Modern evidence‐based perinatal care is dependent on the ability of registration systems to record birth outcome precisely and reliably. In the English‐speaking countries, this began in the early 20th century with stillbirth registration in a few states in the US. England and Wales followed in 1927, Scotland in 1939, the Irish Republic in 1959 and Northern Ireland in 1961. In The Netherlands, Belgium and France, stillbirth registration began in the mid‐19th century. However, in Norway and Denmark, registration had been part of the national system for nearly 200 years, and in Sweden it began as early as the 1750s. In the Scandinavian countries, registration of stillbirths was from the very beginning thought to be an instrument with which to monitor birth attendance and to obtain evidence on what could be considered best practice. In 1802, all clergymen in Denmark and Norway were ordered to include the number of stillborn in their yearly statistics and all midwives were also obliged to report every birth to the local clergyman “where the infant came dead to the world or died within 24 hours after birth”. The report should include
…in which month of the pregnancy the mother gave birth, the reason for the premature delivery, if it could be known; with regard to the confinement, if the fetus came easily, was natural or difficult, required turning or was delivered by instrument; if there was life to be seen or not after it was born; in the first case, how long the life lasted; if the midwife used any manipulations or remedies to bring it to life, or keep it alive, and what; or not, and why not; if the mother formerly had given birth to any stillborn infant.1
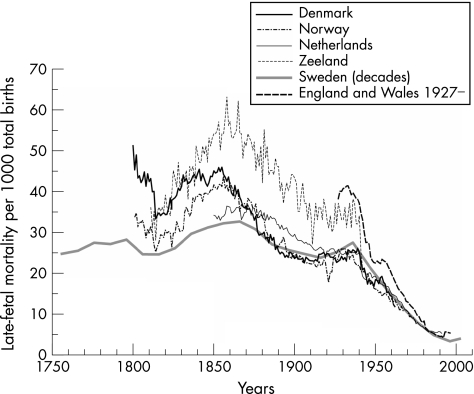
Of course, many difficulties had to be met before such an ambitious programme was carried out to the letter, and the health authorities of the time did not have the resources to manage all the useful knowledge from this huge amount of information. However, fig 1 suggests that in the long run, registering the stillborn did make a difference when it was connected with investments in providing the whole population with educated, authorised and affordable midwives, as was done in the Scandinavian countries. This figure shows the late‐fetal mortality (stillbirths per 1000 total births (stillbirths and live births)) for five countries and the Dutch province of Zeeland. The periods covered are the longest possible time series in each case. Despite shifting registration practices over the years and lack of uniform definitions between countries (especially in terms of fetal gestational age and vital signs at birth), this simple comparison of the long‐run time series offers some unexpected clues.
Figure 1 Late‐fetal mortality: comparison of European experiences (the five countries, and Zeeland).
For historical demographers and medical historians, the most intriguing aspects of fig 1 relate to the hill‐shaped trend in the 19th century and to the obvious difference between England and Wales and the other four examples in the 20th century.
Concerning the hill shape, more detailed studies have to be conducted. We do not yet have a thorough understanding of either the causes of the trend or the divergent levels among the Scandinavian countries. The increase from the 1820s to the 1850s is to a certain degree associated with improvements in the quality of stillbirth registration. For example, it is known that in Denmark and Norway, it required both time and much instruction to make the clergy understand that infant deaths during the first 24 h should be reported as stillborn. And when the report criteria were changed (1839 in Norway and 1860 in Denmark), so that only infants “lifeless” at birth (ie, lacking any vital signs) should count as stillborn, it again took a while to get this new requirement known.2 However, Sweden shows a hill shape too, although there had been no dispute about the criteria there. Even more surprising is the fact that the Dutch province of Zeeland (fig 1) mirrors the Scandinavian countries, but at a higher level. This case is known, because modern demographers have constructed a particularly good database from the civil registers, so we now have an enhanced body of aggregated knowledge that was not available in the past. The Zeeland case is particularly important because it is both well documented and geographically distinct from the Scandinavian examples, yet it has the same key turning points.3
The simultaneity of rise and fall in the four areas suggests that the trend in late‐fetal mortality measured by the stillbirth rate has not followed a linear decline. Furthermore, there must have been influences shared not only between the relatively homogeneous, highly regulated Scandinavian countries but also with the more liberal Zeeland province. It could be that socioeconomic factors were of particular importance, such as maternal nutrition, labour force participation and reproductive history, which has long been known to influence fetal growth and the possibility of premature birth.4 Future studies must explain whether the hill shape can be connected to the rising percentage of poor labourers in the populations, to the famine following the potato blight of the 1840s, to changes in the disease environment in which the mother lived or to something else.
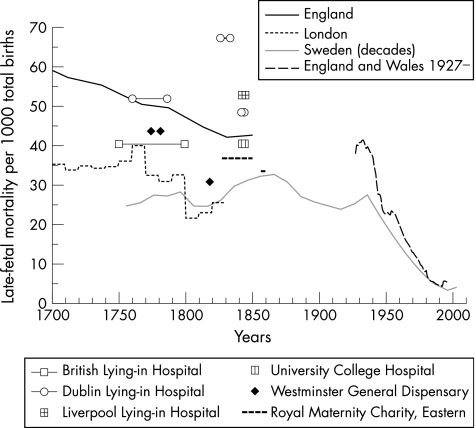
However, we do have some clues to the intriguing position of England and Wales (fig 2). England and Wales experienced a substantially higher rate of late‐fetal mortality than the Scandinavian countries and The Netherlands (40 v 25) during the 1930s, and estimates do not suggest that the 1930s were an exception. Fragments of information make it probable that for England, the rate declined from about 60 to 45 during the 19th century, which is close to where it also lay in the early 1930s,5,6,7 a level that was not much different from the Zeeland case.
Figure 2 Late‐fetal mortality: long‐term trends for England and Wales.
In The Netherlands, it had become evident from the 1850 national statistics that Zeeland had an extraordinary high percentage of stillbirths compared with the rest of The Netherlands. Consequently, several special committees were set up to investigate the causes. Besides an unfavourable economic position, they found a profound absence of trained midwives and doctors in the province. It was also suggested that some doctors showed “a rash use of operative assistance” during the confinements of poverty‐stricken members of the population.8,9 Measures to improve birth assistance in these areas were taken from the late 19th century.10
In contrast, a campaign to provide every parish in Denmark and Norway with an educated, authorised, partly publicly financed midwife had begun as early as 1810 and had been successful by the 1840s. In Sweden, official concern to regulate the quality and quantity of midwives had an even longer history. On the basis of methodologically irreproachable statistical calculations of stillbirth and infant mortality, parishes with excess infant mortality were targeted by the royal health authorities and obliged to engage educated midwives. The peasants complained about the expense, but eventually submitted to official demands. Historical microstudies have shown that in Denmark and Sweden, maternal and infant mortality both decreased from the time the first educated midwife arrived in an area.11,12,13 However in the United Kingdom, midwives were not regulated by the state until the 1902 Midwives Act, and even then contributors to the various Medical Research Council‐sponsored child life investigations during the 1920s found that the poor quality of midwifery was one of the principal causes of high late‐fetal mortality.14
Improvements in the quality of obstetric care and the registration of fetal deaths have gone hand in hand in these six cases. The appreciation that such mortality was above average prompted authorities to act. The duty placed on the midwives in Denmark and Norway in 1802 to report in detail every stillborn and newborn death to the clergy might also have improved the performance of each midwife by obliging her to go through the sequence of birth stages pinpointing were the process went wrong. This production of information for an early evidence‐based perinatal care system had, however, one more advantage unimagined 200 years ago. Evidence is available for us even today. Many of the answers to the detailed questions were dutifully written down by the clergyman, signed by him, the midwife and two women present at the birth, and kept in the archives. Modern research finds these materials invaluable, and their absence in countries such as the United Kingdom both highly important and rather disconcerting.
Acknowledgements
FvP thanks the Zeeuws Archief ISIS (Zeeland Archives) for permitting the use of death certificates for the province of Zeeland.
Footnotes
Funding: RIW acknowledges the financial support from the Wellcome Trust for a project entitled “Fetal Health and Mortality in the Past”.
Competing interests: None.
References
- 1.Home Office, Copenhagen Cancelli cirkulære [circular]. 24 Dec 1802
- 2.Løkke A.Døden i barndommen. Copenhagen: Gyldendal, 1998
- 3.van Poppel F. Historical trends in mortality around birth in the Netherlands: registration practices, trends and regional differentials in the 19th and early 20th centuries. Paper presented at the Social Science History Association Conference, 12–16 Nov 2003, Baltimore
- 4.Baird D. The influence of social and economic factors on stillbirths and neonatal deaths. J Obstet Gynaecol Br Empire 194552217–34, 33966. [Google Scholar]
- 5.Woods R I. The measurement of historical trends in fetal mortality in England and Wales. Popul Stud 200559147–162. [DOI] [PubMed] [Google Scholar]
- 6.Woods R I. Mortality in eighteenth‐century London: a new look at the Bills. Local Popul Stud 2006776–12. [PubMed] [Google Scholar]
- 7.Woods R I.Children remembered: responses to untimely death in the past. Liverpool: Liverpool University Press, 200649–55.
- 8.Evers J C G.Bijdrage tot de bevolkingsleer van Nederland. 's‐Gravenhage: Belinfante, 1882
- 9.Bruinsma G W. Aanteekeningen op een paar ministerieele circulaires. Nederlands Tijdschrift voor Geneeskunde 18832761–68. [Google Scholar]
- 10.van Lieburg M J, Marland H. Midwifery regulation, education, and practice in the Netherlands during the nineteenth century. In: van Teijlingen E, Lewis G, McCaffery P, Porter M, eds. Midwifery and the medicalization of childbirth. New York: Nova Science, 2004127–143.
- 11.Løkke A. The ‘antiseptic' transformation of Danish midwives, 1860–920. In: Marland H, Rafferty AM, eds. Midwives, society and childbirth. London: Routledge, 1997102–133.
- 12.Løkke A. Did midwives matter, 1787–1845? Pathways of the past, time and thought. Report No 7;59–72. Oslo University of Oslo 2002
- 13.Brändström A.De Kärlekslösa mödrarna. Umeå: Almqvist & Wiksell, 1984
- 14.Holland E L, Lane‐Claypon J E.Child life investigations: a clinical and pathological study of 1,673 cases of dead‐births and neo‐natal deaths. Medical Research Council, Special Report Series No 109, London HMSO 1926