Abstract
Neuroendocrine neoplasm of the larynx is a morphologically heterogeneous group of tumors. This unusual neoplasm includes the four different type of tumors. Paraganglioma is the best-known neural origin tumor. The epithelial origin tumor is further divided based on the degree of differentiation into well, moderately, and poorly differentiated carcinoma. The diverse biological behavior of neuroendocrine neoplasm of larynx makes an accurate diagnosis of paramount importance, since treatment depends on diagnostic accuracy. The diagnosis is based primarily on light microscopy, and immunohistochemical and/or ultrastructural investigations are needed to diagnose correctly. The mainstay of treatment of moderately differentiated neuroendocrine carcinoma of the larynx is surgery. Elective neck treatment should be performed considering the high likelihood of cervical lymph node metastases. The 5-yr survival rate approximates 50%, and 10-yr survival rate is only 30%.
Keywords: Neuroendocrine carcinoma
INTRODUCTION
Neuroendocrine neoplasm can occur in any organ of the body, yet it is generally localized in the gastrointestinal system or the bronchial system. Goldman et al. (1) in 1969 first described laryngeal neuroendocrine neoplasm as a distinct clinical and pathologic entity, and over 500 cases of this neoplasm have been reported in the English literature since then. The clinical behavior and overall prognosis show wide variations between the different tumor types. In this article, we describe a rare case of a moderately differentiated neuroendocrine carcinoma of the larynx and we summarize the current literature regarding this unusual tumor (2-4).
CASE REPORT
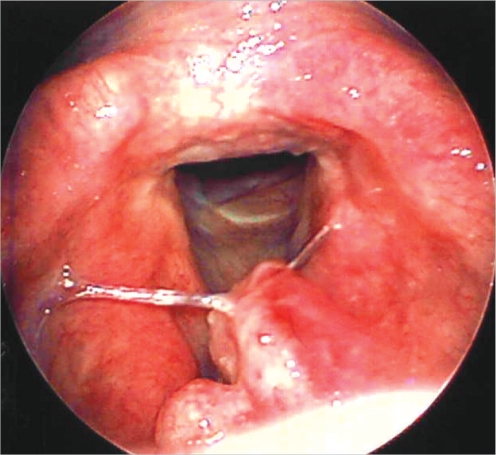
A 59-yr-old man with a history of heavy smoking presented with a change of voice that he'd experienced for one month. The patient had no other symptoms. On laryngoscopic examination, a submucosal mass was seen on the laryngeal surface of the epiglottis. Both the true vocal cords were mobile (Fig. 1). Two enlarged lymph nodes were palpable on the neck examination at the left level II and III areas.
Fig. 1.
Laryngoscopic image showing a submucosal mass involving laryngeal surface of the epiglottis. Both true vocal cords are mobile and the tumor has no glottic extension. Anterior commisure is free of tumor.
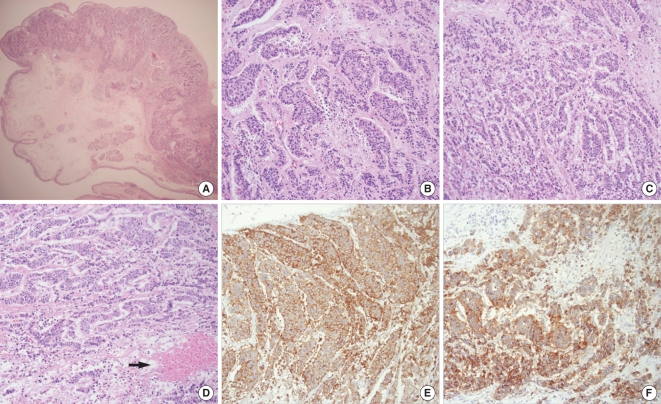
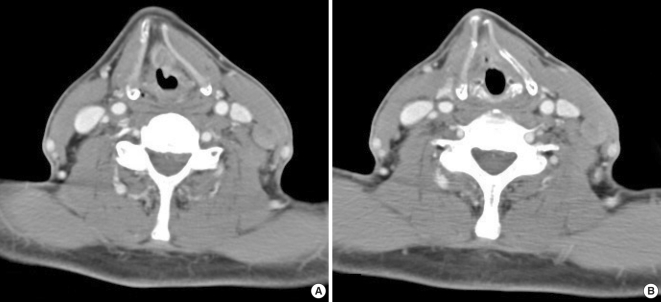
We performed biopsy and mapped the tumor with using a suspension laryngoscope. The tumor had no glottic extension and the anterior commissure was free of tumor. Histopathologic analysis showed moderately differentiated neuroendocrine carcinoma (Fig. 2). The CT scan demonstrated a supraglottic mass invading the pre-epiglottic space, and there were multiple metastatic neck nodes at the left level II and III areas (Fig. 3). No distant metastatic lesion was noted on the chest X-ray, abdominal sonogram, Gfiber exam and bone scan.
Fig. 2.
Pathologic pictures. (A) Low power view with overlying intact mucosa (hematoxylin-eosin [H&E], magnification ×20). (B) High-power view showing pseudogland and rodget arrangement as a neuroendocrine differentiation (H&E, magnification ×200). (C) Cord and trabecular arrangement with nuclear and cellular pleomorphism (H&E, magnification ×200). (D) Tumor necrosis area (arrow) (H&E, magnification ×200). (E) Positive immunoreaction to chromogranin (magnification ×200). (F) Positive immunoreaction to synaptophysin (magnification ×200).
Fig. 3.
The contrast-enhanced CT scans. (A) Supraglottic tumor invades the pre-epiglottic space. (B) Multiple neck metastases are seen at the left level II, III areas.
The patient subsequently underwent supraglottic partial laryngectomy with left radical neck dissection. The histopathology of the surgical specimens revealed moderately differentiated neuroendocrine carcinoma with a tumor-free resection margin. Four metastatic lymph nodes were identified in the neck dissection specimen. The patient's postoperative course was not complicated except for a chyle fistula that was resolved with conservative management. Postoperative radiation treatment was done on the location of the primary tumor and both neck areas.
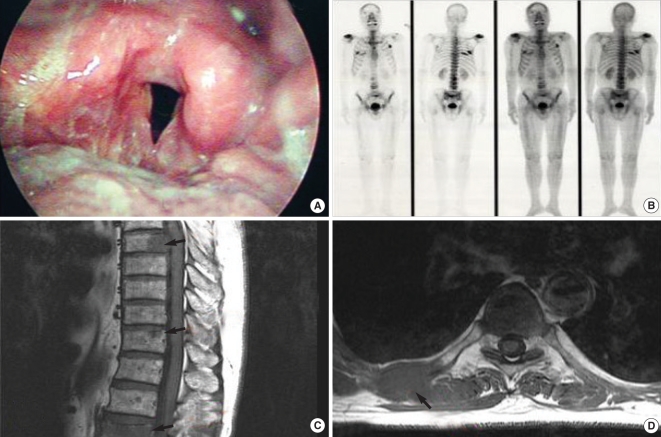
At the 6 months postoperative follow-up exam, the patient complained of back pain with a tingling sense in the lower leg. A bone scan showed multiple bone metastases. Multiple metastatic lesions at the T7 and T11 levels with a compression fracture at the L2 level were identified on the spine MRI scan (Fig. 4). Radiation therapy was administered on the lumbar spine for the pathologic fracture and palliative chemotherapy was also performed, but the patient died from his cancer 3 weeks later.
Fig. 4.
At the follow-up of 6 months after operation. (A) Laryngoscopic image shows postradiation edema around previous operative area. But there is no evidence of local recurrence. (B) Bone scan image demonstrates multiple bone metastases (rib, spine, shoulder, skull base). (C) T1-weighted sagittal MRI scan shows metastatic lesions at T7, T11 level with compression fracture at L2 level (arrows). (D) Expansile metastatic lesion is noted at the right 7th rib (T1-weighted axial MRI scan, arrow).
DISCUSSION
Although neuroendocrine neoplasm of the larynx is uncommon, it is the most common non-epidermoid neoplasm of this organ. This tumor can be divided into the epithelial and neural origin groups. The best-known neural origin tumor is paraganglioma. The epithelial origin tumors are further subclassified based on the degree of differentiation (well, moderately, and poorly differentiated carcinoma). Well differentiated neuroendocrine carcinoma (typical carcinoid) is an extremely rare subtype and it carries the best prognosis. This tumor is preferably treated by conservative surgery unless this is expensive, and elective neck dissection is not indicated. Poorly differentiated or small cell neuroendocrine carcinoma is similar in appearance and behavior to small cell lung carcinoma. It is the most highly malignant neoplasm with frequent metastases and a poor survival rate. The same as for small cell lung carcinoma, chemotherapy, and radiation therapy are the preferred treatment modalities (2, 5, 6).
The neuroendocrine neoplasm that's caused the greatest diagnostic confusion for moderately differentiated neuroendocrine carcinoma is laryngeal paraganglioma. However, its biological behavior is typically benign (2, 3, 7). Complete surgical resection is the treatment of choice; elective neck dissection is not necessary and metastasis is very rare. Overall, the prognosis for patients with this tumor is excellent (2, 8).
Moderately differentiated neuroendocrine carcinoma (atypical carcinoid) is the most common neuroendocrine tumor of the larynx. It is more common in the older age men (6th decade) who have a history of cigarette smoking. The vast majority of this tumor shows a supraglottic origin (5). The diagnosis may be difficult, especially on the initial biopsy evaluation, but making a precise diagnosis is crucial for selecting the proper therapy and achieving a good patient outcome. In contrast with well differentiated laryngeal tumor, mitosis, cellular pleomorphism, and necrosis are the critical features for the diagnosis. Immunohistochemical staining is important for making the correct diagnosis of atypical carcinoid. Carcinoma cells are usually positive for markers such as chromogranin, synaptophysin, keratin, calcitonin and carcinoembryonic antigen. The final diagnosis should not be based solely on the presence or absence of a single immunohistochemical stain marker, and a panel of immunohistochemical antibodies should be utilized (3, 5, 8). Unlike well differentiated laryngeal tumor, moderately differentiated neuroendocrine carcinoma of the larynx is an aggressive and potentially widely metastasizing malignancy. Nodal metastases are frequent and distant metastases are not uncommon (2). The ideal therapy remains a subject of debate. Complete surgical removal is recommended and supraglottic laryngectomy is often indicated when considering the primary site of the lesion. Bilateral elective neck treatment should be performed for the N0 cases because of the high risk of cervical lymph node metastases. This tumor is reported to be radiotherapy and chemo therapy resistant. However, the addition of radiation therapy appears warranted for cases of local extension, multiple nodal metastases or extracapsular disease (5, 8, 9). Batsakis et al. (10) reported that elevated calcitonin levels could be regarded as a specific marker for laryngeal atypical carcinoid. However, Mcbride et al. (2) revealed that an elevated serum calcitonin level was almost always present in patients with medullary thyroid carcinoma, but an elevated serum calcitonin level has been only occasionally reported in patients with atypical laryngeal carcinoid. Future studies will be required to investigate the role of calcitonin as a postoperative follow-up tool. In a minority of cases, paraneoplastic syndrome may precede the clinical manifestation of persistent or recurrent tumor, or asymptomatic metastases (7). The 5-yr survival rate is approximately 50%, and the 10-yr survival rate is only 30% (2,8).
In conclusion, this heterogeneous group of disorders has different prognoses and rational for their management. Therefore, a precise histological diagnosis is crucial for administering the appropriate therapy.
References
- 1.Goldman NC, Hood CI, Singleton GT. Carcinoid of the larynx. Arch Otolaryngol. 1969 Jul;90(1):64–67. doi: 10.1001/archotol.1969.00770030066013. [DOI] [PubMed] [Google Scholar]
- 2.McBride LC, Righi PD, Krakovitz PR. Case study of well-differentiated carcinoid tumor of the larynx and review of laryngeal neuroendocrine tumors. Otolaryngol Head Neck Surg. 1999 Apr;120(4):536–539. doi: 10.1053/hn.1999.v120.a85070. [DOI] [PubMed] [Google Scholar]
- 3.Ferlito A, Barnes L, Rinaldo A, Gnepp DR, Milroy CM. A review of neuroendocrine neoplasms of the larynx: update on diagnosis and treatment. J Laryngol Otol. 1998 Sep;112(9):827–834. doi: 10.1017/s0022215100141830. [DOI] [PubMed] [Google Scholar]
- 4.Hauser H, Wolf G, Uranus S, Klimpfinger M. Neuroendocrine tumors in various organ systems in a ten-year period. Eur J Surg Oncol. 1995 Jun;21(3):297–300. doi: 10.1016/s0748-7983(95)91624-5. [DOI] [PubMed] [Google Scholar]
- 5.Gillenwater A, Lewin J, Roberts D, El-Naggar A. Moderately differentiated neuroendocrine carcinoma (atypical carcinoid) of the larynx: a clinically aggressive tumor. Laryngoscope. 2005 Jul;115(7):1191–1195. doi: 10.1097/01.MLG.0000166179.40750.1B. [DOI] [PubMed] [Google Scholar]
- 6.Ferlito A, Rinaldo A. The spectrum of endocrinocarcinomas of the larynx. Oral Oncol. 2005 Oct;41(9):878–883. doi: 10.1016/j.oraloncology.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Chung JH, Lee SS, Shim YS, Kim SY, Nam SY, Kim DH, et al. A study of moderately differentiated neuroendocrine carcinomas of the larynx and an examination of non-neoplastic larynx tissue for neuroendocrine cells. Laryngoscope. 2004 Jul;114(7):1264–1270. doi: 10.1097/00005537-200407000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Ferlito A, Shaha AR, Rinaldo A. Neuroendocrine neoplasms of the larynx: diagnosis, treatment and prognosis. ORL J Otorhinolaryngol Relat Spec. 2002 Mar–Apr;64(2):108–113. doi: 10.1159/000057788. [DOI] [PubMed] [Google Scholar]
- 9.Shemen L, Petratos P, Patel S, Horowitz L. Infiltrating, moderately differentiated neuroendocrine tumor of the larynx: a brief report. Ear Nose Throat J. 2003 Mar;82(3):205–207. [PubMed] [Google Scholar]
- 10.Batsakis JG, el-Naggar AK, Luna MA. Neuroendocrine tumors of larynx. Ann Otol Rhinol Laryngol. 1992 Aug;101(8):710–714. doi: 10.1177/000348949210100817. [DOI] [PubMed] [Google Scholar]