Abstract
Objectives
To determine the cerebrospinal fluid (CSF) white blood cell (WBC) count of normal term neonates, and compare the CSF WBC profile of normal and symptomatic infants without infection of the central nervous system (CNS).
Method
Neonates were included if (a) they were at risk of congenital Toxoplasma infection and had undergone a lumbar puncture to assess CNS involvement, and (b) serial specific serum IgG and IgM determinations had ruled out congenital infection. According to neonatal chart reviews, 30 consecutive patients without CNS infection were classified as normal (absolutely asymptomatic) or symptomatic (any kind of symptoms).
Results
CSF WBC count was higher in 11 symptomatic (7/mm3, 0–30/mm3) than in 19 normal (1/mm3, 0–5/mm3) neonates (p<0.01).
Conclusion
Normal neonatal CSF contains up to 5 WBCs/mm3. Mild pleocytosis can be found in symptomatic infants without CNS infection.
Keywords: cerebrospinal fluid, leucocytes, reference values, infection
Normal cerebrospinal fluid (CSF) in adults and children contains no more than 5 white blood cells (WBCs)/mm3. However, normal CSF of neonates contains an imprecisely defined number of WBCs, which may be as many as 15–30/mm3. The greater permeability of the immature blood‐brain barrier has been claimed to be responsible. However, leucocyte trafficking implies a set of strictly regulated cell‐cell and cell‐matrix interactions, and therefore other factors are probably involved.
The purpose of our study was to test the hypothesis that the CSF WBC profile of healthy neonates is no different from that of children and adults. Our objectives were (a) to examine the CSF WBC count of normal term neonates, and (b) to compare the CSF WBC profile of normal and symptomatic infants without infection of the central nervous system (CNS).
Patients and methods
Criteria for inclusion in the study were: (a) newborn infants at risk of congenital Toxoplasma infection (greater than threefold rise in specific maternal serum IgG or high specific IgG and IgM titres), born at 36 or more weeks gestation, who had undergone a lumbar puncture to assess CNS involvement; (b) serial specific serum IgG and IgM determinations had ruled out congenital infection. Neonatal charts were reviewed for clinical evolution, serum analysis, and neuroradiological examinations by one investigator blinded to the CSF analysis (AMA). Criteria for exclusion were congenital infections, perinatal CNS infections, and CSF samples with more than 1000 erythrocytes/mm3. Patients were classified as: (a) normal neonates (absolutely asymptomatic); (b) symptomatic neonates (any kind of symptoms). The study was approved by the committee on ethics in clinical research.
CSF samples were collected in plastic tubes. CSF total WBC count was determined using the improved Neubauer counting chamber under light microscopy. An aliquot was cultured. Cranial sonographic evaluations were performed in every infant.
Data are expressed as mean (SD) or median (range) for descriptive purposes. The Mann‐Whitney test was applied to analyse differences among groups.
Results
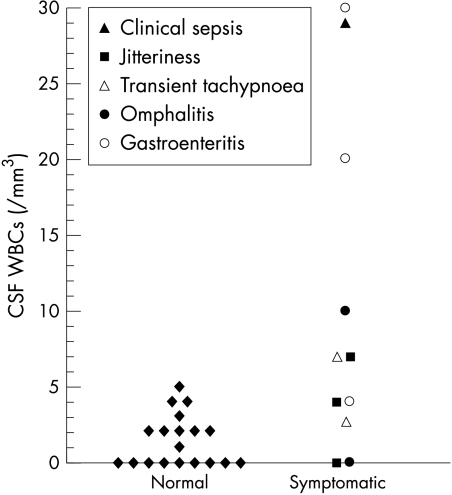
Thirty seven consecutive patients met the entry criteria. Seven were excluded because of blood contaminated CSF. Nineteen infants were asymptomatic. Eleven infants showed different kinds of symptoms within the first days of life (fig 1). No significant differences were found between the groups with regard to sex (40% male v 60% female), gestational age (39.5 (0.4) v 39.2 (0.5) weeks), birth weight (3191 (99) v 3228 (144) g), and age at lumbar puncture (1 day (range 0–8) v 1 day (range 0–6)).
Figure 1 Cerebrospinal fluid (CSF) white blood cell (WBC) count in normal and symptomatic neonates.
All neonates but one had normal cranial sonographic examinations. The one exception (jitteriness, 0 leucocytes/mm3 in the CSF) had findings compatible with mild left germinal matrix haemorrhage without intraventricular blood. Only the neonate with suspected clinical sepsis received intravenous treatment (ampicillin and gentamicin for 7 days).
The median CSF WBC count for the normal neonates was 1/mm3 (range 0–5). CSF WBC count in symptomatic neonates was 7/mm3 (0–30)—significantly higher than in normal neonates (p<0.01) (fig 1).
Discussion
The results of this study provide the first evidence that the normal CSF leucocyte profile in the neonate is similar to the normal adult profile, containing up to 5 WBCs/mm3. It has been traditionally considered that the normal values in the neonate are higher. However, a well defined population of healthy newborn infants without risk factors for sepsis, and completely asymptomatic, has not previously been evaluated. Differences in the populations included in previous studies (positive Wasserman reaction, convulsions, inborn neonates with clinical findings of infection, outpatients with acute illnesses) may be in part responsible for the high variability in the CSF leucocyte counts reported (table 1).
Table 1 Main data of previous studies that have evaluated the cerebrospinal fluid white blood cell (WBC) count during the neonatal period.
| Study | No of patients | Age at LP (days) | WBC count/mm3 |
|---|---|---|---|
| Roberts1 | 423 | 1 | 6.3 (0–17) |
| Naidoo2 | 135 | 0 | 12 (0–42) |
| 20 | 7 | 3 (0–9) | |
| Sarff et al3 | 87 | <7 | 8.2 (7.1) (0–32) |
| Pappu et al4 | 24 | 0–32 | 11 (1–38) |
| Portnoy and Olson5 | 64 | 0–42 | 3.73 (3.4) |
| Bonadio et al6 | 35 | 0–28 | 11.0 (10.4) |
| Carraccio et al7 | 95 | 0–31 | 6.9 (8.0) |
| Ahmed et al8 | 108 | 0–30 | 7.3 (14) |
| Nascimento et al9 | 25 | 1–25 | 4.5 (3.3) |
Data are expressed as mean (SD) or mean (range).
LP, Lumbar puncture.
In this study, the CSF WBC count was significantly higher in symptomatic neonates without CNS infection than in healthy neonates. Values in symptomatic infants were similar to those reported in previous studies for high risk neonates without CNS infection. This finding may not be restricted to the neonatal period. A significant number of infants older than 1 month may also show mild pleocytosis (6–30/mm3) in the context of infectious diseases not involving the CNS.5,6,10,11,12 However, the incidence of mild pleocytosis may be higher for patients in younger age ranges.5,6,12
When the immune system is stimulated by a specific challenge, the entire body including the nervous system is surveyed. Inflammatory cytokines locally generated in response to an infection may communicate with the brain through different pathways. The mild pleocytosis observed in symptomatic children without CNS infection may reflect one aspect of immune surveillance of the CNS during disease. Higher neonatal blood‐brain barrier permeability to proteins may allow easier passage of circulating substances, both molecules from microorganisms and pro‐inflammatory mediators. This may also be in part responsible for the higher incidence of mild pleocytosis in the younger symptomatic infants without CNS involvement.
Examination of the CSF WBC count is one of the main tools for evaluating an infant with suspected CNS infection. Mild pleocytosis can be found in symptomatic infants without CNS infection. On the other hand, it has been recognised that patients with meningitis can have apparently normal CSF findings, mainly when the lumbar punctures are performed early in the course of infection. The results of our study further underline that medicine is more an art than just mathematics. The CSF cell count should be evaluated in conjunction with other clinical and laboratory findings, in some cases including ancillary tools such as β2 microglobulin. Mild pleocytosis does not necessarily indicate CNS infection, but cannot be regarded as a normal finding, and should raise our index of suspicion. This is particularly relevant for asymptomatic infants at risk of congenital infection; the unexpected finding of mild pleocytosis may be an early sign of congenital CNS involvement.
What is already known on this topic
The normal cerebrospinal (CSF) white blood cell (WBC) count of neonates is thought to be higher (up to 15–30/mm3) than that of older children and adults (⩽5 WBCs/mm3)
Reference values for CSF WBC count in neonates have been obtained from high risk infants in whom central nervous system (CNS) infection was ruled out, and not from normal newborns
What this study adds
This study provides the first evidence that the CSF WBC profile of the neonate is similar to that of the adult (⩽5 WBCs/mm3), which fits with stringent regulation of WBC migration into the CNS
Mild pleocytosis can be found in symptomatic infants without CNS infection, but it cannot be regarded as a normal finding and should raise our index of suspicion. This is particularly relevant for asymptomatic infants at risk of congenital infection: the unexpected finding of mild pleocytosis may be an early sign of congenital CNS involvement
Acknowledgements
We acknowledge Bartolomé Bonet for his thoughtful criticism during the preparation of this manuscript, and Carmela Baeza for her technical assistance.
Abbreviations
CNS - central nervous system
CSF - cerebrospinal fluid
WBC - white blood cell
Footnotes
Competing interests: none declared
References
- 1.Roberts M H. The spinal fluid in the new‐born. JAMA 192585500–503. [Google Scholar]
- 2.Naidoo B T. The cerebrospinal fluid in the healthy newborn infant. S Afr Med J 196842933–935. [PubMed] [Google Scholar]
- 3.Sarff L D, Platt L H, McCracken G H. Cerebrospinal fluid evaluation in neonates: comparison of high‐risk infants with and without meningitis. J Pediatr 197688473–477. [DOI] [PubMed] [Google Scholar]
- 4.Pappu L D, Purohit D M, Levkoff A H.et al CSF cytology in the neonate. Am J Dis Child 1982136297–298. [DOI] [PubMed] [Google Scholar]
- 5.Portnoy J M, Olson L C. Normal cerebrospinal fluid values in children: another look. Pediatrics 198575484–487. [PubMed] [Google Scholar]
- 6.Bonadio W A, Stanco L, Bruce R.et al Reference values of normal cerebrospinal fluid composition in infants ages 0 to 8 weeks. Pediatr Infect Dis J 199211589–591. [DOI] [PubMed] [Google Scholar]
- 7.Carraccio C, Blotny K, Fisher M C. Cerebrospinal fluid analysis in systemically ill children without central nervous system disease. Pediatrics 19959648–51. [PubMed] [Google Scholar]
- 8.Ahmed A, Hickey S M, Ehrett S.et al Cerebrospinal fluid values in the term neonate. Pediatr Infect Dis J 199615298–303. [DOI] [PubMed] [Google Scholar]
- 9.Nascimento‐Carvalho C M C, Moreno‐Carvalho O A. Normal cerebrospinal fluid values in full‐term gestation and premature neonates. Arq Neuropsiquiatr 199856375–380. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy P L, Grundy G W, Spiesel S Z.et al Bacteremia in children: an outpatient clinical review. Pediatrics 197657861–868. [PubMed] [Google Scholar]
- 11.Olson L C, Portnoy J M. Normal cerebrospinal fluid values. Pediatrics 1985761024. [PubMed] [Google Scholar]
- 12.Syrogiannopoulos G A, Grivea I N, Anastassiou E D.et al Sterile cerebrospinal fluid pleocytosis in young infants with urinary tract infection. Pediatr Infect Dis J 200120927–930. [DOI] [PubMed] [Google Scholar]