Abstract
The study investigated the power of theoretically derived cognitive variables to predict posttraumatic stress disorder (PTSD), travel phobia, and depression following injury in a motor vehicle accident (MVA). MVA survivors (N = 147) were assessed at the emergency department on the day of their accident and 2 weeks, 1 month, 3 months, and 6 months later. Diagnoses were established with the Structured Clinical Interview for DSM–IV. Predictors included initial symptom severities; variables established as predictors of PTSD in E. J. Ozer, S. R. Best, T. L. Lipsey, and D. S. Weiss's (2003) meta-analysis; and variables derived from cognitive models of PTSD, phobia, and depression. Results of nonparametric multiple regression analyses showed that the cognitive variables predicted subsequent PTSD and depression severities over and above what could be predicted from initial symptom levels. They also showed greater predictive power than the established predictors, although the latter showed similar effect sizes as in the meta-analysis. In addition, the predictors derived from cognitive models of PTSD and depression were disorder-specific. The results support the role of cognitive factors in the maintenance of emotional disorders following trauma.
Keywords: posttraumatic stress disorder, depression, travel phobia, motor vehicle accidents, cognition
Traumatic experiences are common in the general population, but only a minority of survivors develop chronic emotional problems, such as posttraumatic stress disorder (PTSD; e.g., Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). For those individuals who develop PTSD, the condition can be highly persistent and disabling (Norris, 1992). Several authors have emphasized the need to identify factors that predict who will develop PTSD following traumatic events, and initial studies have identified some candidate variables (for reviews, see Blanchard & Hickling, 2004; Brewin, Andrews, & Valentine, 2000). A recent meta-analysis identified the following variables as the best established predictors of PTSD: prior trauma, prior psychological adjustment, family history of psychopathology, perceived life threat during the trauma, posttrauma social support, peritraumatic emotional response, and peritraumatic dissociation (Ozer, Best, Lipsey, & Weiss, 2003). The present study aimed to extend this research by (a) considering other trauma-related emotional disorders in addition to PTSD and (b) examining the predictive power of theory-derived cognitive variables.
The Prediction of Emotional Disorders Following Trauma
Past research on predictors of psychological problems following trauma has mainly focused on PTSD. There is, however, evidence that other emotional disorders are also common after traumatic experiences, including depression, other anxiety disorders, and substance use disorders (e.g., Blanchard et al., 2004; Mayou, Bryant, & Ehlers, 2001; O'Donnell, Creamer, Pattison, & Atkin, 2004). To date, studies have mainly investigated these other disorders as comorbid diagnoses of PTSD and found that comorbidity may be the norm rather than an exception (for a review, see Brady, Killeen, Brewerton, & Lucerini, 2000). However, there is also evidence that some survivors develop only a mood, substance use, or other anxiety disorder after trauma but not PTSD (Mayou et al., 2001; O'Donnell, Creamer, Pattison, & Atkin, 2004). Few studies to date have investigated risk factors for these disorders following trauma or tested what factors predict which of the different psychological problems trauma survivors will develop. The results of the existing studies have been inconsistent (Mayou et al., 2001; McFarlane, Atchison, & Yehuda, 1997; O'Donnell, Creamer, & Pattison, 2004; Shalev et al., 1998).
When one is searching for factors that differentially predict the development and maintenance of different emotional problems following trauma, cognitive theories of emotional disorders may offer a useful starting point. These theories postulate content specificity (e.g., Beck, Rush, Shaw, & Emery, 1979; Clark, 1999)—that is, each emotional disorder is thought to be characterized by different cognitive themes and biases. Cognitive models might therefore possess a greater potential to differentially predict psychological disorders than other models suggested in the literature that do not assume such specificity. In line with this idea, a cross-sectional study of motor vehicle accident (MVA) survivors found preliminary evidence that theory-derived cognitive predictors differentially predict PTSD, travel phobias, and depression (Ehring, Ehlers, & Glucksman, 2006). The cognitive variables derived from each disorder-specific model explained significantly greater proportions of the variance of the respective symptom severities than cognitive variables derived from the models of the other disorders. However, the interpretation of the findings is limited by the cross-sectional nature of the study, which only allowed a prediction in a statistical sense. The present prospective longitudinal study aimed to test whether theory-derived cognitive variables allow a temporal prediction of subsequent PTSD, travel phobia, and depression following trauma.
Cognitive–Behavioral Models of PTSD, Phobias, and Depression
Several disorder-specific cognitive models have been developed to explain the disorders under investigation (for reviews, see Clark, 1999; Ingram, Miranda, & Segal, 1998; Salkovskis, 1996). In the following, we summarize the models on which the present study was based.
Cognitive predictors for PTSD were derived from Ehlers and Clark's (2000) model. The authors postulated that people with PTSD perceive a current threat, which has two sources: (a) the nature of the trauma memory, and (b) problematic appraisals of the trauma and/or its aftermath. The memory for the traumatic event is thought to be poorly elaborated and poorly integrated into the autobiographical memory base. Together with other trauma memory characteristics (strong perceptual priming and strong conditioned associations), the poor elaboration is thought to lead to an insufficient inhibition and easy triggering of involuntary memories that lack awareness of the self in the past and other relevant context information. The nature of the trauma memory is thought to be the result of problematic cognitive processing during the trauma, especially a predominance of data-driven processing (i.e., predominant processing of the sensory impressions, as opposed to processing of the meaning of the situation) and a lack of self-referential processing (i.e., insufficient linking of the event to knowledge of the self), both of which overlap, in part, with dissociation (Halligan, Michael, Clark, & Ehlers, 2003). PTSD is thought to be maintained by a range of cognitive and behavioral strategies that the individual uses to control the current threat. These include thought suppression, rumination, avoidance, and safety behaviors (i.e., excessive precautions). Several cross-sectional and prospective longitudinal studies following different types of traumatic events found significant relationships between the cognitive factors specified by Ehlers and Clark (2000) and PTSD (Clohessy & Ehlers, 1999; Dunmore, Clark, & Ehlers, 1999, 2001; Ehlers, Mayou, & Bryant, 1998; Halligan et al., 2003; Laposa & Alden, 2003; Murray, Ehlers, & Mayou, 2002). There is also initial evidence that the theory-derived cognitive variables significantly improve the prediction of PTSD symptom severity over and above initial symptom severity and risk factors identified in earlier research (Dunmore et al., 2001; Ehlers et al., 1998; Ehring et al., 2006; Halligan et al., 2003).
Predictors for travel phobia were derived from a generic cognitive–behavioral conceptualization of specific phobias, which stresses the importance of threat-related appraisals concerning the feared stimulus. These are thought to be maintained by avoidance and safety behaviors that the individual uses to prevent or minimize the predicted feared outcome (Beck, Emery, & Greenberg, 1985; Clark, 1999; Salkovskis, 1996). In the case of travel phobia, for example, people may give up traveling or may only travel when using safety behaviors, such as looking in the mirror frequently or driving excessively slowly. In line with this view, earlier studies have found that individuals with travel phobia endorse negative beliefs about the dangerousness of travel and the anxiety/panic symptoms that they may experience in travel situations and that they employ safety behaviors (Ehlers, Hofmann, Herda, & Roth, 1994; Ehlers et al., 2007; Ehring et al., 2006; J. E. Taylor, Deane, & Podd, 2000). According to conditioning accounts of phobias, high fear during the accident is thought to lead to strong conditioned fear responses and therefore expected to predict travel phobias (S. Taylor & Koch, 1995). Ehring et al. (2006) and Mayou et al. (2001) found that fear during the accident indeed predicted travel phobia. With the exception of Mayou et al. (2001), prospective longitudinal studies of travel phobia after MVA are largely lacking.
Predictors of major depression were derived from cognitive conceptualizations of the disorder (for a review, see Ingram et al., 1998). At the core of these models lies the hypothesis that depression is caused by the interaction of cognitive vulnerability factors and matching stressors. According to this view, depressogenic cognitive patterns are activated when vulnerable individuals encounter stressful situations and/or experience a decline in mood. Typical examples of these cognitive patterns are a tendency to develop negative and self-devaluative thoughts (Ingram et al., 1998), depressive rumination (Nolen-Hoeksema & Morrow, 1991), and the activation of depressogenic schematic models, which result in a feeling tone of sad mood that reflects self-devaluative thinking (Teasdale & Barnard, 1993). Very few studies to date have tested cognitive conceptualizations of major depression following trauma, possibly because in treatment studies trauma survivors rarely present with depression alone. However, prospective studies have shown that some survivors develop trauma-related depression without PTSD (Mayou et al., 2001; O'Donnell, Creamer, Pattison, & Atkin, 2004). Ehring et al.'s (2006) cross-sectional study found preliminary evidence for the role of self-devaluative thoughts and rumination in trauma-related depression, and Nolen-Hoeksema and Morrow (1991) found that depressive rumination prior to a natural disaster predicted subsequent depression.
Aims and Hypotheses
The aim of the study was to investigate the power of disorder-specific cognitive models in predicting PTSD, travel phobias, and depression following MVA, using a prospective longitudinal design. Predictor variables were assessed on the day of the accident and 2 weeks after the MVA. Outcome measures were assessed at 2 weeks, 1 month, 3 months, and 6 months following the event. It was expected that (a) variables derived from specific cognitive–behavioral models would be more powerful in predicting the severity of PTSD, phobias, and depression than established predictors of posttraumatic stress symptoms identified in the recent meta-analysis by Ozer et al. (2003); (b) the different sets of cognitive predictors would be disorder-specific in that the symptom severity of each disorder would be best accounted for by its specific model; and (c) the cognitive predictors would improve the prediction of long-term outcome above what could be predicted from initial symptom levels.
Method
Participants
Sample description
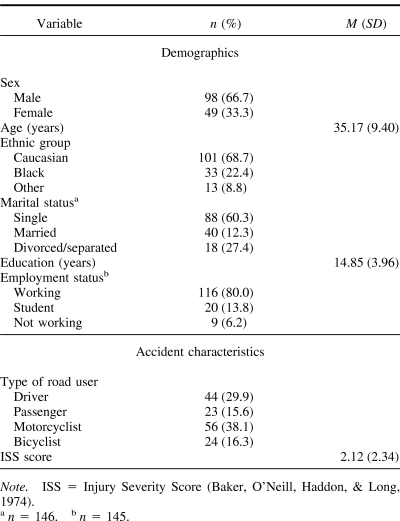
The sample comprised 147 injured MVA survivors. Participants were recruited over a period of 19 months from the emergency department of a large urban teaching hospital. Inclusion criteria were as follows: injury in an MVA as a driver, passenger, motorcyclist, or cyclist; injuries more severe than triage category “blue” (very mild injuries); age between 18 and 65 years; and address in local catchment area. Exclusion criteria were as follows: left before receiving medical treatment; attended the emergency department more than 12 hr after the accident; currently psychotic or suicidal; command of English was insufficient to complete interviews. Table 1 shows demographic and accident characteristics. The study sample did not significantly differ from a random sample of MVA admissions at the same hospital (N = 223) in terms of sex (67% vs. 61% male), χ2(1, N = 368), p = .32; ethnic background (69% vs. 61% Caucasian), χ2(1, N = 370), p = .22; or injury severity scores (M = 2.12, SD = 2.34, vs. M = 1.88, SD = 2.27), t(288) = −0.89, p = .38. There was a marginally significant difference for age, t(328.63) = −1.97, p = .05; participants were, on average, 2 years older than the random sample of MVA survivors (M = 35.17, SD = 9.40, vs. M = 33.11, SD = 10.37).
Table 1. Demographic and Accident Characteristics.
Recruitment
First contact with participants was established in two ways: First, a researcher approached 115 MVA survivors at the emergency department within hours after their MVA. Of the 74 survivors who were initially interested, 21 did not proceed, and 53 (72%) participated. Second, MVA survivors who attended the emergency department outside the hours when recruitment staff were present received an invitation letter and an information sheet in the mail between 1 and 5 days following their accident. Two days later, a researcher contacted these individuals via the telephone to establish whether they were interested and eligible to take part in the study. Of the 269 individuals who were contacted, 20 were excluded as they did not meet inclusion criteria, and 123 declined. Of the 130 MVA survivors who were initially interested in the study, 36 did not proceed, and 94 (72%) participated. The two recruitment methods yielded identical results (e.g., yielded similar patterns of correlations with the outcome measures), and the results are therefore presented for the full sample of 147 participants. Data from the follow-up assessment at 6 months were available for 141 (96%) participants.
Outcome Measures
Diagnostic interviews
The presence of PTSD, travel phobia, and major depressive disorder was assessed with the Structured Clinical Interview for DSM–IV (SCID; First, Spitzer, Gibbon, & Williams, 1996). At the 2-week assessment, the presence of PTSD Symptom Criteria A to D and F was assessed, as the Duration Criterion E was not fulfilled yet. For a diagnosis of travel phobia, participants had to meet Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) criteria for a specific phobia, with the phobic situation being one or more travel situations (i.e., driving a car, being a passenger in a car or on a bus, riding a motorbike or a bicycle). However, Criterion G (symptoms are not better accounted for by PTSD) was not used for the present analyses. The DSM–IV is inconsistent in that it allows comorbid diagnoses of PTSD and depression but not of PTSD and travel phobia. Determining whether participants met criteria for travel phobia, regardless of whether they also had PTSD, made it possible to (a) relate the degree of phobic symptoms to the predictor variables and (b) examine the overlap between symptoms of PTSD and travel phobia in our sample, especially the percentage of participants with PTSD who also met full criteria for travel phobia when the hierarchy rule was not applied. Interrater reliability for the SCID interviews was high (PTSD: κ = .82; specific phobia: κ = .85; major depression: κ = 1; n = 56 randomly chosen interviews from this and a related study; two raters). The SCID manual states that kappas above .70 indicate good reliability (First et al., 1996).
Self-report scales
Each of the psychological outcomes was assessed with standardized self-report measures: the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997; α = .93–.95), a validated and widely used self-report measure of PTSD symptom severity; the Beck Depression Inventory (BDI; Beck et al., 1979; α = .90–.95), a standardized questionnaire of established reliability and validity to assess the severity of depressive symptoms; and the Travel Phobia Questionnaire (TPQ; Ehring et al., 2006; α = .94–.96), a measure of the severity of travel phobia. The TPQ closely follows DSM–IV criteria for specific phobia and comprises 12 items about the participant's fear in travel situations, items related to the DSM–IV criteria of insight and interference, and the degree of avoidance related to travel. Ehring et al. (2006) reported that the TPQ showed good internal consistency, retest reliability, agreement with SCID assessments of phobia, and predictive validity.
Established Predictors From Ozer et al.'s (2003) Meta-Analysis
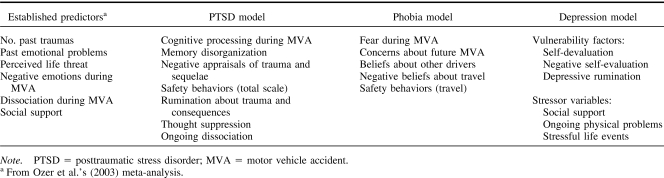
Table 2 gives an overview of the predictor variables. Self-report questionnaires and semistructured interviews assessed six predictors identified in Ozer et al.'s (2003) meta-analysis. For practical reasons, one of the predictors from the meta-analysis, namely family history of psychopathology, could not be assessed in this study. This variable showed the lowest effect size in the meta-analysis and generally has not been found to predict PTSD following MVA (Blanchard & Hickling, 2004).
Table 2. Sets of Predictor Variables.
Number of past traumas
The Trauma History Interview determined the number of traumatic events fulfilling the DSM–IV stressor criteria that participants had experienced before the MVA. It was based on similar trauma checklists (Blake et al., 1995; Foa et al., 1997).
Past emotional problems
The SCID assessed whether participants had a history of past major depression, PTSD, or travel phobia. In addition, participants reported whether they had had any past treatment for emotional problems or substance abuse.
Perceived life threat during the accident
Participants rated, on a scale from 0 (not at all) to 4 (very strongly), how much they had believed they were going to die during the accident.
Negative emotions during the MVA
The Peritraumatic Emotions Questionnaire (Evans, Ehlers, Mezey, & Clark, 2007; Halligan et al., 2003; α = .89) asks participants to rate the extent to which they experienced each of 15 negative emotions during the accident and until help arrived. This questionnaire has been shown to have good internal consistency and to predict PTSD symptoms after assault (Evans et al., 2007; Halligan et al., 2003).
Dissociation during the MVA
The State Dissociation Questionnaire (SDQ; Murray et al., 2002; α = .90) is a nine-item scale assessing different aspects of dissociation, such as derealization, depersonalization, detachment, altered time sense, emotional numbing, and reduction of awareness in surroundings. The SDQ has shown good reliability and validity in traumatized and nontraumatized samples (e.g., Ehring et al., 2006; Halligan et al., 2003; Murray et al., 2002). It correlates strongly with the Peritraumatic Dissociation Scale (Marmar, Weiss, & Metzler, 1997).
Social support after the MVA
The Crisis Support Scale (Joseph, 1999; seven items; α = .76) is a widely used measure of social support in PTSD research. One item about personal contact with other trauma survivors was omitted from the scale, as it did not appear applicable to all MVA survivors. Instead, two items about informational support (“Did people give you advice and helpful information?”) and companionship support (“Did people invite you to participate in social or leisure activities?”) were included.
Cognitive Predictors of PTSD
Seven variables derived from Ehlers and Clark's (2000) cognitive model of PTSD were assessed.
Cognitive processing during the MVA
The Cognitive Processing Questionnaire (Halligan, Clark, & Ehlers, 2002; Halligan et al., 2003) measures three aspects of cognitive processing during the trauma, namely data-driven processing (eight items; e.g., “My mind was fully occupied with what I felt, saw, heard and smelled”), lack of self-referential processing (eight items; e.g., “I felt as if the accident was happening to someone else”), and dissociation (nine items; see the description of the SDQ above). The questionnaire was developed in a series of studies (Halligan et al., 2002, 2003; Murray et al., 2002) and showed good reliability and validity in predicting intrusive memories and PTSD. The sum score of all 25 items was used in this study (α = .95).
Memory disorganization
The Trauma Memory Questionnaire (Halligan et al., 2003) asks participants to describe the quality of their trauma memories. The Disorganization subscale consists of five items that assess deficits in intentional recall (e.g., “I cannot get what happened during the accident straight in my mind”). The measure demonstrated good reliability and validity in earlier studies (Evans et al., 2007; Halligan et al., 2002, 2003). The internal consistency in this study was .91.
Negative appraisals of the trauma and its sequelae
These were assessed with the Negative Thoughts About the Self subscale of the Posttraumatic Cognitions Inventory (Foa, Ehlers, Clark, Tolin, & Orsillo, 1999; 21 items; α = .94). The scale has been shown to have good reliability and convergent validity and to discriminate between traumatized people with and without PTSD (Foa et al., 1999). It includes items that measure negative interpretations of the initial PTSD symptoms (Dunmore et al., 2001; Ehlers et al., 1998; Ehlers & Steil, 1995).
Safety behaviors (i.e., excessive precautions)
The Safety Behaviors Questionnaire assesses excessive precautions related to travel (14 items; e.g., “I keep checking the position of other traffic”; α = .94) as well as generalized safety behaviors (10 items; e.g., “I check carefully whether doors/windows are locked”; α = .86). The total score is the sum of all 24 items (α = .94). It was developed over a series of studies (Dunmore et al., 1999, 2001; Ehring et al., 2006) and has shown good internal consistencies and correlations with PTSD severity.
Rumination and thought suppression
The Responses to Intrusions Questionnaire assesses aspects of trauma survivors' responses to intrusive memories, namely rumination about the trauma and/or its consequences (eight items; e.g., “I think about why the event happened to me”; α = .86), and thought suppression (six items; e.g., “I try to push them out of my mind:; α = .92). It was developed in a series of studies (Clohessy & Ehlers, 1999; Ehlers et al., 1998; Halligan et al., 2003; Murray et al., 2002) and has shown good reliability and predictive validity.
Ongoing dissociation
Dissociation at the time of assessment was assessed with the Current Dissociation subscale of the SDQ (Murray et al., 2002). Participants were asked to rate the items regarding how they had felt during the preceding week (α = .94).
Cognitive Predictors of Travel Phobia
Five potential predictors of travel phobia following MVA were assessed.
Fear during the accident
Fear was assessed with five items of the Peritraumatic Emotions Questionnaire (Halligan et al., 2003) described above (terrified, alarmed, frozen, fearful, and shocked; α = .84).
Negative beliefs related to travel
Concerns about future accidents (four items; e.g., “I will be injured in an accident”; α = .75) and negative beliefs about travel (nine items; e.g., “Now I have had one accident, I am more likely to have another one” and “If I am anxious in traffic, this shows that I must be in danger”; α = .75) were assessed with the Travel Phobia Beliefs Questionnaire (Ehring et al., 2006). Negative beliefs about other drivers were assessed with an adapted version of the Other Drivers subscale of the Motor Vehicle Accident Scale (Fedoroff, Taylor, Asmundson, & Koch, 2000; nine items; α = .82).
Safety behaviors while traveling
These were assessed with the Travel subscale of the Safety Behaviors Questionnaire described above.
Cognitive Predictors of Depression
Six variables representing the cognitive vulnerability–stress model of depression were assessed.
Self-devaluation
The Depressed States Checklist (Teasdale & Cox, 2001) asked participants to describe how they had felt when their mood started to deteriorate during the preceding month by rating 28 adjectives on a scale from 0 (not at all) to 4 (extremely). The scale is based on Teasdale and Barnard's (1993) interactive cognitive subsystems theory. Relevant to this study was the sum of the 14 adjectives that imply self-devaluation (e.g., unacceptable, rejected, unwanted, worthless; α = .95). A second measure of self-devaluation was the Negative Self-Evaluation subscale of the Leiden Inventory of Depression Sensitivity (Van der Does, 2002; eight items; e.g., “When in a sad mood, I think that fewer people value me”; α = .87). This measure assesses cognitive reactivity to sad mood.
Depressive rumination
The 10-item short version of the Response Style Questionnaire (Nolen-Hoeksema & Morrow, 1991; α = .89), a well-validated measure of depressive rumination, was used.
Social support
This was measured with the Crisis Support Scale described above.
Severity of ongoing physical problem
Participants rated the extent to which they still suffered from ongoing physical problems from the MVA on a scale from 0 (not at all severe) to 10 (very severe).
Stressful life events
The Stressful Life Events Interview was developed for this project on the basis of similar instruments (see Wethington, Brown, & Kessler, 1997) to assess stressful life events that participants had experienced within the past year. It probes for the domains of family, friends, social life, work, health, legal problems, finances, accommodation, and other events, and it asks participants to name relevant events within each domain and rate the distress caused by each event on a scale from 0 (not at all distressing) to 100 (very distressing). The total number of stressful life events with a minimum distress rating of 50 was used for the analysis.
Additional measures
Demographics and characteristics of the accident were assessed via a self-report questionnaire. A trained nurse specializing in emergency medicine coded the severity of the participant's injuries using the Injury Severity Score (Baker, O'Neill, Haddon, & Long, 1974).
Procedure
The study was approved by the local research ethics committees, and participants gave written informed consent. Participants received £50 as reimbursement for their time and travel expenses. They were recruited and first tested at the emergency department on the day of their accident or recruited via telephone within the 1st week following their MVA. Participants attended a 2-hr session 2 weeks after the accident (M = 14 days, SD = 4.2). The session took place at the research department (n = 95), at the participant's home (n = 35), in the hospital ward (for 6 participants who were still hospitalized), or via telephone if no session could be arranged (n = 11). The session included the completion of questionnaires assessing predictor variables and symptom severities (PDS, BDI, TPQ) as well as the SCID. In addition, experimental tasks were carried out that will be reported elsewhere. Participants were then sent follow-up questionnaires assessing outcome variables (PDS, BDI, TPQ) at 1 month, 3 months, and 6 months following the accident. In addition, the 6-month follow-up involved a telephone interview with the same interviewer who had conducted the research session at 2 weeks, including the SCID and the Stressful Life Events Interview.
Data Analyses
Spearman's rank correlation coefficients (Spearman's rho) tested the associations between the continuous predictor variables and symptom severity measures, because many variables were skewed. Rank biserial correlation coefficients were computed for dichotomous predictor variables (Willson, 1976).
Preanalysis screening tests showed that parametric regressions were inappropriate, as the assumptions regarding the normality of residuals and homoscedasticity were violated and could not be corrected by transformations of the variables. Therefore, nonparametric regression analyses were conducted via a generalized linear models analysis with cases bootstrapping, as implemented in Stata Version 8.1 (StataCorp, 2003). Bootstrapping is an approach for estimating standard errors in regression analyses that does not make any distributional assumptions (Chernick, 1999). This involves repeatedly resampling the sample with replacement to approximate what would happen if the population were sampled. The number of bootstrap samples drawn for each analysis was set to 1,999. We decided to use a data analytic approach that allowed us to simultaneously include information on the dependent variables from all time points (overall analyses) while controlling for the clustered data structure (i.e., the fact that several observations of the same individual were included). Symptom severity scores from all time points were considered simultaneously as the dependent variable in this analysis, whereby the correlation structure was maintained by resampling within subject clusters—the cluster(subject) option as implemented in Stata. It has been suggested that this approach is superior to analyzing only the last assessment point (endpoint analyses) or conducting a time-by-time analysis for each assessment point separately, as both options result in loss of information (Everitt, 1998).
The predictive powers of the different sets of predictor variables were compared with the Bayesian information criterion (BIC) derived for each regression model. BIC is an index of the goodness of fit of the prediction model, with low scores (which can be negative) indicating a better fit. As differences between BICs cannot be statistically tested, differences in the magnitude of BICs were interpreted. As previous studies mainly used endpoint analyses, we also conducted parallel analyses predicting symptom severity measures at the 6-month follow-up only. These gave the same results as the more comprehensive overall analyses (details of these results are published as online supplemental material).
Calculating statistical power for regression models with clustered data structures is complex, and no standard procedure to establish the optimal sample size for this type of analysis has been developed to date (Cohen, Cohen, West, & Aiken, 2003). However, the number of participants in our sample (i.e., the higher level sample size for the clustered regression analysis) lies well above the minimum number of 100 suggested by Hox (1995). In addition, one can approximate the power for our analyses by establishing the power for parallel parametric analyses. According to Green's (1991) formula, 44 participants are required to test a multiple correlation of a large effect size (as found in the earlier study by Ehring et al., 2006) with seven predictor variables and a power of .80 (α = .05), whereas 103 participants are required to test a medium effect size.
As sex differences in PTSD prevalence have consistently been identified in the literature (Tolin & Foa, 2006), we conducted all analyses separately for male and female participants. The pattern of results was the same for both sexes, and the article therefore presents the analyses for the whole sample.
Results
PTSD, Phobia, and Depression
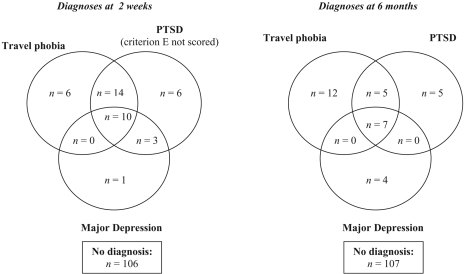
Results of the SCID assessment at 2 weeks showed that 33 of the 147 participants (22.4%) met criteria for PTSD when Criterion E (duration for at least 1 month) was not applied. In addition, 3 participants (2%) met criteria for PTSD related to a different event but did not meet full PTSD criteria in relation to the MVA. These participants were included in the PTSD group for the present analyses. Excluding them did not change the results. Thirty participants (20.4%) met criteria for travel phobia at 2 weeks, and 14 (9.6%) met criteria for a current major depressive episode. At the 6-month follow-up, 17 of the 141 participants (12.1%) met criteria for PTSD related to the accident, 25 (17.7%) met criteria for travel phobia, and 11 (7.8%) met criteria for a current major depressive episode. As shown in Figure 1, there was substantial comorbidity between the disorders at both assessments.
Figure 1. Distribution of psychological disorders at the 2-week and 6-month follow-ups, as determined by the Structured Clinical Interview for DSM–IV. PTSD = posttraumatic stress disorder.
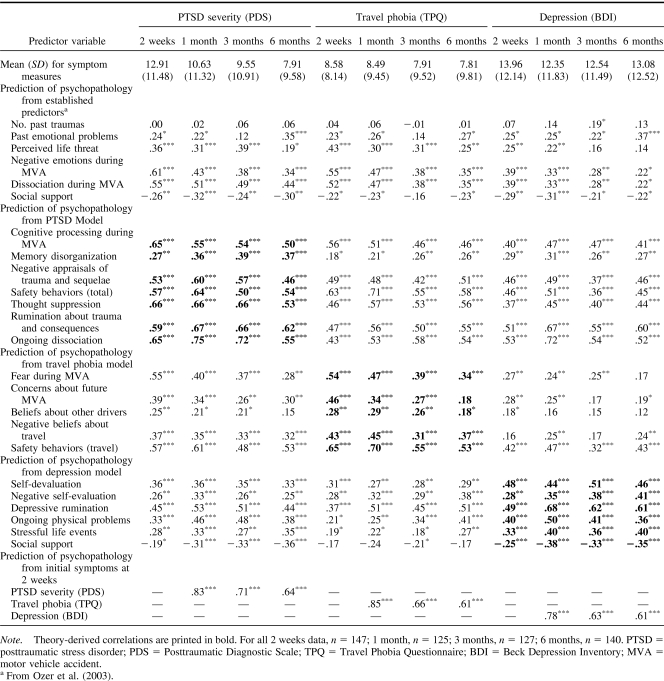
Participants showed, on average, moderate symptom levels of PTSD and travel phobia as well as mild levels of depression (see Table 3). Mean PDS scores decreased significantly during the course of the study, F(3, 342) = 15.18, p < .001. In contrast, no significant change over time was found for symptom levels of travel phobia, F(3, 312) = 0.27, p = .85, or depression, F(3, 315) = 1.54, p = .21.
Table 3. Zero-Order Correlations (Spearman's Rho) Between Predictor Variables and Symptom Severities.
Relationship Between Accident Characteristics and Symptom Severities
Injury severity as assessed with the Injury Severity Score was not significantly correlated with PTSD or depressive symptom severity at any assessment (|ρ| < .15, ps > .12). However, significant negative correlations between injury severity and symptom levels of travel phobia were found at 2 weeks (ρ = −.21, p < .05) and 1 month (ρ = −.23, p < .05), and greater injury severity was related to lower fear and avoidance of travel. This finding might have been influenced by the fact that most of the participants with severe injuries had not traveled since the MVA at these assessments (53.1% of all participants at 2 weeks and 37.9% of all participants at 1 month).
Kruskal–Wallis one-way analyses of variance showed an effect of type of road usage during the accident (i.e., drivers, motorcyclists, bicyclists, or passengers) on symptom levels for most measures, χ2s(3) > 8, ps < .05, with the exception of BDI scores at 2 weeks, χ2(3, N = 126) = 6.20, p = .11, and TPQ scores at 6 months, χ2(3, N = 127) = 2.80, p = .42. Follow-up Mann–Whitney tests were conducted for pairwise comparisons. Results showed that both drivers and passengers showed significantly higher symptom levels than motorcyclists and bicyclists. No other differences were significant.
Comparison of Established and Theory-Derived Cognitive Predictors
Table 3 shows the zero-order correlations between the predictor variables and PTSD, phobia, and depression severities. The established predictors derived from Ozer et al.'s (2003) meta-analysis showed small to moderate correlations with the psychological outcomes. An exception was that the number of past traumas was only significantly correlated with symptom levels of depression at the 3-month follow-up, not with any other outcome measure. All theory-derived cognitive variables correlated moderately to highly with the respective psychological outcome at most assessments.
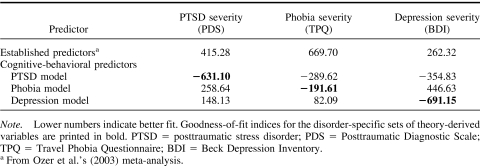
The results of the nonparametric regression analyses that included outcome data from all time points are summarized in Table 4 (detailed results are published online as supplemental material). The theory-derived regression models were better at predicting each of the disorders than the set of established predictors from the meta-analysis, as indicated by lower values of the BIC.
Table 4. Goodness-of-Fit Indexes (Bayesian Information Criteria) From Regression Analyses.
Specificity of Cognitive Models
If cognitive–behavioral models are specific, then each disorder should be best explained by its disorder-specific model. As shown in Table 4, the PTSD model yielded a much smaller BIC (i.e., a better fit) in predicting PTSD symptom severity than the phobia and depression models. Similarly, the depression model showed the best model fit in predicting depression, compared to the PTSD and travel phobia models. However, in contrast to the hypotheses, the PTSD model showed the best model fit in the prediction of phobic symptom severities, followed by the phobia model.
Prediction Beyond Initial Symptom Levels
As shown in Table 3, initial symptom levels at 2 weeks predicted subsequent symptoms levels for all disorders. This raises the question of whether the other predictors predicted symptom severity levels at the 6-month follow-up beyond what could be predicted from initial symptom levels. For each outcome measure, we therefore compared the BIC for three regression analyses with the following predictor variables: (a) symptom levels at 2 weeks only, (b) symptom levels at 2 weeks plus the established predictors from the meta-analysis, and (c) symptom levels at 2 weeks plus the variables from the disorder-specific cognitive model.
PDS scores at 2 weeks significantly predicted PDS scores at 6 months (incidence rate ratio [IRR] = 1.06, p < .001; BIC = 139.43). Adding the variables from the meta-analysis led to little change in the goodness of fit (BIC = 105.14). In contrast, the model fit parameter improved considerably when the variables from the PTSD model were included (BIC = −1.56). This compares to a BIC of 73.58 when only the theory-derived variables were included in the endpoint analysis predicting PTSD severity at 6 months. Similarly, BDI scores at 2 weeks significantly predicted BDI scores at 6 months (IRR = 1.07, p < .001; BIC = 354.23). Adding the variables from the meta-analysis improved the model fit to BIC = 212.67. The best prediction was achieved when BDI scores at 2 weeks were combined with the variables from the cognitive depression model (BIC = 36.60) or when depression at 6 months was predicted on the basis of theory-derived variables alone (BIC = 37.40). Finally, travel phobia symptoms at 2 weeks significantly predicted phobia symptoms at 6 months (IRR = 1.04, p < .001; BIC = 399.29). However, adding either the established predictors (BIC = 355.09) or the variables from the travel phobia model (BIC = 344.76) contributed little change in model fit. The BIC for the theory-derived predictors alone was 407.47.
Discussion
This prospective longitudinal study aimed to investigate the power of disorder-specific cognitive–behavioral models in predicting PTSD, travel phobias, and depression following injury in an MVA. In line with previous studies (e.g., Blanchard et al., 2004; Ehring et al., 2006; Mayou et al., 2001; O'Donnell, Creamer, Pattison, & Atkin, 2004; Shalev et al., 1998), a substantial minority of participants developed PTSD, travel phobias, and/or depression. As expected, the three psychological outcomes were predicted by (a) initial symptom severities, (b) a set of established predictors of PTSD identified in a recent meta-analysis (Ozer et al., 2003), and (c) three sets of predictors derived from specific cognitive–behavioral models of the disorders. Nonparametric regression analyses compared the relative power of the sets of predictors in predicting each of the disorders. In line with the hypotheses, symptom levels of PTSD, phobia, and depression were better predicted by the theory-derived cognitive variables than by the predictors established in the meta-analysis, as indicated by a better goodness of fit of the regression models. These results replicate and extend those of Ehring et al. (2006) with a prospective longitudinal design.
The better performance of the theory-derived variables was not due to an unusually low predictive power of the variables derived from the meta-analysis in this population. The correlations reported in Table 3 all match well the confidence intervals reported by Ozer et al. (2003); for example, the rhos of −.26 to −.32 found for social support for the different time points match their results of a confidence interval of −.15 to −.40 and weighted average of r = −.29. The only exception was the correlation of the number of past traumas, which fell below Ozer et al.'s confidence interval of .11 to .22. It is unclear whether differences in samples or differences in the assessment of past traumas, such as the types of previous traumas under consideration, may account for the latter finding. Alternatively, the fact that PTSD was prospectively determined soon after trauma in the present study, whereas the meta-analysis mainly relied on cross-sectional studies, including those with trauma recencies of 18 to more than 40 years, may, in part, explain the discrepancy. It is interesting that Ozer et al. (2003) identified three studies of accident survivors with recencies of 4 months and less that all showed correlations of trauma history and PTSD between .00 and .03, as in the present study. Thus, our results replicate the results of the meta-analysis well, supporting the validity of the findings.
Initial symptom levels after trauma have repeatedly been shown to predict subsequent severity of symptoms (e.g., Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992; Shalev et al., 1998) and are easy to measure. This raises the question of whether the predictors studied in this article provide added value in predicting the long-term psychological outcomes of trauma. The results of the regression analyses indicate that the predictors identified in Ozer et al.'s (2003) meta-analysis did not predict long-term outcome when initial symptom levels were controlled. A possible explanation for this negative finding is that these variables mainly predict the onset of symptoms but do not add to the prediction of long-term outcome, as maintaining factors are not included (Ehlers & Steil, 1995). In contrast, the variables derived from a cognitive model of PTSD (Ehlers & Clark, 2000) explained PTSD symptoms at 6 months above symptom levels at 2 weeks. These results are in line with those of previous prospective studies (Dunmore et al., 2001; Ehlers et al., 1998; Halligan et al., 2003). They extend the previous results in that predictors in the present study were assessed very soon after the trauma. It thus appears that the cognitive variables as specified in this model were already predictive from 2 weeks after the trauma onward. Similarly, variables derived from the vulnerability–stress model of depression (Ingram et al., 1998) improved the goodness of fit of the prediction of depression scores at 6 months above what could be predicted from initial depression at 2 weeks. Taken together, the results support the role of cognitive factors in the maintenance of PTSD and depression following MVA.
These results are also important for the question of possible criterion contamination between the cognitive predictor and outcome variables. It is important to note that there was no overlap between any of the predictors and the dependent variables in this study. However, critics may argue that it is still possible that some of the theory-derived variables in this study were affected by symptom levels (e.g., depressive rumination, thought suppression). Our finding that the theory-derived variables predicted outcome at follow-up when initial symptom levels were statistically controlled shows that their predictive power cannot be explained by criterion contamination.
Cognitive models of psychopathology postulate content specificity—that is, specific sets of cognitions are thought to be involved in the development and maintenance of each disorder (e.g., Beck et al., 1979; Clark, 1999). The specificity hypothesis implies that each of the three psychological outcomes should be best predicted by its disorder-specific model. The results support specificity for PTSD and depression. However, for travel phobia, the PTSD model showed a better fit than the phobia model. The results are consistent with those of a cross-sectional study by Ehring et al. (2006) and with Mayou et al.'s (2001) finding that some variables predicted PTSD as well as phobias after MVA but not depression.
Thus, whereas the results clearly support the role of cognitive factors in the prediction of PTSD and depression, they are less clear for the prediction of travel phobia. The variables derived from the cognitive–behavioral phobia model failed to substantially predict symptom levels at follow-up above initial symptom levels and performed worse at predicting outcome than the PTSD model. The results are in contrast to the findings of the cross-sectional study by Ehring et al. (2006), in which cognitive–behavioral variables were found to be specific when symptom levels of travel phobia were predicted. Thus, the variables derived from the phobia model appear to specifically fail when predicting chronic levels of travel phobia from early assessments. One possible explanation is that restrictions in travel due to injuries may have interfered with the early assessment of thoughts, feelings, and behaviors in travel situations. Approximately 50% of participants were still unable to travel when the predictors were assessed at 2 weeks or had only been in travel situations that were less relevant to their fear (e.g., being a passenger in a car for motorcyclists). This might have compromised the accuracy of their ratings. Furthermore, conditioned emotional reactions may be difficult to assess with self-report measures. Conversely, the findings could also reflect limitations of the theoretical model. The pattern of results is consistent with the idea that travel-related cognitions and safety behaviors are a consequence or an epiphenomenon of phobic travel anxiety rather than a causal or maintaining factor (Öhman & Mineka, 2001). This would explain the high concurrent associations between these variables and symptom measures but comparably poor predictive power. Finally, travel phobia might have had different sources in different participants and might have been a symptom of PTSD or subthreshold PTSD (Blanchard et al., 1996) in a subgroup of participants. Such lack of homogeneity might have increased error variance and would explain the high power of the PTSD model in predicting phobic symptom levels. More research is needed before a decision between these alternative explanations can be made.
A number of limitations of the study are noteworthy. First, the assessment of predictors relied on participants' self-report, which is susceptible to a range of biases. It would be desirable to conduct additional studies with objective tasks and/or experimental designs to further test the role of the cognitive factors in maintaining PTSD and depression after trauma. A number of such studies have yielded mostly supportive results for the PTSD model investigated in this article (e.g., Ehring, Frank, & Ehlers, in press; Halligan et al., 2002, 2003; Michael, Ehlers, & Halligan, 2005), but corresponding data on the maintenance of depression after trauma are lacking. Second, only six of the seven variables from Ozer et al.'s (2003) meta-analysis were included in the present study. However, it appears unlikely that this omission reduced the predictive power of the set of established predictors, as family psychopathology had the lowest effect sizes in the meta-analysis and has generally not been found to predict PTSD following MVA (Blanchard & Hickling, 2004).
Third, like other studies, this study found substantial comorbidity and high correlations between the symptom measures of PTSD, phobia, and depression. This raises the question of whether the outcome variables studied indeed represented different constructs. As we used self-report measures that have been validated against structured clinical interviews (Beck et al., 1979; Ehring et al., 2006; Foa et al., 1997), we assume that the different scales indeed measured different constructs and that the high correlations were due to high comorbidity in the sample. In addition, the high intercorrelations of the outcome measures worked against the study hypothesis in that they decreased the chances to establish specificity of the predictions. The fact that we found evidence for specificity despite high comorbidity is in line with the hypothesis that PTSD and depression, and possibly also travel phobia, are distinct responses to MVAs and not a unitary phenomenon, as suggested by some authors (for a more detailed discussion of this controversy, see Blanchard, Buckley, Hickling, & Taylor, 1998; Breslau, Chase, & Anthony, 2002; O'Donnell, Creamer, & Pattison, 2004). However, given the high comorbidity between the disorders as well as the symptom overlap, it might be useful for future research to adopt a dimensional, rather than categorical, approach to studying differential outcomes of MVA by investigating symptom clusters across disorders rather than symptom dimensions based on different diagnostic entities. Such an approach could also sharpen theoretical ideas about the mechanisms underlying the disorders.
Fourth, the distribution of the data required nonparametric regression analyses. These allowed us neither to compute significance tests for differences in prediction accuracy by the different models nor to report effect sizes for the multivariate analyses. However, the size of the zero-order correlations was similar to those in the Ehring et al. (2006) cross-sectional study, so their data can serve as a rough estimate of multivariate effect sizes. In Ehring et al.'s (2006) study, predictors from Ozer et al.'s (2003) meta-analyses predicted between 40% and 46% of the variance of symptom severities, whereas the variables derived from the cognitive models accounted for a significantly higher proportion of the variance (between 66% and 76%). The PTSD model explained 13%–15% more variance of PTSD severity than the other models, and the depression model explained 7% more variance of depression severity than the PTSD model and 34% more variance than the phobia model.
Fifth, the number of participants in each disorder category was relatively small, so that we could compare neither subgroups of participants with different single disorders nor participants with one disorder only versus those with several comorbid disorders. In addition, the sample was self-selected. However, results from a comparison with a random sample of MVA admissions at the same hospital suggest that the sample was largely representative of the population studied. Replication of the results with larger and, ideally, consecutive samples is desirable. Finally, the study only included one type of trauma, MVA with relatively low injury severity, and participants were assessed shortly after trauma. Future research needs to determine whether the results generalize to other types of trauma. It is encouraging to note that a recent study of assault survivors found similar results (Kleim, 2006). Nevertheless, given the broad evidence for the established predictors from Ozer et al.'s (2003) meta-analysis, other replications of the superior predictive power of the theory-derived cognitive variables are necessary before firm conclusions can be drawn (see also Kleim, Ehlers, & Glucksman, 2007). It would also be of interest to test whether the cognitive models apply equally well to trauma survivors who present many years after the event. As these models emphasize maintaining factors, we expect that the results should generalize well to very chronic populations.
The results have a number of clinical implications: First, as MVAs are common but only few survivors develop chronic emotional problems, the early identification of vulnerable individuals in need of treatment is an important clinical problem. The results suggest that theory-derived cognitive variables, but not the established predictors from Ozer et al.'s (2003) meta-analysis, improved the prediction of chronic PTSD and depression above initial symptom levels. As the cognitive predictors were assessed soon after the trauma, they can be regarded as promising candidates for the early identification of people at risk for chronic emotional problems. Second, the results support cognitive conceptualizations of PTSD and depression following MVA, and they suggest that individual differences in maintaining factors are important in predicting chronic PTSD and depression after trauma and thus also provide promising targets for psychological treatment.
Supplementary Material
Acknowledgments
Thomas Ehring is now at the Department of Clinical Psychology, University of Amsterdam, Amsterdam, the Netherlands.
The present study was supported by a Wellcome Prize Studentship awarded to Thomas Ehring and by a Wellcome Trust Principal Research Fellowship awarded to Anke Ehlers. We thank Inga Böllinghaus, Birgit Kleim, Anke Weidmann, Silke Frank, Ines Sengstock, Stephanie Spengler, Jennifer Baumeister, Franziska Wallott, Johanna Hissbach, and the staff of King's College Hospital's Accident and Emergency Department for their support. We thank Sabine Landau for statistical advice and Melanie Walwyn Martin for the Injury Severity Score ratings.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Baker S. P., O'Neill B., Haddon W. Jr., & Long W. B. (1974). The Injury Severity Score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma, 14, 187–196. [PubMed] [Google Scholar]
- Beck A. T., Emery G., & Greenberg R. L. (1985). Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books. [Google Scholar]
- Beck A. T., Rush A. J., Shaw B. F., & Emery G. (1979). Cognitive therapy of depression. New York: Guilford Press. [Google Scholar]
- Blake D. D., Weathers F. W., Nagy L. M., Kaloupek D. G., Gusman F. D., Charney D. S., et al. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Blanchard E. B., Buckley T. C., Hickling E. J., & Taylor A. E. (1998). Posttraumatic stress disorder and comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders, 12, 21–37. [DOI] [PubMed] [Google Scholar]
- Blanchard E. B., & Hickling E. J. (2004). After the crash: Psychological assessment and treatment of survivors of motor vehicle accidents. Washington, DC: American Psychological Association. [Google Scholar]
- Blanchard E. B., Hickling E. J., Freidenberg B. M., Malta L. S., Kuhn E., & Sykes M. A. (2004). Two studies of psychiatric morbidity among motor vehicle accident survivors 1 year after the crash. Behaviour Research and Therapy, 42, 569–583. [DOI] [PubMed] [Google Scholar]
- Blanchard E. B., Hickling E. J., Taylor A. E., Loos W. R., Forneris C. A., & Jaccard J. (1996). Who develops PTSD from motor vehicle accidents? Behaviour Research and Therapy, 34, 1–10. [DOI] [PubMed] [Google Scholar]
- Brady K. T., Killeen T. K., Brewerton T., & Lucerini S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32. [PubMed] [Google Scholar]
- Breslau N., Chase G. A., & Anthony J. C. (2002). “A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection.” Reply. Psychological Medicine, 32, 1480–1483. [Google Scholar]
- Brewin C. R., Andrews B., & Valentine J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. [DOI] [PubMed] [Google Scholar]
- Chernick M. R. (1999). Bootstrap methods: A practitioner's guide. New York: Wiley. [Google Scholar]
- Clark D. M. (1999). Anxiety disorders: Why they persist and how to treat them. Behaviour Research and Therapy, 37, S5–S27. [DOI] [PubMed] [Google Scholar]
- Clohessy S., & Ehlers A. (1999). PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology, 38, 251–265. [DOI] [PubMed] [Google Scholar]
- Cohen J., Cohen P., West S. G., & Aiken L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, NJ: Erlbaum. [Google Scholar]
- Dunmore E., Clark D. M., & Ehlers A. (1999). Cognitive factors involved in the onset and maintenance of posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 37, 809–829. [DOI] [PubMed] [Google Scholar]
- Dunmore E., Clark D. M., & Ehlers A. (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 39, 1063–1084. [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Clark D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Hofmann S. G., Herda C. A., & Roth W. T. (1994). Clinical characteristics of driving phobia. Journal of Anxiety Disorders, 8, 323–339. [Google Scholar]
- Ehlers A., Mayou R. A., & Bryant B. (1998). Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology, 107, 508–519. [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Steil R. (1995). Maintenance of intrusive memories in posttraumatic stress disorder: A cognitive approach. Behavioural and Cognitive Psychotherapy, 23, 217–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A., Taylor J. E., Ehring T., Hofmann S. G., Deane F. P., Roth W. T., et al. (2007). The Driving Cognitions Questionnaire: Development and preliminary psychometric properties. Journal of Anxiety Disorders, 21, 493–509. [DOI] [PubMed] [Google Scholar]
- Ehring T., Frank S., & Ehlers A. (in press). The role of rumination and reduced concreteness in the maintenance of PTSD and depression following trauma. Cognitive Therapy and Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T., Ehlers A., & Glucksman E. (2006). Contribution of cognitive factors to the prediction of post-traumatic stress disorder, phobia and depression after motor vehicle accidents. Behaviour Research and Therapy, 44, 1699–1716. [DOI] [PubMed] [Google Scholar]
- Evans C., Ehlers A., Mezey G., & Clark D. M. (2007). Intrusive memories in perpetrators of violent crime: Emotions and cognitions. Journal of Consulting and Clinical Psychology, 75, 134–144. [DOI] [PubMed] [Google Scholar]
- Everitt B. S. (1998). Analysis of longitudinal data: Beyond MANOVA. British Journal of Psychiatry, 172, 7–10. [DOI] [PubMed] [Google Scholar]
- Fedoroff I. C., Taylor S., Asmundson G. J. G., & Koch W. J. (2000). Cognitive factors in traumatic stress reactions: Predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behavioural and Cognitive Psychotherapy, 28, 5–15. [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., & Williams J. B. W. (1996). Structured clinical interview for DSM–IV Axis I disorders. Washington, DC: American Psychiatric Press. [Google Scholar]
- Foa E. B., Cashman L., Jaycox L., & Perry K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9, 445–451. [Google Scholar]
- Foa E. B., Ehlers A., Clark D. M., Tolin D. F., & Orsillo S. M. (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. [Google Scholar]
- Green S. B. (1991). How many subjects does it take to do a regression analysis? Multivariate Behavioral Research, 26, 499–510. [DOI] [PubMed] [Google Scholar]
- Halligan S. L., Clark D. M., & Ehlers A. (2002). Cognitive processing, memory, and the development of PTSD symptoms: Two experimental analogue studies. Journal of Behavior Therapy and Experimental Psychiatry, 33, 73–89. [DOI] [PubMed] [Google Scholar]
- Halligan S. L., Michael T., Clark D. M., & Ehlers A. (2003). Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of Consulting and Clinical Psychology, 71, 419–431. [DOI] [PubMed] [Google Scholar]
- Hox J. J. (1995). Applied multi-level analysis. Amsterdam: TT-Publikaties. [Google Scholar]
- Ingram R. E., Miranda J., & Segal Z. V. (1998). Cognitive vulnerability to depression. New York: Guilford Press. [Google Scholar]
- Joseph S. (1999). Social support and mental health following trauma. In Yule W. (Ed.), Post-traumatic stress disorder: Concepts and therapy (pp. 71–91). Chichester, England: Wiley. [Google Scholar]
- Kessler R. C., Sonnega A., Bromet E., Hughes M., & Nelson C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kleim B. (2006). Cognitive and physiological predictors of PTSD, depression, and phobia following assault. London: King's College London. [Google Scholar]
- Kleim B., Ehlers A., & Glucksman E. (2007). Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychological Medicine, 37, 1457–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laposa J. M., & Alden L. E. (2003). Posttraumatic stress disorder in the emergency room: Exploration of a cognitive model. Behaviour Research and Therapy, 41, 49–65. [DOI] [PubMed] [Google Scholar]
- Marmar C. R., Weiss D. S., & Metzler T. J. (1997). The Peritraumatic Dissociative Experiences Questionnaire. In Keane T. M. & Wilson J. P. (Eds.), Assessing psychological trauma and PTSD (pp. 412–428). New York: Guilford Press. [Google Scholar]
- Mayou R. A., Bryant B. M., & Ehlers A. (2001). Prediction of psychological outcomes one year after a motor vehicle accident. American Journal of Psychiatry, 158, 1231–1238. [DOI] [PubMed] [Google Scholar]
- McFarlane A. C., Atchison M., & Yehuda R. (1997). The acute stress response following motor vehicle accidents and its relation to PTSD. Annals of the New York Academy of Sciences, 821, 437–441. [DOI] [PubMed] [Google Scholar]
- Michael T., Ehlers A., & Halligan S. L. (2005). Enhanced priming for trauma-related material in posttraumatic stress disorder. Emotion, 5, 103–112. [DOI] [PubMed] [Google Scholar]
- Murray J., Ehlers A., & Mayou R. A. (2002). Dissociation and posttraumatic stress disorder: Two prospective studies of motor vehicle accident survivors. British Journal of Psychiatry, 180, 363–368. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., & Morrow J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology, 61, 115–121. [DOI] [PubMed] [Google Scholar]
- Norris F. H. (1992). Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology, 60, 409–418. [DOI] [PubMed] [Google Scholar]
- O'Donnell M. L., Creamer M., & Pattison P. (2004). Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry, 161, 1390–1396. [DOI] [PubMed] [Google Scholar]
- O'Donnell M. L., Creamer M., Pattison P., & Atkin C. (2004). Psychiatric morbidity following injury. American Journal of Psychiatry, 161, 507–514. [DOI] [PubMed] [Google Scholar]
- Öhman A., & Mineka S. (2001). Fears, phobias, and preparedness: Toward an evolved module of fear and fear learning. Psychological Review,108,483–522. [DOI] [PubMed] [Google Scholar]
- Ozer E. J., Best S. R., Lipsey T. L., & Weiss D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. [DOI] [PubMed] [Google Scholar]
- Rothbaum B. O., Foa E. B., Riggs D. S., Murdock T. B., & Walsh W. (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5, 455–475. [Google Scholar]
- Salkovskis P. M. (1996). The cognitive approach to anxiety: Threat beliefs, safety-seeking behavior, and the special case of health anxiety and obsession. In Salkovskis P. M. (Ed.), Frontiers of cognitive therapy (pp. 48–74). New York: Guilford Press. [Google Scholar]
- Shalev A. Y., Freedman S., Peri T., Brandes D., Sahar T., Orr S. P., et al. (1998). Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry, 155, 630–637. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2003). Stata Version 8.1 [computer software]. College Station, TX: Author. [Google Scholar]
- Taylor J. E., Deane F. P., & Podd J. V. (2000). Determining the focus of driving fears. Journal of Anxiety Disorders, 14, 453–470. [DOI] [PubMed] [Google Scholar]
- Taylor S., & Koch W. J. (1995). Anxiety disorders due to motor vehicle accidents: Nature and treatment. Clinical Psychology Review, 15, 721–738. [Google Scholar]
- Teasdale J. D., & Barnard P. J. (1993). Affect, cognition, and change: Re-modelling depressive thought. Hove, England: Erlbaum. [Google Scholar]
- Teasdale J. D., & Cox S. G. (2001). Dysphoria: Self-devaluative and affective components in recovered depressed patients and never depressed controls. Psychological Medicine, 31, 1311–1316. [DOI] [PubMed] [Google Scholar]
- Tolin D. F., & Foa E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992. [DOI] [PubMed] [Google Scholar]
- Van der Does W. (2002). Cognitive reactivity to sad mood: Structure and validity of a new measure. Behaviour Research and Therapy, 40, 105–120. [DOI] [PubMed] [Google Scholar]
- Wethington E., Brown G. W., & Kessler R. C. (1997). Interview measurement of stressful life events. In Cohen S., Kessler R. C., & Gordon L. U. (Eds.), Measuring stress: A guide for health and social scientists (pp. 59–79). New York: Oxford University Press. [Google Scholar]
- Willson V. L. (1976). Critical values of the rank-biserial correlation coefficient. Educational and Psychological Measurement, 36, 297–300. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.