaviour disturbance and other predictors of carer burden in Alzheimer’s disease. Int J Geriatr Psychiatry. 1997;12:331–6. [PubMed] [Google Scholar]
- Colerick EJ, George LK. Predictors of institutionalization among caregivers of patients with Alzheimer’s disease. J Am Geriatr Soc. 1986;34:493–8. doi: 10.1111/j.1532-5415.1986.tb04239.x. [DOI] [PubMed] [Google Scholar]
- Cummings JL, Mega M, Gray K, et al. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–14. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- Davis KL, Marin DB, Kane R, et al. The Caregiver Activity Survey (CAS): development and validation of a new measure for caregivers of persons with Alzheimer’s disease. Int J Geriatr Psychiatry. 1997;12:978–88. doi: 10.1002/(sici)1099-1166(199710)12:10<978::aid-gps659>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Elmstahl S, Ingvad B, Annerstedt L. Family caregiving in dementia: prediction of caregiver burden 12 months after relocation to group-living care. Int Psychogeriatr. 1998;10:127–46. doi: 10.1017/s1041610298005249. [DOI] [PubMed] [Google Scholar]
- Fillit HM, Gutterman EM, Brooks RL. Impact of donepezil on care-giving burden for patients with Alzheimer’s disease. Int Psychogeriatr. 2000;12:389–401. doi: 10.1017/s1041610200006499. [DOI] [PubMed] [Google Scholar]
- Folstein MS, Folstein SE, McHugh PR. “Mini Mental State”: A practical method for grading the cognitive state of patients for the clinician”. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gallicchio L, Siddiqi N, Langenberg P, et al. Gender differences in burden and depression among informal caregivers of demented elders in the community. Int J Geriatr Psychiatry. 2002;17:154–63. doi: 10.1002/gps.538. [DOI] [PubMed] [Google Scholar]
- Garre-Olmo J, Lopez-Pousa S, Vilalta-Franch J, et al. Carga del cuidador y síntomas depresivos en pacientes con enfermedad de Alzheimer. Evolución a los 12 meses. [Caregiver burden and depressive symptoms in Alzheimer’s patients. Evolution at 12 months] Rev Neurol. 2002;34:601–7. [PubMed] [Google Scholar]
- Gilleard CJ, Belford H, Gilleard E, et al. Emotional distress amongst the supporters of the elderly mentally infirm. Br J Psychiatry. 1984;145:172–7. doi: 10.1192/bjp.145.2.172. [DOI] [PubMed] [Google Scholar]
- Hepburn KW, Tornatore J, Center B, et al. Dementia family caregiver training: affecting beliefs about caregiving and caregiver outcomes. J Am Geriatr Soc. 2001;49:450–7. doi: 10.1046/j.1532-5415.2001.49090.x. [DOI] [PubMed] [Google Scholar]
- Hughes CD, Berg L, Danziger L, et al. A new rating scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- Irwin M, Hauger R, Patterson TL, et al. Alzheimer caregiver stress: basal natural killer cell activity, pituitary-adrenal cortical function, and sympathetic tone. Ann Behav Med. 1997;19:83–90. doi: 10.1007/BF02883324. [DOI] [PubMed] [Google Scholar]
- Jorm AF. The epidemiology of Alzheimer’s disease and related disorders. London: Chapman and Hall; 1990. [Google Scholar]
- Lyketsos CG, Steinberg M, Tschanz JT, et al. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry. 2000;157:708–714. doi: 10.1176/appi.ajp.157.5.708. [DOI] [PubMed] [Google Scholar]
- Mangone CA, Sanguinetti RM, Baumann PD, et al. Influence of feelings of burden on the caregiver’s perception of patient’s functional status. Dementia. 1993;4:287–93. doi: 10.1159/000107335. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: Report of NINCDS-ADRDA work group under the auspices of Department of Health and Human Service Task Force on Alzheimer’s disease. Neurology. 1984;34:939–44. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Nagaratnam N, Lewis-Jones M, Scott D, et al. Behavioral and psychiatric manifestations in dementia patients in a community: caregiver burden and outcome. Alzheimer Dis Assoc Disord. 1998;12:330–4. doi: 10.1097/00002093-199812000-00013. [DOI] [PubMed] [Google Scholar]
- Pang FC, Chow TW, Cummings JL, et al. Effect of neuropsychiatric symptoms of Alzheimer’s disease on Chinese and American caregivers. Int J Geriatr Psychiatry. 2002;17:29–34. doi: 10.1002/gps.510. [DOI] [PubMed] [Google Scholar]
- Patterson CJ, Gauthier S, Bergman H, et al. The recognition, assessment and management of dementing disorders: conclusions from the Canadian Consensus Conference on Dementia. Dementia. 1999;15(Suppl 12):S1–15. [PMC free article] [PubMed] [Google Scholar]
- Schulz RS, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215–19. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Seltzer B, Vasterling JJ, Yoder JA, et al. Awareness of deficit in Alzheimer’s disease: relation to caregiver burden. Gerontologist. 1997;37:20–4. doi: 10.1093/geront/37.1.20. [DOI] [PubMed] [Google Scholar]
- Shanks-McElroy HA, Strobino J. Male caregivers of spouses with Alzheimer’s disease: risk factors and health status. Am J Alzheimers Dis Other Demen. 2001;16:167–75. doi: 10.1177/153331750101600308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigenobu K, Ikeda M, Fukuhara R, et al. Reducing the burden of caring for Alzheimer’s disease through the amelioration of “delusions of theft” by drug therapy. Int J Geriatr Psychiatry. 2002;17:211–17. doi: 10.1002/gps.551. [DOI] [PubMed] [Google Scholar]
- Shikiar R, Shakespeare A, Sagnier PP, et al. The impact of metrifonate therapy on caregivers of patients with Alzheimer’s disease: results from the MALT clinical trial. Metrifonate in Alzheimer’s disease trial. J Am Geriatr Soc. 2000;48:268–74. doi: 10.1111/j.1532-5415.2000.tb02645.x. [DOI] [PubMed] [Google Scholar]
- Teri L. Behavior and caregiver burden: behavioral problems in patients with Alzheimer disease and its association with caregiver distress. Alzheimer Dis Assoc Disord. 1997;11(Suppl 4):S35–8. [PubMed] [Google Scholar]
- Thommessen B, Aarsland D, Braekhus A, et al. The psychosocial burden on spouses of the elderly with stroke, dementia and Parkinson’s disease. Int J Geriatr Psychiatry. 2002;17:78–4. doi: 10.1002/gps.524. [DOI] [PubMed] [Google Scholar]
- Vetter PH, Krauss S, Steiner O, et al. Vascular dementia versus dementia of Alzheimer’s type: do they have differential effects on caregivers’ burden? J Gerontol B Psychol Sci Soc Sci. 1999;54:S93–8. doi: 10.1093/geronb/54b.2.s93. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Fox P, Newcomer R, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287:2090–7. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Orr NK, Zarit JM. The hidden victims of Alzheimer’s disease: families under stress. New York: New York University Pr; 1985. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649–55. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]