Abstract
More severe hip fractures such as displaced femoral neck (FN) fractures and unstable intertrochanteric (IT) fractures lead to poorer outcomes, but risk factors for severe fractures have not been studied. To identify risk factors for severe types of hip fracture, we performed a prospective cohort study and obtained preoperative hip radiographs from women who sustained an incident hip fracture (excluding traumatic fractures). A single radiologist scored the severity of FN fractures by the Garden System: grades I and II, undisplaced; grades III and IV, displaced. The severity of IT hip fractures was rated by the Kyle System: grades I and II, stable; grades III and IV, unstable. A total of 249 women had FN fractures: 75 (30%) were undisplaced. A total of 213 women had IT fractures: 59 (28%) were stable. Both types of hip fracture increased with age, but older age was even more strongly associated with more severe hip fractures. Low BMD was more strongly related to undisplaced FN fractures (p interaction BMD × FN type, p = 0.0008) and stable IT fractures (p interaction BMD × IT type, p = 0.04). Similar findings were observed for estimated volumetric BMD and hip geometric parameters. Corticosteroid use was only associated with displaced FN fractures, and Parkinson's disease was only associated with stable IT fractures. Little difference was reported in the self-reported circumstances surrounding each type of fracture. In conclusion, the lower the BMD, the greater the likelihood of experiencing a hip fracture that is less displaced and more stable.
Key words: hip fracture, severity, intertrochanteric, femoral neck, osteoporosis, Kyle-Garden classification
INTRODUCTION
Numerous studies have evaluated hip fracture as if it were a homogenous condition,(1,2) when indeed it includes two distinct anatomical types: fractures of the femoral neck (FN) and fractures of the intertrochanteric (IT) region. FN and IT fractures account for >90% of hip fractures and occur in almost equal proportions.(3,4) Given the fact that the bone composition differs at each site, it is possible that the etiology of the fracture may also differ. The trochanteric region has a greater proportion of trabecular bone compared with the FN region (50% versus 25%).(5) FN fractures are positioned in the area distal to the femoral head but proximal to the greater and lesser trochanters; they are considered intracapsular fractures.(6) The IT fractures, however, occur between the greater and lesser trochanters, are extracapsular fractures, and do not typically present with the healing complications characteristic of FN fractures.(6)
Some, but not all, studies have shown that risk factors for the two most common anatomical types of hip fracture, FN and IT, are different. Several studies have shown that BMD is significantly lower among women with IT fractures compared with FN fractures.(7–12) In the Study of Osteoporotic Fractures (SOF), we previously showed that both low FN BMD and increased functional difficulty increased the risk of both FN and IT fractures.(13) Moreover, corticosteroid use and impaired functional status seemed to be stronger predictors for FN, rather than IT, fractures, whereas poor health status was a stronger predictor for IT than FN fractures.(13) In addition, others have shown that women with IT fractures were thinner, older, and often had a history of vertebral fractures compared with women with a FN fracture.(10,14) Greenspan et al.,(8) however, did not show an association between fall characteristics, sex, age, body habitus, and type of hip fracture. These apparent differences in risk factors for FN and IT fractures are important to recognize because outcomes and treatment options may differ.(15–17)
FN fractures may also be characterized by whether they are displaced (proximal and distal fragments altered from their normal alignment) or not. Displacement may be graded using the Garden System, in which grade I and II fractures are considered together as nondisplaced and grade III and IV fractures are considered together as displaced. Using these criteria, ∼70% of FN fractures are categorized as displaced.(1,2) This distinction is clinically important because most of the vascular supply to the femoral head lies along the surface of the FN, and FN fractures, especially those that are displaced, pose a higher risk for disrupting this blood supply.(11,12) In turn, this may lead to an increased risk of postfracture healing complications such as avascular necrosis of the femoral head or nonunion of the fracture.(13) IT fractures are classified by the Kyle System: grades I and II, stable; grades III and IV, unstable.(18)
At present, little is known about whether risk factors for fracture vary by severity of hip fracture. To examine the proportion of FN hip fractures that are displaced and the proportion of IT fractures that are unstable, we examined data from SOF, a multicenter, community-based study of a cohort of ambulatory older women. From this, we evaluated whether risk factors for a hip fracture differed in their relationship to hip fractures by radiographic severity using the Garden and Kyle Systems for FN and IT fractures, respectively. In addition, we examined whether the circumstances surrounding the fracture were important predictors of the severity of hip fracture that occurred.
MATERIALS AND METHODS
Subjects
The SOF is a prospective cohort study of risk factors for fractures in older women. From September 1986 to October 1988, women who were at least 65 yr of age were recruited from population-based listings in four areas of the United States: Portland, OR; Minneapolis, MN; Baltimore, MD; and the Monongahela Valley near Pittsburgh, PA. A detailed description of recruitment procedures are outlined elsewhere.(19) Black women were initially excluded from SOF because of their low incidence of hip fracture. We also excluded women who were unable to walk without assistance of another person and women with a history of bilateral hip replacement. The study protocol was approved by the institutional review committee, and all subjects gave written informed consent.
Measurement of bone mass
Between November 1988 and December 1990, the women were invited for a follow-up examination that included a DXA scan of the proximal femur (Hologic 1000; Hologic, Bedford, MA, USA). The right hip was scanned in all cases except in the event of right hip replacement or severe degenerative change. Areal BMD was determined for the FN and IT region. The in vivo CV between centers was 1.2% for the FN, and the interscanner CV was 0.9% for an anthropometric hip phantom and <1% at the IT region.(18)
To test whether a volumetric measurement of BMD is a stronger predictor of severity of hip fracture, we calculated the FN and IT bone mineral apparent density (BMAD) using the formula BMD/area2 (g/cm3).
Hip structural analysis
The hip structural analysis (HSA) program uses the distribution of mineral mass in a line of pixels across the bone axis to measure geometric properties of cross-sections in cut planes traversing the bone at that location.(20,21) Current versions average measurements for five parallel mass profiles spaced ∼1 mm apart along the bone axis, effectively corresponding to a 5-mm section thickness. Analysis locations for this analysis were the narrow neck (NN) region across the narrowest point of the FN and IT region across the bisector of the neck shaft angle.
BMD, bone cross-sectional area (CSA, i.e., surface area of bone in the cross-section excluding soft tissue voids, equivalent to an estimate of BMC), bone outer diameter (subperiosteal width), and cross-sectional moment of inertia (CSMI) were measured directly from mineral mass distributions using algorithms described previously.(21) Section modulus was calculated as CSMI divided by the greater of the measured distances from the center of mass to the medial or lateral surface.
Assumptions of cross-sectional shape are needed for estimates of average cortical thickness and buckling ratio, an approximate index of cortical instability.(22) Buckling ratios were calculated as the ratio of maximum distance from the center of mass to the outer cortical margin divided by the mean cortical thickness. As in previous studies, cortices of the narrow neck and shaft regions were modeled as circular annuli with 60% and 100% of the measured mass in the cortex, respectively.(21) The IT estimate assumes an elliptical annulus with 70% of the measured bone mass in the cortex, and the anteroposterior diameter is assumed to be the subperiosteal diameter of the shaft region. The HSA program also measures the femur neck length and the neck shaft angle, which influence the effective bending moment in a fall. CVs measured for geometric properties on a similar QDR1000 scanner ranged from 0.8% to 4.7%, averaging 2.2% in a study by Nelson et al.(23) and from 1.8% to 7.2% in a study by Khoo et al.(24) that included osteoporotic women only.
Assessment of fractures
To ascertain fractures, participants were asked to notify the local clinical center as soon as possible after any fracture. Participants were also contacted every 4 mo by letter or telephone to ask whether they had sustained a fracture. These contacts were >95% complete. After receiving a report of a fracture, clinic staff interviewed participants about the type of fracture and how it occurred. Copies of radiological reports were obtained for all reported fractures. We obtained preoperative radiographs on 462 incident nontraumatic hip fractures. These radiographs were classified according to type and severity by a single radiologist (H.K.G.).
At present, the two most common classification systems include the Garden System for FN fractures, which classifies fractures according to the degree of displacement,(25) and the Kyle System, which categorizes with respect to stability and degree of displacement.(26) FN fractures were classified using the Garden System: grades I and II, undisplaced; grades III and IV, displaced(25). Grade I is an incomplete fracture line, the distal fragment is in external rotation, the proximal fragment is in valgus, and the trabeculae form a 180° angle with the femoral cortex. Grade II fractures have a complete oblique line through the FN, the capital fragment is undisplaced, and the distal fragment has a normal alignment with the proximal fragment. The femoral head internal area trabeculae make an angle of ∼160° with those of the femoral cortex. Grade III fractures have a complete fracture line with partial displacement <50%. The distal fragment is in external rotation, and the proximal fragment is tilted into varus and rotated medially. Consequently, the medial trabeculae of the femoral head are not in alignment with those of the pelvis because of the fragment rotation. Grade IV fractures have a complete fracture line with fragment displacement >50% and dissociation; consequently, the capital fragment is detached from the distal fragment and has retuned to its normal position in the acetabulum. The medial trabeculae of the head now are in alignment with those of the pelvis. The distal fragment is displaced proximally and is in full lateral rotation.
IT hip fractures are classified by the Kyle System: grades I and II, stable; grades III and IV, unstable. A grade I IT fracture is a stable undisplaced IT line fracture; grade II is a stable displaced IT line fracture with varus deformity and includes fractures of the lesser trochanter; grade III is an unstable displaced fracture of the greater trochanter with posterior medial comminution and varus deformity; and grade IV is an unstable displaced comminuted fracture of the greater trochanter and intersubtrochanteric regions with posterior medial comminution with a subtrochanteric component.(26)
Circumstances of the fracture
Women were interviewed about the circumstances of the fracture. We collected information on whether the fracture occurred because of a fall, height of the fall (greater than standing height or less), activity before the fall, direction of the fall, surface of impact, body part landed on, and whether they tried to break their fall with their hand. We also collected information on intrinsic factors related to a fall (dizziness, alcohol consumption, use of sleep medications) and where the fall occurred (indoors/outdoors).
Predictor variables
Participants were asked to complete a self-administered questionnaire and were interviewed and examined at clinical centers. Information was collected on maternal history of hip fracture, history of two or more falls in the previous 12 mo, pregnancy, type of menopause, walking for exercise, on feet >4 h/d, and weight at age 25. These factors have previously been associated with hip fractures.(19) A history of selected medical conditions was obtained by asking participants whether a physician had ever told them that they had the given condition. Diseases included in this analysis included Parkinsonism, diabetes, osteoporosis, and previous fractures including hip, wrist, and spine. Detailed information was obtained on past and present health habits, including cigarette consumption, alcohol intake, and physical activity. Physical activity was estimated using a modified Paffenbarger scale that assesses participation in a wide variety of activities.(27)
Participants were asked to bring all medications with them to the clinic for verification of use. Medications considered for this analysis included estrogen, calcium, and corticosteroid use. Calcium intake was assessed using the method developed from the NHANES II survey.(28) Weight was measured in indoor clothing with shoes removed using a balance beam scale, and height was recorded with a wall-mounted Harpenden Stadiometer.(29) Contrast sensitivity was determined using the Vistech Contrast Sensitivity Test System.(30) Five spatial frequencies (1.5, 3.0, 6.0, 12.0, and 18.0 cycles/°) were tested at a 10-ft (3.048 m) distance. The measure of contrast sensitivity used in the analysis was the average of the contrast scores at all five frequencies. Contrast sensitivity assessed whether the women could differentiate different degrees of gray according to Ginsburg's test. Near depth perception was assessed using the Randot Circles method(31) and was expressed as a numeric score (highest number box for which the subject chose the correct circle twice).
Grip strength was measured using a hand dynamometer (Preston Grip dynamometer; Takei Kikikogyo, Tokyo, Japan); strength of the dominant hand was used in this analysis. Quadriceps extensor strength was measured on the subject's right side in a supine position (Body Master), and the best performance of two trials was used in this analysis. Walking speed was measured as the average time to complete two trials on a standard 6-m course. Inter-rater reliability of these measurements was as follows: grip strength, r = 0.93; walking speed, r = 0.84. Walking speed was measured as the average time to complete two trials on a standard 6-m course.
Statistical analyses
FN hip fractures were divided into two categories: grades I and II (undisplaced) and grades III and IV (displaced); IT fractures were grouped into grades I and II (stable) and grades III and IV (unstable). Initially we compared characteristics of participants by the severity of hip fracture versus no hip fracture using t-tests and χ2. We also compared the characteristics of women with undisplaced versus displaced FN hip fracture and stable versus unstable IT hip fractures.
We calculated the incidence rate (per 1000 person-years) of each type of FN and IT fracture across 5-yr age groups. To identify risk factors for each type of hip fracture, predictor variables were selected based on their past association with hip fractures from previous studies and included the following: age, weight, weight change from age 25 (baseline weight − weight at age 25), height, height at age 25, history of fracture, maternal hip fracture, estrogen use, calcium use, corticosteroid use, caffeine intake, alcohol intake, diabetes, Parkinson's disease, two or more falls in the last year, ever pregnant, surgical menopause, and take walks for exercise.(32–34) Cox proportional hazards models were used to calculate the HR and 95% CI. The unit for the HR for continuous variables corresponded to 1 SD. Women without a hip fracture were the referent group. These models were used to examine predictor variables on the risk of displaced and undisplaced FN and stable and unstable IT fractures, versus no hip fracture, separately. We initially adjusted for age. Multivariable adjusted models were run with and without BMD. Risk factors/predictor variables were entered into multivariate (MV) models if they were significant at p < 0.05 in age-adjusted models. Tests for interaction between BMD and severity of hip fracture were carried out using the competing risk analysis.(35)
To test whether estimated volumetric BMD (BMAD) or measures of hip geometry estimated by the HSA are related to type and severity of hip fracture, we analyzed the HR of 1 SD decrease (or increase; e.g., buckling ratio) in each skeletal parameter in age-adjusted and MV models. The variables included in these MV models were identified from the previously described modeling procedures. We limited this analysis to those HSA parameters that were shown to predict hip fractures in SOF.(36)
Cox proportional hazards regression models were computed to examine the effect of the predictor variables on the risk of displaced versus undisplaced FN fractures and in unstable versus stable IT fractures. Individual risk factors were adjusted for age. Subjects with no hip fracture were excluded from these later models. HRs >1 indicated that the displaced and unstable fractures were more likely than undisplaced or stable fractures. Finally, we compared the circumstance of FN fractures (undisplaced versus displaced) and IT fractures (stable versus unstable) by χ2.
We compared circumstance of fractures by severity of hip fracture using χ2 tests. For these analyses, we combined severe FN and IT fractures (grades II and IV) and less severe FN and IT fractures (grades I and II) together.
RESULTS
Participant characteristics
Over the first 10.5 yr of follow-up, 462 first incident hip fractures were reported and included in this analysis. Of these, 249 were FN fractures: 75 (30%) undisplaced and 174 (70%) displaced. A total of 213 were IT fractures: 59 (28%) stable and 154 (72%), unstable. Women having an FN fracture tended to be older, weighed less, gained less weight since age 25, were more likely to reported a previous fracture and a maternal history of hip fracture, less likely to consume alcohol, be ever pregnant and have a surgical menopause, and had lower grip and quadriceps strengths, slower walking speed, compromised vision as measured by contrast sensitivity and near depth perception, and lower BMD than women without hip fracture (Table 1). There were no differences in a woman's current height, estrogen use, calcium supplement use, caffeine intake, history of diabetes, diagnosis of Parkinson's disease, two or more falls last year, being on feet <4 h/d, or pulse rate when comparing women having an undisplaced or displaced FN fracture to those without a hip fracture (Table 1). Comparing women with undisplaced versus displaced hip fractures showed few differences except that women with undisplaced FN fractures were less likely to walk for exercise (p = 0.04).
Table 1.
Baseline Characteristics by FN Hip Fracture Grade vs. no Hip Fracture
| Undisplaced (grade I and II fracture) (N = 75) | Displaced (grade III and IV fracture) (N = 174) | No hip fracture (N = 8696) | |
| Age (yr) | 73.8 ± 5.2* | 74.1 ± 5.4* | 71.3 ± 5.1 |
| Weight (kg) | 62.2 ± 9.7† | 64.3 ± 11.7† | 67.5 ± 12.5 |
| Weight change from age 25 (kg) | 6.9 ± 9.5† | 9.6 ± 14.2 | 11.2 ± 11.1 |
| Height (cm) | 158.5 ± 6.9 | 159.6 ± 6.4 | 159.1 ± 6.0 |
| Height at age 25 (cm) | 162.9 ± 6.5 | 163.8 ± 6.4‡ | 162.5 ± 5.9 |
| History of fracture (yes) | 51.4%‡ | 49.1%* | 34.6% |
| Maternal hip fracture (yes) | 21.1% | 17.0% | 12.8% |
| Estrogen use (yes) | 8.1% | 11.2% | 14.2% |
| Calcium intake (yes) | 44.0% | 42.4% | 42.0% |
| Steroid use (yes) | 2.7% | 4.0%§ | 1.8% |
| Caffeine intake (mg/day) | 0.15 ± 0.14 | 0.17 ± 0.14 | 0.16 ± 0.14 |
| Alcohol use (yes) | 65.3% | 62.6%§ | 70.8% |
| Diabetes (yes) | 6.7% | 8.1% | 7.0% |
| Parkinson's (yes) | 1.3% | 0.6% | 0.5% |
| 2+ falls last year (yes) | 14.7% | 13.3% | 10.1% |
| Ever pregnant (yes) | 81.1% | 74.7%† | 84.4% |
| Surgical menopause (yes) | 7.1% | 8.4% | 12.7% |
| Take walk for exercise (yes) | 38.7%§ | 52.9% | 50.8% |
| On feet <4 h/d (yes) | 14.7% | 11.5% | 9.3% |
| Walking speed (m/s) | 0.93 ± 0.22† | 0.95 ± 0.20* | 1.03 ± 0.22 |
| Grip strength (kg) | 18.3 ± 4.8* | 20.0 ± 4.5† | 21.1 ± 4.3 |
| Quadriceps strength (kg) | 50.0 ± 19.9‡ | 52.8 ± 23.3‡ | 59.8 ± 25.6 |
| Pulse rate (beats/min) | 70.4 ± 10.6 | 70.0 ± 10.7 | 68.9 ± 10.1 |
| Near depth perception¶ | 4.2 ± 2.9§ | 4.3 ± 3.0† | 5.0 ± 2.9 |
| Contrast sensitivity | 1.02 ± 0.50† | 1.09 ± 0.51† | 1.24 ± 0.58 |
| Femoral neck BMD (g/cm2) | 0.55 ± 0.07* | 0.59 ± 0.09* | 0.66 ± 0.11 |
| Femoral neck BMAD (g/cm3) | 0.11 ± 0.03* | 0.12 ± 0.03* | 0.14 ± 0.03 |
| Intertrochanteric BMD (g/cm2) | 0.78 ± 0.12* | 0.80 ± 0.14* | 0.89 ± 0.16 |
| Intertrochanteric BMAD (g/cm3) | 0.04 ± 0.01* | 0.04 ± 0.01* | 0.04 ± 0.01 |
| Neck length (cm) | 4.24 ± 0.70 | 4.32 ± 0.58 | 4.33 ± 0.62 |
| Neck-shaft angle (degree) | 129.6 ± 6.0‡ | 128.6 ± 5.8§ | 127.2 ± 6.0 |
| Narrow neck buckling ratio | 16.12 ± 3.62* | 15.11 ± 2.99* | 12.80 ± 3.09 |
| Narrow neck cortical thickness (cm) | 0.11 ± 0.02* | 0.12 ± 0.02* | 0.14 ± 0.03 |
| Narrow neck CSA (cm2) | 1.83 ± 0.29* | 1.93 ± 0.33* | 2.09 ± 0.38 |
| Narrow neck CSMI (cm4) | 1.61 ± 0.48 | 1.69 ± 0.40 | 1.71 ± 0.51 |
| Narrow neck sectional module (cm3) | 0.90 ± 0.19† | 0.96 ± 0.19‡ | 1.02 ± 0.23 |
| Narrow neck width (cm) | 3.23 ± 0.37† | 3.21 ± 0.23* | 3.10 ± 0.29 |
Values are mean ± SD or percent.
* p < 0.0001 vs. no hip fracture.
† p < 0.001 vs. no hip fracture.
‡ p < 0.01 vs. no hip fracture.
§ p < 0.05 vs. no hip fracture.
¶ Number correct twice.
Similar results were observed when comparing both stable and unstable IT fractures to women with no hip fracture (Table 2). Women who experienced an IT fracture were older, weighed less, gained less weight since age 25, were shorter, were more likely to report a history of fracture, maternal history of fracture, Parkinson's disease, were less likely to report alcohol consumption, be ever pregnant and have a surgical menopause, had worse vision as measured by contrast sensitivity, and near depth perception, lower grip and quadriceps strengths, slower walking speed, and lower BMD compared with women with no hip fracture.
Table 2.
Baseline Characteristics by IT Hip Fracture Grade vs. no Hip Fracture
| Stable (grade I and II fracture) (N = 59) | Unstable (grade III and IV fracture) (N = 154) | No hip fracture (N = 8696) | |
| Age (yr) | 75.1 ± 6.0* | 76.4 ± 6.3* | 71.3 ± 5.1 |
| Weight (kg) | 61.6 ± 11.8† | 65.9 ± 12.7 | 67.5 ± 12.5 |
| Weight change from age 25 | 6.8 ± 9.1‡ | 8.9 ± 11.2§ | 11.2 ± 11.1 |
| Height (cm) | 156.9 ± 6.1‡ | 157.5 ± 6.7‡ | 159.1 ± 6.0 |
| Height at age 25 (cm) | 162.1 ± 6.0 | 162.8 ± 6.3 | 162.5 ± 5.9 |
| History of fracture (yes) | 54.2%‡ | 50.0%* | 34.6% |
| Maternal hip fracture (yes) | 22.7%§ | 18.3% | 12.8% |
| Estrogen use (yes) | 8.5% | 11.8% | 14.2% |
| Calcium use (yes) | 50.9% | 44.4% | 42.0% |
| Steroid use (yes) | 3.5% | 3.4% | 1.8% |
| Caffeine use (mg/day) | 0.19 ± 0.15 | 0.15 ± 0.14 | 0.16 ± 0.14 |
| Alcohol use (yes) | 66.1% | 60.8%‡ | 70.8% |
| Diabetes (yes) | 3.4% | 9.7% | 7.0% |
| Parkinson's (yes) | 3.4%‡ | 1.3% | 0.5% |
| 2+ falls last year (yes) | 15.3% | 11.7% | 10.1% |
| Ever pregnant (yes) | 79.7% | 72.7%* | 84.4% |
| Surgical menopause (yes) | 3.8% | 8.8% | 12.7% |
| Take walk for exercise (yes) | 52.5% | 44.2% | 50.8% |
| On feet <4 h/d (yes) | 10.2% | 11.0% | 9.3% |
| Walking speed (m/s) | 0.97 ± 0.22 | 0.93 ± 0.18* | 1.03 ± 0.22 |
| Grip strength (kg) | 19.0 ± 3.6† | 19.2 ± 4.2* | 21.1 ± 4.3 |
| Quadriceps strength (kg) | 47.6 ± 25.3‡ | 48.3 ± 24.1* | 59.8 ± 25.6 |
| Pulse rate (beats/min) | 70.0 ± 10.1 | 68.8 ± 9.3 | 68.9 ± 10.1 |
| Near depth perception¶ | 4.7 ± 3.1 | 3.9 ± 2.8* | 5.0 ± 2.9 |
| Contrast sensitivity | 0.97 ± 0.45† | 0.98 ± 0.56* | 1.24 ± 0.58 |
| Femoral neck BMD (g/cm2) | 0.56 ± 0.11* | 0.59 ± 0.10* | 0.66 ± 0.11 |
| Femoral neck BMAD (g/cm3) | 0.12 ± 0.04‡ | 0.12 ± 0.03* | 0.14 ± 0.03 |
| Intertrochanteric BMD (g/cm2) | 0.73 ± 0.15* | 0.78 ± 0.13* | 0.89 ± 0.16 |
| Intertrochanteric BMAD (g/cm3) | 0.03 ± 0.01* | 0.03 ± 0.01* | 0.04 ± 0.01 |
| Neck length (cm) | 4.15 ± 0.62 | 4.19 ± 0.63§ | 4.33 ± 0.62 |
| Neck-shaft angle (degree) | 127.3 ± 6.6 | 127.2 ± 5.7 | 127.2 ± 6.0 |
| Intertrochanter buckling ratio | 14.94 ± 3.84* | 14.09 ± 3.41* | 11.17 ± 2.74 |
| Intertrochanter cortical thickness (cm) | 0.22 ± 0.05* | 0.23 ± 0.05* | 0.28 ± 0.06 |
| Intertrochanter CSA (cm2) | 2.92 ± 0.63* | 3.13 ± 0.59* | 3.63 ± 0.71 |
| Intertrochanter CSMI (cm4) | 8.77 ± 2.41† | 9.42 ± 2.34‡ | 10.11 ± 2.53 |
| Intertrochanter sectional module (cm3) | 2.78 ± 0.71* | 2.99 ± 0.66* | 3.34 ± 0.74 |
| Intertrochanter width (cm) | 5.60 ± 0.40‡ | 5.62 ± 0.35* | 5.45 ± 0.34 |
Values are mean ± SD or percent.
* p < 0.0001 vs. no hip fracture.
† p < 0.001 vs. no hip fracture.
‡ p < 0.01 vs. no hip fracture.
§ p < 0.05 vs. no hip fracture.
¶ Number correct twice.
Comparing women with stable versus unstable IT fractures showed that women with a stable fracture weighted ∼4 kg less than women with an unstable IT fracture (p = 0.03). Parkinson's disease was also more common among women with a stable IT fracture compared with unstable IT, but it was not significant.
Age associations with hip fractures
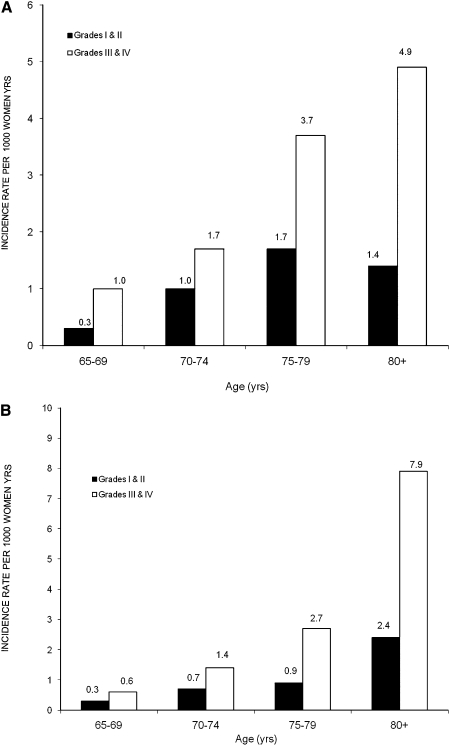
A 5-yr increase in age was associated with an increased risk of both types of FN hip fractures (HR = 1.70 [1.40, 2.06] and 1.81 [1.59, 2.05] for grades I and II and grades III and IV, respectively, in age-adjusted models). When we examined the association of FN fracture severity across 5-yr increments in age, there was an increase in the incidence rate (per 1000 person-years) of displaced FN fractures from 1.0 in women 65–69 yr of age to an incidence rate of 4.9 in women ≥80 yr of age (Fig. 1A). At every age, displaced fractures were more common, especially among the oldest women.
FIG. 1.
(A) Incidence rate of FN hip fractures by age: grades I and II (undisplaced) vs. grades III and IV (displaced) per 1000 woman-years. (B) Incidence rate of IT hip fractures by age: grades I and II (stable) vs. grades III and IV (unstable) per 1000 woman-years.
Each 5-yr increase in age was associated with a 2-fold increased risk of stable IT fracture (HR = 2.10 [1.70, 2.59]) and a 2.4 times increased risk of unstable IT fracture (HR = 2.42 [2.14, 2.75]). The incidence of both stable and unstable IT hip fractures increased with age (Fig. 1B) in unadjusted models. Unstable fractures were particularly common in women age 80+.
BMD associations with hip fractures
There were site-specific differences in BMD for both FN and IT hip fractures. Women with an undisplaced FN fracture had an ∼7% lower FN BMD compared with those with a displaced fracture (p = 0.002; Table 1). The magnitude of this difference was about one third of 1 SD. In contrast, IT BMD was similar in the two groups of FN hip fracture cases (p = 0.43). For IT fractures, IT BMD was ∼6.8% lower in stable versus unstable IT fractures (p = 0.03; Table 2), but the difference in FN BMD was not significant (p = 0.11).
FN hip fractures
In age-adjusted models, lower body weight, positive history of fracture, lower quadriceps strength, slower walking speed, and lower BMD were associated with an increased risk of both undisplaced and displaced FN hip fractures (Table 3). Several risk factors showed different relationships between undisplaced and displaced FN hip fractures. Each SD increase in height at age 25 was associated with a 30% increased risk of displaced FN hip fracture. Corticosteroid use was associated with a 2.5 times increased risk of displaced FN fracture. Alcohol consumption and parity were protective for displaced FN fractures. On the other hand, a 1 SD decrease in grip strength was associated with an 80% increased risk of an undisplaced FN hip fracture but was unrelated to displaced FN fracture. Similarly, greater weight loss and poor vision as measured by contrast sensitivity was associated with an increased risk of undisplaced FN hip fractures. Whereas low BMD increased the risk of both severe and not severe FN fractures, the association was much stronger for the less severe FN fracture. Each SD decrease in FN BMD was associated with a >3-fold increased risk of an undisplaced fracture but with a 94% increased risk of a displaced fracture (p interaction = 0.0008).
Table 3.
Risk Factors for Undisplaced (Grade I and II) and Displaced (Grade III and IV) FN Hip Fracture vs. no Hip Fracture
| Variable (unit)* | Age adjusted [HR (95% CI)] | MV adjusted without BMD [HR (95% CI)] | MV adjusted with BMD [HR (95% CI)] | |
| Undisplaced (grade I and II) | ||||
| Age (5 yr) | — | 1.28 (0.98, 1.67) | 1.09 (0.83, 1.44) | |
| Weight (−12.5 kg) | 1.61 (1.21, 2.13) | 1.45 (0.88, 2.38) | 0.97 (0.58, 1.62) | |
| Weight change from age 25 (−11.1 kg) | 1.51 (1.16, 1.96) | 1.17 (0.73, 1.85) | 1.11 (0.69, 1.77) | |
| Height at age 25 (5.93 cm) | — | — | — | |
| History of fracture (yes) | 1.90 (1.20, 3.00) | 1.31 (0.76, 2.25) | 1.03 (0.59, 1.81) | |
| Maternal hip fracture (yes) | 1.85 (0.98, 3.49) | — | — | |
| Steroid use (yes) | — | — | — | |
| Alcohol use (yes) | — | — | — | |
| Ever pregnant (yes) | — | — | — | |
| Surgical menopause (yes) | — | — | — | |
| Take walks for exercise (yes) | 0.64 (0.40, 1.02) | — | — | |
| Quadriceps strength (−25.6 kg) | 1.41 (1.05, 1.88) | 1.05 (0.75, 1.46) | 0.98 (0.70, 1.38) | |
| Walking speed (−0.22 m/s) | 1.49 (1.18, 1.87) | 1.29 (0.95, 1.75) | 1.22 (0.90, 1.65) | |
| Grip strength (−4.3 kg) | 1.81 (1.44, 2.28) | 1.48 (1.09, 2.03) | 1.44 (1.06, 1.95) | |
| Near depth perception (2.94) † | 1.24 (0.98, 1.56) | — | — | |
| Contrast sensitivity (−0.58) | 1.42 (1.06, 1.89) | 1.14 (0.83, 1.58) | 1.07 (0.77, 1.47) | |
| Femoral neck BMD (−0.11 g/cm2) | 3.57 (2.60, 4.89) | — | 3.26 (2.20, 4.84) | |
| Displaced (grade III and IV) | ||||
| Age (5 yr) | — | 1.55 (1.31, 1.83) | 1.38 (1.16, 1.65) | |
| Weight (−12.5 kg) | 1.25 (1.05, 1.49) | 1.29 (1.03, 1.62) | 0.95 (0.75, 1.21) | |
| Weight change from age 25 (−11.1 kg) | 1.10 (0.93, 1.29) | — | — | |
| Height at age 25 (5.93 cm) | 1.30 (1.12, 1.51) | 1.35 (1.12, 1.64) | 1.28 (1.05, 1.56) | |
| History of fracture (yes) | 1.71 (1.27, 2.31) | 1.41 (0.98, 2.02) | 1.24 (0.86, 1.81) | |
| Maternal hip fracture (yes) | — | — | — | |
| Steroid use (yes) | 2.56 (1.20, 5.46) | 2.98 (1.38, 6.42) | 2.98 (1.38, 6.43) | |
| Alcohol use (yes) | 0.72 (0.53, 0.98) | 0.64 (0.44, 0.93) | 0.67 (0.46, 0.99) | |
| Ever pregnant (yes) | 0.64 (0.45, 0.90) | 0.74 (0.48, 1.13) | 0.72 (0.46, 1.10) | |
| Surgical menopause (yes) | 0.70 (0.40, 1.21) | — | — | |
| Take walks for exercise (yes) | — | — | — | |
| Quadriceps strength (−25.6 kg) | 1.22 (1.01, 1.48) | 1.15 (0.93, 1.41) | 1.14 (0.92, 1.41) | |
| Walking speed (−0.22 m/s) | 1.30 (1.11, 1.51) | 1.24 (1.02, 1.52) | 1.19 (0.96, 1.46) | |
| Grip strength (−4.3 kg) | 1.16 (0.99, 1.37) | — | — | |
| Near depth perception (2.94)† | 1.16 (1.00, 1.35) | — | — | |
| Contrast sensitivity (−0.58) | 1.14 (0.96, 1.36) | — | — | |
| Femoral neck BMD (−0.11 g/cm2) | 1.94 (1.58, 2.38) | — | 2.00 (1.56, 2.57) | |
Values in bold are statistically significant.
* Relative hazard per SD decrease for continuous variable.
† Number correct twice.
In MV-adjusted models with or without BMD, lower grip strength was associated with a >40% increased risk of undisplaced FN hip fractures. A 1 SD decrease in FN BMD was associated with a >3-fold increased risk of undisplaced FN hip fracture. Older age and lower walking speed were marginally associated with an increased risk of undisplaced fractures, but these associations were completely attenuated in models with BMD.
Older age, lower body weight, taller height at age 25, corticosteroid use, slower walking speed, and alcohol consumption were independently associated with an increased risk of displaced FN hip fractures (Table 3). Further adjustment for BMD attenuated the association with body weight and walking speed.
Displaced versus undisplaced FN hip fracture
We tested predictors of displaced versus undisplaced fractures, and no variables were able to discriminate the two types of FN hip fracture (Table 1).
IT fractures
In age-adjusted models, a positive fracture history, maternal history of hip fracture, reduced quadriceps and grip strength, less weight change, and poor vision were associated with an increased risk of stable and unstable IT hip fractures, Table 4. Low body weight, Parkinson's disease, and poor vision were associated with an increased risk of stable IT hip fractures but not unstable IT hip fractures; slower walking speed and alcohol consumption were associated with unstable IT hip fractures only. Similar to what we observed for FN hip fractures, lower BMD was associated with an increased risk of both types of IT hip fractures, but the association was much stronger for stable IT hip fractures (p interaction = 0.04).
Table 4.
Risk Factors for Stable (Grade I and II) and Unstable (Grade III and IV) IT Fractures
| Variable (unit)* | Age adjusted [HR (95% CI)] | MV adjusted without BMD [HR (95% CI)] | MV adjusted with BMD [HR (95% CI)] | |
| Stable (grade I and II) | ||||
| Age (5 yr) | — | 1.12 (0.79, 1.59) | 1.03 (0.71, 1.49) | |
| Weight (−12.5 kg) | 1.69 (1.22, 2.35) | 1.29 (0.69, 2.41) | 0.90 (0.46, 1.74) | |
| Weight change from age 25 (−11.1 kg) | 1.48 (1.10, 1.99) | 1.42 (0.79, 2.57) | 1.09 (0.61, 1.97) | |
| Height at age 25 (5.93 cm) | 1.26 (0.97, 1.64) | — | — | |
| History of fracture (yes) | 2.05 (1.23, 3.43) | 2.58 (1.27, 5.23) | 1.96 (0.93, 4.12) | |
| Maternal hip fracture (yes) | 2.03 (1.00, 4.11) | 2.43 (1.12, 5.27) | 1.91 (0.84, 4.34) | |
| Alcohol use (yes) | — | — | — | |
| Parkinson's disease (yes) | 5.15 (1.25, 21.2) | 8.91 (2.02, 39.4) | 9.09 (2.09, 39.5) | |
| Ever pregnant (yes) | — | — | — | |
| Surgical menopause (yes) | 0.31 (0.07, 1.25) | — | — | |
| Quadriceps strength (−25.6 kg) | 1.55 (1.10, 2.19) | 1.36 (0.90, 2.06) | 1.17 (0.76, 1.79) | |
| Walking speed (−0.22 m/s) | 1.12 (0.86, 1.47) | — | — | |
| Grip strength (−4.3 kg) | 1.44 (1.09, 1.89) | 1.05 (0.69, 1.60) | 1.00 (0.64, 1.54) | |
| Near depth perception (2.94)† | — | — | — | |
| Contrast sensitivity (−0.58) | 1.42 (1.02, 1.98) | 1.83, (1.13, 2.97) | 1.64 (1.01, 2.68) | |
| Intertrochanteric BMD (−0.16 g/cm2) | 3.23 (2.27, 4.59) | — | 3.17 (1.90, 5.29) | |
| Unstable (grade III and IV) | ||||
| Age (5 yr) | — | 2.11 (1.74, 2.56) | 1.87 (1.53, 2.29) | |
| Weight (−12.5 kg) | — | — | — | |
| Weight change from age 25 (−11.1 kg) | 1.08 (0.91, 1.29) | — | — | |
| Height at age 25 (5.93 cm) | 1.06 (0.90, 1.25) | — | — | |
| History of fracture (yes) | 1.65 (1.20, 2.27) | 1.71 (1.11, 2.63) | 1.41 (0.90, 2.21) | |
| Maternal hip fracture (yes) | 1.61 (1.00, 2.59) | 1.70 (0.98, 2.94) | 1.67 (0.94, 2.94) | |
| Alcohol use (yes) | 0.72 (0.52, 0.99) | 0.67 (0.44, 1.04) | 0.64 (0.41, 1.00) | |
| Parkinson's disease (yes) | — | — | — | |
| Ever pregnant (yes) | 0.63 (0.44, 0.90) | 0.66 (0.41, 1.05) | 0.59 (0.37, 0.95) | |
| Surgical menopause (yes) | — | — | — | |
| Quadriceps strength (−25.6 kg) | 1.34 (1.09, 1.65) | 1.23 (0.95, 1.61) | 1.13 (0.85, 1.49) | |
| Walking speed (−0.22 m/s) | 1.31 (1.11, 1.55) | 1.27 (1.00, 1.61) | 1.29 (1.01, 1.65) | |
| Grip strength (−4.3 kg) | 1.26 (1.06, 1.49) | 1.05 (0.81, 1.35) | 1.04 (0.80, 1.35) | |
| Near depth perception (2.94)† | 1.17 (0.99, 1.38) | — | — | |
| Contrast sensitivity (−0.58) | 1.22 (1.00, 1.49) | — | — | |
| Intertrochanteric BMD (−0.16 g/cm2) | 1.79 (1.47, 2.18) | — | 1.83 (1.42, 2.37) | |
Values in bold are statistically significant.
* Relative hazard per SD decrease for continuous variable.
† Number correct twice.
In MV models with and without BMD, Parkinson's disease was associated with a 9-fold increased risk of stable IT hip fractures. Adjustment for BMD had little effect on this association. Poor vision as measured by contrast sensitivity was also associated with an increased risk of stable IT hip fractures, independent of BMD. In multivariable models without BMD, both positive fracture history and maternal history of hip fracture were associated with an ∼2.5-fold increased risk of stable IT fractures, but adjustment for BMD attenuated these associations and they were not significant.
Older age, slower walking speed, and lower BMD were independently associated with an increased risk of unstable IT hip fractures (Table 4). Positive fracture history was associated with a 70% increased risk of unstable hip fracture, but this association was no longer significant in models adjusting for BMD. Both alcohol consumption and positive pregnancy history were associated with a lower risk of unstable IT fractures after adjusting for BMD.
Unstable versus stable IT fracture
A 5-yr increase in age was associated with an increased risk of unstable IT fracture (HR = 1.15 [1.02, 1.32]) and faster walking speed an increased risk of unstable IT hip fracture (HR= 1.19 [1.01, 1.41]) compared with stable IT fractures. Women who reported a positive pregnancy history (HR = 0.65 [0.45, 0.94]) and walking for exercise (HR = 0.68 [0.49, 0.93]) were less likely to have an unstable IT hip fracture compared with women with a stable IT hip fracture.
Estimated volumetric BMD and hip geometry (HSA)
We repeated the age and MV models substituting BMAD and the HSA variables previously shown to predict hip fracture.(36) As shown in Tables 5 (FN fractures) and 6 (IT fractures), results were fairly consistent with results using areal BMD. In general, the relationships between each skeletal parameter were stronger for the less severe hip fracture. The interactions between severity of FN fracture and BMAD (p = 0.02) and between severity of IT fracture and CSA (p = 0.07) were significant. All other interactions were not significant.
Table 5.
HR (95% CI) for FN Hip Fracture per 1 SD Decrease in BMAD and HSA Variables
| Variable | Age adjusted [HR (95% CI)] | MV adjusted with skeletal parameter [HR (95% CI)] |
| Undisplaced (grade I and II) | ||
| Femoral neck BMAD | 3.09 (2.07, 4.62) | 2.46 (1.61, 3.76) |
| Narrow neck | ||
| Buckling ratio* | 2.07 (1.71, 2.50) | 1.96 (1.54, 2.48) |
| Cortical thickness | 3.37 (2.30, 4.95) | 2.90 (1.85, 4.53) |
| CSA | 2.30 (1.62, 3.26) | 1.89 (1.24, 2.88) |
| CSMI | 1.22 (0.90, 1.66) | 1.00 (0.73, 1.38) |
| Section modulus | 1.85 (1.34, 2.57) | 1.56 (1.07, 2.28) |
| Width* | 1.46 (1.16, 1.83) | 1.53 (1.21, 1.94) |
| Neck shaft angle* | 1.50 (1.15, 1.96) | 1.53 (1.15, 2.02) |
| Displaced (grade III and IV) | ||
| Femoral neck BMAD | 1.60 (1.28, 2.00) | 1.41 (1.11, 1.81) |
| Narrow neck | ||
| Buckling ratio* | 1.71 (1.49, 1.97) | 1.68 (1.42, 1.98) |
| Cortical thickness | 2.02 (1.60, 2.53) | 2.10 (1.59, 2.77) |
| CSA | 1.51 (1.22, 1.87) | 1.58 (1.21, 2.06) |
| CSMI | 1.03 (0.86, 1.23) | 1.02 (0.83, 1.26) |
| Section modulus | 1.28 (1.05, 1.56) | 1.29 (1.02, 1.63) |
| Width* | 1.38 (1.18, 1.61) | 1.36 (1.13, 1.62) |
| Neck shaft angle* | 1.27 (1.07, 1.51) | 1.22 (1.01, 1.48) |
For undisplaced fractures, MV was adjusted for age, fracture history, contrast sensitivity, grip strength, weight, weight change since age 25, gait speed, and quadriceps strength; for displaced fractures, MV was adjusted for age, fracture history, alcohol consumption, weight height at age 25, pregnancy history, gait sped, steroid use, quadriceps.
* Per 1 SD increase.
Table 6.
HR (95% CI) for IT Hip Fracture per 1 SD Decrease in BMAD and HSA Variables
| Variable | Age adjusted [HR (95% CI)] | MV adjusted with skeletal parameter [HR (95% CI)] |
| Stable (grade I and II) | ||
| Intertrochanteric BMAD | 3.89 (2.45, 6.20) | 3.29 (1.81, 6.00) |
| Intertrochanteric | ||
| Buckling ratio* | 1.97 (1.65, 2.34) | 1.74 (1.35, 2.25) |
| Cortical thickness | 3.53 (2.31, 5.40) | 3.60 (1.94, 6.67) |
| CSA | 3.48 (2.29, 5.22) | 4.21 (2.22, 7.97) |
| CSMI | 1.79 (1.23, 2.61) | 1.92 (1.04, 3.55) |
| Section modulus | 2.35 (1.60, 3.43) | 2.53 (1.41, 4.53) |
| Width* | 1.46 (1.09, 1.97 | 1.65 (1.09, 2.50) |
| Neck shaft angle* | 1.04 (0.77, 1.42) | 0.93 (0.62, 1.37) |
| Unstable (grade III and IV) | ||
| Intertrochanteric BMAD | 2.36 (1.83, 3.06) | 2.54 (1.83, 3.53) |
| Intertrochanteric | ||
| Buckling ratio* | 1.66 (1.48, 1.87) | 1.64 (1.41, 1.90) |
| Cortical thickness | 2.35 (1.86, 2.96) | 2.28 (1.69, 3.07) |
| CSA | 2.00 (1.60, 2.50) | 1.88 (1.41, 2.51) |
| CSMI | 1.24 (1.01, 1.52) | 1.10 (0.84, 1.43) |
| Section modulus | 1.54 (1.25, 1.90) | 1.39 (1.06, 1.83) |
| Width* | 1.48 (1.24, 1.76) | 1.59 (1.27, 1.98) |
| Neck shaft angle* | 1.03 (0.86, 1.24) | 1.16 (0.93, 1.44) |
For stable fractures, MV model was adjusted for age, fracture history, maternal history of hip fracture, contrast sensitivity, grip strength weight, weight change since age 25, Parkinson's disease, and quadriceps strength; for unstable fractures, MV model was adjusted for age, fracture history, maternal hisory of hip fracture, alcohol consumption, grip strength, ever pregnant, gait speed, and quadriceps strength.
* Per 1 SD increase.
Circumstances of falls and hip fractures
Ninety-seven percent of all the hip fractures occurred because of a fall; ∼15% were from a fall above a standing height, but this did not differ by severity. There were also no differences in the direction of the fall, the activity before the fall, the part of the body landed on, the type of surface where it occurred, location of fall, and intrinsic factors such as the use of alcohol or sedatives before the fracture by severity of hip fracture (Table 7). The only circumstances that differed by severity was whether the woman landed on her hands when she fell or whether she tried to break the fall with her hand. A lower proportion of women who reported landing on her hand or using her hand to break the fall experienced a severe hip fracture.
Table 7.
Circumstances of Combined Fractures or of Falls That Caused Fractures
| Grades I and II | Grades III and IV | p | |
| Degree of trauma | 0.37 | ||
| Less than standing height | 83.1% | 81.9% | |
| Higher than standing height | 15.4% | 14.0% | |
| Direction of fall | 0.08 | ||
| Forward | 15.9% | 7.2% | |
| Straight down | 6.4% | 7.5% | |
| Laterally | 38.1% | 39.9% | |
| Posteriorly | 11.9% | 14.3% | |
| Other/don't know | 27.8% | 31.1% | |
| Activity before fall | 0.79 | ||
| Sits/lies/bends/reaches/transfers | 32.1% | 36.6% | |
| Running/climbing/up and down stairs | 11.5% | 10.3% | |
| Walking | 40.5% | 36.6% | |
| Other | 16.0% | 16.6% | |
| Part of body landed on | 0.16 | ||
| Front | 12.7% | 6.1% | |
| Side | 48.4% | 53.2% | |
| Back | 12.7% | 14.3% | |
| Don't know | 26.2% | 26.3% | |
| Surface of impact | 0.44 | ||
| Wood/linoleum/carpet | 65.9% | 63.5% | |
| Ceramic tile/cement | 25.4% | 22.2% | |
| Snow/ice/dirt | 4.0% | 5.8% | |
| Intermediary object | 4.8% | 8.5% | |
| Location of fall | 0.39 | ||
| Away from home | 24.4% | 20.3% | 0.34 |
| Outdoor | 19.9% | 23.1% | |
| Intrinsic | 0.82 | ||
| Dizziness | 3.2% | 3.4% | 0.28 |
| Alcohol | 2.3% | 1.6% | 0.69 |
| Sleep medications | 13.0% | 10.3% | |
| Land on hand when fell | 0.007 | ||
| Yes | 15.9% | 7.9% | |
| No | 25.4% | 37.9% | |
| Don't know | 58.7% | 54.3% | |
| Tried to break fall with hand | 0.06 | ||
| Yes | 22.2% | 14.0% | |
| No | 20.6% | 28.3% | |
| Don't know | 57.1% | 57.7% |
DISCUSSION
Contrary to our hypothesis, we found that lower hip BMD is associated with less severe FN and IT fractures. Perhaps, the lower the BMD, the weaker the mechanical forces that are necessary to cause the hip fractures, thereby leading to less displacement and more stable fractures. This suggests that a greater degree of trauma required to fracture a hip with higher bone mass may lead to a more severe displaced and unstable type of fracture. This indicates that prevention of hip fractures may be as—or more—beneficial in women who have a high risk of hip fracture for reasons besides very low hip BMD.
The clinical importance of distinguishing between the type and severity of hip fracture is apparent in the formulation of potentially fracture-specific treatment modalities. For example, displacement of an FN fracture may be an important determinant of treatment(15) compared with the treatment of a stable IT fracture.(16) Outcomes may also vary by the severity of the hip fracture. In a recent study by Cornwall et al.,(17) mortality was the lowest for patients with undisplaced FN fractures and highest for patients with displaced FN fractures. After 6 mo of follow-up, functional outcome was the best for those who experienced an undisplaced FN fracture and the worst for patients with unstable IT fractures. Of interest, only preinjury function was an independent predictor of functional outcome or mortality, rather than fracture type.
Other skeletal factors may also determine the severity and type of hip fracture. The ability of proximal femur geometry parameters, for example, to distinguish between FN and trochanteric fractures in comparison with other osteoporotic fractures was studied by Gnudi et al.(37) Gnudi et al.(37) reported proximal femur geometry parameters including hip axis length, FN shaft angle, and FN diameter were statistically different in subjects with a vertebral fractures in comparison with hip fractures. However, this study did not distinguish the type or severity of hip fracture. We estimated hip geometry from DXA scans using HSA. Our results are consistent with the findings with aBMD that the geometric parameters were more strongly linked with the less severe type of hip fracture, although interaction terms were mostly not significant.
Older age was associated with an increased incidence of both FN and IT fractures irrespective of severity. However, in MV models, age was no longer significantly associated with the less severe fractures. Previously in SOF(13) and elsewhere,(16) it was reported that older women are especially predisposed to IT fractures. However, our results suggest that older age is, indeed, related to displaced FN fractures.(16) The relative proportion of undisplaced FN fractures may account for the age differences observed between FN and IT fractures. Taller height was associated with an increased risk of displaced (not undisplaced) FN fractures, which may reflect greater trauma. The impact of the fall may be greater in taller people leading to more displacement.
The high fracture risk associated with chronic corticosteroid therapy is well established.(38,39) We previously reported that corticosteroid use was associated with an increased risk of FN fractures.(13) These findings suggest that corticosteroid use is specifically associated with more severe displaced FN fractures. This association was independent of BMD and likely reflects the negative effects of glucocorticoids on osteoblasts and osteocytes, which adversely affects the architecture of bone, and ultimately, the strength of bone.(40)
Previously in SOF, poor functional ability was largely related to FN hip fractures.(13) We examined several measures of functional ability, including grip and quadriceps strengths and walking speed. These results suggest that poor functional ability as measured by lower grip strength was an independent predictor of undisplaced FN fracture and was unrelated to displaced FN fracture. This is consistent with our observation that women who reported landing on her hand or using her hand to break the fall were more likely to experience an undisplaced fracture. Lower grip strength may result in an inability to break the impact of the fall, thus leading to an undisplaced FN fracture.
Alcohol consumption was associated with a lower risk of both displaced FN fractures and unstable IT fractures. Previous studies have shown that moderate alcohol consumption (<2 drinks/d) has a positive association with bone mass in women.(41) The mechanism is unclear, but it likely reflects a “healthy user” effect, because moderate alcohol consumption is associated with lower total mortality.(42)
Parkinson's disease was a strong risk factor for stable IT fractures. This observation is consistent with a previous finding that Parkinson's disease was a risk factor for subsequent hip fracture; however, in this paper, these associations were attenuated and no longer significant after MV adjustment, in particular, body weight.(43) In addition, these previous results were based on the combination of FN and IT fractures, despite the fact that 73% of all hip fractures in women with Parkinson's disease were IT. Our results show that Parkinson's disease increases the risk of stable IT fractures in particular, and this increased risk is independent of body weight and BMD.
Poor vision as measured by contrast sensitivity and slower walking speed were also predictors of IT fractures. Poor vision, Parkinson's disease, and poor mobility are associated with an increased risk of falls(44–46) and, hence, fall-related factors may especially increase the risk of IT fractures. The observation that positive pregnancy history reduces the risk of IT fracture is consistent with our observation that parity reduces hip fracture.(47)
The type and severity of fracture could also be attributed to the rotation angle of the leg at the moment it has contact with the floor. Nevitt and Cummings,(48) for example, have supported the idea that the nature of a fall determines the type of fracture. We collected a variety of information on the circumstances of the fall surrounding the hip fracture. Except for falling on the hand or using the hand to break the fall, none of these circumstances differentiated the severity of the fracture.
There are several limitations to our analysis. Our results are limited to older white women and may not be generalized to other population groups. Women were interviewed about the circumstances surrounding the fracture for up to 6 mo after their hip fracture, and recall bias could have influenced our findings. Many women could not recall the specific circumstances of their fracture. Women were more likely to have a displaced or unstable hip fractures, and we had limited power to identity risk factors for undisplaced and stable hip fractures. Reliability of the classification systems used for IT fractures is not well established.(49) For any classification system, the observer's experience may be one of the more important factors impacting reliability. In one study, the system used to classify IT fractures was shown to be more reliable than the Kyle System.(49) We used a single trained radiologist to review all of the radiographs for this study.
The Garden System is the most common FN fracture classification system. In a recent survey of 298 orthopedic surgeons across North America and Europe, 72% supported the Garden System as the primary FN fracture classification system.(50) Ninety-six percent of surgeons reported that they could differentiate between undisplaced (Garden grades I and II) and displaced (Garden grades III and IV) fractures. At present, the use of four categories of the Garden System is not implemented because of poor reliability and value in distinguishing between grades I and II or grades II and IV. Additionally, in a Canadian study by Beimers et al.,(51) it was concluded that the original four-stage Garden System was unreliable and that fractures should be categorized as stable and unstable fractures.
In conclusion, lower BMD is associated with an absolute increased risk of hip fracture; however, the relative percentage of these fractures is less likely to be severe radiographically. It is possible that the lower the BMD, the weaker the mechanical forces that are needed to cause the hip fracture, thus leading to less displacement and more stable fractures. Parkinson's disease was associated with an increased risk of less severe fractures, perhaps reflecting the shuffling, slower gait of women with Parkinson's disease and the lower impact of a fall in these subjects. Corticosteroid use resulted in an increased risk of the more severe fractures, independent of BMD. This finding may reflect other aspects of bone strength weakened by the steroids that might predispose someone to a more severe hip fracture. The findings from this study emphasize the heterogeneity of hip fractures and underscore the need to further understand risk factors that differentially increase the risk for more severe hip fractures.
ACKNOWLEDGMENTS
The Study of Osteoporotic Fractures (SOF) was supported by the National Institutes of Health (NIH) funding under the following grant numbers: AG05407, AR35582, AG05394, AR35584, and AR35583 for 20 yr. The competing renewal of SOF (2006) is supported by Public Health Service grants from the National Institute of Aging (NIA) under the following grant numbers: AG005407, AG027576, AG005394, and AG027574.
APPENDIX: INVESTIGATORS IN THE STUDY OF OSTEOPOROTIC FRACTURES RESEARCH GROUP
San Francisco Coordinating Center (California Pacific Medical Center Research Institute and University of California San Francisco): S. R. Cummings (principal investigator), M. C. Nevitt (co-investigator), D. C. Bauer (co-investigator), D. M. Black (co-investigator), K. L. Stone (co-investigator), W. Browner (co-investigator), R. Benard, T. Blackwell, P. M. Cawthon, L. Concepcion, M. Dockrell, S. Ewing, M. Farrell, C. Fox, R. Fullman, S. L. Harrison, M. Jaime-Chavez, W. Liu, L. Lui, L. Palermo, N. Parimi, M. Rahorst, D. Kriesel, C. Schambach, R. Scott, J. Ziarno.
University of Maryland: M. C. Hochberg (principal investigator), R. Nichols (clinic coordinator), S. Link.
University of Minnesota: K. E. Ensrud (principal investigator), S. Diem (co-investigator), M. Homan (co-investigator), P. Van Coevering (program coordinator), S. Fillhouer (clinic director), N. Nelson (clinic coordinator), K. Moen (assistant program coordinator), F. Imker-Witte, K. Jacobson, M. Slindee, R. Gran, M. Forseth, R. Andrews, C. Bowie, N. Muehlbauer, S. Luthi, K. Atchison.
University of Pittsburgh: J. A. Cauley (principal investigator), L. H. Kuller (co-principal investigator), J. M. Zmuda (co-investigator), L. Harper (project director), L. Buck (clinic coordinator), M. Danielson (project administrator), C. Bashada, D. Cusick, A. Flaugh, M. Gorecki, M. Nasim, C. Newman, N. Watson.
The Kaiser Permanente Center for Health Research, Portland, Oregon: T. Hillier (principal investigator), K. Vesco (co-investigator), K. Pedula (co-investigator), J. Van Marter (project director), M. Summer (clinic coordinator), A. MacFarlane, J. Rizzo, K. Snider, J. Wallace.
Footnotes
Dr. Cauley has received research support from Merck, Eli Lilly & Co., Pfizer Pharmaceuticals, Procter & Gamble, and Novartis Pharmaceuticals. She has also received consulting fees from Novartis Pharmaceuticals. Dr. Genant has corporate appointments from Synarc; consulting fees from Merck, Eli Lilly & Co., Amgen, Servier, GlaxoSmithKline, and Roche and stock ownership from Synarc. Dr. Bauer has received research support from Novartis Pharmaceuticals, Amgen, and Procter & Gamble and honoraria from Merck and Roche. All other authors state that they have no conflicts of interest.
REFERENCES
- 1.Greenspan SL, Myers ER, Maitland LA, Resnick NM, Hayes WC. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. JAMA. 1994;271:128–133. [PubMed] [Google Scholar]
- 2.Kelsey JL, Hoffman S. Risk factors for hip fracture. N Engl J Med. 1987;316:404–406. doi: 10.1056/NEJM198702123160709. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher JC, Melton LJ, Riggs BL, Bergstrath E. Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res. 1980:163–171. [PubMed] [Google Scholar]
- 4.Alffram PA. An epidemiologic study of cervical and trochanteric fractures of the femur in an urban population. Analysis of 1,664 cases with special reference to etiologic factors. Acta Orthop Scand Suppl. 1964;65(Suppl 65):61–109. doi: 10.3109/ort.1964.35.suppl-65.01. [DOI] [PubMed] [Google Scholar]
- 5.Riggs BL, Wahner HW, Seeman E, Offord KP, Dunn WL, Mazess RB, Johnson KA, Melton LJ., III Changes in bone mineral density of the proximal femur and spine with aging. Differences between the postmenopausal and senile osteoporosis syndromes. J Clin Invest. 1982;70:716–723. doi: 10.1172/JCI110667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 7.Lips P, Netelenbos JC, Jongen MJ, van Ginkel FC, Althuis AL, van Schaik CL, van der Vijgh WJ, Vermeiden JP, van der Meer C. Histomorphometric profile and vitamin D status in patients with femoral neck fracture. Metab Bone Dis Relat Res. 1982;4:85–93. doi: 10.1016/0221-8747(82)90021-2. [DOI] [PubMed] [Google Scholar]
- 8.Greenspan SL, Myers ER, Maitland LA, Kido TH, Krasnow MB, Hayes WC. Trochanteric bone mineral density is associated with type of hip fracture in the elderly. J Bone Miner Res. 1994;9:1889–1894. doi: 10.1002/jbmr.5650091208. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson SA, Widhe TL. Bone mass in women with hip fracture. Acta Orthop Scand. 1988;59:19–23. doi: 10.3109/17453678809149337. [DOI] [PubMed] [Google Scholar]
- 10.Vega E, Mautalen C, Gomez H, Garrido A, Melo L, Sahores AO. Bone mineral density in patients with cervical and trochanteric fractures of the proximal femur. Osteoporos Int. 1991;1:81–86. doi: 10.1007/BF01880448. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura N, Kyou T, Takaoka K, Ohzono K, Ono K. Bone mineral density in the proximal femur and hip fracture type in the elderly. J Bone Miner Res. 1992;7:755–759. doi: 10.1002/jbmr.5650070705. [DOI] [PubMed] [Google Scholar]
- 12.Duboeuf F, Hans D, Schott AM, Kotzki PO, Favier F, Marcelli C, Menuier PJ, Delmas PD. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: The EPIDOS Study. J Bone Miner Res. 1997;12:1895–1902. doi: 10.1359/jbmr.1997.12.11.1895. [DOI] [PubMed] [Google Scholar]
- 13.Fox KM, Cummings SR, Williams E, Stone K. Femoral neck and intertrochanteric fractures have different risk factors: A prospective study. Osteoporos Int. 2000;11:1018–1023. doi: 10.1007/s001980070022. [DOI] [PubMed] [Google Scholar]
- 14.Mautalen CA, Vega EM, Einhorn TA. Are the etiologies of cervical and trochanteric hip fractures different? Bone. 1996;18(Suppl):133S–137S. doi: 10.1016/8756-3282(95)00490-4. [DOI] [PubMed] [Google Scholar]
- 15.Baumgaertner MR. Femoral neck fractures. In: Bucholz RW, Heckman JD, editors. Rockwood and Green's Fractures in Adults. Philadelphia, PA, USA: Lippincott Williams & Williams; 1991. pp. 1579–1634. [Google Scholar]
- 16.Koval KJ. Intertrochanteric fractures. In: Bucholz RW, Heckman JD, editors. Rockwood and Green's Fractures in Adults vol. 2001. Philadelphia, PA, USA: Lippincott Williams & Williams; 2001. pp. 1635–1663. [Google Scholar]
- 17.Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: A function of patient characteristics. Clin Orthop Relat Res. 2004:64–71. doi: 10.1097/01.blo.0000132406.37763.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steiger P, Cummings SR, Black DM, Spencer NE, Genant HK. Age-related decrements in bone mineral density in women over 65. J Bone Miner Res. 1992;7:625–632. doi: 10.1002/jbmr.5650070606. [DOI] [PubMed] [Google Scholar]
- 19.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 20.Beck TJ, Ruff CB, Warden KE, Scott WW, Jr, Rao GU. Predicting femoral neck strength from bone mineral data. A structural approach. Invest Radiol. 1990;25:6–18. doi: 10.1097/00004424-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Beck TJ, Looker AC, Ruff CB, Sievanen H, Wahner HW. Structural trends in the aging femoral neck and proximal shaft: Analysis of the Third National Health and Nutrition Examination Survey dual-energy X-ray absorptiometry data. J Bone Miner Res. 2000;15:2297–2304. doi: 10.1359/jbmr.2000.15.12.2297. [DOI] [PubMed] [Google Scholar]
- 22.Beck TJ, Oreskovic TL, Stone KL, Ruff CB, Ensrud K, Nevitt MC, Genant HK, Cummings SR. Structural adaptation to changing skeletal load in the progression toward hip fragility: The Study of Osteoporotic Fractures. J Bone Miner Res. 2001;16:1108–1119. doi: 10.1359/jbmr.2001.16.6.1108. [DOI] [PubMed] [Google Scholar]
- 23.Nelson DA, Barondess DA, Hendrix SL, Beck TJ. Cross-sectional geometry, bone strength, and bone mass in the proximal femur in black and white postmenopausal women. J Bone Miner Res. 2000;15:1992–1997. doi: 10.1359/jbmr.2000.15.10.1992. [DOI] [PubMed] [Google Scholar]
- 24.Khoo BC, Beck TJ, Qiao QH, Parakh P, Semanick L, Prince RL, Singer KP, Price RI. In vivo short-term precision of hip structure analysis variables in comparison with bone mineral density using paired dual-energy X-ray absorptiometry scans from multi-center clinical trials. Bone. 2005;37:112–121. doi: 10.1016/j.bone.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Garden RS. Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br. 1961;46:630–647. [PubMed] [Google Scholar]
- 26.Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61:216–221. [PubMed] [Google Scholar]
- 27.Paffenbarger RS, Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 28.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 29.Lohman TG, Roche AF, Martorell R. Champaign, Illinois: Human Kinetics Publishers, Inc; 1988. Anthropometric Standardization Reference Manual; p. 177. [Google Scholar]
- 30.Scialfa CT, Adams EM, Giovanetto M. Reliability of the Vistech contrast test system in a life-span adult sample. Optom Vis Sci. 1991;68:270–274. doi: 10.1097/00006324-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Simons K. A comparison of the Frisby, Random-Dot E, TNO, and Randot circles stereotests in screening and office use. Arch Ophthalmol. 1981;99:446–452. doi: 10.1001/archopht.1981.03930010448011. [DOI] [PubMed] [Google Scholar]
- 32.Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, Mascioli SR, Scott JC, Seeley DG, Steiger P, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. Jama. 1990;263:665–668. [PubMed] [Google Scholar]
- 33.Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 34.Melton LJ, Riggs BL. Epidemiology of age-related fractures. In: Avioli LV, editor. The Osteoporotic Syndrome. 2nd ed. New York, NY, USA: Grune and Stratton; 1987. pp. 1–30. [Google Scholar]
- 35.Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;51:524–532. [PubMed] [Google Scholar]
- 36.Kaptoge S, Beck TJ, Reeve J, Stone KL, Hillier TA, Cauley JA, Cummings SR. Prediction of incident hip fracture risk by femur geometry variables measured by hip structural analysis in the Study of Osteoporotic Fractures. J Bone Miner Res. 2008;23:1892–1904. doi: 10.1359/JBMR.080802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gnudi S, Malavolta N, Testi D, Viceconti M. Differences in proximal femur geometry distinguish vertebral from femoral neck fractures in osteoporotic women. Br J Radiol. 2004;77:219–223. doi: 10.1259/bjr/79551075. [DOI] [PubMed] [Google Scholar]
- 38.Shaker JL, Lukert BP. Osteoporosis associated with excess glucocorticoids. Endocrinol Metab Clin North Am. 2005;34:341–356. doi: 10.1016/j.ecl.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 39.van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: A meta-analysis. Osteoporos Int. 2002;13:777–787. doi: 10.1007/s001980200108. [DOI] [PubMed] [Google Scholar]
- 40.Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoid-induced osteoporosis: Pathophysiology and therapy. Osteoporos Int. 2007;18:1319–1328. doi: 10.1007/s00198-007-0394-0. [DOI] [PubMed] [Google Scholar]
- 41.Holbrook TL, Barrett-Connor E. The association of lifetime weight and weight control patterns with bone mineral density in an adult community. Bone Miner. 1993;20:141–149. doi: 10.1016/s0169-6009(08)80023-2. [DOI] [PubMed] [Google Scholar]
- 42.Gronbaek M, Johansen D, Becker U, Hein HO, Schnohr P, Jensen G, Vestbo J, Sorensen TI. Changes in alcohol intake and mortality: A longitudinal population-based study. Epidemiology. 2004;15:222–228. doi: 10.1097/01.ede.0000112219.01955.56. [DOI] [PubMed] [Google Scholar]
- 43.Schneider JL, Fink HA, Ewing SK, Ensrud KE, Cummings SR. The association of Parkinson's disease with bone mineral density and fracture in older women. Osteoporos Int. 2008;19:1093–1097. doi: 10.1007/s00198-008-0583-5. [DOI] [PubMed] [Google Scholar]
- 44.Coleman AL, Stone K, Ewing SK, Nevitt M, Cummings S, Cauley JA, Ensrud KE, Harris EL, Hochberg MC, Mangione CM. Higher risk of multiple falls among elderly women who lose visual acuity. Ophthalmology. 2004;111:857–862. doi: 10.1016/j.ophtha.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 45.Klein BE, Klein R, Knudtson MD, Lee KE. Relationship of measures of frailty to visual function: The Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2003;101:191–196. [PMC free article] [PubMed] [Google Scholar]
- 46.Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: The Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46:58–64. doi: 10.1111/j.1532-5415.1998.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 47.Hillier TA, Rizzo JH, Pedula KL, Stone KL, Cauley JA, Bauer DC, Cummings SR. Nulliparity and fracture risk in older women: The study of osteoporotic fractures. J Bone Miner Res. 2003;18:893–899. doi: 10.1359/jbmr.2003.18.5.893. [DOI] [PubMed] [Google Scholar]
- 48.Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: The study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 1993;41:1226–1234. doi: 10.1111/j.1532-5415.1993.tb07307.x. [DOI] [PubMed] [Google Scholar]
- 49.Jin WJ, Dai LY, Cui YM, Zhou Q, Jiang LS, Lu H. Reliability of classification systems for intertrochanteric fractures of the proximal femur in experienced orthopaedic surgeons. Injury. 2005;36:858–861. doi: 10.1016/j.injury.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 50.Zlowodzki M, Bhandari M, Keel M, Hanson BP, Schemitsch E. Perception of Garden's classification for femoral neck fractures: An international survey of 298 orthopaedic trauma surgeons. Arch Orthop Trauma Surg. 2005;125:503–505. doi: 10.1007/s00402-005-0022-4. [DOI] [PubMed] [Google Scholar]
- 51.Beimers L, Kreder HJ, Berry GK, Stephen DJ, Schemitsch EH, McKee MD, Jaglal S. Subcapital hip fractures: the Garden classification should be replaced, not collapsed. Can J Surg. 2002;45:411–414. [PMC free article] [PubMed] [Google Scholar]