Abstract
Purpose of review
Robot-assisted laparoscopic surgery in urology has gained immense popularity with the Da Vinci system but a lot of research teams are working on new robots. The purpose of this paper is to review current urologic robots and present future developments directions.
Recent findings
Future systems are expected to advance in two directions: improvements of remote manipulation robots and developments of image-guided robots.
Summary
The final goal of robots is to allow safer and more homogeneous outcomes with less variability of surgeon performance, as well as new tools to perform tasks based on medical transcutaneous imaging, in a less invasive way, at lower costs. It is expected that improvements for remote system could be augmented reality, haptic feed back, size reduction and development of new tools for NOTES surgery. The paradigm of image-guided robots is close to a clinical availability and the most advanced robots are presented with end-user technical assessments. It is also notable that the potential of robots lies much further ahead than the accomplishments of the daVinci system. The integration of imaging with robotics holds a substantial promise, because this can accomplish tasks otherwise impossible. Image guided robots have the potential to offer a paradigm shift.
Keywords: Robot, Image-Guided, Computer Aided Surgery
I. Introduction
A robot is a mechanical device controlled by a computer. Medical robots have been classified in several ways. Three types were distinguished from an operational point of view [1]: remote controlled, synergistic [2], and automated or semi-automated robots. In the first two types, the physician has direct real-time control of the robotic instrument either from a console, or by handling the instrument itself. For the later class, the physician does not have to continuously control the motion of the robot, but rather define its task and monitor the execution.
Robots in different categories are significantly dissimilar from the technical point of view, having other design requirements. It is commonly the case that directly controlled robots have less precision requirements because the motion is compensated by the physician but have additional complexity for implementing the direct control of the physician. Image-guided robots do not normally need a surgeon console, but need to be more accurate and precise to operate without human compensation.
This article gives a short presentation of the achievements and developments in the field, a few key concepts of robotics and medical robotics, and several examples of these technologies commercial and under development.
II. Urology Robots in Current Clinical Use
The daVinci® Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA) platform is the only robotic system use in common practice with more than 800 robots installed worldwide. The robot is a surgeon-driven system with 3 ou 4 arms allowing endowrist capabilities and a 3D visualization of the surgical field. Even though several drawbacks have been echoed about its functionality and possible improvements, this system popularized the concept and instrumentation of robotic surgery.
In large majority the robots are used for robotic assisted laparoscopic radical prostatectomy (RALP) [3]. Even if the review of published literature on RALP and open radical prostatectomy (ORP) is currently insufficient to favour one surgical technique, it seems that short-term outcomes of RALP achieve equivalence to open surgery with regards to complications and functional results [4]. Applications to bladder cancer, renal cancer, uretero-pelvic junction obstruction, and pelvic prolapse have also been explored [5]. The main technical improvement since the first release of the system was the addition of a fourth robotic arm, yet other features especially with respect to improved sensory feedback could significantly improve its performance and surgeon acceptance.
III. Future
Developments aim systems with decreased learning curves that would allow for safer and more homogeneous outcomes with less variability of surgeon performance, as well as new tools to perform more autonomous tasks in a less invasive way at lower costs. Conceptually, robotic developments are an integral part of the Computer Aided Surgery (CAS) paradigm [6]. This integrates preoperative planning, intraoperative guidance, robotic assistance, and postoperative verification and follow-up. Augmented reality is a part of this concept including image fusion from various imaging modalities, such as preoperative CT with laparoscopic images [7] or CT and ultrasound images [8].
Based on the CAS concepts, future systems are expected to advance in the following two directions: Improvements of remote manipulation robots for surgery, developments of image-guided robots for interventions, and possibly combining the two categories.
A. Remote Manipulation Robots
Current surgical robotic research shows a trend of size reduction compared to the daVinci system. For example, the NeuroArm (University of Calgary, Canada) proceeds with the development of a remotely controlled bilateral arm robot for neurosurgical operations. Part of the scope is to reduce its size to where the robot could be brought in the bore of an MRI scanner. Even though this is not yet possible, their current version is substantially smaller than the daVinci, and has additional features such as force feedback [9]. Another example is the VikY system [10], which is a very compact robot allowing to move a laparoscopic camera. Technical works to hold surgical tools on this platform are ongoing (Figure 1).
Figure 1.
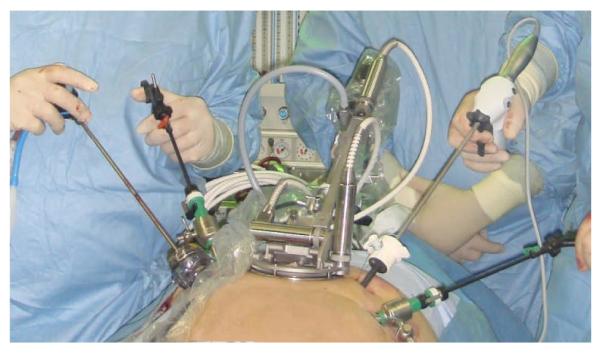
VikY Robot
A common concern with the daVinci robot is the lack of haptic feedback. Several teams are pursuing additions to the existing system for augmenting sensory feedback [11] and with modified trocar instruments for allowing the measurement of manipulation forces [12].
A novel approach is pursuing the development of tools to be deployed in the peritoneal cavity and controlled externally with magnetic fields for reducing the number of transabdominal trocars and for increasing the range of motion and accessibility [13].
The development of natural orifice translumenal endoscopic surgery (NOTES) is potentially the next paradigm shift in minimally invasive surgery. The concept is to access to the peritoneal cavity without passing through the anterior abdominal wall. The first clinical case, performed in 2007, was a cholecystectomy in a woman via a transvaginal approach [14]. Nevertheless, NOTES procedures are performed using modified endoscopic tools with significant constraints and new tools are necessary to allow the surgeon to better visualize and dexterously manipulate within the surgical environment. A two-armed dexterous miniature robot with stereoscopic vision capabilities is under development [15].
B. Direct Image-Guided Robots
Traditionally, image-guidance and navigation of instruments has been performed manually based on pre-acquired images with the use of spatial localizers such as optical [16] and magnetic trackers [17]. However, robots have the potential to improve the precision, accuracy, and reliability of performance in image-guidance interventions because the tasks are done in a full digital way, from image to instrument manipulation.
Robots for interventions with needles or other slender probes or instruments can be connected to an imaging modality (CT, MRI, ultrasound, fluoroscopy, etc.). Targets and paths are defined in the image based on planning algorithms, and the robot aligns and may insert the needle accordingly. The true potential of needle delivery mechanisms relies on their ability to operate with, be guided by, and use feedback from medical imaging equipment.
Moreover, robots can do complex movements, impossible to perform by a human to limit tissue and needle deformations during the insertion. Indeed, decreasing the force of needle insertion has been proposed with special movements as for example a rotating needle for increasing the accuracy of reaching a target [18]. Another option as suggested by Podder and al. [19] is to insert multiple needles simultaneously for prostate therapies to reduce operative time.
Image input
Image-guided robots have stringent requirements for imager compatibility, precision, sterility, safety, as well as size and ergonomics [6]. A robot’s compatibility with a medical imager refers to the capability of the robot to safely operate within the confined space of the imager while performing its clinical function, without interfering with the functionality of the imager [20].
The current research trend is to embed the robot with the imager (CT, MRI, ultrasound, fluoroscopy, etc.) for re-imaging during the intervention, for relocalization treatment planning updates and quality control. We term these procedures Direct Image-Guided Interventions (DIGI). The performance of DIGI interventions is not new, in fact the routine TRUS biopsy is done under direct guidance, however the new term is essential for distinguishing this important class of Image Guided Intervention (IGI) from navigation based on pre-acquired imaging data.
Among all types of imagers, the MRI is the most demanding and the development of MRI compatible robots is a very challenging engineering task [21]. But, this also makes MRI compatible multi-imager compatible, if care is taken for the selection of radiolucent materials for the components in immediate proximity of the imaging site [20]. Due to the strong requirements needed to build a MRI compatible robot, the following description of many robots under development is presented with respect to their capabilities of operation leading up to use with the MRI.
Robots using X-Ray based and Ultrasound Guidance
From historic point of view the first systems were robots with image-guided capabilities. Davies developed a robot for prostatectomies, called Probot [22], based on an industrial Unimate Puma robot constrained within a frame for safety consideration. The robot was guided by transrectal ultrasound images and it was the first robotic device used to remove tissue from a patient when it underwent its first clinical trial in March of 1991.
A few years later, the URobot system was developed in Singapore by Ng and al. The robot was designed to performed a trans-urethral and trans-perinal access to the prostate for laser resection in 2001 [23] or brachytherapy [24] respectively.
Professor Brian Davies has also reported the development of a simple robot that performs similar to the brachytherapy template [25]. Rotation about the axis of the needle is added in order to reduce needle deflections. The system uses 2D TRUS guidance and the report describes successful preclinical testing.
In the Robarts Research Institute (London, Canada) [26] and in the Nanyang Technological University (Singapore) [27], three dimensional (3D) reconstruction from a regular 2D TRUS probe has been investigated by sweeping the probe about its axis. This was integrated with a robot in a system for prostate brachytherapy or biopsy. Mockup tests demonstrated a precision on the order of one millimeter and a clinical study for biopsy is ongoing in Singapore.
Our URobotics laboratory at Johns Hopkins has also developed several versions of a CT-guided robot and performed numerous clinical tests for urology applications [28]. Recently, the AcuBot robot was instrumented with a new end-effecter, the Revolving Needle Driver (RND). The RND is a fully actuated driver for needle insertion, spinning, release, and force measurement (Figure 2). The driver supports the needle from its head, and provides an additional needle support guide in close proximity of the skin entry point. This is similar to holding the needle with two finger-like grippers, one from its head and one from its barrel next to the skin. The top one pushes the needle in and out, while the lower holds the guide to support the direction of the needle as close as possible to the skin. Both grippers can simultaneously release the needle automatically. Finally, the new driver is also equipped with a set of force sensors to measure the interaction of the nozzle with the patient and the force of needle insertion [29].
Figure 2.

Revolving Needle Driver on the AcuBot robot
MRI Compatible Robots
The earliest work for MRI guided prostate intervention robots was performed at the Brigham and Women’s Hospital (BWH), Boston MA in collaboration with AIST-MITI, Japan [30, 31]. A robotic intervention assistant was constructed for open MRI to provide a guide for needles and probes [32, 33]. The system assists the physician by positioning a needle guide for manual needle intervention. Applications included prostate biopsy and brachytherapy [34] but resolution and functional imaging are limited by the low magnetic field of the open MR.
The Institute for Medical Engineering and Biophysics (IMB), Karlsruhe, Germany reported several versions of a robotic system for breast lesion biopsy and therapy under MR guidance [35, 36]. Currently, the development is done by Innomedic (Germany) and their last version used a cylinder for driving an end-effector axis [37]. The robot orients the needle about the axial-sagittal planes for interventions targeting abdominal organs. However, a group from Frankfurt, Germany has recently used the Innomotion system for targeting the prostate [38]. The limitations of the robot restricted the access to the transgluteal path (prone patient with needle pointing down) for which the needle path is much deeper than normal (∼14 cm reported in the cadever experiment) [20]. A 15Ga needle was needed to prevent deflections. Manual needle insertion was performed through the guide after retracting the table from the scanner. Even though the Innomedic system is not FDA approved and its designed application range does not include the prostate, it is approved for clinical use in Europe and is a commercial DIGI robot.
Our group at Johns Hopkins has also developed an MRI compatible robot for prostate access [39]. MrBot, was constructed to be multi-imager compatible, which includes compatibility with all classes of medical imaging equipment (ultrasound, X-Ray, and MR based imagers) [40]. All robotic components are constructed of nonmagnetic and dielectric materials. To overcome MRI incompatibilities a new type of motor, PneuStep [9], was purposely designed. The robot presents 6 degrees of freedom (DOF), 5 for positioning and orienting the injector, and one for setting the depth of needle insertion. Various needle drivers can be mounted in the robot for performing various needle interventions. The first driver was developed for fully automated low dose (seed) brachytherapy [41] (Figure 3).
Figure 3.
MrBot robot for MRI guided prostate interventions
Compared with the classic template of needle guide holes commonly used in TRUS interventions, the robot gives additional freedom of motion for better targeting. For example the skin entry point may be chosen ahead of time and targeting can be performed with angulations, which is impossible with the template, thus allowing for targeting otherwise inaccessible regions of the prostate. As such, multiple needle insertions can be performed through the same skin entry point.
The robot is controlled from a unit remotely located outside the imager’s room. The robot is connected to the control cabinet by a bundle of hoses.
Precision tests in tissue mock-ups yielded a mean seed placement error of 0.72 +/- 0.36 mm [42]. With different needle drivers, the MrBot applies to various automated DIGI, such as biopsy, therapy injections, and thermal or radiofrequency ablations. The system is presently in preclinical testing with cadaver and animal experiments, but tests show very promising results and clinical trials will follow.
C. Image-augmented remote manipulation robots
The combination of the two classes presented above, remote manipulation and direct image-guided robots is a very likely, highly promising direction of future developments. Augmenting guidance from medical imagers to surgical procedures could substantially improve the way that operations are being performed, and would give a clear undisputable advantage for using robotic technologies in surgery.
The NeuroArm robot under development in Canada is a good example of these technologies. Even though it may not yet operate inside the MRI scanner as planned, this may operate next to the MRI scanner and take advantage of recently acquired images to guide the surgery. This does not qualify as MRI safe and compatible, but is a “mini daVinci” with force feedback. Image processing algorithms used in robotic surgery could also improve the localization of the surgical tools and intraoperative analyses.
V. Conclusion
The most popular medical robot thus far is perhaps the daVinci system. In only a few years since its commercial release, this technology has seen significant widespread adoption and use in operating rooms across the world. Most importantly, robotic technology such as the daVinci robot has also shown the potential of these new medical instruments and has substantially boosted the confidence of the physicians in using these technologies in the operating room environment. Concerns regarding its current capabilities and possible upgrades have been echoed, especially about its lack of force feedback. Nevertheless, daVinci represents a significant technology breakthrough and advances will improve its performance.
It is also notable that the potential of robots lies much further ahead than the accomplishments of the daVinci system. The integration of imaging with robotics holds a substantial promise, because this can accomplish tasks otherwise impossible. Image guided robots have the potential to offer a paradigm shift. The final goal of robots is to allow safer and more homogeneous outcomes with less variability of surgeon performance, as well as new tools to perform tasks based on medical transcutaneous imaging, in a less invasive way and at lower costs.
Acknowledgments
The work reported from the Urology Robotics lab at Johns Hopkins has been partially supported by the National Cancer Institute (NCI) of the National Institutes of Health (NIH), the Prostate Cancer Foundation (PCF), the Patrick C. Walsh Prostate Cancer Foundation (PCW), and the Prostate Cancer Research Program of the Department of Defense (PCRP). The contents are solely the responsibility of the authors and do not necessarily represent the official views of NCI, PCF, PCW, or the PCRP.
References
- 1.Davies B. A review of robotics in surgery. Proc Inst Mech Eng [H] 2000;Vol.214(1):129–140. doi: 10.1243/0954411001535309. [DOI] [PubMed] [Google Scholar]
- 2.Troccaz J, Peshkin M, Davies B. Guiding systems for computer-assisted surgery: introducing synergistic devices and discussing the different approaches. Med Image Anal. 1998 Jun;Vol.2(2):101–119. doi: 10.1016/s1361-8415(98)80006-6. [DOI] [PubMed] [Google Scholar]
- 3.Badani KK, Kaul S, Menon M. Evolution of robotic radical prostatectomy: assessment after 2766 procedures. Cancer. 2007 Nov 1;Vol.110(9):1951–1958. doi: 10.1002/cncr.23027. [DOI] [PubMed] [Google Scholar]
- 4.Rassweiler J, Hruza M, Teber D, Su LM. Laparoscopic and robotic assisted radical prostatectomy--critical analysis of the results. Eur Urol. 2006 Apr;Vol.49(4):612–624. doi: 10.1016/j.eururo.2005.12.054. [DOI] [PubMed] [Google Scholar]
- 5.Dasgupta P. Robotics in urology. Int J Med Robot. 2008 Mar;Vol.4(1):1–2. doi: 10.1002/rcs.190. [DOI] [PubMed] [Google Scholar]
- 6.Taylor RH, Stoianovici D. Medical robotics in computer-integrated surgery. IEEE Transactions on Robotics and Automation. 2003 Oct;Vol.19(5):765–781. http://urology.jhu.edu/urobotics/pub/2003-taylor-ieeetra.pdf.
- 7.Ukimura O, Gill IS. Imaging-assisted endoscopic surgery: Cleveland Clinic experience. J Endourol. 2008 Apr;Vol.22(4):803–810. doi: 10.1089/end.2007.9823. [DOI] [PubMed] [Google Scholar]
- 8.Mozer P, Leroy A, Payan Y, Troccaz J, Chartier-Kastler E, Richard F. Computer-assisted access to the kidney. Int J Med Robot. 2005 Dec;Vol.1(4):58–66. doi: 10.1002/rcs.58. [DOI] [PubMed] [Google Scholar]
- 9.Sutherland GR, Latour I, Greer AD. Integrating an image-guided robot with intraoperative MRI: a review of the design and construction of neuroArm. IEEE Eng Med Biol Mag. 2008 May-Jun;Vol.27(3):59–65. doi: 10.1109/EMB.2007.910272. [DOI] [PubMed] [Google Scholar]
- 10.Long JA, Cinquin P, Troccaz J, Voros S, Berkelman P, Descotes JL, Letoublon C, Rambeaud JJ. Development of miniaturized light endoscope-holder robot for laparoscopic surgery. J Endourol. 2007 Aug;Vol.21(8):911–914. doi: 10.1089/end.2006.0328. [DOI] [PubMed] [Google Scholar]
- 11.Reiley CE, Akinbiyi T, Burschka D, Chang DC, Okamura AM, Yuh DD. Effects of visual force feedback on robot-assisted surgical task performance. J Thorac Cardiovasc Surg. 2008 Jan;Vol.135(1):196–202. doi: 10.1016/j.jtcvs.2007.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zemiti N, Morel G, Ortmaier T, Bonnet N. Mechatronic Design of a New Robot for Force Control in Minimally Invasive Surgery. Mechatronics, IEEE/ASME Transactions on. 2007;Vol.12(2):143–153. [Google Scholar]
- 13.Zeltser IS, Cadeddu JA. A novel magnetic anchoring and guidance system to facilitate single trocar laparoscopic nephrectomy. Curr Urol Rep. 2008 Jan;Vol.9(1):62–64. doi: 10.1007/s11934-008-0012-5. [DOI] [PubMed] [Google Scholar]
- 14.Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007 Sep;Vol.142(9):823–826. doi: 10.1001/archsurg.142.9.823. discussion 826-827.Special Interest: First human NOTES procedure.
- 15.Lehman AC, Dumpert J, Wood NA, Visty AQ, Farritor SM, Oleynikov D. In vivo robotics for natural orifice transgastric peritoneoscopy. Stud Health Technol Inform. 2008;Vol.132:236–241. [PubMed] [Google Scholar]
- 16.Bucki M, Dauliac B, Daanen V, Moalic R, Descotes J-L, Troccaz J. PRONAV: A NAVIGATION SOFTWARE FOR PROSTATE BIOPSIES. Surgetica’2005: Sauramps Medical. 2005:479–483. %U http://www-timc.imag.fr/Jocelyne.Troccaz/applis-cliniques_fichiers/ProNav-Surgetica405.pdf.
- 17.Xu S, Kruecker J, Guion P, Glossop N, Neeman Z, Choyke P, Singh A, Wood B. Closed-Loop Control in Fused MR-TRUS Image-Guided Prostate Biopsy. 2007. [DOI] [PMC free article] [PubMed]
- 18.Abolhassani N, Patel RV, Ayazi F. Minimization of needle deflection in robot-assisted percutaneous therapy. Int J Med Robot. 2007 Jun;Vol.3(2):140–148. doi: 10.1002/rcs.136. [DOI] [PubMed] [Google Scholar]
- 19.Podder TK, Ng WS, Yu Y. Multi-channel robotic system for prostate brachytherapy. 2007;Vol.1:1233–1236. doi: 10.1109/IEMBS.2007.4352520. [DOI] [PubMed] [Google Scholar]
- 20.Stoianovici D. Multi-Imager Compatible Actuation Principles in Surgical Robotics. International Journal of Medical Robotics and Computer Assisted Surgery. 2005 January 15;Vol.1(2):86–100. doi: 10.1002/rcs.19. http://urology.jhu.edu/urobotics/pub/2005-stoianovici-MRCASJ.pdf. [DOI] [PMC free article] [PubMed]
- 21.Gassert R, Yamamoto A, Chapuis D, Dovat L, Bleuler H, Burdet E. Actuation methods for applications in MR environments. Concepts in Magnetic Resonance Part B-Magnetic Resonance Engineering. 2006 Oct;Vol.29B(4):191–209. <Go to ISI>://000241550200005. [Google Scholar]
- 22.Davies BL, Hibberd RD, Ng WS, Timoney AG, Wickham JE. The development of a surgeon robot for prostatectomies. Proc Inst Mech Eng [H] 1991;Vol.205(1):35–38. doi: 10.1243/PIME_PROC_1991_205_259_02. [DOI] [PubMed] [Google Scholar]
- 23.Ho G, Ng WS, Teo MY, Kwoh CK, Cheng WS. Experimental study of transurethral robotic laser resection of the prostate using the LaserTrode lightguide. J Biomed Opt. 2001 Apr;Vol.6(2):244–251. doi: 10.1117/1.1353797. [DOI] [PubMed] [Google Scholar]
- 24.Ng WS, Chung VR, Vasan S, Lim P. Robotic radiation seed implantation for prostatic cancer. 1996;Vol 1:231–233. vol.231. [Google Scholar]
- 25.DAVIES BLHSJ, DIBBLE E. Brachytherapy - an example of a urological minimally invasive robotic procedure. Int. J. Medical Robotics and Computer Assisted Surgery. 2004;(1):88–96. doi: 10.1002/rcs.10. [DOI] [PubMed] [Google Scholar]
- 26.Wei Z, Wan G, Gardi L, Mills G, Downey D, Fenster A. Robot-assisted 3D-TRUS guided prostate brachytherapy: system integration and validation. Med Phys. 2004 Mar;Vol.31(3):539–548. doi: 10.1118/1.1645680. [DOI] [PubMed] [Google Scholar]
- 27.Yu, Podder, Zhang, Ng, Misic, Sherman, Fu, Fuller, Messing, Rubens, Strang, Brasacchio Robot-Assisted Prostate Brachytherapy. 2006. [DOI] [PubMed]
- 28.Chinzei K, Hata N, Jolesz FA, Kikinis R. MR compatible surgical assist robot: System integration and preliminary feasibility study. Medical Image Computing and Computer-Assisted Intervention - Miccai 2000. 2000;Vol.1935:921–930. [Google Scholar]
- 29.Chinzei K, Miller K. Towards MRI guided surgical manipulator. Med Sci Monit. 2001 Jan-Feb;Vol.7(1):153–163. [PubMed] [Google Scholar]
- 30.Koseki Y, Koyachi N, Arai T, Chinzei K. Remote actuation mechanism for MR-compatible manipulator using leverage and parallelogram - workspace analysis, workspace control, and stiffness evaluation. 2003;Vol.1:652–657. vol.651. [Google Scholar]
- 31.Koseki Y, Kikinis R, Jolesz FA, Chinzei K. Precise evaluation of positioning repeatability of MR-compatible manipulator inside MRI. Medical Image Computing and Computer-Assisted Intervention - Miccai 2004, Pt 2, Proceedings. 2004;Vol.3217:192–199. [Google Scholar]
- 32.Kaiser WA, Fischer H, Vagner J, Selig M. Robotic system for biopsy and therapy of breast lesions in a high-field whole-body magnetic resonance tomography unit. Invest Radiol. 2000 Aug;Vol.35(8):513–519. doi: 10.1097/00004424-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Felden A, Vagner J, Hinz A, Fischer H, Pfleiderer SO, Reichenbach JR, Kaiser WA. ROBITOM-robot for biopsy and therapy of the mamma. Biomed Tech (Berl) 2002;Vol.47(Suppl 1 Pt 1):2–5. doi: 10.1515/bmte.2002.47.s1a.2. [DOI] [PubMed] [Google Scholar]
- 34.Hempel E, Fischer H, Gumb L, Hohn T, Krause H, Voges U, Breitwieser H, Gutmann B, Durke J, Bock M, Melzer A. An MRI-compatible surgical robot for precise radiological interventions. Comput Aided Surg. 2003;Vol.8(4):180–191. doi: 10.3109/10929080309146052. [DOI] [PubMed] [Google Scholar]
- 35.Zangos S, Eichler K, Thalhammer A, Schoepf JU, Costello P, Herzog C, Mack MG, Vogl TJ. MR-guided interventions of the prostate gland. Minim Invasive Ther Allied Technol. 2007;Vol.16(4):222–229. doi: 10.1080/13645700701520669. [DOI] [PubMed] [Google Scholar]
- 36.Zangos S, Herzog C, Eichler K, Hammerstingl R, Lukoschek A, Guthmann S, Gutmann B, Schoepf UJ, Costello P, Vogl TJ. MR-compatible assistance system for punction in a high-field system: device and feasibility of transgluteal biopsies of the prostate gland. Eur Radiol. 2007 Apr;Vol.17(4):1118–1124. doi: 10.1007/s00330-006-0421-0. [DOI] [PubMed] [Google Scholar]
- 37.Zangos, Herzog, Eichler, Hammerstingl, Lukoschek, Guthmann, Gutmann, Schoepf, Costello, Vogl MR-compatible assistance system for punction in a high-field system: device and feasibility of transgluteal biopsies of the prostate gland. 2007;Vol.17(4):1118–1124. doi: 10.1007/s00330-006-0421-0. %U. [DOI] [PubMed] [Google Scholar]
- 38.Stoianovici D, Song D, Petrisor D, Ursu D, Mazilu D, Muntener M, Schar M, Patriciu A. “MRI Stealth” Robot for Prostate Interventions. Minimally Invasive Therapy & Allied Technologies. 2007;Vol.16(4):241–248. doi: 10.1080/13645700701520735. http://urology.jhu.edu/urobotics/pub/2007-stoianovici-mitat.pdf.Paper reports the first fully automated MRI compatible robot.
- 39.Stoianovici D, Patriciu A, Mazilu D, Petrisor D, Kavoussi L. A New Type of Motor: Pneumatic Step Motor. IEEE/ASME Transactions on Mechatronics. 2007 Feb;Vol.12(1):98–106. doi: 10.1109/TMECH.2006.886258. 2008 Best Paper Award of the Journal. http://urology.jhu.edu/urobotics/pub/2007-stoianovici-tmech.pdf.The only motor that can safely and precisely operate in the MRI without image interference.
- 40.Muntener M, Patriciu A, Petrisor D, Mazilu D, Kavoussi L, Cleary K, Stoianovici D. Magnetic Resonance Imaging Compatible Robotic System for Fully Automated Brachytherapy Seed Placement. Urology. 2006 Dec;Vol.68(6):1313–1317. doi: 10.1016/j.urology.2006.08.1089. http://urology.jhu.edu/urobotics/pub/2006-muntener-urology.pdf. [DOI] [PMC free article] [PubMed]
- 41.Patriciu A, Petrisor D, Muntener M, Mazilu D, Schar M, Stoianovici D. Automatic Brachytherapy Seed Placement under MRI Guidance. IEEE Transactions on Biomedical Engineering. 2007 Aug;Vol.54(8):1499–1506. doi: 10.1109/TBME.2007.900816. http://urology.jhu.edu/urobotics/pub/2007-patriciu-tbme.pdf. [DOI] [PMC free article] [PubMed]
- 42.Reiley CE, Lin HC, Varadarajan B, Vagvolgyi B, Khudanpur S, Yuh DD, Hager GD. Automatic recognition of surgical motions using statistical modeling for capturing variability. Stud Health Technol Inform. 2008;Vol.132:396–401. [PubMed] [Google Scholar]



