Abstract
Problem
Recent progress in vaccine availability and affordability has raised prospects for reducing death and disability from neurological infections in children. In many Asian countries, however, the epidemiology and public health burden of neurological diseases such as Japanese encephalitis and bacterial meningitis are poorly understood.
Approach
A sentinel surveillance system for Japanese encephalitis was developed and embedded within the routine meningoencephalitis syndromic surveillance system in Cambodia in 2006. The sentinel surveillance system was designed so surveillance and laboratory testing for other etiologies of neurological infection could be incorporated.
Local setting
The Communicable Disease Control department of the Ministry of Health in Cambodia worked with partners to establish the sentinel surveillance system.
Relevant changes
The sentinel surveillance system has provided important information on the disease burden of Japanese encephalitis in Cambodia and is now providing a platform for expansion to incorporate laboratory testing for other vaccine-preventable neurological infections in children.
Lessons learned
Sentinel surveillance systems, when linked to syndromic reporting systems, can characterize the epidemiology of meningoencephalitis and identify the proportion of hospital-based neurological infection in children that is vaccine preventable. Integrated systems enable consistency in data collection, analysis and information dissemination, and they enhance the capacity of public health managers to provide more credible and integrated information to policy-makers. This will assist decision-making about the potential role of immunization in reducing the incidence of childhood neurological infections.
Résumé
Problématique
Les progrès récemment enregistrés en matière de disponibilité et d’accessibilité économique des vaccins ont soulevé des espoirs de réduire la mortalité et l’incapacité dues aux infections neurologiques chez l’enfant. Dans de nombreux pays asiatiques cependant, on appréhende mal le poids épidémiologique et le fardeau pour la santé publique que représentent les maladies neurologiques telles que l’encéphalite japonaise et la méningite bactérienne.
Démarche
Un système de surveillance sentinelle pour l’encéphalite japonaise a été développé et intégré au système de surveillance syndromique systématique de la méningo-encéphalite au Cambodge en 2006. Le système de surveillance sentinelle a été conçu de manière à pouvoir intégrer la surveillance et les analyses en laboratoire relatives à d’autres étiologies d’infection neurologique.
Contexte local
Le Département Lutte contre les maladies transmissibles du Ministère de la santé cambodgien a collaboré avec ses partenaires pour mettre en place ce système de surveillance sentinelle.
Modifications pertinentes
Le système de surveillance sentinelle a fourni des informations importantes sur la charge de morbidité due à l’encéphalite japonaise au Cambodge et offre actuellement une plateforme de développement permettant l’intégration de tests de laboratoires pour d’autres infections neurologiques infantiles évitables par la vaccination.
Enseignements tirés
Lorsqu’il est couplé à un système de notification des syndromes, un système de surveillance sentinelle peut caractériser l’épidémiologie de la méningo-encéphalite et identifier la proportion d’infections neurologiques nosocomiales évitables par la vaccination dans la population infantile. L’intégration de ces systèmes permet une plus grande cohérence dans la collecte des données et dans l’analyse et la diffusion des informations et renforce la capacité des gestionnaires de la santé publique à fournir des informations plus crédibles et plus synthétiques aux décideurs politiques. Cela contribuera à la prise de décisions concernant le rôle potentiel de la vaccination dans la réduction de l’incidence des infections neurologiques chez l’enfant.
Resumen
Problema
Los recientes progresos en materia de disponibilidad y asequibilidad de las vacunas han avivado las expectativas de reducir la mortalidad y las discapacidades por infecciones neurológicas en los niños. En muchos países asiáticos, sin embargo, no se conocen lo suficiente la epidemiología y la carga de salud pública de enfermedades neurológicas como la encefalitis japonesa y las meningitis bacterianas.
Enfoque
Se desarrolló un sistema de vigilancia centinela de la encefalitis japonesa, que pasó a integrarse en el sistema de vigilancia sindrómica sistemática de la meningoencefalitis en Camboya en 2006. El sistema de vigilancia centinela se diseñó de modo que pudiera incorporar pruebas de vigilancia y de laboratorio para otras causas de infección neurológica.
Contexto local
El departamento de Control de las Enfermedades Transmisibles del Ministerio de Salud de Camboya colaboró con diversos asociados a fin de establecer el sistema de vigilancia centinela.
Cambios destacables
El sistema de vigilancia centinela ha facilitado información relevante sobre la carga de morbilidad por encefalitis japonesa en Camboya y proporciona hoy una plataforma de expansión que permite incorporar las pruebas de laboratorio necesarias para otras infecciones neurológicas prevenibles mediante vacunación en la niñez.
Enseñanzas extraídas
Si se vinculan a sistemas de notificación de síndromes, los sistemas de vigilancia centinela permiten caracterizar la epidemiología de la meningoencefalitis y determinar a nivel hospitalario la proporción de infecciones neurológicas prevenibles mediante vacunación en la población infantil. Los sistemas integrados redundan en una mayor coherencia en la recogida de datos, el análisis y la difusión de información, así como en una mayor capacidad de los responsables de gestionar la salud pública para suministrar información más fiable e integrada a las instancias normativas. De ese modo se facilita la adopción de decisiones sobre la contribución potencial de la inmunización a la reducción de la incidencia de infecciones neurológicas en la niñez.
ملخص
المشكلة
لقد أدَّى التقدُّم الحالي في توافر اللقاحات والقدرة على شرائها إلى توقُّع انخفاض الوفيات والعجز الناجمين عن العدوى العصبية لدى الأطفال. إلا أن الفهم لازال قاصراً في العديد من البلدان الآسيوية عن الإحاطة بالعبء الذي تنوء به الوبائيات والصحة العمومية بسبب تلك الأمراض مثل التهاب الدماغ الياباني والتهاب السحايا الجرثومي.
الأسلوب
لقد طُوِّر نظام ترصُّد خافر لالتهاب الدماغ الياباني وأدمج ضمن نظام الترصُّد الروتيني المتلازمي لالتهاب السحايا والدماغ في كمبوديا في عام 2006. وقد صمِّم نظام الترصُّد الخافر بحيث يمكن أن يُدْمَج ضمنه الترصُّد والفحوص المختبرية للأسباب الإمراضية للعداوى العصبية.
الموقع المحلي
قسم مكافحة الأمراض السارية في وزارة الصحة الكمبودية، الذي عمل مع شركاء لتأسيس نظام ترصدٍ خافر.
التغيرات ذات العلاقة
قدم نظام الترصُّد الخافر معلومات هامة حول عبء أمراض التهاب الدماغ الياباني في كمبوديا، وهو يقدِّم الآن منطلقاً لتوسيع دمج الفحوص المختبرية للعداوى العصبية الأخرى التي يمكن توقيها باللقاحات لدى الأطفال.
الدروس المستفادة
يمكن لنظم الترصُّد الخافر عند ربطها بنظم الإبلاغ المتلازمي أن تقدِّم وصفا للخصائص الوبائية لالتهاب السحايا والدماغ وأن تتعرَّف من واقع المعلومات المستمدة من المستشفيات على النسبة المئوية للعدوى العصبية بين الأطفال والتي يمكن توقِّيها باللقاحات، حيث إن النظم المتكاملة تمكِّن من اتساق جمع المعطيات وتحليل المعلومات ونشرها، كما أنها تعزِّز قدرة القائمين على إدارة الصحة العمومية على تقديم معلومات أكثر موثوقية وتكاملاً لأصحاب القرار السياسي؛ مما يساعد على اتِّخاذ القرارات حول الدور الممكن للتمنيع في خفض معدلات العدوى العصبية في الطفولة.
Introduction
Neurological infection is an important cause of death and disability in children in Asia.1–4 Major vaccine-preventable etiologies of meningoencephalitis (ME) in Asia include Japanese encephalitis (JE) virus and bacteria such as Haemophilus influenzae type b (Hib), Neisseria meningitidis and Streptococcus pneumoniae. Public health initiatives to control these diseases are becoming more feasible with improved vaccine availability and affordability.5
However, in many Asian countries, the epidemiology and public health burden of JE and bacterial meningitis are poorly understood. Generation of disease-specific data for ME was spearheaded in some countries by the establishment of vertical disease-specific initiatives for control of JE, Hib and pneumococcal diseases (e.g. JE project at PATH, and the GAVI Alliance’s Hib Initiative and pneumoADIP). However, the benefits of combining surveillance for meningitis and encephalitis are evident in terms of case identification, simplified logistics and systems, and the potential for more coordinated data analysis and consistent information to assist decision-makers in relation to vaccine introduction programmes.
This paper provides an example of development of an integrated ME surveillance system in Cambodia and, on the basis of this case study, presents the rationale and challenges for design and operation of such systems more generally in Asia.
System design for ME surveillance
A JE sentinel surveillance system was developed and embedded within the routine ME syndromic surveillance system in Cambodia in 2006. The sentinel system was designed so that it could provide a platform to incorporate laboratory testing for other central nervous system (CNS) infections in children.
The goal of the ME surveillance system in Cambodia is to assess disease burden due to neurological infection in children. Weekly reporting to the national level on the number of clinical syndromic ME cases and deaths is required from all district and provincial hospitals across the country. The syndromic ME surveillance is part of the national outbreak surveillance and response system.
The JE sentinel surveillance system was incorporated within this system. Six hospitals were chosen as sentinel sites from geographically diverse parts of the country. ME patients have epidemiological data gathered at these sites. When cerebrospinal fluid and blood are collected for routine case management, tubes are also collected for specific etiology testing. These additional samples are transported weekly to the National Institute of Public Health laboratory in the capital, Phnom Penh. Initially, only JE diagnostic testing by enzyme-linked immunosorbent assay (ELISA) was conducted. The system has been expanded recently and testing for vaccine-preventable etiologies of bacterial meningitis is now being added.
In the first year of surveillance, 47 of 275 (17.1%) ME cases reported from six sentinel sites were laboratory-confirmed as JE. The initial findings from the JE sentinel surveillance system are consistent with results of several previous research studies that have indicated approximately 20–30% of all acute encephalitis cases in Cambodia are attributable to JE virus infection.6,7 With this preliminary data, an estimate of national ME incidence of 42.6 cases per 100 000 children aged less than 15 years and a minimum JE incidence of 7.3 per 100 000 children aged less than 15 years were calculated. Although many factors limit the precision of this estimate, the figure provides a useful estimate of childhood JE incidence in Cambodia.
Many challenges were confronted in the planning and implementation of the surveillance system. In the following section, we outline these challenges and the responses made.
Challenges and responses with system development
Determination of case definition
Challenge
The WHO standards for surveillance of vaccine-preventable diseases do not currently include a case definition for meningoencephalitis, although there are separate standards for bacterial meningitis and for acute encephalitis syndrome/JE.8
Response
The clinical case definition that had been developed when syndromic ME surveillance was established in Cambodia in 2005 was “a person with acute onset of fever (≥ 38 °C) and at least one of the following: neck stiffness, altered consciousness, other meningeal sign”. This case definition more closely resembles the WHO-recommended case definition for bacterial meningitis than acute encephalitis.8 However, because the definition was considered to be sufficiently broad to include most presentations of encephalitis, and clinicians were already familiar with the definition, it was maintained when JE sentinel surveillance was incorporated in 2006.
Collection and testing of clinical samples
Challenge
Collection of cerebrospinal fluid – the key biological sample required for ME surveillance – is often a challenge. Health systems in developing countries are not always equipped to routinely conduct lumbar punctures, staff have not always been trained to conduct them and hesitancy may occur among clinicians as well as family members because of perceived risks. The prioritization for use of a (potentially limited) cerebrospinal fluid sample must also be clearly defined. The first priority for all specimens must be to guide the immediate management and treatment of the patient. Logistics may also be a challenge. Some diagnostic tests cannot be conducted in the local hospital laboratory and samples need to be transported. Requirements for storage and transport may differ when different types of diagnostic tests are conducted. Good coordination of clinicians, laboratory technicians and others who may handle the specimens is required.
Response
In addition to standard operating procedures for specimen collection and management, which included a schema for appropriate laboratory testing of specimens, ME case management guidelines and associated training programmes were developed as a complementary strategy to surveillance capacity-building. Indicators for assessing effective functioning of the surveillance system were defined and monitored.
Managing the limitations
Challenge
Underestimation of population incidence of disease attributable to specific etiologies may occur as a result of limitations of currently available diagnostic testing methodologies. Timing of specimen collection or prior use of antibiotics can affect the likelihood of a positive result. In addition, different testing methodologies used (e.g. ELISA for JE diagnosis, or bacterial culture, polymerase chain reaction or latex agglutination antigen tests for diagnosis of causes of bacterial meningitis) have different sensitivities and specificities.
There are also challenges with relying on sentinel surveillance to provide data to determine the national picture of disease burden. In most Asian countries, laboratory testing of every ME patient nationwide is not feasible. Hence, the accepted model is sentinel surveillance, with testing of samples from patients at selected sites only. If sentinel sites are not truly representative, biases in disease burden estimates occur. For example, if there is less access to hospital facilities for rural rather than urban populations, then JE, a predominantly rural disease, may be under-represented.
To estimate national incidences of particular vaccine-preventable CNS diseases, accurate syndromic ME data are also needed. Under-reporting may occur due to multiple factors. For example, individuals who die before presentation or do not access hospital facilities will not be included. Lack of reporting from private-sector health services may also affect results.
Response
Systems to ensure quality of laboratory data were implemented, including a laboratory quality assurance programme, and individual strategies such as encouraging collection of convalescent serum samples for JE diagnostic testing. The need for careful interpretation of laboratory data was reinforced, ensuring it was understood that the percentage of cases due to a particular viral or bacterial etiology could not necessarily be directly compared based on laboratory results.
Sentinel sites were selected after assessment visits and were carefully chosen from diverse geographical areas, also taking into account other factors including capacity of the hospital to collect and transport specimens. Monitoring of quality of data collection was undertaken during routine supervision visits.
Discussion
Common causes of ME in Asia – JE, Hib and pneumococcal disease – are all vaccine preventable. With Hib and pneumococcal disease, the impact of immunization is not just on CNS disease but on respiratory and other invasive disease. These vaccines could therefore significantly reduce death and disability among children. Data from the recently established sentinel ME surveillance system and more substantial data from the region, and globally, suggest that 50% or more CNS infections in children in Cambodia could be prevented through vaccination.
There is a risk that a focus on individual neurological diseases may result in the emergence of a wide variety of vertical laboratory testing and reporting systems that do not coordinate with national health information systems, leading to fragmentation and inefficiencies in data collection and reporting. This is the single most important lesson learned from the development of other vaccine-preventable disease surveillance systems such as acute flaccid paralysis, measles and tetanus. Surveillance systems are often de-linked in terms of planning, financing and data collection and analysis, resulting in widespread inefficiencies and duplication of scarce financial and human resources.
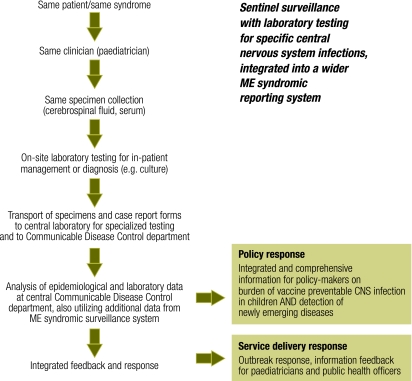
In relation to feasibility of integration of meningitis and encephalitis surveillance, it is crucial to consider that we are dealing with one syndrome and one specimen collection procedure. In addition, the overall operating system – consisting of the patient, the clinician, the surveillance forms, the on-site laboratory testing, the transport system and the reference laboratory structure – remains constant. Based on experience from Cambodia, Table 1 summarizes the rationale for integration of ME surveillance, Fig. 1 provides an overview of an integrated ME surveillance structure and Box 1 summarizes the lessons learned.
Table 1. Rationale for integrated meningoencephalitis surveillance in Asia.
| Rationale | Comments | |
|---|---|---|
| Increasing case detection through a syndromic approach to overlapping clinical syndromes | In patients with CNS infections, there is a clear overlap between those that meet the case definition for “acute encephalitis syndrome” and for “bacterial meningitis”. Initial assignment of patients for reporting through one particular system could result in incomplete case detection and an inaccurate representation of disease burden. | |
| Consistency with routine clinical management procedures | The approach to investigation of a patient with suspected meningitis or encephalitis is the same – a lumbar puncture is routinely recommended for collection of cerebrospinal fluid to assist diagnosis and guide treatment. Samples can be collected at the same time for treatment and public health purposes. | |
| Streamlining of surveillance systems | Low-income countries frequently lack operational expenses for basic health services, so the best use of resources is essential and an integrated system can help reduce programmatic duplication and streamline staff time. It also provides an operational system for surveillance for other diseases that may become public health priorities (e.g. mumps and enterovirus infection) and for newly emerging infectious neurological diseases. | |
| Facilitation of decision-making and evaluation of new vaccine introduction programmes | Integrated surveillance has the potential to provide disease burden data on several vaccine-preventable CNS diseases of public health importance in a comprehensive and coordinated way. The same system can be used for both decision-making (burden of disease) and evaluation of vaccine introduction programmes. | |
| Highlighting the impact of childhood neurological disease | Meningoencephalitis surveillance with collection of clinical outcome data will demonstrate the impact of CNS infections and reinforce the need to strengthen capacity for good clinical case management to improve outcomes. It will also focus attention on the need to support children disabled from disease, consistent with the 2005 World Health Assembly resolution to improve outcomes for persons with disabilities.9 |
CNS, central nervous system.
Fig. 1.
Overview of an integrated meningoencephalitis surveillance system
CNS, central nervous system; ME, meningoencephalitis.
Box 1. Lessons learned.
Sentinel surveillance systems, when linked to syndromic reporting systems, can characterize the epidemiology of meningoencephalitis and identify the proportion of hospital-based neurological infection in children that is vaccine preventable.
Integrated systems enable consistency in data collection, analysis and information dissemination and enhance the capacity of public health managers to provide more credible and integrated information to policy-makers.
This will assist decision-making about the potential role of immunization in reducing the incidence of childhood neurological infections.
Integrated ME surveillance is in line with WHO’s newly released strategy for vaccine-preventable disease surveillance, the Global Framework for Immunization Monitoring and Surveillance.10,11 Four of the seven goals of the framework include linking epidemiological and laboratory surveillance, building surveillance capacity at the country level for disease burden estimates and impact monitoring, expanding laboratory networks for viral and bacterial diseases and, finally, linking with other surveillance and monitoring systems for early detection and response to emerging infections. Integration of meningitis and encephalitis surveillance has the potential to successfully address these goals.
Conclusion
As demonstrated by this case study from Cambodia, an integrated ME surveillance system in Asia has the potential to better define the population incidence and proportion of infectious CNS disease in children that is vaccine-preventable. Public health priorities in the country, availability of viral and bacterial diagnostics, and local disease patterns may all determine the appropriateness of this approach. However, integrated surveillance has the potential to enhance the capability of public health managers to provide more credible and integrated information to policy-makers about the potential role of immunization in reducing childhood CNS infection-related death and disability. Additionally, it would provide a platform for surveillance and investigation of any new or emerging CNS-related infections, monitor the impact of new vaccine programmes and streamline information and reporting in resource-poor public health systems in developing countries. ■
Acknowledgements
We thank the laboratory staff at the National Institute of Public Health and at hospital sentinel sites, the various clinicians, communicable disease control staff, and national immunization programme staff and managers, who have supported the development of the surveillance system in Cambodia. We would also like to thank the following PATH staff: Kathy Neuzil, acting director of JE project, for her review of the manuscript; Jodi Udd for editing support; and the staff in the Cambodia office.
Footnotes
Funding: The work undertaken was funded by PATH’s Japanese Encephalitis Project, supported by the Bill & Melinda Gates Foundation. As a partnership programme, the Ministry of Health in Cambodia has full control of primary data.
Competing interests: None declared.
References
- 1.Tsai TF. New initiatives for the control of Japanese encephalitis by vaccination: minutes of a WHO/CVI meeting, Bangkok, Thailand, 13-15 October 1998. Vaccine. 2000;18(Suppl 2):1–25. doi: 10.1016/S0264-410X(00)00037-2. [DOI] [PubMed] [Google Scholar]
- 2.Wang CH, Lin TY. Invasive Haemophilus influenzae diseases and purulent meningitis in Taiwan. J Formos Med Assoc. 1996;95:599–604. [PubMed] [Google Scholar]
- 3.Solomon T, Dung NM, Kneen R, Gainsborough M, Vaughn DW, Khanh VT. Japanese encephalitis. J Neurol Neurosurg Psychiatry. 2000;68:405–15. doi: 10.1136/jnnp.68.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chotpitayasunondh T. Bacterial meningitis in children: etiology and clinical features, an 11-year review of 618 cases. Southeast Asian J Trop Med Public Health. 1994;25:107–15. [PubMed] [Google Scholar]
- 5.Beasley DW, Lewthwaite P, Solomon T. Current use and development of vaccines for Japanese encephalitis. Expert Opin Biol Ther. 2008;8:95–106. doi: 10.1517/14712598.8.1.95. [DOI] [PubMed] [Google Scholar]
- 6.Chhour YM, Ruble G, Hong R, Minn K, Kdan Y, Sok T, et al. Hospital-based diagnosis of hemorrhagic fever, encephalitis, and hepatitis in Cambodian children. Emerg Infect Dis. 2002;8:485–9. doi: 10.3201/eid0805.010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Srey VH, Sadones H, Ong S, Mam M, Yim C, Sor S, et al. Etiology of encephalitis syndrome among hospitalized children and adults in Takeo, Cambodia, 1999-2000. Am J Trop Med Hyg. 2002;66:200–7. doi: 10.4269/ajtmh.2002.66.200. [DOI] [PubMed] [Google Scholar]
- 8.WHO-recommended standards for surveillance of selected vaccine-preventable diseases Geneva: World Health Organization; 2006. [Google Scholar]
- 9.Disability, including prevention, management and rehabilitation. In: Fifty-eighth World Health Assembly, Geneva, May 2005. Resolutions and decisions Geneva: World Health Organization; 2005. pp. 97-100. [Google Scholar]
- 10.Dabbagh A, Eggers R, Cochi S, Dietz V, Strebel P, Cherian T. A new global framework for immunization monitoring and surveillance. Bull World Health Organ. 2007;85:904–5. doi: 10.2471/BLT.07.048223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Global framework for immunization monitoring and surveillance Geneva: World Health Organization; 2007 (WHO/IVB/07.06). [DOI] [PMC free article] [PubMed]