Abstract
INTRODUCTION AND OBJECTIVES:
Many dispensing errors occur in the hospital, and these can endanger patients. The purpose of this study was to assess the rate of dispensing errors by a unit dose drug dispensing system, to categorize the most frequent types of errors, and to evaluate their potential clinical significance.
METHODS:
A prospective study using a direct observation method to detect medication-dispensing errors was used. From March 2007 to April 2007, “errors detected by pharmacists” and “errors detected by nurses” were recorded under six categories: unauthorized drug, incorrect form of drug, improper dose, omission, incorrect time, and deteriorated drug errors. The potential clinical significance of the “errors detected by nurses” was evaluated.
RESULTS:
Among the 734 filled medication cassettes, 179 errors were detected corresponding to a total of 7249 correctly fulfilled and omitted unit doses. An overall error rate of 2.5% was found. Errors detected by pharmacists and nurses represented 155 (86.6%) and 24 (13.4%) of the 179 errors, respectively. The most frequent types of errors were improper dose (n = 57, 31.8%) and omission (n = 54, 30.2%). Nearly 45% of the 24 errors detected by nurses had the potential to cause a significant (n = 7, 29.2%) or serious (n = 4, 16.6%) adverse drug event.
CONCLUSIONS:
Even if none of the errors reached the patients in this study, a 2.5% error rate indicates the need for improving the unit dose drug-dispensing system. Furthermore, it is almost certain that this study failed to detect some medication errors, further arguing for strategies to prevent their recurrence.
Keywords: Adverse Event, Drug Error, Patient security, Risk Management, Unit Dose
INTRODUCTION
Reducing the incidence of drug-related iatrogenic disease is a public health concern in France and around the world. Reports on the quality of care by the USA Institute of Medicine, found that in the USA, over one million injuries and at least 44 000 deaths occur annually as a result of medical errors. Particularly in the USA medication errors cause over 7 000 deaths per year and result in adverse effects in 2% of in-hospital patients.1Medication errors are recognized as a major cause of medical errors, which can harm patients and induce adverse drug events (ADEs).2,3 Furthermore in the USA medication errors compromise patient confidence in the health care system and increase health care costs. Bates et al. 4 estimated that 0.3 medication errors occur per patient per day and approximately 1% of medication errors cause an ADE. In an intensive care unit, also in the USA, Kopp et al.5 identified one error for every five doses of medication administered. Notably, the outcome or clinical significance of many medication errors may be minimal, with few or no consequences that adversely affect a patient. But, because hospitalized patients are often critically ill, some medications errors cannot be taken lightly. In a large study conducted in 11 medical and surgical units in two tertiary care hospitals in the USA, Bates et al.6 found that 42% of serious and life-threatening ADEs were preventable.
Medication errors are an important clinical problem that can occur at every stage of the drug delivery process.7 Effective systems for prescribing, dispensing, and administering medications should be established with safeguards to prevent errors. Dispensing errors are usually associated with poor safety and inefficient dispensing systems. Despite various methodologies, several previous studies8–11 have reported rates of pharmacy-dispensing errors detected by pharmacists ranging from 1.0% to 2.9%. In a 4-year study in the USA, Roland12 reported 82 dispensing errors, two of which were considered major errors and resulted from incorrect drug selection. However, this study relied on self-reporting to detect dispensing errors and probably underestimated the incidence of these errors. Klein et al.13 compared error rates for a manual dispensing system and an automated one and found error rates of 0.84% and 0.65%, respectively. Thus, detecting dispensing errors should be a component of the pharmacy’s routine quality control. Even if the hospital pharmacy’s medication dispensing process is recognized as a source of medication errors and potential ADEs, the potential for patient harm is rarely evaluated. For the sake of efficiency, pharmacy technicians fill the medication cassettes of a unit dose drug-dispensing system, and then pharmacists check their work. In March 2007, in order to achieve the highest possible safety level, the cardiovascular department of the Percy military hospital established a unit dose drug-dispensing system unusual for France. The purpose of the present study was to assess the rate of dispensing errors in this central pharmacy and in the cardiovascular department as a whole. The analysis examined the most frequent types of errors and evaluated their potential clinical significance.
MATERIALS AND METHODS
Setting
The study was conducted in the central pharmacy and cardiovascular department (30 beds) of the 354-bed Percy military hospital in Clamart (France) during the two-month period of March and April, 2007. The study followed the dispensing activities of the pharmacy between 8 a.m. and 6 p.m. from Monday to Friday. In the central pharmacy, drugs were dispensed over the weekend, but not prescriptions were accepted. Every day, the medical staff brought photocopies of all written physicians’ prescriptions to the central pharmacy. Handwritten prescriptions were clinically reviewed, modified if necessary, and approved by a pharmacist. After pharmacist approval, a pharmacy technician filled the medication cassette using the original approved (or modified and approved) prescription. Oral pharmaceutical forms were dispensed in aliquots with enough tablets or capsules for one patient for 24 hours, in a unit dose medication cassette made up of 4 compartments: morning, midday, evening and night. At the end of the drug-filling process, pharmacists examined medication cassettes. Dispensing errors defined as errors detected by pharmacists (EDPs) were corrected before delivery of the medication to the cardiovascular department. In the cardiovascular department, nurses performed a second check just before administering medications. Errors detected by nurses (EDNs) were defined as technicians’ errors in filling prescriptions that were missed by pharmacists but intercepted and corrected by nurses. Pharmacy technicians, pharmacists, and nurses were aware of the checks performed at the different stages of the drug delivery process, but they were not informed of the study and its purpose. During the study, the names of the persons who committed the errors were not documented. Moreover, during the study, pharmacists and nurses did not share information about errors they had detected. All EDPs and EDNs were recorded by an independent pharmacist observer. In addition, both a physician of the cardiovascular department and the pharmacist observer reviewed and assessed the potential clinical significance of all EDNs. Each reviewer determined whether the patient could have suffered an injury if the dispensing error had not been intercepted by nurses prior to administering the erroneous drug. A three-scale classification system was used: no potential to cause an ADE, potential to cause a significant ADE, or potential to cause a serious ADE.
Definitions
For the purpose of this study, a dispensing error was defined as any discrepancy between the interpretable written prescription, including modifications made by a pharmacist following contact with the physician or in accordance with pharmacy policy, and the contents of the medication cassette. The medication dispensing error rate was calculated by dividing the total number of erroneous doses by the total of filled and omitted doses. Errors were classified into six categories according to type of error; the six error types were taken from the American Society of Hospital Pharmacists:14 unauthorized drug error; incorrect dosage-form error; improper dose error; omission error; incorrect time error; deteriorated drug error. Doses were considered to have been filled at the wrong time if they were dispensed in an incorrect compartment of the medication cassette, e.g. if a dose was mistakenly given in the morning compartment instead of the evening compartment.
RESULTS
From March 2007 to April 2007, 734 unit dose medication cassettes were filled by pharmacy technicians and checked by both pharmacists and nurses. During the study, 179 errors were detected, corresponding to a total of 7249 unit doses filled (n = 7195) and omitted (n = 54) in medication cassettes. The overall dispensing error rate was 2.5%, corresponding to approximately 0.24 dispensing errors detected per medication cassette. At the first step of the error-checking process, pharmacists failed to detect 13.4% (n = 24) of all technicians’ errors when filling prescriptions.
Table 1 indicates the types of dispensing errors detected during the 2-month period. Improper dose errors and omission errors occurred in 57 (31.8%) and 54 (30.2%) of the 179 reported dispensing errors, respectively. Omission errors (n = 51, 32.9%), improper dose errors (n = 44, 28.4%) and incorrect time errors (n = 36, 23.2%) accounted for 84.5% of the 155 EDPs.
Table 1-.
Types of medication-dispensing errors detected by pharmacists and nurses
| Type of error |
|||||||
|---|---|---|---|---|---|---|---|
| unauthorized drug | incorrect dosage-form | improper dose | omission | incorrect time | deteriorated drug | Total | |
| Errors detected by pharmacists (EDPs) | 22 | 0 | 44 | 51 | 36 | 2 | 155 |
| Errors detected by nurses (EDNs) | 5 | 2 | 13 | 3 | 1 | 0 | 24 |
| Total | 27 | 2 | 57 | 54 | 37 | 2 | 179 |
| % (of total errors) | 15.1 | 1.1 | 31.8 | 30.2 | 20.7 | 1.1 | 100 |
Among the 24 EDNs registered, the most common error types were improper dose errors (n = 13, 54.2%) and unauthorized drug errors (n = 5, 20.8%). Examples of improper dose EDNs included prescriptions for amlodipine filled at 10 mg instead of 5 mg, prescriptions for acetylsalicylic acid filled at 500 mg instead of 1000 mg, and prescriptions for acenocoumarol filled at 1 mg instead of 2 mg. Most of the unauthorized drug selections detected by nurses involved drug names that sounded alike or looked alike, or drugs with similar packaging, such as confusion between CORVASAL® 2 mg (molsidomine) and COVERSYL® 2 mg (perindopril). Incorrect dosage-form errors (n = 2, 8.3%) included dispensing of a non-controlled-release formulation of verapamil instead of a controlled-release formulation.
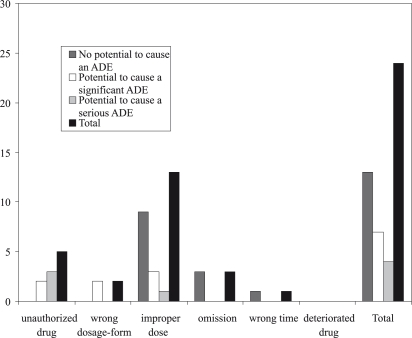
Figure 1 indicates the potential clinical significance of EDNs. Nearly 45% (n = 11) of the EDNs had the potential to induce ADEs if they had not been intercepted; 16.6% (n = 4) could have caused serious ADE and 29.2% (n = 7) could have led to a significant ADE. The most common error types with a potential for serious ADEs were unauthorized drug errors (n = 3). These three occurrences involved the dispensing of 50 mg ketoprofene instead of 10 mg hydrocortisone to a 90-year-old man. The improper dose error that could have led to a serious ADE involved an 86-year-old woman’s prescription for verapamil 40 mg, which was mistakenly filled at a dose of 240 mg.
Figure 1-.
Potential clinical significance of medication dispensing errors detected by nurses
DISCUSSION
An accurate dispensing system helps to prevent and reduce medication errors by minimizing the opportunity for dispensing errors in a pharmacy. In the 1960s, North American hospital pharmacists developed the unit dose system with the goal of reducing medication error rates and drug costs and thus improving the quality of health care.15 Indeed, the unit dose drug dispensing system has a lower medication error rate than the ward stock distribution system.16 We therefore sought to assess the error rate of the unit dose system in our own hospital. Valid meta-analyses regarding medication dispensing errors are extremely difficult to perform because of differences in clinical settings, factors measured, patient populations, and drug dispensing methods. Although the direct observation method utilized here is recognized as an efficient method for detecting medication errors,17 our study results should be interpreted with some caution. First, our study was not designed to completely account for all errors. Second, it relied on human observers, who might have failed to detect some dispensing errors. Consequently, the number of total errors reported here likely underestimates the true overall rate of dispensing errors.
Nevertheless, the results of our study show that a wide range of errors occurred during the filling of medication cassettes. Although similar studies differ from ours in some of the methods and definitions, our results are comparable to theirs. In their analysis of a unit dose drug-dispensing system, Taylor et al.8 and Jornet-Montana et al.9 reported dispensing error rates of 1.7% and 1.0%, respectively; however, they did not evaluate dispensing errors missed by pharmacists. During a 2-week study of dispensing errors identified at the pharmacy’s final check stage, Beso et al.10 found a 2.7% error rate. In a study by Cina et al,11 5 075 pharmacy errors were made out of a total of 140 755 doses filled by pharmacy technicians to an overall pharmacy dispensing error rate of 3.6%. This overall error rate could be broken down into 2.9% due to technicians’ errors when filling prescriptions, which were detected during the pharmacist verification step; and 0.7% due to errors intercepted after the pharmacist verification step.
The dispensing process therefore has inherent risks that require improved procedures for detecting errors. Pharmacy detection of dispensing errors may also provide ongoing benefits by preventing potential ADEs in the medication process. It is essential that the dispensing system involve adequately trained and supervised health professionals, adequate communication, and final checks performed by separate individuals. Clearly, the check performed by pharmacists remains necessary to reduce the occurrence of all dispensing-related ADEs. Recognizing the incidence and types of medication dispensing errors that occur in a central pharmacy allows us to analyze their causes and change the different stages of the process accordingly in order to ensure maximal patient safety. In our study, the most frequent error types were improper dose and omission errors. These findings are consistent with previous studies that indicate that improper dose and omission errors are among the most frequent error types occurring at the dispensing stage.8,18 One possible explanation is that technicians perform an incomplete, incorrect, or rushed reading of the prescription during the filling process. However, most preventable injuries are not due to just one system failure but result from breakdown at several points in the dispensing system. Although causes were not systematically recorded in this 2-month study, the multiplicity of factors contributing to dispensing errors has been reported to include communication failures, working environment, heavy workload, distractions, failure to read the prescription, and complex prescriptions involving several medical orders per patient.19,20 Moreover, errors can arise because of similarities in drug labeling and packaging, as well as similarities in drug names; these similarities may explain unauthorized drug errors, which pose a real threat to patient safety.
Because the clinical implications of medication dispensing errors remain uncertain, preventive strategies to reduce their occurrence should target all stages of the drug delivery process. For example, the central pharmacy at Percy hospital now implements some of the recommendations of the National Coordinating Council for Medication Error Reporting and Prevention21. For example, the noise level was reduced, and the prescription check is performed in a different area from the prescription filling. In order to reduce unauthorized drug errors, incorrect dosage-form errors and deteriorated drug errors, technicians are reminded on a daily basis to perform an attentive reading of dosing instructions. In addition, technicians and pharmacists share information about the errors detected by technicians after the filling process in order to prevent future errors. Finally, to limit dispensing errors due to workload and distractions, an additional pharmacy technician has been hired.
In our study, pharmacists failed to detect approximately 13% of medication selection errors made by technicians. A similar result was found by Facchinetti et al.,22 who showed that pharmacists were more accurate than nurses in checking unit dose medication cassettes; nonetheless, pharmacists failed to detect 100 of the 812 errors (12.3%) artificially introduced into the unit dose distribution system. In the study by Cina et al.,11 20.9% of all technician-filling errors were overlooked by pharmacists during the verification process. It is well known that a dispensing process relying exclusively on repetitive human inspection is subject to human fatigue; the pharmacists may find it difficult to vigilantly check the medication cassettes. Adding a second pharmacist verification step may therefore reduce the number of dispensing errors overlooked by pharmacists. However, an additional verification step may delay the delivery of medication cassettes to the clinical unit. At Percy hospital, the check is currently performed by pharmacists who spend at least one hour per day on the verification process. Several studies23–25 have shown that pharmacy technicians can check medications in a unit dose distribution system without compromising the accuracy. Thus, trained and certified pharmacy technicians could safely and accurately check unit dose medication cassettes filled by other technicians. The results of our study and the major factors contributing to the occurrence of dispensing errors have been explained to the pharmacy technicians. In addition, Percy pharmacists have developed a training program to teach technicians how to reduce errors. Pharmacy technicians now perform the check of unit dose medication cassettes under the supervision of a pharmacist. While it seems evident that if pharmacists miss errors, technicians will as well, but delegating this task to technicians may probably increase their awareness of dispensing errors. Moreover, this delegation should allow pharmacists to spend additional time on clinical activities and thereby contribute to pharmaceutical care.
One of the pharmacist’s missions is to ensure that patients make the best use of medications. This is in accordance with the Institute of Medicine’s recommendations 26, which seek to improve the quality and safety of medication use. The report lays out a blueprint for how pharmacists can become involved in the medicine dispensing process in order to improve it. The pharmacist should also lead collaborative, multidisciplinary efforts to prevent, detect, and resolve medication errors and drug-related problems and to educate patients about their medication. Several studies27,28 have reported a decrease in medication errors after implementing a program to improve clinical pharmacy activity in medical care units.
In our study, poor handwriting may be considered as a major source of error. Ambiguous, incomplete, or confusing prescriptions may lead to poor understanding of fundamental information necessary for correct drug dispensing. Although introducing a computerized physician order entry system can lead to its own types of errors,29 several studies have reported decreases in medication errors with a computerized prescription system.30,31 A computerized prescribing and dispensing system also provides other advantages, since it can be integrated with a program that will analyze the pharmacology of the prescriptions in order to detect errors (e.g. dose errors, contraindications because of other medicines being given to the same patient) and inventory control software. At Percy hospital, the planned implementation of a computerized prescription and dispensing system is expected to decrease the incidence of dispensing errors and increase the chances of intercepting medications errors that do occur. Other new technologies, such as bar-code medication systems32 and automated medication-dispensing systems,13,33 have been shown to reduce pharmacies’ dispensing error rates.
Undetected dispensing errors continue to be an important concern. Even if none of the EDNs identified during our study affected the patients’ health, 16.6% would have caused serious ADEs. Some of these errors, especially unauthorized drug errors, might have threatened patient health if they had not been intercepted. Extrapolating our results to a 1–year period indicates 140 EDNs, 24 of which could cause a serious ADE. Similar to our study, the study of Cina et al.11 assessed the clinical significance of the errors undetected by pharmacists. They found that 23.5% of these errors would have caused ADEs, and 6.8% of these errors would have caused serious or life-threatening ADEs. Although differences in setting and methods make it challenging to compare our study with that of Cina et al., both found the most frequent errors with potential clinical significance to be unauthorized drug errors and improper dose errors. Furthermore, our study found that most errors with significant or serious clinical severity concerned cardiology medication and occurred primarily in elderly patients. These results may reflect the fact that our study was carried out in a cardiovascular department; the results may be different in another clinical department.
Our study emphasized the need for nurses to intercept dispensing errors. Because the check performed by nurses is the last step before drug administration, it must be regarded as a high-risk activity, especially since it has been shown that nurses intercept only approximately 33% of serious medication dispensing errors.34 Following the two-month period of this study, the results were presented to the nursing staff in order to enhance their awareness of dispensing errors, of the potential clinical significance of such errors, and of the usefulness of error reporting. Following the completion of this study, every dispensing error detected and reported by nurses is analyzed by several different specialists. Dispensing errors reported by nurses must be seen by the pharmacy as opportunities to identify areas for improvement. If changes are made to the medication dispensing system, it is important for the pharmacy staff to track the effects of those changes.
Lastly, reducing medication errors will require increased emphasis on education about drug-related iatrogenic disease.35 The teaching and training of health professionals is recognized as an important tool to prevent mistakes and increase patient safety.36 Since 2007, pharmacists at Percy hospital have set up an educational program for nurses and pharmacy technicians, which is part of the hospital’s general policy of quality assurance and risk prevention.37 This one-day educational program is conducted by a pharmacist. Carried out using best practices and actual case studies, the program aims to increase the awareness of nurses and pharmacy technicians about preventing and detecting medication dispensing errors.
CONCLUSIONS
This study increased the awareness of the pharmacy and nursing staffs with regard to the reality and potential severity of medication dispensing errors. Although none of the errors registered during this study reached the patients, the 2.5% error rate indicates a weakness in the unit dose drug-dispensing system. Our hospital plans to improve the dispensing system to reduce errors. Reducing dispensing errors also depends on research into their causes.
REFERENCES
- 1.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: Committee on Quality of Health Care in America, Institute of Medicine, National Academy Press; 1999. [Google Scholar]
- 2. Phillips DP, Christenfeld N, Glynn LM. Increase in US medication-error deaths between 1983 and 1993. Lancet. 1998;351:643–4. doi: 10.1016/S0140-6736(98)24009-8. [DOI] [PubMed] [Google Scholar]
- 3. Ferner RE, Aronson JK. Medication errors, worse than a crime. Lancet. 2000;355:947–8. doi: 10.1016/s0140-6736(00)99025-1. [DOI] [PubMed] [Google Scholar]
- 4. Bates DW, Boyle DL, James Schneider MB, Leape LL. Relationship between medication errors and adverse drug events. J Gen Intern Med. 1995;10:199–205. doi: 10.1007/BF02600255. [DOI] [PubMed] [Google Scholar]
- 5. Kopp BJ, Erstad BL, Allen ME, Theodorou AA, Priestley G. Medication errors and adverse drug events in an intensive care unit: direct observation approach for detection. Crit Care Med. 2006;34:415–25. doi: 10.1097/01.ccm.0000198106.54306.d7. [DOI] [PubMed] [Google Scholar]
- 6. Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events. Implication for prevention. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 7. Lisby M, Nielsen LP, Mainz J. Errors in the medication process: frequency, type, and potential clinical consequences. Int J Qual Health Care. 2005;17:15–22. doi: 10.1093/intqhc/mzi015. [DOI] [PubMed] [Google Scholar]
- 8. Taylor J, Gaucher M. Medication selection errors made by pharmacy technicians in filling unit dose orders. Can J Hosp Pharm. 1986;39:9–12. [PubMed] [Google Scholar]
- 9. Jornet Montana S, Canadell Vilarasa L, Calabuig Muoz M, Riera Sendra G, Vuelta Arce M, Bardaji Ruiz A, et al. Detection and classification of medication errors at Joan XXIII University Hospital. Farm Hosp. 2004;28:90–6. [PubMed] [Google Scholar]
- 10. Beso A, Franklin BD, Barber N. The frequency and potential causes of dispensing errors in a hospital pharmacy. Pharm World Sci. 2005;27:182–90. doi: 10.1007/s11096-004-2270-8. [DOI] [PubMed] [Google Scholar]
- 11. Cina JL, Gandhi TK, Churchill W, Fanikos J, McCrea M, Mitton P, et al. How many hospital pharmacy medication dispensing errors go undetected? Jt Comm J Qual Patient Saf. 2006;32:73–80. doi: 10.1016/s1553-7250(06)32010-7. [DOI] [PubMed] [Google Scholar]
- 12. Rolland P. Occurrence of dispensing errors and efforts to reduce medication errors at the Central Arkansas Veteran’s Healthcare System. Drug Saf. 2004;27:271–82. doi: 10.2165/00002018-200427040-00004. [DOI] [PubMed] [Google Scholar]
- 13. Klein EG, Santora JA, Pascale PM, Kitrenos JG. Medication cart-filling time accuracy, and cost with an automated dispensing system. Am J Hosp Pharm. 1994;51:1193–6. [PubMed] [Google Scholar]
- 14. American society of hospital pharmacists ASHP guidelines on preventing medication errors in hospitals. Am J Hosp Pharm. 1993;50:305–14. [PubMed] [Google Scholar]
- 15. Parker PF. Drug distribution in hospitals. Unit-dose systems reduce error, increase efficiency. Hospitals. 1968;42:65–72. [PubMed] [Google Scholar]
- 16. Taxis K, Dean B, Barber N. Hospital drug distribution systems in the UK and Germany. A study of medication errors. Pharm World Sci. 1999;21:25–31. doi: 10.1023/a:1008616622472. [DOI] [PubMed] [Google Scholar]
- 17. Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm. 2002;59:436–46. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- 18. Anacleto TA, Perini E, Rosa MB, Cesar CC. Drug-dispensing errors in the hospital pharmacy. Clinics. 2007;62:243–50. doi: 10.1590/s1807-59322007000300007. [DOI] [PubMed] [Google Scholar]
- 19. Anacleto TA, Perini E, Rosa MB, Cesar CC. Medication errors and drug-dispensing systems in a hospital pharmacy. Clinics. 2005;60:325–32. doi: 10.1590/s1807-59322005000400011. [DOI] [PubMed] [Google Scholar]
- 20.Cohen MR. Medication errors. 2nd ed. Washington: American Pharmacists Association; 2007. p. 680. [Google Scholar]
- 21.National Coordinating Council for Medication Error Reporting and Prevention. Recommendations to enhance accuracy of dispensing medications. 19992005. Available from http://www.nccmerp.org/council/council1999-03-19.html
- 22. Facchinetti NJ, Campbell GM, Jones DP. Evaluating dispensing error detection rate in a hospital pharmacy. Med Care. 1999;37:39–43. doi: 10.1097/00005650-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 23. Ness JE, Sullivan SD, Stergachis A. Accuracy of technicians and pharmacists in identifying dispensing errors. Am J Hosp Pharm. 1994;51:354–7. [PubMed] [Google Scholar]
- 24. Spooner SH, Emerson PK. Using hospital pharmacy technicians to check unit dose carts. Hosp Pharm. 1994;29:433–7. [PubMed] [Google Scholar]
- 25. Ambrose PJ, Saya FG, Lovett LT, Tan S, Adams DW, Shane R. Evaluating the accuracy of technicians and pharmacists in checking unit dose medication cassettes. Am J Health Syst Pharm. 2002;59:1183–8. doi: 10.1093/ajhp/59.12.1183. [DOI] [PubMed] [Google Scholar]
- 26.Aspden P, Wollcott J, Bootman JL, Cronenwett LR, editors. Committee on Identifying and Preventing Medication Errors. Preventing medication errors. Institute of Medicine. Whasington, DC: National Academy Press; 2007. p. 393. [Google Scholar]
- 27. Scarsi KK, Fotis MA, Noskin GA. Pharmacist participation in medical rounds reduces medication errors. Am J Health Syst Pharm. 2002;59:2089–92. doi: 10.1093/ajhp/59.21.2089. [DOI] [PubMed] [Google Scholar]
- 28. Bond Ca, Rahel C, Franke T. Medication errors in United States hospitals. Pharmacotherapy. 2001;21:1023–36. doi: 10.1592/phco.21.13.1023.34617. [DOI] [PubMed] [Google Scholar]
- 29. Weant KA, Cook AM, Armitstead JA. Medication-error reporting and pharmacy resident experience during implementation of computerized prescriber order entry. Am J Health Syst Pharm. 2007;64:526–30. doi: 10.2146/ajhp060001. [DOI] [PubMed] [Google Scholar]
- 30. Fontan JE, Maneglier V, Nguyen VX, Loirat C, Brion F. Medication errors in hospitals: computerized unit dose drug dispensing system versus ward stock distribution system. Pharm World Sci. 2003;25:112–7. doi: 10.1023/a:1024053514359. [DOI] [PubMed] [Google Scholar]
- 31. Mirco A, Campos L, Falcao F, Nunes JS, Aleixo A. Medication errors in an internal medicine department. Evaluation of a computerized prescription system. Pharm World Sci. 2005;27:351–2. doi: 10.1007/s11096-005-2452-z. [DOI] [PubMed] [Google Scholar]
- 32. Poon EG, Cina JL, Churchill W, Patel N, Featherstone E, Rothschild JM, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar code technology in the pharmacy. Ann Intern Med. 2006;145:426–34. doi: 10.7326/0003-4819-145-6-200609190-00006. [DOI] [PubMed] [Google Scholar]
- 33. Scott O, Caldwell R. Dispensing error rate after implementation of an automated pharmacy caroussel system. Am J Health Syst Pharm. 2007;64:1427–31. doi: 10.2146/ajhp060313. [DOI] [PubMed] [Google Scholar]
- 34. Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T, et al. Systems analysis of adverse drug events. JAMA. 1995;274:35–43. [PubMed] [Google Scholar]
- 35. Desselle SP. Certified pharmacy technicians’ views on their medication preparation errors and educational needs. Am J Health-Syst Pharm. 2005;62:1992–7. doi: 10.2146/ajhp040549. [DOI] [PubMed] [Google Scholar]
- 36. Navaneethan S, Venkatesh S, Nannapaneni S, Shrivastava R. Educational intervention: a tool for decreasing medication errors. Int J Qual Health Care. 2005;17:83. doi: 10.1093/intqhc/mzi009. [DOI] [PubMed] [Google Scholar]
- 37.Mullot H, Simon L, Cannonge B, Lefeuvre L, Bohand X.Challenging drug iatrogenic disease and iatrogenic risk : a military hospital experience of a program training for nurses J Pharm Belg 20086343–50.[in press] [Google Scholar]