Abstract
In a retrospective study of 22 neonates with congenital diaphragmatic hernia, fetal lung volume (FLV) measured by magnetic resonance imaging was associated with survival; the best FLV ratio cut‐off to predict mortality was 30% of expected FLV. This study supports a correlation between FLV and the chances of survival.
Keywords: diaphragmatic hernia, lung volume, prenatal, prognosis
Despite advances in postnatal care, the death rate in patients with congenital diaphragmatic hernia (CDH) remains as high as 40–60%.1 Reliable outcome predictors are needed to provide families with accurate prognostic information, to optimise postnatal care, and to detect patients who may be candidates for future prenatal treatments.1 However, prenatal prediction of prognosis in patients with isolated CDH remains a challenge.1
Lung hypoplasia is a key prognostic factor.1 This can be estimated by fetal lung volume (FLV) measured by magnetic resonance imaging.2 However, the predictive value of FLV remains controversial.3,4,5 We evaluated the potential for FLV to predict survival in neonates with CDH.
Study design
Patients
We conducted a retrospective study of neonates with prenatal diagnosis of CDH between January 1996 and August 2004 and FLV measurement by magnetic resonance imaging. We excluded voluntarily terminated pregnancies and neonates without FLV measurement. Neonates were inborn and managed according to the same protocol through the years.
Measurement of FLV
Magnetic resonance imaging was performed at 30–32 weeks gestation, using a 1.5 T system. Lung boundaries were manually outlined on axial T2 weighted sequences. The lung surface area was multiplied by section thickness and corrected for gap to yield a partial FLV. The sum of partial FLV yielded the FLV.2
Predicted FLVs were estimated as FLV = 0.0033 × g2.86, where g is gestational age.2 We then computed the ratio of observed over predicted FLV (hereafter designated “FLV ratio”).
The primary evaluation criterion was the association between postnatal mortality and FLV ratio. We also compared the prognostic value of FLV with that of gestational age at birth, gestational age at diagnosis of CDH, fetal sex, side of CDH, and liver herniation. Data are reported as mean (SD) unless specified otherwise.
Results
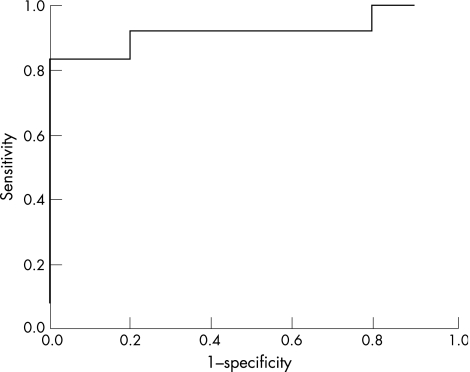
Twenty two neonates were studied, and 10 survived. The FLV ratio was lower in non‐survivors than in survivors (25.1 (12.8)% v 46.9 (11.6)% respectively; p<0.01). The area under the receiver operator characteristic curve of sensitivity and specificity of various ratio cut‐offs for predicting postnatal death was 0.92 (fig 1). The best cut‐off was 30%, with a sensitivity of 0.83 (0.55–0.95) and a specificity of 1.00 (0.72–1.00). In our study, the FLV ratio was the only variable significantly associated with mortality (p<0.01) (table 1).
Figure 1 Receiver operator characteristic curve showing performance of various fetal lung volume ratio cut‐offs for discriminating between survivors (n = 12) and non‐survivors (n = 10). Area under the curve is 0.92.
Table 1 Potential risk factors in survivors and non‐survivors.
| Died (n = 12) | Survived (n = 10) | p Value | Odds ratio (95% CI) | |
|---|---|---|---|---|
| FLV ratio (%) | 25 (13) | 47 (12) | 0.01 | 0.87 (0.78 to 0.97) |
| FLV ratio <30% | 10 (83%) | 0 (0%) | <0.01 | 50 (3.90 to 644) |
| Gestational age at CDH diagnosis (weeks) | 24 (6) | 25 (5) | 0.59 | 0.99 (0.84 to 1.17) |
| Male | 7 (58%) | 5 (50%) | 0.70 | 1.40 (0.26 to 7.6) |
| Right sided CDH | 2 (17%) | 2 (20%) | 0.99 | 0.8 (0.09 to 7.0) |
| Liver herniation | 6 (50%) | 4 (40%) | 0.69 | 1.5 (0.27 to 8.2) |
| Concomitant congenital defects | 4 (33%)* | 2 (20%)† | 0.64 | 2.0 (0.28 to 14) |
| Gestational age at birth (weeks) | 38 (2) | 39 (1) | 0.15 | 0.63 (0.35 to 1.12) |
| Birth weight (g) | 2737 (708) | 3173 (386) | 0.19 | 0.22 (0.03 to 1.51) |
Continuous variables are reported as mean (SD) and compared using Mann‐Whitney tests. Categorical variables are reported as numbers (%) and compared using χ2 tests or Fisher exact test.
*One Fryns' syndrome, one brachycephaly, one hydronephrosis, and one single umbilical artery.
†One hypospadias, and one with renal agenesis, vertebral anomaly, and anal atresia.
CDH, Congenital diaphragmatic hernia; CI, Confidence interval.
Discussion
In this retrospective study of 22 neonates with CDH, the FLV ratio correlated with neonatal survival. The receiver operator characteristic curve identified 30% as the best FLV ratio cut‐off for predicting survival.
Prognostic interest of FLV in CDH has previously been evaluated in three studies.3,4,5 Walsh et al5 reported no statistical difference in FLV between survivors and non‐survivors in a retrospective study of 41 cases. However, FLVs were not expressed as a percentage of an expected value, but were divided by gestational age. FLV increase with gestational age is non‐linear,2 so this standardisation method may contribute to the difference from our results. In contrast, Paek et al3 and Mahieu‐Caputo et al4 reported a relation between FLV and survival, in 11 and 13 CDH cases respectively. Similar to our results, the likelihood of survival was low in patients with FLV ratio <30–40%.3,4
In our study, mortality was not influenced by gestational age at diagnosis, liver herniation, or concomitant congenital defects, but the size of each group is small. The long period of inclusion is another limitation, but there was no major change in the CDH treatment protocol during that period.
Our data support an association between FLV and neonatal survival. These data indicate a need for a prospective study with a larger number of patients.
Acknowledgements
We are indebted to Patrice François for reviewing the statistical analysis.
Abbreviations
CDH - congenital diaphragmatic hernia
FLV - fetal lung volume
Footnotes
Competing interests: none declared
References
- 1.Bohn D. Congenital diaphragmatic hernia. Am J Respir Crit Care Med 2002166911–915. [DOI] [PubMed] [Google Scholar]
- 2.Rypens F, Metens T, Rocourt N.et al Fetal lung volume: estimation at MR imaging‐initial results. Radiology 2001219236–241. [DOI] [PubMed] [Google Scholar]
- 3.Paek B W, Coackley F V, Lu Y.et al Congenital diaphragmatic hernia: prenatal evaluation with MR lung volumetry. Preliminary experience. Radiology 200122063–67. [DOI] [PubMed] [Google Scholar]
- 4.Mahieu‐Caputo D, Sonigo P, Dommergues M.et al Fetal lung volume measurement by magnetic resonance imaging in congenital diaphragmatic hernia. Br J Obstet Gynaecol 2001108863–868. [DOI] [PubMed] [Google Scholar]
- 5.Walsh D S, Hubbard A M, Olutoye O O.et al Assessment of fetal lung volumes and liver herniation with magnetic resonance imaging in congenital diaphragmatic hernia. Am J Obstet Gynecol 20001831067–1069. [DOI] [PubMed] [Google Scholar]