Abstract
Necrotizing Sialometaplasia (NS) is a benign, self-limiting inflammatory disease of the mucus-secreting glands, and this illness mainly involves the minor salivary glands. The significance of NS resides in its clinical and histopathological resemblance to malignancy. We present here a case of necrotizing sialometaplasia on the soft palate, and this was accompanied by adenoid cystic carcinoma. We report here on this case to draw attention to the difficulty for deciding the extent of resecting a malignancy, and especially when the malignancy is simultaneously accompanied by necrotizing sialometaplasia.
Keywords: Necrotizing sialometaplasia, Adenoid cystic carcinoma
INTRODUCTION
Necrotizing Sialometaplasia (NS) was initially defined by Abrams et al. (1) in 1973 as a reactive necrotizing inflammatory process involving the mucous salivary glands on the hard palate. It can be found at any site that contains salivary gland tissue, from the paranasal sinuses to the lung, but most of the cases have been reported in the oral cavity, including the hard palate, soft palate and lip (2). About two thirds of these lesions are unilateral; however, bilateral (3) and midline locations (4) have also been reported. The general manifestation is a painful ulcer or submucosal swelling (1). The pathogenesis of this lesion is thought to involve ischemia because infarction is seen microscopically in the early stage (5). This ischemic condition may occur after local trauma, smoking, bulimia, a surgical procedure or injection of local anesthesia (5). Complete healing usually occurs without treatment within 3-12 weeks (5). Recognition of necrotizing sialometaplasia is important because this lesion may mimic malignancy, both clinically and histologically, such as squamous cell carcinoma or mucoepidermoid carcinoma (6). Misdiagnosis may result in unnecessary or inappropriate surgical therapy (7, 8). We report here on a case of necrotizing sialometaplasia of the soft palate that was accompanied by adenoid cystic carcinoma. We want to draw attention to the difficulty for deciding the extent of resecting a malignancy, and especially when the malignancy is simultaneously accompanied by necrotizing sialometaplasia.
CASE REPORT
An otherwise healthy 58-yr-old man presented with a 4-month history of a painful lesion on the soft palate. On physical examination, a painful 1×1 cm sized submucosal mass was palpated on the right side of the soft palate. An incisional biopsy was taken from the mass. The histopathologic result of the incisional biopsy specimen was reported as adenoid cystic carcinoma (Fig. 1). The MRI scan demonstrated a diffuse infiltrating lesion involving the entire soft palate, the right anterior pillar and the hard palate submucosal area (Fig. 2). On the operative field, as was expected, we couldn't determine the clear-cut margin of the mass. A portion of the mass had expanded into the nasal cavity. We removed the mass as widely as possible. The resection margin was confirmed on the frozen section. The defect of the soft palate was reconstructed with a superior-based posterior pharyngeal wall mucosal flap. However, the final histopathologic report showed that adenoid cystic carcinoma was only present in a small portion (2×1×1 cm) in the superficial side and the underlying deep portion of the surgical specimen showed the histopathologic feature of necrotizing sialometaplasia (Fig. 3, 4). Post-operative radiotherapy was done (6,000 cGy) for treating the perineural invasion of the adenoid cystic carcinoma. The patient has had no recurrence during one-year of follow-up.
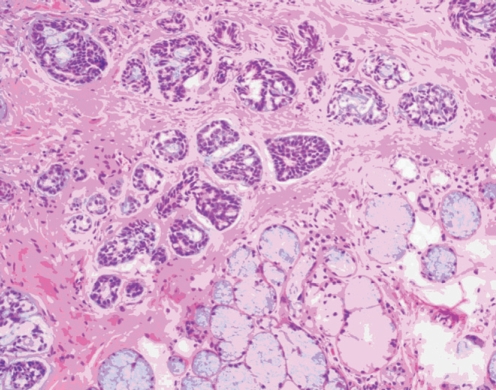
Fig. 1.
The specimen from the first incisional biopsy demonstrated adenoid cystic carcinoma that showed a cribriform pattern without any evidence of NS.
NS: necrotizing sialometaplasia.
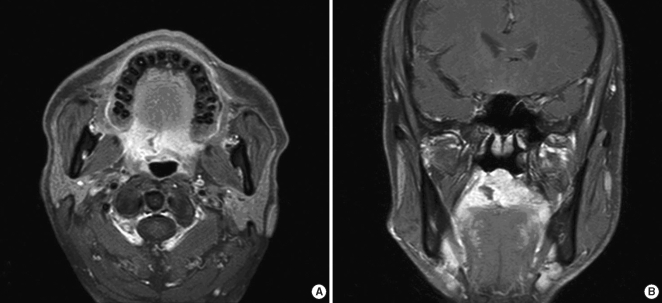
Fig. 2.
The gadolinium enhanced T1-weighted axial (A) and coronal (B) images demonstrate diffuse enhancement involving the entire soft palate, the right anterior pillar and the submucosal area of the hard palate. The incisional biopsy site is seen as a defect on the right site of the soft palate.
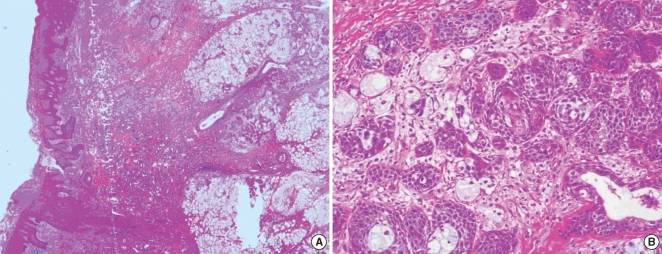
Fig. 3.
A sample from the wide excisional specimen demonstrated superficially remaining adenoid cystic carcinoma and NS in the underlying tissue of the deeper portion (A). The NS was composed of chronic inflammation, mild fibrosis, hemorrhage and metaplastic squamous epithelium that mimicked well differentiated squamous cell carcinoma (B).
NS: necrotizing sialometaplasia.
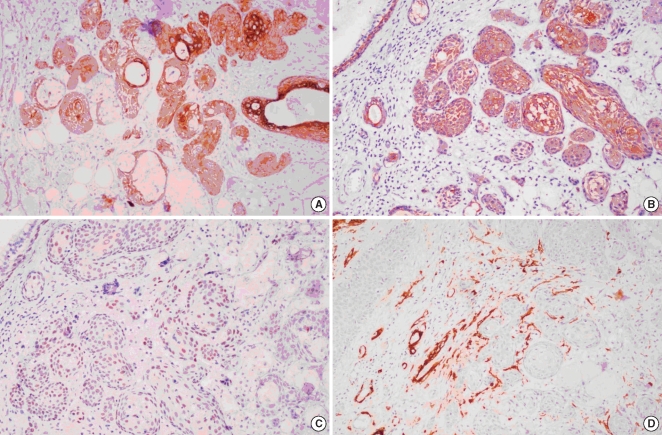
Fig. 4.
Immunohistochemical staining of NS. CK7 showed moderate diffuse cytoplasmic and membranous reactivity in the metaplastic cells (A), and CK5/6 showed strong diffuse cytoplasmic positivity in all the metaplastic cells (B). P63 showed moderate nuclear positivity in the basal layer of the ducts and metaplastic cells (C). SMA showed focal positivity in the periphery of the metaplastic squamous nests (D).
NS: necrotizing sialometaplasia; CK: cytokeratin; SMA: smooth muscle actin.
DISCUSSION
To the best of our knowledge, this case represents the first reported case of NS accompanied by adenoid cystic carcinoma.
Most of the recently reported NS cases have emphasized that the resemblance of the clinical and histological findings of NS to malignancy might result in misdiagnosis and unnecessary or inappropriate surgical therapy (1-8). These reports have also emphasized that an incisional biopsy must be performed on the lesion and careful histopathologic examination should be done to determine the proper treatment and management regimen (9). But in this case, on the contrary, NS and adenoid cystic carcinoma coexisted simultaneously when we performed MRI, so we couldn't discriminate between benign and malignant lesion according to the radiological evaluation at that time. We usually we decide on the extent of the surgical resection according to the preoperative radiologic findings or by the results of the frozen biopsy from the operative field. So eventually, according to the MRI findings and the incisional biopsy report, we couldn't perform wide enough excision of tumor even though the malignancy was restricted to only a small portion.
There are two possible explanations for the pathogenesis of NS in this case. First, the incisional biopsy or the local anesthesia that was administered for the biopsy can be a possible cause of the NS (5). We performed MRI during the 6 day period after incisional biopsy. Brannon et al. (2) reported on 25 cases of NS that developed after the patients had undergone initial surgical procedures, and this malady was noted from 6 to 53 days postoperatively, with a mean interval of 18 days. Six days is thought to be enough time to develop NS. Second, the tumor itself could be another predisposing factor to cause NS (5). For our case, we can postulate that the pressure from the tumor on the adjacent vascular structures could have helped generate the NS (5). In any case, as tumor could be the cause of NS, the chance of coexisting tumor and NS is always possible. When they coexist at the same area, it is absolutely important to discriminate one from the other, especially when one is malignant disease and the other is benign disease. But unfortunately, the result of incisional biopsy might be different depending on the exact site of biopsy (Fig. 5).
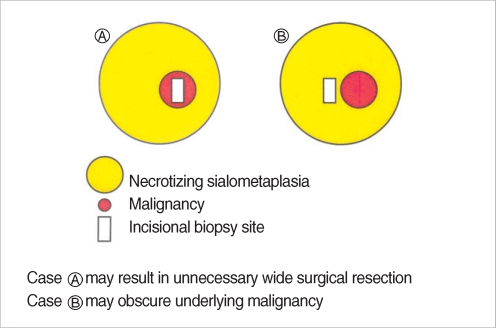
Fig. 5.
The diagram demonstrates that the result of incisional biopsy might be different depending on the exact site where the biopsy is taken.
Farina et al. (10) reported the MRI findings of necrotizing sialometaplasia in their study. They said that a fluid-like appearance of a mass lesion and the absence of contrast enhancement could help to exclude salivary gland neoplasm and this might be the MRI findings suggestive of NS (10). But in our case, neither a fluid-like appearance nor the absence of contrast enhancement was found in MRI. On the contrary, the gadolinium enhanced T1 weighted image showed diffuse enhancement on the entire soft palate, the right anterior pillar and the submucosal area of the hard palate. That's the reason why we thought it might be an infiltrating tumor and so we performed wide excision of the tumor. We think that the MRI findings might be different for each stage of NS.
Anneroth and Hansen (11) defined the pathogenesis of NS by five histologic stages: Infarction, sequestration, ulceration, the reparative stage and healed stage. Brannon et al. (2) described microscopic finding that included coagulation necrosis of the salivary gland acini during the early stage and squamous metaplasia of the ducts and reactive fibrosis during the late stage. Necrosis of the glandular acini could easily be found in the infarct stage (5). An extensive infarct leads to sequestration of the necrotic acini, resulting in ulceration (5). Pseudoepitheliomatous hyperplasia could develop during the healing process of ulceration (5). However, if the infarct is limited in its extent, then sequestration and ulceration do not occur, and necrosis might occur just in a small portion (5).
The significance of NS lies in the fact that it can be confused with malignant neoplasm (1-8). The repair of the ductal epithelium and acini by squamous metaplasia with the accompanying pseudoepitheliomatous hyperplasia can be confused on the microscopy examination with mucoepidermoid carcinoma or squamous cell carcinoma (5).
Rizkalla and Toner (6) investigated the use of immunohistochemistry to distinguish NS from squamous cell and mucoepidermoid carcinoma by identifying myoepithelial cells and the cytokeratin expression. They used several immunohistochemical markers such as calponin, S100, smooth muscle actin (SMA), p63, cytokeratin 7 (CK7), cytokeratin 5 (CK5), cytokeratin 6 (CK6) and CAM5.2 (6). Their results showed that residual myoepithelial cells were identified at the periphery of the epithelial islands in all case of NS, in contrast to mucoepidermoid and squamous cell carcinoma (6). They also reported that a moderate expression rather than an extensive expression of CK7 could help to distinguish NS from mucoepidermoid carcinoma (6). In our case, we used the immunohistochemical marker S-100 and SMA for myoepithelial cells, CK7 for duct epithelial cells and CK5/6 and p63 for basal cells. The result of SMA was focally positivity in the periphery of the squamous metaplasia. CK7 showed diffuse cytoplasmic positivity in the metaplastic nests, and this was especially strong in the central or luminal portion of the nests. CK5/6 showed strong diffuse cytoplasmic positivity in almost all the metaplastic cells. P63 stained moderately in the nuclei of metaplastic cells.
In summary, recognition of necrotizing sialometaplasia is essential because this lesion may mimic malignancy such as squamous cell carcinoma or mucoepidermoid carcinoma both clinically and histologically. An adequate biopsy and an awareness of this disease entity are important to avoid inappropriate and unnecessary surgical resection.
References
- 1.Abrams AM, Melrose RJ, Howell FV. Necrotizing sialometaplasia: a disease simulating malignancy. Cancer. 1973 Jul;32(1):130–135. doi: 10.1002/1097-0142(197307)32:1<130::aid-cncr2820320118>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 2.Brannon RB, Fowler CB, Hartman KS. Necrotizing sialometaplasia: a clinicopathologic study of sixty-nine cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1991 Sep;72(3):317–325. doi: 10.1016/0030-4220(91)90225-2. [DOI] [PubMed] [Google Scholar]
- 3.Keogh PV, O'Regan E, Toner M, Flint S. Necrotizing sialometaplasia: an unusual bilateral presentation associated with antecedent anaesthesia and lack of response to intralesional steroids. Case report and review of the literature. Br Dent J. 2004 Jan;196(2):79–81. doi: 10.1038/sj.bdj.4810892. [DOI] [PubMed] [Google Scholar]
- 4.Daudia A, Murty GE. First case of full-thickness palatal necrotizing sialometaplasia. J Laryngol Otol. 2002 Mar;116(3):219–220. doi: 10.1258/0022215021910384. [DOI] [PubMed] [Google Scholar]
- 5.Imbery TA, Edwards PA. Necrotizing sialometaplasia: literature review and case reports. J Am Dent Assoc. 1996 Jul;127(7):1087–1092. doi: 10.14219/jada.archive.1996.0334. [DOI] [PubMed] [Google Scholar]
- 6.Rizkalla H, Toner M. Necrotizing sialometaplasia versus invasive carcinoma of the head and neck: the use of myoepithelial markers and keratin subtypes as an adjunct to diagnosis. Histopathology. 2007 Aug;51(2):184–189. doi: 10.1111/j.1365-2559.2007.02762.x. [DOI] [PubMed] [Google Scholar]
- 7.Fechner RE. Necrotizing sialometaplasia: a source of confusion with carcinoma of the palate. Am J Clin Pathol. 1977 Apr;67(4):315–317. doi: 10.1093/ajcp/67.4.315. [DOI] [PubMed] [Google Scholar]
- 8.Mesa ML, Gertler RS, Schneider LC. Necrotizing sialometaplasia: frequencyof histologic misdiagnosis. Oral Surg Oral Med Oral Pathol. 1984 Jan;57(1):71–73. doi: 10.1016/0030-4220(84)90264-0. [DOI] [PubMed] [Google Scholar]
- 9.Correll RW, Wescott WB, Pierce GL. Asymptomatic, nonulcerated swelling of the posterior hard palate. J Am Dent Assoc. 1982 Sep;105(3):512–513. doi: 10.14219/jada.archive.1982.0345. [DOI] [PubMed] [Google Scholar]
- 10.Farina D, Gavazzi E, Avigo C, Borghesi A, Maroldi R. Case report. MRI findings of necrotizing sialometaplasia. Br J Radiol. 2008 Jun;81(966):e173–e175. doi: 10.1259/bjr/51447334. [DOI] [PubMed] [Google Scholar]
- 11.Anneroth G, Hansen LS. Necrotizing sialometaplasia: the relationship of its pathogenesis to its clinical characteristics. Int J Oral Surg. 1982 Oct;11(5):283–291. doi: 10.1016/s0300-9785(82)80027-6. [DOI] [PubMed] [Google Scholar]