Abstract
Vitamin E is an important natural antioxidant, and its most common and biologically active form is α-tocopherol. In addition to this, specific regulatory effects of vitamin E have been revealing. The body exerts a certain effort to regulate its tissue levels with specific tocopherol transport proteins and membrane receptors. Antiproliferative and protein kinase C-supressing effects of alpha-tocopherol have been previously demonstrated, which have not been mimicked by beta-tocopherol or probucol. Protein kinase C promises to be an important area of interest in the means of glaucoma and cataractogenesis. It has been shown in different models that retinal vasculer dysfunction due to hyperglycemia could be prevented by alpha-tocopherol via the diachylglycerol-protein kinase C pathway. Glutamate transporter activity has been shown to be modulated by protein kinase C. This pathway is also important in intraocular pressure-lowering effects of prostaglandin and its analogs in glaucoma therapy. Filtran surgery became another possible area of usage of alpha-tocopherol since its antiproliferative effect has been demonstrated in human Tenon's capsule fibroblasts. Prevention of posterior capsule opacification is another area for future studies. It is evident that when correct and safe modulation is the objective, alpha-tocopherol merits a concern beyond its mere antioxidant properties.
Introduction
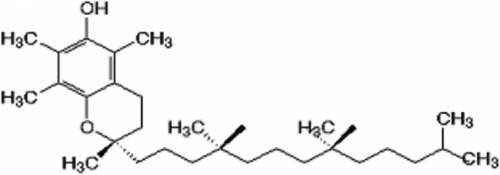
Vitamin E is a natural, highly tolerable and cost effective molecule. This generic term is used for tocopherol and tocotrienols consisting of two rings with a hydrocarbon chain. Both structures are similar, although the tocotrienol structure has double bonds on the isoprenoid units. Natural vitamin Es are known as α, β, γ, and δ according to the methyl or proton groups that are bound to their Benzene rings, and the most common and biologically active form is alpha-tocopherol (Figure 1) [1]. When produced synthetically, it is composed of eight stereoisomers in which RRR-α-tocopherol is the most biologically active form [2].
Figure 1.
Molecular structure of α-tocopherol. Shown is the molecular structure of α-tocopherol, consisting of two benzene rings with a hydrocarbon chain
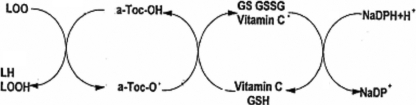
While the recommended daily allowance (RDA) for vitamin E is 8 mg (12 IU) for females and 10 mg (15 IU) for males, Packer [3] recommends up to 1,000–1,200 IU intake of vitamin E in some pathologies including cataract. The principal reserve of natural vitamin E is vegetable oil where its function is to protect tissue from oxidative demage. It is a liposoluble molecule, and, therefore, after dietary intake, vitamin E is not only absorbed easily from the intestinal lumen but is also dispersed between lipids and proteins in cell membranes. Vitamin E molecules can interrupt free radical chain reactions by capturing the free radical. This imparts to them their antioxidant properties. The free hydroxyl group on the aromatic ring is responsible for the antioxidant properties. The hydrogen from this group is donated to the free radical, resulting in a relatively stable free radical form of vitamin E (Figure 2) [2].
Figure 2.
Antioxidant mechanism of tocopherols. LH: Lipid molecule, LOOH: Lipid peroxide, LOO+: Lipid Peroxide radical, a-Toc-OH: α-Tocopherol, a-Toc-O+: α-Tocopherol radical, GSH: Glutathione, Vitamin C+: Vitamin C radical, GS+: Glutathione radical, GSSG: Oxidized glutathione, NADPH: Reduced nicotinamide adenine dinucleotide phosphate, NADP+: Oxidized nicotinamide adenine dinucleotide phosphate.
Regarding the pharmacodynamics of tocopherols, it has been reported in a study conducted in human eyes that the retinal levels of vitamin E are higher than those of the choroid or vitreous and is correlated with serum levels of vitamin E [4]. It is known that vitamin E can only reach its theraupetic levels in aqueous humor and lens via topical application and is accumulated within the retina when applied via the oral or parenteral route [5]. Moreover, it is reported in animal studies that when 100 mg/kg α-tocopherol is applied via oral or parenteral route, it causes a similar threefold to sixfold increase to its serum levels, though the retinal and vitreal increases are somewhat slower via the oral route [6].
Based on the common knowledge summarized above, vitamin E is occasionally prescribed in ophthalmology clinics. This article provides an overview of the existing literature regarding other effects of this molecule that illuminates the potential usage of this drug as an effective, specific therapeutic tool in several ocular pathologies.
Discussion
Beyond the nonspecific antioxidant effect
Specific effects of Vitamin E, which includes gene regulation, have been revealing, and non-antioxidant properties of tocopherols are current topics of interest [7]. In many in vivo and in vitro studies, the antiproliferative effect vitamin E has been shown [8-10].
Protein kinase C (PKC) is one of the pathways used by α-tocopherol [11]. Sharma et al. [12] reported that tocopherol inhibits not only free radical formation but also tyrosine kinase activity in Tissue Plasminogen Activator (TPA)-induced primary human fibroblasts or HL-60 cells. Results of many published in vivo and in vitro collaborative studies illuminate the antiproliferative effect of α-tocopherol via the PKC pathway in the vascular smooth muscle cell model, and they have been summarized by Ozer et al. [13]. In smooth muscle cell cultures, neither the antiproliferative nor the PKC-supressing effects of α-tocopherol have been shown by its isomer, β-tocopherol, or another antioxidant, probucol. It is also shown that, 3H Timidin incorporations and PKC activities gradually decline as the α-tocopherol level in the medium rises. On the other hand, linkage of Activator Protein (AP-1) to DNA has been supressed by the application of α-tocopherol in para-methoxyamphetamine (PMA)-stimulated cells, but this effect has not seen in phase G0 cells. These findings are also succesfully supported by rabbit studies in the atherosclerosis model.
The existence of sensitive mechanisms to regulate tissue levels is an important and distinctive feature of vitamin E [10,14]. The tocopherol transfer protein, responsible for the intracellular transportation of vitamin E, has been shown and described in cell cultures [15], animals [16-19], and various human tissues [20-22]. Furthermore, discovery of α-tocopherol specific membrane receptors [23] and cytosolic transfer proteins strengthen the thesis that vitamin E possesses properties beyond a mere antioxidant function [10]. Specifically for the eye, scavenger receptor class B type I at the inner blood-retinal barrier has been described in vitro, which is responsible for α-tocopherol uptake from the circulating blood and plays a key role in maintaining α-tocopherol in the neural retina [24].
Clinical importance
Protective effects of vitamin E have been shown in almost all eye tissues with in clinical, in vitro, and in vivo studies. For instance, vitamin E is known to double the rabbit corneal endothelial cell survival time [25] and enhances retinal cell survival via its effect on mitochondrial activity [26]. Also, α-tocopherol can protect the retina from light injury for up to 24 h of exposure [27]. Vitamin E plays an important prophylactic role against several serious light-induced diseases and conditions of the eye (cataractogenesis and retinal photodeterioration) and skin (erythrocyte photohemolysis, photoerythema, photoaging, and photocarcinogenesis) that are mediated by photooxidative damage to cell membranes [28]. These findings do not have to be explained with antioxidant mechanisms, especially for α-tocopherol. As Azzi [20] stated: “A number of lines of evidence, evolutionary, genetic, biochemical, and functional, have indicated that the natural function of α-tocopherol is that of cell signaling. Such a property is not shared by any other antioxidant molecule.”.
An association between α-tocopherol and some ocular pathologies has also been demonstrated previously. For example, retinitis pigmentosa is shown to be related to an H101Q mutation in the α-tocopherol transfer protein gene [29]. The combination of cryotherapy with vitamin E prophylaxis appeared to decrease the severity and sequelae of threshold retinopathy of prematurity [30]. Average levels of α-tocopherol were shown to be lower in people with exudative macular degeneration [31].
Developments in the understanding of these molecules have increased the attention paid to properties beyond their antioxidant function, including antiproliferative effects. Retinal pigment epithelium cells migrating through the damaged retina play an important role in the pathogenesis of proliferative vitreoretinopathy. Majon et al. [32] found that α-tocopherol inhibits proliferation of human retina pigment epithelium (RPE) cells in culture without exerting cytotoxic effects. Maximal inhibition was achieved with 100 μM α-tocopherol. It has been found that α-tocopherol succinate inhibits proliferation and migration of retinal pigment epithelial cells in vitro [33]. α-Tocopherol and α-tocopheryl acid succinate in saline solution presented a retardation of proliferative vitreoretinopathy in retinal detachments [34].
The protective function of α-tocopherol against the process of cataractogenesis in humans is reported in epidemiologic studies [35]. In the Beaver Dam Eye Study, it is shown that age-related lens opacities in humans are linked inversely to vitamin E status [36].
Glaucoma is another possible area of usage for vitamin E. Failure in glaucoma surgery is primarily due to fibrocellular scar formation, derived from Tenon's capsule fibroblasts. It has been found that d-α-tocopherol (vitamin E) was able to inhibit proliferation of in vitro human Tenon's capsule fibroblasts [37]. Following this, filtran surgery became another model in which an antiproliferative effect has been shown in vivo. α-Tocopherol derivatives showed antiproliferative properties in the experimental models of filtering surgery and showed better intraocular pressure (IOP) control and bleb survival [38,39]. Cell culture studies further illuminated this effect, and comparative studies with other antimetabolites have been performed [40].
On the other hand, dual effects of α-tocopherol and PKC on the eye are of interest in the means of glaucoma therapy. Kunisaki et al. in 1995 [41] and Lee at al. in 1999 [42] showed in different models that retinal vasculer dysfunction due to hyperglycemia could be prevented by α-tocopherol via a diachylglycerol-PKC pathway. In a study performed by Engin et al. [43], 60 glaucomatous eyes from 30 patients were divided into three groups. While group A patients recieved no tocopherol, group B and group C patients were given 300 and 600 mg/day of oral α-tocopheril acetate, respectively. Visual fields and retinal blood flows of ophthalmic and posterior ciliary arteries with Doppler ultrasonography were evaluated in the beginning of the study, as well 6 and 12 months after treatment. Compared with group A, differences of pulsatilty and resistivity indexes of ophthalmic and posterior ciliary arteries were lower in groups B and C 6 and 12 months after treatment. Posterior ciliary artery differences of resistivity indexes in the 6th and 12th months and ophthalmic artery differences of pulsatilty indexes reductions in the sixth month were statistically significant. Differences of mean deviations with visual fields in groups B and C were significantly lower than that of group A.
Focus on protein kinase C
Among other signaling pathways that have been shown to be affected by α-tocopherol, PKC promises to be an important area of interest. It is a widespread serin/threonine kinase responsible for transduction of the signals taken from the G protein coupled, tyrosine kinase receptors, and nonreceptor tyrosine kinases to the nucleus via phospholipid hydrolysis [44]. c-Jun, c-fos, and c-myc are reported to be the transcription factors that have been activated [45]. Although AP-1 is the mostly considered family [46-48], nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) [49] and Transcriptional enhance factor-1 (TEF-1) [50] are among other transcription factors known to be affected by PKC.
Beside its role in retinal vasoregulation mentioned above, the PKC pathway boasts a decisive factor in the pathogenesis for and on the clinical course of glaucoma. Glaucoma is one of the neurodegenerative conditions arising from a compromised glutamate homeostasis. Glutamate transporter activity has been shown to be modulated by PKC [51]. PKC have been shown to affect nonvascular smooth muscle cells such as the iris sphincter [52]. Wiederholt et al. [53] have reported that various pathways and ion channels affect PKC isomers producing different responses in eye nonvascular smooth muscle cells, but in general, PKC inhibitors relax trabecular meshwork while leaving the ciliary muscle comparatively unaffected.
Alexander and Acott [54] have reported that the PKC pathway is crucial in glaucoma therapy for the intraocular pressure-lowering effects of Prostaglandin F 2α (PGF2α) and its analog, latanoprost. The cytokine, Tumor Necrosis Factor α (TNFα), is a strong modulator of trabecular meshwork matrix metalloproteinase (MMP) and tissue inhibitor (TIMP) expressions. TNFα treatment triggered some PKC isoform translocations. Exposure of trabecular cells to TNFα for 72 h differentially downregulated several PKC isoforms. Treatment with a phorbol mitogen that stimulates most PKC isoforms produced strong increases in these MMPs. Effects of TNFα on MMP and TIMP expressions were completely blocked by only one PKC inhibitor.
Further studies were conducted to identify signal-transduction pathways involved. In a study performed concerning cat iris sphincter smooth muscle cells, the relaxing effects of PGF2α and carbachol have been shown to be produced by mitogen activated protein (MAP) kinases in a PKC-dependent manner [55]. On the other hand, PKC activators strongly stimulate the phosphorylation of AQP4 (aquaporin in the ciliary body) and inhibit AQP4 activity in a dose-dependent manner [56].
The prevention of posterior capsule opacification (PCO) is another area for future studies. Despite recent advances in cataract extraction, lens epithelial cells remaining in the capsule proliferate and eventually cause opacification within days of surgery [57]. Although inhibition of lens epithelial cells can be observed with various agents, toxic side effects to the ciliary body, cornea epithelium, and iris limit their use in human subjects [58-60]. PCO is a process mainly involving proliferation and migration of the lens epithelium [61], and PKC is a signaling pathway that is known to result in major effects on this process.
PKC activity exists in the cytosol and particulate fractions of bovine lens epithelial cells [62], and its role in both cell differentiation [63] and proliferation [64] have been shown in rabbit lens epithelial cells. Furthermore, it is shown in lens epithelial cells that, 12(S)HETE-dependent activation of PKCα and βII acts in concert with other epidermal growth factor (EGF)-dependent signals to induce c-fos mRNA and that this is independent of the extracellular signal-regulated kinases 1/2 (Erk1/2) pathway [65]. The PKC dependent inositol signaling system also regulates K+ fluxes in these highly proliferative lens epithelial cells primarily by affecting the rate via a Na+-Cl--K+ cotransport mechanism [66]. In addition, PKCγ has a direct or indirect inhibitory effect on gap junction communication in lens epithelial cells [67,68] via phosphorylation of Connexin43 on serine and this causes disassembly and loss of gap junction from the cell surface [69]. PKC also plays a role in cataractogenesis by phosphorylating proteins from calf lens fiber membranes [70] and activating neutral proteases [71]. The PKC-inhibiting effect of vitamin E is known to exist in epithelial cells [72]. Intramuscular vitamin E supplementation is sufficient in protecting histopathologic changes in the lens epithelium [73].
Intracellular functions of vitamin E -beyond its general antioxidant role was an interesting issue even in 1946 [20]. Today, molecular biology is an important discipline to solve curent challenges in ophthalmology. It is already known that certain isomers of vitamin E exert specific effects, and this suggests that proper use of a correctly selected type of vitamin E is likely to provide a significant improvement in the prevention and treatment of many ocular pathologies. Numerous drugs with the potential to manipulate intracellular signal transmission pathways are still being tried. However, both the variations between the receptor and ion-chanel subtypes and the fact that a certain blocker binds to various regions in a condition-dependent manner preclude the production of therapeutics that will bind correctly to the appropriate location. Also, side effects of those substances gravely limit their clinical use. Currently, it is evident that regarding correct and safe intracellular signal modulation, α-tocopherol, a natural, safe, and cost effective drug, merits a careful look beyond its mere antioxidant properties.
References
- 1.Brigelius-Flohe R, Traber MG. Vitamin E: Function and metabolism. FASEB J. 1999;13:1145–55. [PubMed] [Google Scholar]
- 2.Sies H, Murphy ME. Role of tocopherols in the protection of biological systems against oxidative damage. J Photochem Photobiol B. 1991;8:211–8. doi: 10.1016/1011-1344(91)80061-l. [DOI] [PubMed] [Google Scholar]
- 3.Packer L. Protective role of Vitamin E in biological systems. Am J Clin Nutr. 1991;53:1050S–5S. doi: 10.1093/ajcn/53.4.1050S. [DOI] [PubMed] [Google Scholar]
- 4.Bhat R. Serum, retinal, choroidal vitreal Vitamin E concentrations in human infants. Pediatrics. 1986;78:866–70. [PubMed] [Google Scholar]
- 5.Nagata M, Kawazu K, Midori Y, Kojima M, Shirasawa E, Sasaki K. Intracameral and lenticular penetration of locally applied stable isotope-labeled vitamin E. Jpn J Ophthalmol. 2001;45:125–7. doi: 10.1016/s0021-5155(00)00361-0. [DOI] [PubMed] [Google Scholar]
- 6.Bhat R, Raju T, Barrada A, Evans M. Disposition of Vitamin E in the eye. Pediatr Res. 1987;22:16–20. doi: 10.1203/00006450-198707000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Azzi A, Stocker A. Vitamin E: non-antioxidant roles. Prog Lipid Res. 2000;39:231–55. doi: 10.1016/s0163-7827(00)00006-0. [DOI] [PubMed] [Google Scholar]
- 8.Tran K, Chan A. RRR-alpha tocopherol potentiates prostacyclin release in human endothelial cells. Evidence for structural specifity of tocopherol molecule. Biochim Biophys Acta. 1990;1043:189–97. doi: 10.1016/0005-2760(90)90295-9. [DOI] [PubMed] [Google Scholar]
- 9.Chatelain E, Boscobionik DO, Bartoli GM, Kagan VE, Gey FK, Packer L, Azzi A. Inhibition of smooth muscle cell proliferation and protein kinase C activity by tocopherols and tocotrienols. Biochim Biophys Acta. 1993;1176:83–9. doi: 10.1016/0167-4889(93)90181-n. [DOI] [PubMed] [Google Scholar]
- 10.Traber MG, Packer L. Vitamin E beyond antioxidant function. Am J Clin Nutr. 1995;62(6 Suppl):1501S–9S. doi: 10.1093/ajcn/62.6.1501S. [DOI] [PubMed] [Google Scholar]
- 11.Boscoboinik D, Szewczyk A, Hensey C, Azzi A. Inhibition of cell proliferation by α-tocopherol. Role of protein kinase. J Biol Chem. 1991;266:6188–94. [PubMed] [Google Scholar]
- 12.Sharma S, Stutzman JD, Kelloff GJ, Steele VE. Screening of potential chemopreventive agents using biochemical markers of carcinogenesis. Cancer Res. 1994;54:5848–55. [PubMed] [Google Scholar]
- 13.Özer NK, Şirikçi Ö, Taha S, Engin KN, Boscobionik D, Clement S, Stocker A, Azzi A. Prevention of atherosclerosis by α-tocopherol in smooth muscle cells by a mechanism involving signal transduction modulation. In: Özben T, editors. Free radicals, oxidative stress and antioxidants. NATO ASI Series A. New York: Plenum Press; 1998. p. 333–42. [Google Scholar]
- 14.Kayden HJ, Traber MG. Absorbtion, lipoprotein transport and regulation of plasma concentrations of vitamin E in humans. J Lipid Res. 1993;34:343–58. [PubMed] [Google Scholar]
- 15.Horiguchi M, Arita M, Kaempf-Rotzoll DE, Tsujimoto M, Inoue K, Arai H. pH-dependent translocation of alpha-tocopherol transfer protein (alpha-TTP) between hepatic cytosol and late endosomes. Genes Cells. 2003;8:789–800. doi: 10.1046/j.1365-2443.2003.00676.x. [DOI] [PubMed] [Google Scholar]
- 16.Dutta-Roy AK, Gordon MJ, Leishman DJ, Duthie GG, James WPT. Purification and partial caracterization of an α-tocopherol binding protein from rabbit heart cytosol. Mol Cell Biochem. 1993;123:139–44. doi: 10.1007/BF01076485. [DOI] [PubMed] [Google Scholar]
- 17.Murphy DJ, Mavis RD. Membrane transfer of α-tocopherol. J Biol Chem. 1981;256:10464–8. [PubMed] [Google Scholar]
- 18.Sato Y, Hagiwara K, Arai H, Inoue K. Purification and characterization of α−tocopherol transfer protein from rat liver. FEBS Lett. 1991;288:41–5. doi: 10.1016/0014-5793(91)80999-j. [DOI] [PubMed] [Google Scholar]
- 19.Zimmer S, Stocker A, Sarbolouki MN, Spycher SE, Sassoon J, Azzi A. A novel human tocopherol-associated protein: cloning, in vitro expression, and characterization. J Biol Chem. 2000;275:25672–80. doi: 10.1074/jbc.M000851200. [DOI] [PubMed] [Google Scholar]
- 20.Azzi A. Molecular mechanism of alpha-tocopherol action. Free Radic Biol Med. 2007;43:16–21. doi: 10.1016/j.freeradbiomed.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Arita M, Sato Y, Miyata A. Human α-tocopherol transfer protein: cDNA cloning, expression and chromozomal location. Biochem J. 1995;306:437–43. doi: 10.1042/bj3060437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Traber MG. Determinants of plasma vitamin E concentrations. Free Radic Biol Med. 1994;16:229–39. doi: 10.1016/0891-5849(94)90148-1. [DOI] [PubMed] [Google Scholar]
- 23.Urano S, Inomori Y, Sugawara T. Vitamin E: Inhibition of retinol induced hemolysis and membrane stabilizing behavior. J Biol Chem. 1992;267:18365–70. [PubMed] [Google Scholar]
- 24.Tachikawa M, Okayasu S, Hosoya K. Functional involvement of scavenger receptor class B, type I, in the uptake of alpha-tocopherol using cultured rat retinal capillary endothelial cells. Mol Vis. 2007;13:2041–7. [PubMed] [Google Scholar]
- 25.Neuwirth-Lux O, Billson F. Vitamin E and rabbit corneal endothelial cell survival. Aust N Z J Ophthalmol. 1987;15:309–14. doi: 10.1111/j.1442-9071.1987.tb00088.x. [DOI] [PubMed] [Google Scholar]
- 26.Rego AC, Santos MS, Proenca MT, Oliveira CR. Influence of vitamin E succinate on retinal cell survival. Toxicology. 1998;128:113–24. doi: 10.1016/s0300-483x(98)00054-7. [DOI] [PubMed] [Google Scholar]
- 27.Aonuma H, Koide K, Masuda K, Watanabe I. Retinal light damage: protective effect of alpha-tocopherol. Jpn J Ophthalmol. 1997;41:160–07. doi: 10.1016/s0021-5155(97)00034-8. [DOI] [PubMed] [Google Scholar]
- 28.Fryer MJ. Evidence for the photoprotective effects of vitamin E. Photochem Photobiol. 1993;58:304–12. doi: 10.1111/j.1751-1097.1993.tb09566.x. [DOI] [PubMed] [Google Scholar]
- 29.Pang J, Kiyosawa M, Seko Y, Yokota T, Harino S, Suzuki J. Clinicopathological report of retinitis pigmentosa with vitamin E deficiency caused by mutation of the alpha-tocopherol transfer protein gene. Jpn J Ophthalmol. 2001;45:672–6. doi: 10.1016/s0021-5155(01)00425-7. [DOI] [PubMed] [Google Scholar]
- 30.Johnson L, Quinn GE, Abbasi S, Gerdes J, Bowen FW, Bhutani V. Severe retinopathy of prematurity in infants with birth weights less than 1250 grams: incidence and outcome of treatment with pharmacologic serum levels of vitamin E in addition to cryotherapy from 1985 to 1991. J Pediatr. 1995;127:632–9. doi: 10.1016/s0022-3476(95)70129-x. [DOI] [PubMed] [Google Scholar]
- 31.Mares-Perlman JA, Brady WE, Klein R, Klein BE, Bowen P, Stacewicz-Sapuntzakis M, Palta M. Serum antioxidants and age-related macular degeneration in a population-based case-control study. Arch Ophthalmol. 1995;113:1518–23. doi: 10.1001/archopht.1995.01100120048007. [DOI] [PubMed] [Google Scholar]
- 32.Mojon D, Boscoboinik D, Haas A, Bohnke M, Azzi A. Vitamin E inhibits retinal pigment epithelium cell proliferation in vitro. Ophthalmic Res. 1994;26:304–9. doi: 10.1159/000267493. [DOI] [PubMed] [Google Scholar]
- 33.Sakamoto T, Hinton DR, Kimura H, Spee C, Gopalakrishna R, Ryan SJ. Vitamin E succinate inhibits proliferation and migration of retinal pigment epithelial cells in vitro: therapeutic implication for proliferative vitreoretinopathy. Graefes Arch Clin Exp Ophthalmol. 1996;234:186–92. doi: 10.1007/BF00462031. [DOI] [PubMed] [Google Scholar]
- 34.Larrosa JM, Veloso AA, Jr, Leong FL, Refojo MF. Antiproliferative effect of intravitreal alpha-tocopherol and alpha-tocopheryl-acid-succinate in a rabbit model of PVR. Curr Eye Res. 1997;16:1030–5. doi: 10.1076/ceyr.16.10.1030.9022. [DOI] [PubMed] [Google Scholar]
- 35.Seth RK, Kharb S. Protective function of alpha-tocopherol against the process of cataractogenesis in humans. Ann Nutr Metab. 1999;43:286–9. doi: 10.1159/000012796. [DOI] [PubMed] [Google Scholar]
- 36.Lyle BJ, Mares-Perlman JA, Klein BE, Klein R, Palta M, Bowen PE, Greger JL. Serum carotenoids and tocopherols and incidence of age-related nuclear cataract. Am J Clin Nutr. 1999;69:272–7. doi: 10.1093/ajcn/69.2.272. [DOI] [PubMed] [Google Scholar]
- 37.Haas AL, Boscoboinik D, Mojon DS, Bohnke M, Azzi A. Vitamin E inhibits proliferation of human Tenon's capsule fibroblasts in vitro. Ophthalmic Res. 1996;28:171–5. doi: 10.1159/000267899. [DOI] [PubMed] [Google Scholar]
- 38.Larrosa JM, Polo V, Ramirez T, Pinilla I, Pablo LE, Honrubia FM. Alpha-tocopherol derivatives and wound healing in an experimental model of filtering surgery. Ophthalmic Surg Lasers. 2000;31:131–5. [PubMed] [Google Scholar]
- 39.Pinilla I, Larrosa JM, Polo V, Honrubia FM. Alpha-tocopherol derivatives in an experimental model of filtering surgery. Ophthalmic Res. 1999;31:440–5. doi: 10.1159/000055569. [DOI] [PubMed] [Google Scholar]
- 40.Meyenberg A, Goldblum D, Zingg JM, Azzi A, Nesaretnam K, Kilchenmann M, Frueh BE. Tocotrienol inhibits proliferation of human Tenon’s 's fibroblasts in vitro: a comparative study with vitamin E forms and mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2005;243:1263–71. doi: 10.1007/s00417-005-1165-2. [DOI] [PubMed] [Google Scholar]
- 41.Kunisaki M, Bursell S, Clermont AC, Ishii H, Ballas LM, Jirousek MR, Umeda F, Nawata H, King GL. Vitamin E prevents diabetes-induced abnormal retinal blood flow via the diacylglycerol-protein kinase C pathway. Am J Physiol. 1995;269:E239–46. doi: 10.1152/ajpendo.1995.269.2.E239. [DOI] [PubMed] [Google Scholar]
- 42.Lee IK, Koya D, Ishi H, Kanoh H, King GL. d-α-tocopherol prevents the hyperglycemia induced activation of diacylglycerol (DAG)-protein kinase C (PKC) pathway in vascular smooth muscle cell by an increase of DAG kinase activity. Diabetes Res Clin Pract. 1999;45:183–90. doi: 10.1016/s0168-8227(99)00048-0. [DOI] [PubMed] [Google Scholar]
- 43.Engin KN, Engin G, Kücükşahin H, Oncu M, Engin G, Guvener B. Clinical evaluation of the neuroprotective effect of α-tocopherol on retına against glaucomatous damage. Eur J Ophthalmol. 2007;17:528–33. doi: 10.1177/112067210701700408. [DOI] [PubMed] [Google Scholar]
- 44.Lee MW, Severson DL. Signal transduction in vascular smooth muscle: Diacylglycerol second messengers and PKC action. Am J Physiol. 1994;267:C659–78. doi: 10.1152/ajpcell.1994.267.3.C659. [DOI] [PubMed] [Google Scholar]
- 45.Newton AC. Regulation of protein kinase C. Curr Opin Cell Biol. 1997;9:161–7. doi: 10.1016/s0955-0674(97)80058-0. [DOI] [PubMed] [Google Scholar]
- 46.Komuro I, Katoh Y, Kaida T, Shibazaki Y, Kurabayashi M, Hoh E, Takaku F, Yazaki Y. Mechanical loading stimulates cell hypertrophy and specific gene expression in cultured rat cardiac myocytes: possible role of protein kinase C expression. J Biol Chem. 1991;266:1265–8. [PubMed] [Google Scholar]
- 47.Boyle WJ, Smeal T, Defize LHK. Activation of protein kinase C decreases proliferation of c-jun at sites that negatively regulate its DNA binding activity. Cell. 1991;64:573–84. doi: 10.1016/0092-8674(91)90241-p. [DOI] [PubMed] [Google Scholar]
- 48.Miano JM, Tota RR, Vlasic N, Danishefsky KJ, Stemerman MB. Early proto-oncogene expression in rat aortic smooth muscle cells following endothelial removal. Am J Pathol. 1990;137:761–5. [PMC free article] [PubMed] [Google Scholar]
- 49.Dominguez I, Sanz L, Arenzana-Seisdedos F, Diaz-Meco MT, Virelizier JL, Moscat J. Inhibition of protein kinase Cζ subspecies blocks the activation of an NFκB−like activity in Xenopus Laevis oocytes. Mol Cell Biol. 1993;13:1290–5. doi: 10.1128/mcb.13.2.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kariya K, Farrance IK, Simpson PC. Transcriptional enhance factor-1 in cardiac myocytes interacts with an α1 adrenergic and β protein kinase C-inducible element in the rat β-myosin heavy chain promoter. J Biol Chem. 1993;268:26658–62. [PubMed] [Google Scholar]
- 51.Bull ND, Barnett NL. Antagonists of protein kinase C inhibit rat retinal glutamate transport activity in situ. J Neurochem. 2002;81:472–80. doi: 10.1046/j.1471-4159.2002.00819.x. [DOI] [PubMed] [Google Scholar]
- 52.Abdel-Latif AA. Cross talk between cyclic AMP and the polyphosphoinositide signaling cascade in iris sphincter and other nonvascular smooth muscle. Proc Soc Exp Biol Med. 1996;211:163–77. doi: 10.3181/00379727-211-43959b. [DOI] [PubMed] [Google Scholar]
- 53.Wiederholt M, Thieme H, Stumpff F. The regulation of trabecular meshwork and ciliary muscle contractility. Prog Retin Eye Res. 2000;19:271–95. doi: 10.1016/s1350-9462(99)00015-4. [DOI] [PubMed] [Google Scholar]
- 54.Alexander JP, Acott TS. Involvement of protein kinase C in TNFalpha regulation of trabecular matrix metalloproteinases and TIMPs. Invest Ophthalmol Vis Sci. 2001;42:2831–8. [PubMed] [Google Scholar]
- 55.Husain S, Abdel-Latif AA. Effects of prostaglandin F(2alpha) and carbachol on MAP kinases, cytosolic phospholipase A(2) and rachidonic acid release in cat iris sphincter smooth muscle cells. Exp Eye Res. 2001;72:581–90. doi: 10.1006/exer.2001.0991. [DOI] [PubMed] [Google Scholar]
- 56.Han Z, Wax MB, Patil RV. Regulation of aquaporin-4 water channels by phorbol ester-dependent protein phosphorylation. J Biol Chem. 1998;273:6001–4. doi: 10.1074/jbc.273.11.6001. [DOI] [PubMed] [Google Scholar]
- 57.Spalton DJ. Posterior capsular opacification after cataract surgery. Eye. 1999;13:489–92. doi: 10.1038/eye.1999.127. [DOI] [PubMed] [Google Scholar]
- 58.Elgohary MA, Hollick EJ, Bender LE, Heatley CJ, Wren SM, Boyce J, Missotten T, Spalton DJ, Dowler JG. Hydrophobic acrylic and plate-haptic silicone intraocular lens implantation in diabetic patients: pilot randomized clinical trial. J Cataract Refract Surg. 2006;32:1188–95. doi: 10.1016/j.jcrs.2006.01.106. [DOI] [PubMed] [Google Scholar]
- 59.Liu CSC, Duncan G, Wormstone IM, Marcantonio JM, Webb SF, Davies PD. Strategies to prevent lens cell growth causing posterior capsule opacification: An in vitro study. Invest Ophthalmol Vis Sci. 1996;37:906–14. [PubMed] [Google Scholar]
- 60.Behar-Cohen FF, David T, D'Hermies F, Pouliquen YM, Buechler Y, Nova MP, Houston LL, Courtois Y. In vivo inhibition of lens regrowth by fibroblast growth factor 2-saporin. Invest Ophthalmol Vis Sci. 1995;36:2434–48. [PubMed] [Google Scholar]
- 61.Apple DJ, Solomon KD, Tetz MR, Assia EI, Holland EY, Legler UF, Tsai JC, Castaneda VE, Hoggatt JP, Kostick AM. Posterior capsular opacification. Surv Ophthalmol. 1992;37:73–116. doi: 10.1016/0039-6257(92)90073-3. [DOI] [PubMed] [Google Scholar]
- 62.Cammarata PR, Fan W, Jin Y, Yorio T. Protein kinase C activity and its relationship to myo-inositol uptake during hyperglycemic conditions in cultured bovine lens epithelial cells. Curr Eye Res. 1993;12:403–12. doi: 10.3109/02713689309024622. [DOI] [PubMed] [Google Scholar]
- 63.Wagner LM, Takemoto DJ. PKCalpha and PKCgamma overexpression causes lentoid body formation in the N/N 1003A rabbit lens epithelial cell line. Mol Vis. 2001;7:138–44. [PubMed] [Google Scholar]
- 64.Sidjanin D, Grdina D, Woloschak GE. UV-induced changes in cell cycle and gene expression within rabbit lens epithelial cells. Photochem Photobiol. 1996;63:79–85. doi: 10.1111/j.1751-1097.1996.tb02995.x. [DOI] [PubMed] [Google Scholar]
- 65.Seth RK, Haque MS, Zelenka PS. Regulation of c-fos induction in lens epithelial cells by 12(S)HETE-dependent activation of PKC. Invest Ophthalmol Vis Sci. 2001;42:3239–46. [PubMed] [Google Scholar]
- 66.Alvarez LJ, Candia OA. Na(+)-Cl(-)-K+ cotransport activity in cultured bovine lens epithelial cells and its absence in intact bovine lenses. Exp Eye Res. 1994;58:479–90. doi: 10.1006/exer.1994.1041. [DOI] [PubMed] [Google Scholar]
- 67.Reynhout JK, Lampe PD, Johnson RG. An activator of protein kinase C inhibits gap junction communication between cultured bovine lens cells. Exp Cell Res. 1992;198:337–42. doi: 10.1016/0014-4827(92)90388-o. [DOI] [PubMed] [Google Scholar]
- 68.Saleh SM, Takemoto DJ. Overexpression of protein kinase Cgamma inhibits gap junctional intercellular communication in the lens epithelial cells. Exp Eye Res. 2000;71:99–102. doi: 10.1006/exer.2000.0847. [DOI] [PubMed] [Google Scholar]
- 69.Wagner LM, Saleh SM, Boyle DJ, Takemoto DJ. Effect of protein kinase Cgamma on gap junction disassembly in lens epithelial cells and retinal cells in culture. Mol Vis. 2002;8:59–66. [PubMed] [Google Scholar]
- 70.van den Eijnden-van Raaij AJ, Feijen A, Snoek GT. EDTA-extractable proteins from calf lens fiber membranes are phosphorylated by Ca2+-phospholipid-dependent protein kinase. Exp Eye Res. 1987;45:215–25. doi: 10.1016/s0014-4835(87)80145-8. [DOI] [PubMed] [Google Scholar]
- 71.Andersson M, Sjostrand J, Karlsson JO. Calpains in the human lens: relations to membranes and possible role in cataract formation. Ophthalmic Res. 1996;28(Suppl 1):51–4. doi: 10.1159/000267944. [DOI] [PubMed] [Google Scholar]
- 72.Sylvester PW, McIntyre BS, Gapor A, Briski KP. Vitamin E inhibition of normal mammary epithelial cell growth is associated with a reduction in protein kinase C(alpha) activation. Cell Prolif. 2001;34:347–57. doi: 10.1046/j.1365-2184.2001.00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Avunduk AM, Yardimci S, Avunduk MC, Kurnaz L, Aydin A, Kockar MC, Delibasi T, Dayanir V. Prevention of lens damage associated with cigarette smoke exposure in rats by alpha-tocopherol (vitamin E) treatment. Invest Ophthalmol Vis Sci. 1999;40:537–41. [PubMed] [Google Scholar]