Abstract
Remyelination of the CNS in multiple sclerosis is thought to be important to restore conduction and protect axons against degeneration. Yet the role that remyelination plays in clinical recovery of function remains unproven. Here, we show that cats fed an irradiated diet during gestation developed a severe neurologic disease resulting from extensive myelin vacuolation and subsequent demyelination. Despite the severe myelin degeneration, axons remained essentially intact. There was a prompt endogenous response by cells of the oligodendrocyte lineage to the demyelination, with remyelination occurring simultaneously. Cats that were returned to a normal diet recovered slowly so that by 3–4 months they were neurologically normal. Histological examination of the CNS at this point showed extensive remyelination that was especially notable in the optic nerve where almost the entire nerve was remyelinated. Biochemical analysis of the diet and tissues from affected cats showed no dietary deficiencies or toxic accumulations. Thus, although the etiology of this remarkable disease remains unknown, it shows unequivocally that where axons are preserved remyelination is the default pathway in the CNS in nonimmune-mediated demyelinating disease. Most importantly, it confirms the clinical relevance of remyelination and its ability to restore function.
Keywords: demyelination, irradiated diet, oligodendrocytes, MS
Demyelination of the CNS is a major pathological finding in many acquired and inherited human neurologic disorders. Multiple sclerosis (MS), in particular, is characterized by acute and chronic demyelination, which results in a slowing or block of nerve conduction with subsequent neurologic dysfunction. Both acute and chronic demyelination may lead to axon loss with the eventual clinical progression of the disease to a chronic stage from which clinical recovery does not occur. The CNS can respond to demyelination by endogenous repair or remyelination, with the restoration of nerve conduction to affected fibers (1). Remyelination will also lead to the protection of demyelinated nerve fibers against their loss in ongoing disease as has been shown in both MS (2) and an experimental model of demyelination of the corpus callosum (3). However, it remains unproven whether remyelination alone can lead to complete functional recovery, especially if extensive areas of the CNS are involved. It has been suggested that other mechanisms such as nerve fiber plasticity through the redistribution of sodium channels Nav 1.6 and 1.2 can restore conduction to demyelinated axons and may also be important in functional recovery (4).
To date, there are no models of neurologic dysfunction caused by widespread CNS demyelination that unequivocally define remyelination as the mechanism of functional recovery. Here, we describe a model in the cat in which severe neurologic dysfunction, including ataxia, paresis, paralysis, and vision loss, is seen in pregnant cats fed an irradiated diet. Removal of this diet results in delayed but complete neurologic recovery associated with extensive remyelination along the entire spinal cord and throughout the optic nerve. Axons remain largely intact, proving that remyelination alone of large areas of the CNS can restore function. This finding confirms that remyelination must be a major therapeutic target in MS and the inherited human myelin disorders.
Results
Clinical Signs.
Neurologic dysfunction began approximately 4 months after the introduction of the irradiated diet and presented as a slowly progressive disorder. Cats developed ataxia and paresis of the hindlimbs. These signs worsened and 2 cats became paraplegic. In some cats, vision as tested by the menace reflex was reduced or lost. The neurologic examination, in summary, suggested that these abnormalities were primarily because of spinal cord disease with optic nerve involvement. Over a period of 2–4 months, cats that were returned to a nonirradiated diet gradually recovered ambulation and had a normal neurologic examination with normal vision.
Pathological Changes Seen During Neurologic Dysfunction.
Over the course of observation of this disease, affected tissues from 10 cats during active disease were studied. Gross lesions were not identified in the brain, spinal cord, or other organs in any of the cats. The primary abnormality in the brain and especially the spinal cord was white mater vacuolation. The spinal cord was affected at all levels but most notably in the ventral and lateral columns where demyelinated axons of all sizes were seen scattered throughout the neuropil (Fig. 1). In the dorsal columns, in some cases only mild vacuolation was seen in the fasciculus cuneatus. However, in some cats, the dorsal columns showed changes similar to those in the rest of the spinal white matter and demyelinated axons could be seen in large groups below the pia (Fig. 1). Remarkably, despite the severe vacuolation, axons appeared intact within degenerating myelin sheaths; frequently, macrophages associated with myelin debris were seen within the vacuoles (Fig. 1). The preservation of axons was confirmed in silver-stained sections (see Fig. S1). Although vacuolation and demyelination were profound, axons with thin myelin sheaths indicative of remyelination were also common in areas of myelin degeneration. Remyelination was particularly pronounced in the dorsal column in some cats, where many small-diameter axons with thin myelin sheaths were noted in the presence of ongoing myelin breakdown. In cats that experienced loss of vision, the optic nerves showed extensive myelin degeneration with few intact myelinated fibers remaining (Fig. 2). These changes were more severe than in the spinal cord, with demyelinated axons throughout the entire optic nerve associated with myelin-laden macrophages (Fig. 2).
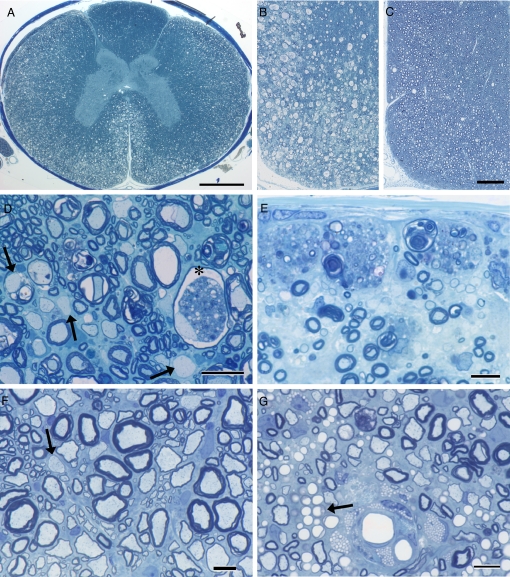
Fig. 1.
Demyelination and remyelination in the spinal cord. During acute disease, extensive changes are seen in the white matter of the spinal cord (A, B, D, and E). In the cervical cord, myelin vacuolation can be seen throughout the lateral and ventral columns (A and B) and on higher power (D). The deeper white matter and dorsal column is less affected (A). Vacuolation of myelin inevitably led to demyelination but with no loss of axons (D). In one myelinated axon, myelin debris is present next to an intact axon (*); other axons can be seen in adjacent fibers undergoing myelin vacuolization. There are numerous scattered remyelinated axons (thin myelin sheaths) and two demyelinated axons (D, arrows). In the dorsal column in a second cat, macrophages filled with myelin debris line the pia above numerous adjacent demyelinated axons. In marked contrast, a cat that had been fed a normal diet for 6 months showed almost complete myelin repair (C and F). Few vacuoles persisted, and the myelinated fiber density appeared normal (C). On higher power (F), it can be seen that many fibers of all diameters were remyelinated with only occasional demyelinated axons remaining (arrow). In 2 cats, although remyelination also was extensive in dorsal columns (G), numerous lipid-filled macrophages persisted adjacent to blood vessels, although many remyelinated axons were also present. There also appeared to be collections of capillaries adjacent to these macrophages (arrow). Toluidine blue. (Scale bars: A, 1.0 mm; B and C, 200 μm; D, 20 μm; E–G, 10 μm.)
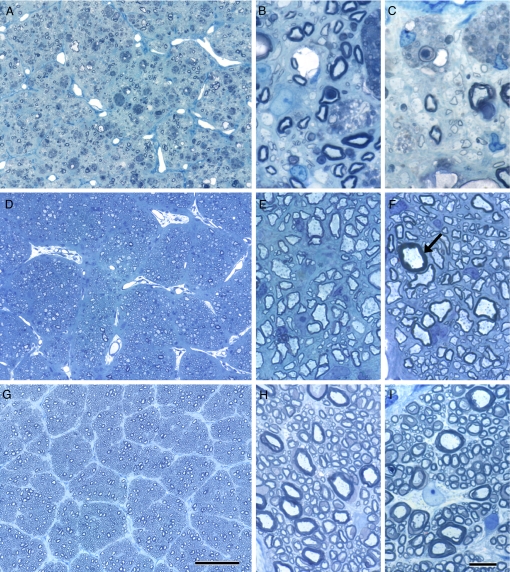
Fig. 2.
Changes in the optic nerve during active disease (A–C), during recovery (D–F), and in controls (G–I). The center of the optic nerve (A) shows almost total myelin loss, representative of changes across the entire optic nerve from the subpial area (B) to the center of the nerve (A and C). Few myelinated fibers remain with many demyelinated axons (arrows) and frequent myelin-filled macrophages (B and C). In contrast, the optic nerve in the recovered cat appears to have an almost normal density of myelinated axons (D–F), although practically all myelin sheaths are thin, both subpial (E) and at the center of the nerve (F) compared with the control cat optic nerve (G–I) sampled at the same levels as the affected and recovered cats (A–F). A single fiber with an intact, thick myelin sheath (F, arrow) represents the only axon not remyelinated. Toluidine blue. (Scale bars: A, D, and G, 100 μm; B, C, E, F, H, and I, 10 μm.)
In the brain, a varying degree of white mater vacuolation was noted in the corona radiata and crus cerebri in all 10 of the cats examined. This finding was also noted although less severe in the corpus callosum in the 2 cats, and in the inferior cerebellar peduncles, caudal colliculi, and pyramidal or medial decussation in individual cases (Fig. S2). Reactive astrogliosis was seen in all cats, with macrophage/microgliosis in most. In both the brain and spinal cord, infrequent perivascular cuffing was seen consisting of predominantly macrophages with less frequent lymphocytes and plasma cells. In contrast to the widespread vacuolation in the CNS, no evidence of myelin pathology was seen in the peripheral nervous system.
Myelin Sheath Changes After Recovery.
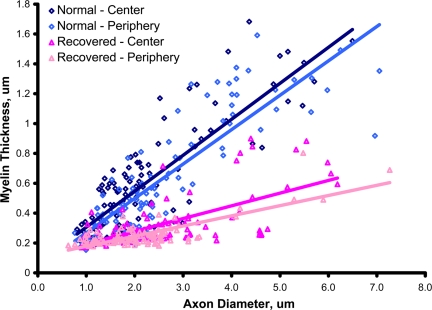
In 2 cases, cats that were no longer fed the irradiated diet for at least 6 months and that had recovered clinically from paraplegia and blindness to being ambulatory and having vision, were studied morphologically. Remarkably, there appeared to be almost total resolution of the vacuolation and demyelination in both the spinal cord and optic nerve (Figs. 1 and 2). In the ventral column, there were many scattered, thinly myelinated (remyelinated) axons present with only a few remaining myelin vacuoles and rare demyelinated axons (Fig. 1). Importantly, the density of myelinated axons appeared normal. Counting the numbers of remyelinated axons in the white matter showed that, in the first cat, 46%, 58%, and 53% of axons in the ventral and lateral white matter of the cervical, thoracic, and lumbar cord, respectively, were remyelinated, compared to 46%, 41%, and 30% of axons in the second cat. In the optic nerve, the density of myelinated axons also appeared normal, but the majority of axons across the entire nerve had thin myelin sheaths compared with the unaffected nerve (i.e., they were all remyelinated) (Fig. 2). Scattered axons with thick myelin sheaths that presumably had not been demyelinated confirmed that the majority were remyelinated. This was confirmed by quantitation, in which it was conclusively shown that the majority of optic nerve axons had thin myelin sheaths (Fig. 3). The g-ratio at both sites of the optic nerves sampled (central and subpial) was significantly different from control; means were 0.789 and 0.793 from the affected cat and 0.654 and 0.677 from control. Occasional demyelinated axons were still present. The only white matter that appeared to have a persistent defect despite clinical resolution was an area within the central dorsal column where scattered demyelinated fibers were seen along with many foamy macrophages (Fig. 1). In these areas, the neuropil appeared gliotic and some axon loss was evident.
Fig. 3.
Myelin sheath thickness is reduced across the optic nerve. Plot of myelin sheath thickness against axon diameter demonstrates a significant difference at both the periphery and center of the nerve. The regression lines are y = 0.241x + 0.0648 (R2 = 0.6926) for normal center; y = 0.2304x + 0.0376 (R2 = 0.7428) for normal periphery; y = 0.0851x + 0.1088 (R2 = 0.4111) for recovered center; and y = 0.0681x + 0.1096 (R2 = 0.6018) for recovered periphery. The differences between wild-type and recovered cat g-ratio in both the center and periphery of the nerve were calculated as significant by the Mann–Whitney rank sum test (P < 0.001).
Discussion
The data presented here provide compelling evidence that global remyelination of the CNS in a severe demyelinating disorder can provide complete restoration of clinical function. Remyelination in this cat model involved the entire spinal cord and optic nerve and likely also certain affected areas of the brain. Although the connection between the irradiated diet, pregnancy, and the extensive myelin degeneration remains unknown, this feline disorder provides an excellent model for future study of endogenous remyelination in vivo by using contemporary imaging techniques and exploration of the cellular and molecular aspects that drive repair.
Definitive proof that remyelination will lead to restoration of function in MS has been largely circumstantial (5), and, in experimental models of demyelination, has not been demonstrated in terms of recovery from overt neurologic disability. In inflammatory disorders of CNS such as MS and experimental autoimmune encephalomyelitis, confounding factors in the pathological milieu that include demyelination, inflammation, gliosis, and axon loss make it difficult to ascribe recovery to the resolution of any one or all of these parameters. Other animal models such as cuprizone toxicity are useful in exploring demyelination and remyelination (6), yet animals given cuprizone and other myelinotoxic chemicals do not demonstrate clear and obvious neurologic dysfunction. In Mice infected with Theiler's virus (7) and in focal demyelinated lesions resulting from ethidium bromide injection (8), behavioral testing (rotarod and beam walking) have been used to show improvement related to remyelination. However, the original deficits were not clinically overt in each case, nor was recovery necessarily complete. Likewise, after cuprizone ingestion, refined behavioral testing was used to show improvement with remyelination (9). The clear difference in our model is that the cats recovered from severe paraparesis or even paraplegia and visual disturbance to being neurologically normal. It appears that the disease we describe here requires some time to develop and resolve. It took 3–4 months of ingesting the irradiated diet to develop neurologic signs and a similar time of resuming a normal diet for disease development and resolution. In regard to repair, despite the fact that active remyelination occurred pari passu with demyelination, it is possible that myelin destruction continued for some time after cessation of the diet, because it took 3–4 months for clinical recovery to occur. Alternatively, remyelination may have been delayed, but this seems less likely given the prominent remyelinating activity seen during the active disease. Further studies, examining various time points after the cessation of the irradiated diet, will be needed to answer this question.
The restoration of the myelin sheath both by endogenous oligodendrocyte precursor cells (OPCs) and from exogenous sources of OPCs or Schwann cells has been shown unequivocally to restore conduction in affected fibers (10, 11). It is clear that the resulting thin myelin sheaths and shorter internodes support fast and secure saltatory conduction, even in axons with as few as 5 lamellae (12). Thus, from a physiological perspective, remyelination is important. However, it is not the only means of recovery, because sodium channel redistribution may also promote slower (continuous) conduction, perhaps forming the basis for the plasticity of the CNS in demyelinating disease (4). Redistribution of ion channels in this model may be unlikely given the apparent prompt remyelination that would lessen the requirement for redistribution of Na channels to promote conduction. In the cat model, recovered cats clearly showed widespread remyelination with very few persistent demyelinated axons, thus confirming that remyelination was the basis of clinical recovery. We also confirm that thinly myelinated axons are sufficient to allow normal function to ensue.
The specificity for the myelin sheath as the target in this disorder is remarkable. Despite the severe myelin vacuolation, axons appeared almost completely unaffected with resultant extensive demyelination. Definitive proof of this comes from the 2 recovered cats, in which the density of myelinated axons appeared normal in both the spinal cord and optic nerve. The only exception to this was in the fasciculus gracilis of the spinal cord, where there was some axon loss and persistent demyelination suggesting a possible reduced OPC recruitment to this site. The failure of total myelin debris removal may have been inhibitory to myelin repair (13) and axon survival. Because the function of axons in this part of the cord is proprioceptive, it is not surprising that these chronic lesions did not result in any clinical deficit. The active remyelination that was seen during the acute disease was remarkable. Thus, endogenous cells in the cat may respond quickly to demyelination. Although the source of these cells is unknown, there is good evidence (14, 15) that an OPC exists in the adult cat CNS, in the optic nerve in particular, and is highly likely the source of remyelinating oligodendrocytes in focal lesions. Here, however, there appears to be little cell death, with only occasional TUNEL-labeled cells, so the question arises as to whether mature oligodendrocytes, stripped of their myelin sheaths, play any role in repair. This would challenge conventional wisdom, which has concluded that remyelination results only from OPC proliferation and differentiation and not adult oligodendrocytes (16), which despite one report (17) are thought to be postmitotic.
A previous report in cats fed an irradiated diet showed some changes similar to those described here, with widespread white matter vacuolation (18). However, there are significant differences including, in our case, the connection between pregnancy and disease development. Additionally, Cassidy et al. (18) described a predominantly axonal disease, whereas we show here that myelin is the target. In the Norwegian silver fox, an inherited disorder resulting in widespread vacuolation with demyelination and remyelination has been reported. However, the distribution of myelin vacuolation is different, and there are other dissimilarities from the cat disorder (19). Myelin vacuolation is a nonspecific finding seen in many other CNS pathologies, ranging from mitochondrial DNA mutations in both humans (20) and animals (21), to a wide spectrum of neurotoxic disorders including hexachlorophene and triethyltin intoxication (22). The key difference, however, between these disorders and that described here is that the myelin vacuolation leads to little demyelination compared with the cat model. The mechanisms of damage to the myelin sheath or oligodendrocytes seen in these diverse disorders appear likely to be different and remain to be determined.
Materials and Methods
Irradiated Diet.
Cats were fed an irradiated diet in a feeding trial first in 1995–1996, and then in a more recent trial. Irradiation of different commercially available diets was carried out by the SteriGenics Radiation Facility (Schaumburg, IL) with a minimum or maximum dose of 25.0 and 50.0 Gy. This diet was being tested for nutritional content in pregnant and lactating cats, but the breeding males and offspring were also fed the same diet. Pregnant cats were maintained throughout gestation and lactation. Analysis of the irradiated diet for macronutrient, minerals, vitamins, and fatty acids compared with nonirradiated diets showed no significant differences. Likewise, sampling of tissue from affected cats, which were analyzed for various vitamins, heavy metals, parathyroid hormone, insulin, ionized calcium, bacterial endotoxins, aflatoxins, and taurine, was all within normal limits. Clinical chemistry examination from affected cats (hematology, blood biochemistry, urinalysis) was all within normal limits. A final feeding trial of 2 irradiated commercial diets compared with the same diets that were autoclaved (15 cats per group) showed that ≈90–95% of pregnant cats on the irradiated diets developed neurologic disease; those that ate more diet developed disease earlier and more severely. Nonpregnant female cats, males and the offspring of females that developed disease postparturition never developed neurologic disease. Neurologic examinations were performed by veterinary neurologists at differing intervals. Attempts to reproduce a similar disorder in pregnant rats fed irradiated rat food were unsuccessful. Methods for animal husbandry and euthanasia in this study were approved by the Institutional Animal Care and Use Committee of Harlan Laboratories.
Histopathology.
Quantitation of myelin sheath abnormalities was carried out as follows. To determine the extent of remyelination in the spinal cords of 2 recovered cats, 1-μm sections of the cervical, thoracic, and lumbar cords were selected, and 3 randomly sampled areas close to the pia of the lateral and ventral columns were photographed at 40× magnification. In each of these areas, myelinated fibers of large and medium caliber were counted and defined as having (i) a normally thick myelin sheath or (ii) a thin myelin sheath defining remyelination. The percentage of remyelinated axons was then calculated in each of the lateral and ventral columns at each level of the cord. In the optic nerves in one of these cats and a control cat, myelin sheath thickness versus axon diameter was measured by using Metavue software at 100× objective magnification with a 2× projection lens. Images were recorded by using a CCD camera. Four randomly selected areas in both the subpial area and in the center of the nerve were photographed from both the normal cat and recovered cats. Axons were measured only if they touched a diagonal line drawn across the photograph. A total of 100 axons was measured from both areas in each cat.
TUNEL Labeling.
Supplementary Material
Acknowledgments.
We are grateful to J. Ramaker, L. Sherrington, and J. Adams for technical support. This work was supported by National Multiple Sclerosis Society Grant TR 3761.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/cgi/content/full/0812500106/DCSupplemental.
References
- 1.Smith KJ, Blakemore WF, McDonald WI. The restoration of conduction by central remyelination. Brain. 1981;104:383–404. doi: 10.1093/brain/104.2.383. [DOI] [PubMed] [Google Scholar]
- 2.Kuhlman T, Lingfeld G, Bitsch A, Schuchardt J, Brück W. Acute axonal damage in multiple sclerosis is most extensive in early disease stages and decreases over time. Brain. 2002;125:2202–2212. doi: 10.1093/brain/awf235. [DOI] [PubMed] [Google Scholar]
- 3.Irvine KA, Blakemore WF. Remyelination protects axons from demyelination-associated axon degeneration. Brain. 2008;131:1464–1477. doi: 10.1093/brain/awn080. [DOI] [PubMed] [Google Scholar]
- 4.Waxman SG. Axonal conduction and injury in multiple sclerosis: The role of sodium channels. Nat Rev Neurosci. 2006;7:932–941. doi: 10.1038/nrn2023. [DOI] [PubMed] [Google Scholar]
- 5.Compston A. In: McAlpine's Multiple Sclerosis. Compston A, editor. Edinburgh: Churchill Livingstone Elsevier; 2006. [Google Scholar]
- 6.Matsushima GK, Morell P. The neurotoxicant, cuprizone, as a model to study demyelination and remyelination in the central nervous system. Brain Pathol. 2001;11:107–116. doi: 10.1111/j.1750-3639.2001.tb00385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray PD, McGavern DB, Sathornsumetee S, Rodriguez M. Spontaneous remyelination following extensive demyelination is associated with improved neurological function in a viral model of multiple sclerosis. Brain. 2001;124:1403–1416. doi: 10.1093/brain/124.7.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeffery ND, Blakemore WF. Locomotor deficits induced by experimental spinal cord demyelination are abolished by spontaneous remyelination. Brain. 1997;120:27–37. doi: 10.1093/brain/120.1.27. [DOI] [PubMed] [Google Scholar]
- 9.Liebetanz D, Merkler D. Effects of commissural de- and remyelination on motor skill behaviour in the cuprizone mouse model of multiple sclerosis. Exp Neurol. 2006;202:217–224. doi: 10.1016/j.expneurol.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 10.Utzschneider DA, Archer DR, Kocsis JD, Waxman SG, Duncan ID. Transplantation of glial cells enhances action potential conduction of ameyelinated spinal cord axons in the myelin-deficient rat. Proc Natl Acad Sci USA. 1994;91:53–57. doi: 10.1073/pnas.91.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felts PA, Baker TA, Smith KJ. Conduction in segmentally demyelinated mammalian central axons. J Neurosci. 2007;17:7267–7277. doi: 10.1523/JNEUROSCI.17-19-07267.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Felts PA, Smith KJ. Conduction properties of central nerve fibers remyelinated by Schwann cells. Brain Res. 1992;574:178–192. doi: 10.1016/0006-8993(92)90815-q. [DOI] [PubMed] [Google Scholar]
- 13.Kotter MR, Li WW, Zhao C, Franklin RJM. Myelin impairs CNS remeyelination by inhibiting oligodendrocyte precursor cell differentiation. J Neurosci. 2006;26:328–332. doi: 10.1523/JNEUROSCI.2615-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carroll WM, Jennings AR, Ironside LJ. Identification of the adult resting progenitor cell by autoradiographic tracking of oligodendrocyte precursors in experimental CNS demyelination. Brain. 1998;121:293–302. doi: 10.1093/brain/121.2.293. [DOI] [PubMed] [Google Scholar]
- 15.Jennings AR, Kirilak Y, Carroll WM. In situ characterization of oligodendrocyte progenitor cells in adult mammalian optic nerve. J Neurocytol. 2002;31:27–39. doi: 10.1023/a:1022567414294. [DOI] [PubMed] [Google Scholar]
- 16.Franklin RJ, ffrench-Constant C. Remyelination in the CNS: From biology to therapy. Nat Neurosci Rev. 2008;9:839–855. doi: 10.1038/nrn2480. [DOI] [PubMed] [Google Scholar]
- 17.Ludwin SK, Bakker DA. Can oligodendrocytes attached to myelin proliferate? J Neurosci. 1988;8:1239–1244. doi: 10.1523/JNEUROSCI.08-04-01239.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cassidy JP, et al. Leukoencephalomyelopathy in specific pathogen-free cats. Vet Pathol. 2007;44:912–916. doi: 10.1354/vp.44-6-912. [DOI] [PubMed] [Google Scholar]
- 19.Hagen G, Blakemore WF, Bjerkås I. Ultrastructural findings in spongy degeneration of white matter in silver foxes (Vulpes vulpes) Acta Neuropathol. 1990;80:590–596. doi: 10.1007/BF00307625. [DOI] [PubMed] [Google Scholar]
- 20.Oldfors A, Tulinius M. Mitochondrial encephalomyopathies. J Neuropathol Exp Neurol. 2003;62:217–227. doi: 10.1093/jnen/62.3.217. [DOI] [PubMed] [Google Scholar]
- 21.Li FY, et al. Canine spongiform leukoencephalomyelopathy is associated with a missense mutation in cytochrome b. Neurobiol Dis. 2006;21:35–42. doi: 10.1016/j.nbd.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 22.Duncan ID. In: Neurotoxicity of Industrial and Commercial Chemicals. O'Donoghue JL, editor. Boca Raton, FL: CRC; 1995. pp. 15–50. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.