Abstract
Background
In utero exposure to antiepileptic drugs (AEDs) can result in several different teratogenic effects including major malformations, dysmorphic facial features, and learning and behavioural problems. It is estimated that there is a 2–3‐fold increase in the risk of malformations compared with the general population. The risk of cognitive impairment and behavioural problems is less clear.
Objective
To report the frequency and specificity of individual dysmorphic features and to relate the dysmorphic facial phenotype to developmental outcome.
Methods
A retrospective study of 375 children born to 219 mothers with epilepsy. The age of the study group ranged from 6 months to 16 years. Each child underwent a physical examination and a battery of neuropsychological tests. Dysmorphic features were scored from photographs on a blind basis by a panel of dysmorphologists.
Results
A total of 274 children were exposed to AEDs (63 to valproate, 94 to carbamazepine, 26 to phenytoin, 15 to other monotherapies, and 76 to polytherapy). Major malformations were identified in 14% of children exposed to valproate in utero, 5% exposed to carbamazepine, and 4% in the non‐exposed group. Overall, 47% of exposed children were correctly identified as having been exposed to AEDs in utero. There was a significant correlation between verbal intelligence quotient and dysmorphic facial features in the valproate exposed children only.
Conclusion
Children exposed to valproate have more distinctive facial features, but a subtle and distinctive facial phenotype is also seen in children exposed to carbamazepine. Nearly half (45%) of unexposed children had some of the facial features associated with AED exposure, showing that many of these features may be seen as part of normal variation and that the diagnosis of the fetal anticonvulsant syndrome is difficult to make on the basis of facial gestalt alone. Developmental surveillance should be offered to children with prenatal exposure to AEDs, particularly those with exposure to high doses of valproate.
Keywords: anticonvulsant syndromes, dysmorphic features, malformations, learning difficulties, valproate teratogenicity
Epilepsy is common, affecting 0.5–1% of the population. Of these, a third are women of reproductive age, and approximately 1 in 250 pregnancies are exposed to antiepileptic drugs (AEDs). AEDs can result in teratogenic effects including major and minor malformations, dysmorphic facial features, and learning and behavioural problems.1,2 The term “fetal anticonvulsant syndrome” (FACS) is often used when referring to children who have suffered adverse teratogenic effects. It is estimated that AED exposure results in a 2–3‐fold increased risk of malformations compared with the general population.3,4 The risk of cognitive impairment and behavioural problems is less clear, although recent studies have focused on this aspect specifically.1,5,6,7 Many studies have described the dysmorphic features associated with AED exposure, but few indicate the frequency and specificity of individual features or relate the dysmorphic facial phenotype with developmental outcome. The purpose of our study was to determine the prevalence of dysmorphic features and major malformations in children exposed to AEDs in utero and to investigate if facial features can be used as a predictor of cognitive impairment in these children.
Patients and methods
In a retrospective study, we recruited 219 mothers with epilepsy; 169 attended regional epilepsy clinics in Manchester and Liverpool, and 50 others presented for antenatal care at a Central Manchester Maternity Hospital between January 1989 and December 1999. Ethical approval was granted for the study, and we sought permission from the mothers to assess their children, both those exposed and those not exposed to AEDs during pregnancy. In total there were 375 children aged between 6 months and 16 years. Structured interviews were conducted with the mothers to collect details of their epilepsy, the AEDs used, their pregnancy history, and details of their children's health and development. Medical records were available to confirm details in about 80% of participants. A clinical examination of all the children in the study was carried out to check the growth parameters and detect dysmorphic features and malformations. Clinical photographs including the face, profile, hands, and feet were available for 340 children. Wherever possible, photographs in early childhood were collected. These photographs were reviewed by a panel of “expert” dysmorphologists, who were blind to the drug exposures. A consensus score on a scale of 0–10 was given to each child based on whether the gestalt was suggestive of FACS. Individual dysmorphic features were recorded on a checklist (table 3). A score of 0 was given if the facies were normal, 1–3 for features mildly suggestive of FACS, 3–6 for moderately suggestive features, and 6–10 for obviously suggestive features. One tenth of the photographs were scored again at the end of the study by the same panel to check for consistency and reproducibility.
Table 3 Relative frequency (%) of dysmorphic features in the different drug groups.
| Features | VPA | CBZ | PHT | PT (no VPA) | PT (with VPA) | NE |
|---|---|---|---|---|---|---|
| Tall/broad forehead | 35.1 | 26.4 | 17.4 | 21.9 | 37.8 | 21.1 |
| Trigonocephaly | 8.8 | 1.1 | 8.7 | 0 | 5.4 | 1.1 |
| Medial deficiency of eyebrows | 47.4 | 16.1 | 0 | 12.5 | 24.3 | 6.7 |
| Infraorbital grooves | 50.9 | 21.8 | 4.3 | 18.8 | 40.5 | 18.9 |
| Epicanthic folds | 7.5 | 3.4 | 4.3 | 3.1 | 5.4 | 4.4 |
| Broad nasal bridge | 59.6 | 32.2 | 8.7 | 18.8 | 32.4 | 17.8 |
| Anteverted nose | 66.7 | 42.5 | 21.7 | 37.5 | 56.8 | 31.1 |
| Abnormal philtrum | 54.4 | 23.0 | 26.1 | 34.4 | 43 | 23.3 |
| Thin upper lip | 61.4 | 20.9 | 13.0 | 31.3 | 48 | 25.6 |
| Everted lower lip | 17.5 | 4.6 | 4.3 | 6.3 | 10.8 | 2.1 |
| Micrognathia | 5.3 | 13.8 | 0 | 6.3 | 2.7 | 3.3 |
| Small mouth | 21.1 | 8.0 | 4.3 | 0 | 5.4 | 3.3 |
| Dysplastic ears | 19.3 | 9.2 | 0 | 6.3 | 8.1 | 1.1 |
| Hypoplastic digits | 17.5 | 10.3 | 8.7 | 9.4 | 18.9 | 10.0 |
| Arachnodactyly | 15.8 | 11.5 | 8.7 | 15.6 | 18.9 | 20.0 |
| Clinodactyly | 42.1 | 36.8 | 13.0 | 37.5 | 51.4 | 28.9 |
| Flat feet | 15.6 | 28.7 | 13.0 | 15.6 | 37.8 | 21.1 |
| Hypoplastic nails | 10.5 | 5.7 | 0 | 9.4 | 2.7 | 7.8 |
VPA, Valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed.
The intelligence quotient (IQ) of children aged 6 to 16 years was assessed by a neuropsychologist using the Wechsler intelligence scale for children (WISC‐III). Children under 6 years were assessed using the schedule of growing skills, but this tool does not give an overall IQ score.
Results
Of the 375 children, 274 were exposed to AEDs, including 63 exposed to valproate, 94 to carbamazepine, and 26 to phenytoin monotherapy. Seventy six children were exposed to polytherapy and 15 to other AEDs.
Growth
Table 1 shows the growth parameters of the children in the various AED groups. Notably 17% of children exposed to valproate had an increased birth weight. This finding was not significant (Pearson χ2 = 1.002, p = 0.317). Microcephaly was present in 11% of children exposed to polytherapy as opposed to 8% in the valproate monotherapy group, 2% in the carbamazepine group, and 4% in the unexposed group. Macrocephaly was present in 11% of children in the polytherapy group and 13% of unexposed children.
Table 1 Growth parameters of children in the different AED groups.
| VPA (%) | CBZ (%) | PT (%) | NE (%) | |
|---|---|---|---|---|
| Birth weight | ||||
| <2500 g | 9.5 | 3.2 | 3.8 | 10.9 |
| >4000 g | 17.4 | 10.8 | 7.6 | 11.8 |
| Height | ||||
| <3rd centile | 9.5 | 6.5 | 6.4 | 3.9 |
| >97th centile | 11 | 14 | 10.2 | 15.8 |
| Weight | ||||
| <3rd centile | 7.9 | 8.6 | 7.7 | 6.9 |
| >97th centile | 7.9 | 8.6 | 12.9 | 12.8 |
| Head circumference | ||||
| <3rd centile | 7.9 | 2.1 | 11.5 | 4.9 |
| >97th centile | 3.1 | 9.8 | 11.5 | 12.8 |
VPA, Valproate; CBZ, carbamazepine; PT, polytherapy; NE, Non‐exposed.
Dysmorphic features
Photographs were available on 340 children: 57 exposed to valproate, 87 to carbamazepine, 23 to phenytoin, 69 to polytherapy, 14 to another AED, and 90 unexposed. Table 2 shows how the patients were scored according to gestalt. A higher proportion of children with moderate or obvious dysmorphic features were in the valproate exposed group. All but one child scoring >6 in the valproate group were exposed to ⩾1 g of the drug per day. A significant dose‐effect correlation was seen only in the valproate exposed group. The correlation coefficient of mean dose and dysmorphic features in this group was 0.533 (p = 0.02). The two children in the polytherapy group who scored as “severe” were also exposed to >1 g valproate per day.
Table 2 Facial features for each AED group by “gestalt category”.
| AED | Normal | Mild | Moderate | Severe |
|---|---|---|---|---|
| VPA (56) | 5 (9%) | 27 (47%) | 16 (28%) | 8 (14%) |
| CBZ (88) | 25 (29%) | 54 (62%) | 8 (9%) | 1 (1%) |
| PHT (23) | 12 (52%) | 11 (48%) | 0 | 0 |
| Others* (14) | 3 (21%) | 9 (64%) | 2 (14%) | 0 |
| PT without VPA (32) | 10 (31%) | 19 (59%) | 3 (9%) | 0 |
| PT with VPA (37) | 9 (39%) | 15 (40%) | 11 (30%) | 2 (5%) |
| NE (90) | 35 (39%) | 53 (59%) | 2 (2%) | 0 |
*Others includes nine children exposed to lamotrigine, two to primidone, two to phenobarbitone, and one to ethosuximide.
AED, Antiepileptic drugs; VPA, valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed.
Individual dysmorphic features
Features often noted in children exposed to valproate were medial deficiency of eyebrows, infraorbital grooves, broad nasal bridge, anteverted nose, abnormal philtrum, and a thin upper lip. Trigonocephaly (triangular shaped skull) was not a common finding. The more commonly noted features with exposure to carbamazepine were full cheeks with a small chin and everted lower lip, giving a “doll‐like” appearance. Table 3 shows the relative frequency with which the features were observed, with evidence of overlap between the different AED exposures.
Evaluation of the scoring system
After the initial scoring procedure, which took place over a period of weeks, a tenth of the photographs were randomly selected and scored afresh by the panel. An identical score was obtained in more than a third of the photos assessed. In the remaining two thirds, the new scores differed on average by only 0.5–1.0 from the previous score. In one case, the score shifted from the moderate to mild category and in another from the moderate to normal category. Our panel identified 47% of children exposed to AEDs in utero as “affected with FACS”. They judged 43% of exposed children as having normal facies and scored 45% of unexposed children as having facies with some FACS features. Overall, the gestalt in fetal valproate syndrome was more specific and easier to identify.
Photographs from early childhood were available in 170 children. Where serial photographs were available, it was noted that the facial features were recognisable at birth and became more apparent during infancy. However, as the children grew older, the features became less distinctive and were subtle in those approaching adulthood. In approximately half of the children for whom early photographs were available (84), they aided the diagnosis.
Malformations and deformations
Major malformations were defined as structural abnormalities requiring medical or surgical intervention to prevent disability. The EUROCAT list of congenital malformations was used as a guideline.8 Table 4 shows the frequency of malformations and deformations in each drug group: in the valproate group, of the nine children with malformations, three had two malformations each. Table 5 shows the type of malformations seen in each group. In the valproate group, 11 of the 12 malformations were seen in mothers taking ⩾ 1 g of the drug per day particularly in the first trimester.
Table 4 Frequency of structural abnormalities in each group.
| AED | Major malformations | OR (95% CI) | Deformations | OR (95% CI) |
|---|---|---|---|---|
| VPA (n = 63) | 9 (14%) | 4.04 (1.19 to 13.74) | 5 (8%) | 1.65 (0.46 to 5.96) |
| CBZ (n = 94) | 5 (5%) | 1.36 (0.36 to 5.23) | 5 (5%) | 1.08 (0.30 to 3.85) |
| PTH (n = 26) | 1 (4%) | 0.97 (0.10 to 9.07) | 0 | |
| Others (n = 15) | 0 | 0 | ||
| PT (n = 76) | 4 (5%) | 1.35 (0.33 to 5.57) | 6 (8%) | 1.65 (0.48 to 5.61) |
| PT without VPA (n = 36) | 0 | 4 (11%) | 2.45 (0.63 to 9.81) | |
| PT with VPA (n = 40) | 4 (10%) | 2.69 (0.64 to 11.35) | 2 (5%) | 1.01 (0.19 to 5.44) |
| NE (n = 101) | 4 (4%) | 1.00 | 5 (5%) | 1.00 |
| Total (n = 375) | 24 (6%) | 22 (6%) |
AED, Antiepileptic drugs; OR, odds ratio, CI, confidence interval; VPA, valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed.
Table 5 Specific malformations seen in each AED group.
| Malformation | VPA | CBZ | PHT | PT | NE |
|---|---|---|---|---|---|
| Cardiac | – | Vsd (2) | Coa/vsd/pda (1) | Vsd (1) | |
| Vsd (1) | |||||
| Neural tube defect | Spina bifida (1) | – | |||
| Hydrocephalus (1) | |||||
| Skeletal | Polydactyly (1) | Polydactyly (1) | |||
| Split hand (1) | |||||
| Genitourinary | Hypospadias (5) | Hypospadias(1) | Hypospadias (1) | Hypospadias (1) | |
| Duplex kidneys (1) | |||||
| Eyes | Coloboma iris (1) | ||||
| Optic disc coloboma (1) | |||||
| Other | Thyroglossal cyst (1) | Cleft lip & palate (1) | Trigonocephaly (1) | Abdominal haemangioma (1) | |
| Pyloric stenosis (1) | |||||
| Total | 12 | 4 | 1 | 4 | 4 |
The number in parentheses indicates the number of children with each abnormality.
AED, Antiepileptic drug; VPA, valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed; vsd, ventricular septal defects; Coa, coarctation of aorta; pda, patent ductus arteriosus.
Deformations defined as alterations in the shape or position of body parts due to mechanical forces acting over a prolonged period of time—for example, talipes, congenital dislocation of the hips (clicky hips)—were seen more often in the polytherapy and valproate exposure groups (table 6).
Table 6 Deformation in each drug group.
| VPA (n = 63) | CBZ (n = 94) | PTH (n = 26) | Others (n = 15) | PT (n = 76) | NE (n = 101) |
|---|---|---|---|---|---|
| Clicky hips (2) | Clicky hips (2) | Clicky hips (3) | Clicky hips (4) | ||
| Fixed flexion deformity of fingers and elbows (1)Postural scoliosis (1) | Dislocated hip (1)Talipes (2)In toe gait (1) | Dislocated hips (1)Talipes (2)Postural | Talipes (2) | ||
| Metatarsus primi varus (1) | Scoliosis (1)Internal femoral torsion (1) |
The number in parentheses indicates the number of children with each abnormality.
VPA, Valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed.
Assessment of IQ
Table 7 shows the WISC scores in children aged 6 and above, by drug exposure. The WISC scores were analysed in 243 of the 256 children over the age of 6 (95%). Further details of IQ scores are reported in a separate paper.9 Children exposed to valproate monotherapy had a significantly lower verbal IQ than the non‐exposed group (p = 0.025). Table 8 shows the relation between the drug dose, presence or absence of malformations, and verbal IQ in the group of children with a severely dysmorphic facies. There was a significant correlation between verbal IQ and dysmorphic features in the valproate exposed group only (Spearman's ρ = −0.436, p = 0.007).
Table 7 WISC score of children aged 6 and above, by AED exposure.
| AED exposure (number exposed) | Mean verbal IQ (95% CI) | Mean performance IQ (95% CI) | Mean full scale IQ (95% CI) |
|---|---|---|---|
| VPA (41) | 83.6 (78.2 to 89.0) | 93.9 (88.9 to 99.0) | 87.2 (81.9 to 92.5) |
| CBZ (52) | 94.1 (89.6 to 98.5) | 89.4 (84.8 to 94.0) | 91.1 (86.4 to 95.8) |
| PHT (21) | 98.5 (90.6 to 106.3) | 97.1 (91.7 to 102.6) | 97.6 (90.3 to 105.0) |
| PT without VPA (21) | 91.9 (85.6 to 98.1) | 89.1 (82.4 to 95.8) | 89.3 (83.5 to 95.2) |
| PT with VPA (28) | 87.1 (81.6 to 92.7) | 89.1 (83.2 to 94.9) | 86.8 (81.2 to 92.4) |
| NE (80) | 90.9 (87.2 to 94.6) | 90.2 (86.1 to 93.0) | 89.5 (85.5 to 93.4) |
AED, Antiepileptic drug; IQ, intelligence quotient; CI, confidence interval; VPA, valproate; CBZ, carbamazepine; PHT, phenytoin; PT, polytherapy; NE, non‐exposed; WISC, Wechsler intelligence scale for children.
Table 8 Relation between drug dose, presence or absence of malformations, and verbal IQ in the group of children with an obviously dysmorphic facies.
| Case no | Gestalt score | AED | 1st trimester dose (mg) | Mean dose (mg) | Malformation | Verbal IQ |
|---|---|---|---|---|---|---|
| MR042001 | 10.0 | VPA | 2000 | 2000 | Hypospadias | 57 |
| MR003001 | 9.5 | VPA | 2000 | 1667 | Hypospadias | 81 |
| Coloboma iris | ||||||
| MR090003 | 9.0 | VPA | 1500 | 1500 | Spina bifida | 0 |
| MR090004 | 9.0 | VPA | 1500 | 1500 | 75 | |
| LR023001 | 9.0 | PHT | 450 | 73 | ||
| VPA | 1800 | |||||
| CBZ | 800 | |||||
| MR224001 | 7.0 | VPA | 1000 | 1267 | 59 | |
| LR305002 | 7.0 | VPA | 2000 | 57 | ||
| CBZ | 1000 | |||||
| MR128001 | 6.0 | VPA | 1500 | 1500 | 72 | |
| MR017003 | 6.0 | VPA | 2000 | 2333 | Split hand | 76 |
| LR270005 | 6.0 | VPA | 800 | 800 | 104 | |
| LR166001 | 6.0 | CBZ | 300 | 100 | 98 |
AED, Antiepileptic drug; IQ, intelligence quotient; VPA, valproate; CBZ, carbamazepine; PHT, phenytoin.
Discussion
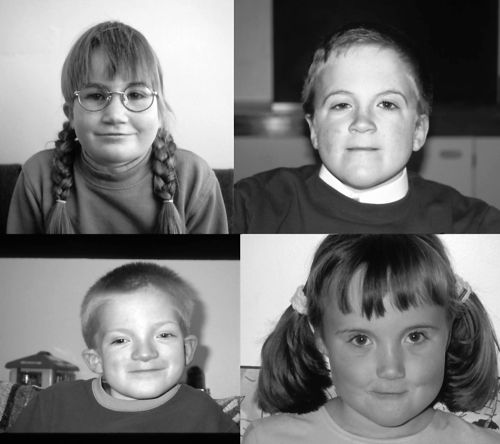
Our study aimed to determine the frequency of dysmorphic features in children exposed to AEDs in utero and correlate this with the degree of learning disability. It has been suggested that the dysmorphic features in FACS are non‐specific and may be seen after exposure to other teratogens such as alcohol and toluene.10,11 Some of the dysmorphic features that are part of the FACS pattern are also commonly seen in the normal population—for example, epicanthic folds, broad nasal bridge. Our study shows that there are clearly difficulties, even for experienced dysmorphologists in diagnosing FACS and that there is an overlap in the features seen with exposure to different AEDs. The facies in fetal valproate syndrome is more distinctive than with other exposures. Our study confirmed previous reports12,13,14 that the typical fetal valproate syndrome face consists of thin arched eyebrows with medial deficiency, broad nasal bridge, short anteverted nose, and smooth long philtrum with thin upper lip (fig 1). The review of photographs of 64 children exposed to carbamazepine monotherapy allowed us to identify a characteristic facial appearance. The features were subtle, but included a doll‐like facies with full cheeks, a short nose, and a relatively small chin (fig 2). In contrast with other AED exposures, the philtrum was well defined in most children exposed to carbamazepine alone. These findings differed somewhat from previously described features of the “carbamazepine face”.15,16 Children exposed to polytherapy containing valproate had dysmorphic features similar to the valproate group, although they appeared less severely affected. Those exposed to polytherapy without valproate were on the whole less obviously dysmorphic. It may be that some children exposed to polytherapy are less dysmorphic because some features caused by one drug may be counterbalanced by the effects of another. On the other hand, the effects of one of the combination drugs may over‐ride those of the others, or the two may compound each other giving rise to a severely dysmorphic facies, as seen in two children in our severely dysmorphic group.
Figure 1 The facies of fetal valproate syndrome. Permission has been obtained for publication of this figure.
Figure 2 The facies of fetal carbamazepine syndrome. Permission has been obtained for publication of this figure.
The scoring method we used to assess the dysmorphism was subjective and relied heavily on the expertise of the panel. However, in every case the panel was able to reach a consensus on the score. Forty six per cent of children in the non‐exposed group were scored as having facies with one or more FACS features. These included features such as epicanthic folds, which are part of normal variation within the general population. We concluded that it is not the individual dysmorphic features but the facial gestalt that helps in the diagnosis of FACS. As our checklist was long (18 items), it was not surprising that a large proportion of participants had one or more of these variations.
The scoring was confounded by the age and ethnicity differences in our cohort. Photographs from early childhood were not available on all children, but helped in the scoring when available. The review of these early photographs supported the fact that the facial dysmorphism in FACS becomes less obvious with age. It would have been difficult to make a diagnosis of FACS in at least 84 children (25%) if early photographs were not available. Although abnormalities of the hands and feet including arachnodactyly, distal digital hypoplasia, and nail hypoplasia have been reported as features of FACS,17 except in one or two cases, photographs of the hands and feet were not helpful in making a diagnosis. Trigonocephaly, which has often been described in fetal valproate syndrome, was rarely observed in our study. This may have been because trigonocephaly is difficult to assess from a full face or profile, and, on reflection, photographing the head from above would have been a more reliable assessment tool. No consistent abnormalities of the ears were noted in the exposed children.
What is already known on this topic
Prenatal exposure to antiepileptic drugs causes teratogenic effects including dysmorphism, malformations, and learning and behavioural difficulties
Many reports have indicated that the teratogenicity is most severe with valproate, but have not correlated the dysmorphic facial phenotype with developmental outcome
The reproducibility of the scores in most instances was very good. However, the panel had significantly variant scores on two occasions. This shows that the dysmorphic face in FACS may be difficult to interpret even to the trained eye. In practice, the clinician considers the history of drug exposure, pattern of growth and development, as well as the clinical features so that the diagnosis of FACS will not rest on assessment of the facial features alone. We observed high birth weights in children exposed to valproate in utero. This observation has been made previously,17 although we did not observe overgrowth in this group subsequently. We were surprised to find a low incidence of microcephaly in the carbamazepine exposed group, as previous studies had suggested that microcephaly was more common in this group.16 Microcephaly was as common as macrocephaly in the polytherapy group and probably reflects the differential effects of the AEDs used in combination. Unfortunately, parental head circumferences were not recorded in the study.
Several investigators have reported a high risk of congenital malformations with maternal doses of valproate above 1 g per day.18,19 This finding has been confirmed in our study. However, the type of malformation varied, suggesting that other factors such as folic acid supplementation and genetic background may influence the susceptibility of the fetus to the teratogenicity of these drugs. We could not examine the influence of folic acid in the prevention of these abnormalities in our study as only 15 mothers took higher dose preconceptual folic acid.
What this study adds
An obviously dysmorphic face may predict learning difficulties
Making a diagnosis of fetal anticonvulsant syndrome based on facial gestalt alone is difficult, but the features of fetal valproate syndrome are the easiest to recognise
Reports of dysmorphic features and cognitive delay in early studies alerted investigators to the possible link between the two in children born to mothers with epilepsy.20,21 In our study, we found that the association between the dysmorphic features and IQ was significant for verbal IQ only and only in the valproate monotherapy group (spearman's ρ = −0.436, 95% confidence −0.107 to −0.827, p = 0.007). Interestingly, the mean IQ in the phenytoin exposed group (n = 21) was 97.6, which differs from previous reports in the literature. Also, somewhat surprisingly, our group of unexposed children had a mean IQ of 89.5. A third of the children with prenatal exposure to AEDs, who had a verbal IQ score of <89 (low average and very low IQ) were found to be mildly dysmorphic or normal (gestalt score <3). Hence, although severely dysmorphic children are likely to have a low verbal IQ, the converse is not true. This highlights the practical difficulties experienced in diagnosing FACS in children who present with a history of prenatal exposure to AEDs and learning problems, but are not dysmorphic and have no major malformations. Dean et al22 have suggested criteria to assist the diagnosis in these children. In children with prenatal exposure to AEDs who do not present the whole spectrum of abnormalities associated with FACS, we suggest that a diagnosis of “fetal anticonvulsant effects” be considered.
In summary, our study shows the difficulties of making a diagnosis of FACS based on facial gestalt alone, particularly in older patients. Of all the anticonvulsant syndromes, fetal valproate syndrome is the easiest to recognise. There is considerable overlap in facial features between the different drugs, but we have delineated more clearly those associated with valproate and carbamazepine exposure. Our study suggests that there is a need to be concerned about future developmental problems in children with obvious facial features of FACS, but this possibility cannot be ruled out if the typical facial features are absent. Therefore, in view of the increased incidence of learning difficulties we observed in children exposed to AEDs in utero, it is prudent to offer developmental surveillance to children with prenatal exposure to AEDs, particularly those exposed to high doses of valproate.
Abbreviations
AED - antiepileptic drug
FACS - fetal anticonvulsant syndrome
IQ - intelligence quotient
WISC - Wechsler intelligence scale for children
Footnotes
Competing interests: none declared.
Permission has been obtained for the publication of figs 1 and 2.
References
- 1.Dean J C, Hailey H, Moore S J.et al Long term health and neurodevelopment in children exposed to antiepileptic drugs before birth. J Med Genet 200239251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mawer G, Clayton‐Smith J, Coyle H.et al Outcome of pregnancy in women attending an outpatient epilepsy clinic: adverse features associated with higher doses of sodium valproate. Seizure 200211512–518. [DOI] [PubMed] [Google Scholar]
- 3.Dieterich E, Steveling A, Lukas A.et al Congenital anomalies in children of epileptic mothers and fathers. Neuropaediatrics 198011274–283. [DOI] [PubMed] [Google Scholar]
- 4.Clayton‐Smith J, Donnai D. Fetal valproate syndrome. J Med Genet 199532724–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scolnik D, Nulman I, Rovet J.et al Neurodevelopment of children exposed in utero to phenytoin and carbamazepine monotherapy. JAMA 1994271767–770. [PubMed] [Google Scholar]
- 6.Ornoy A, Cohen E. Outcome of children born to epileptic mothers treated with carbamazepine during pregnancy. Arch Dis Child 199675517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Granstrom M L, Gaily E. Psychomotor development in children of mothers with epilepsy. Neurology 199242(suppl 5)144–148. [PubMed] [Google Scholar]
- 8.Dolk H. Epidemiologic approaches to identifying environmental causes of birth defects. Am J Med Genet 2004125C4–11. [DOI] [PubMed] [Google Scholar]
- 9.Adab N, Kini U, Vinten J.et al The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry 2004751575–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Astley S J, Clarren S K. A case definition and photographic screening tool for the facial phenotype of fetal alcohol syndrome. J Paediatr 199612933–41. [DOI] [PubMed] [Google Scholar]
- 11.Pearson M A, Hoyme H E, Seaver L H.et al Toluene embryopathy: delineation of the phenotype and comparison with fetal alcohol syndrome. Paediatrics 199493211–215. [PubMed] [Google Scholar]
- 12.DiLiberti J H, Farndon P A, Dennis N R.et al The fetal valproate syndrome. Am J Med Genet 198419473–481. [DOI] [PubMed] [Google Scholar]
- 13.Ardinger H H, Atkin J F, Blackston R D.et al Verification of the fetal valproate syndrome phenotype. Am J Med Genet 198829171–185. [DOI] [PubMed] [Google Scholar]
- 14.Winter R M, Donnai D, Burn J.et al Fetal valproate syndrome: is there a recognisable phenotype? J Med Genet 198724692–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones K L, Lacro R V. Pattern of malformations in the children of women treated with carbamazepine during pregnancy. New Engl J Med 19893201661–1666. [DOI] [PubMed] [Google Scholar]
- 16.Gaily E. Distal phalangeal hypoplasia in children with prenatal phenytoin exposure: results of a controlled anthropometric study. Am J Med Genet 199035574–578. [DOI] [PubMed] [Google Scholar]
- 17.Kozma C. Valproic acid embyopathy: report of two siblings with further expansion of the phenotypic abnormalities and a review of the literature. Am J Med Genet 200198168–175. [PubMed] [Google Scholar]
- 18.Omtzigt J G, Los C, Grobbee F J.et al The risk of spina bifida aperta after first trimester exposure to valproate in a prenatal cohort. Neurology 199242(suppl 5)119–125. [PubMed] [Google Scholar]
- 19.Samren E B, van Duijn C M, Christiaens G C.et al Antiepileptic drug regimens and major congenital abnormalities in the offspring. Ann Neurol 199946739–746. [PubMed] [Google Scholar]
- 20.Vanoverloop D, Schnell R R, Harvey E A.et al The effects of prenatal exposure to phenytoin and other anticonvulsants on intellectual function at 4 to 8 years of age. Neurotoxicol Teratol 199214329–335. [DOI] [PubMed] [Google Scholar]
- 21.Hanson J W, Myrianthopoulos N C, Harvey M A.et al Risks to the offspring of women treated with hydantoin anticonvulsants, with emphasis on the fetal hydantoin syndrome. J Pediatr 197689662–668. [DOI] [PubMed] [Google Scholar]
- 22.Dean J C, Moore S J, Turnpenny P D. Developing diagnostic criteria for the fetal anticonvulsant syndromes. Seizure 20009233–234. [DOI] [PubMed] [Google Scholar]