Abstract
Background
Secondary analyses of clinical trial data suggest that, compared with other agents, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB) are associated with lower risk of incident atrial fibrillation (AF) in patients with heart failure, but data from the hypertension trials have been inconsistent. Information is scant about the association of beta-blocker use with AF risk in hypertensive patients without heart failure.
Methods
We conducted a population-based case-control study to determine whether antihypertensive treatment with ACE inhibitors/ARBs or beta-blockers, compared with diuretics, was associated with the risk of incident AF in a community practice setting. All patients (810 AF cases, 1,512 control subjects) were members of Group Health, an integrated health-care delivery system, were pharmacologically treated for hypertension, and did not have heart failure. Medical records were reviewed to confirm the diagnosis of incident AF and to collect information on medical conditions and health behaviors. Information on antihypertensive medications was obtained from a pharmacy database.
Results
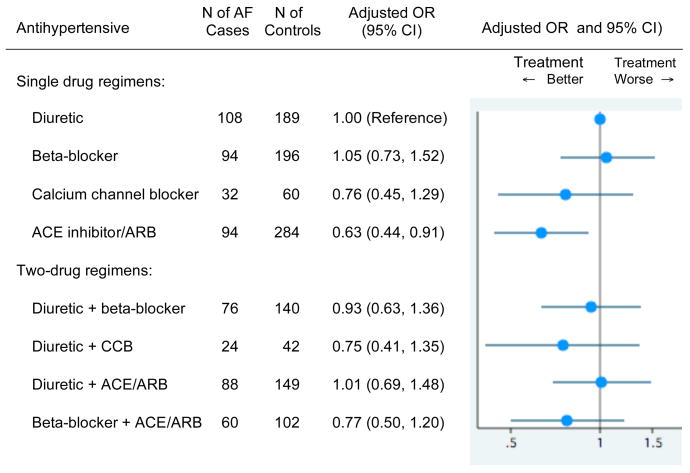
Single-drug users of an ACE inhibitor/ARB had a lower risk of incident AF compared with single-drug users of a diuretic (adjusted odds ratio [OR] 0.63, 95% confidence interval [CI] 0.44–0.91). Single-drug use of beta-blockers was not significantly associated with lower AF risk (OR 1.05, 95% CI 0.73–1.52), and none of the most commonly-used two-drug regimens was significantly associated with AF risk, compared with single-drug use of diuretic.
Conclusion
In a general hypertensive population without heart failure, single-drug use of ACE inhibitors/ARBs was associated with lower AF risk.
Introduction
Atrial fibrillation (AF) is common, affecting over 2 million Americans 1, and is increasing in incidence over time as the population ages 2, 3. Clinical research in AF has generally focused on methods to interrupt AF once it has occurred. Relatively little is known about interventions, including antihypertensive medications, that may prevent or delay AF onset. Given the high morbidity and mortality associated with AF, research to prevent it is critical.
In secondary analyses of data from clinical trials, inhibitors of the renin-angiotensin system, including angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), have been associated with lower AF risk in patients with heart failure 4, 5. On the other hand, in the hypertension trials, the association with AF risk has been inconsistent 4, and a benefit of ACE inhibitors or ARBs in a general hypertensive population has not been demonstrated. The addition of beta-blockers in patients with heart failure who are already receiving ACE inhibitors has also been associated with lower AF risk 6, but information is scant about AF risk in patients without heart failure receiving beta-blocker treatment for hypertension. We conducted a population-based study to determine whether antihypertensive treatment with ACE inhibitors/ARBs or beta-blockers was associated with risk of incident AF in a community practice setting. We hypothesized that compared with diuretics, both therapeutic classes would be associated with lower AF risk.
Methods
Setting and Design
This case-control study was conducted at Group Health (GH), a large integrated health care delivery system in Washington State. The GH Human Subjects Review Committee approved study procedures.
Study Population
We identified all GH enrollees assigned an International Classification of Diseases, Ninth Revision (ICD-9) code for AF (427.31, atrial fibrillation; or 427.32, atrial flutter) during any inpatient or outpatient visit between October 1, 2001 and December 31, 2004, who had never before been assigned an ICD-9 code for AF during their GH enrollment. Trained abstractors reviewed medical records to verify the AF diagnosis and to confirm that the AF was of new onset; verified cases were retained as AF cases. We required that the AF diagnosis be confirmed by 12-lead electrocardiogram and clinically recognized by a provider. Perioperative AF was included only if it persisted to the time of hospital discharge (n = 4 cases), and new AF that occurred as part of a terminal hospitalized illness was excluded.
Control subjects were shared between this study and ongoing case-control studies of myocardial infarction (MI) 7, stroke 8, and venous thromboembolism 9 at GH. Control subjects were chosen at random from GH enrollment lists, were frequency matched to MI cases by age (by decade), sex, and year of identification, and had no history of clinically recognized AF.
We defined an index date for all subjects as the date the AF first came to clinical attention for cases or a random date for control subjects. Eligible subjects were age 30 to 84 years with at least four health care visits before the index date, to increase the likelihood that information would be available on health conditions. Subjects with a pacemaker were excluded as it could interfere with AF identification or could affect the extent of surveillance for AF. Subjects with a diagnosis of heart failure before the index date were excluded because this analysis was designed to study the association of antihypertensive medications with new-onset AF in patients with hypertension but without clinically recognized heart failure. All case and control subjects included in this analysis had a physician diagnosis of hypertension and were treated at the index date with one or more antihypertensive medications.
Data collection
The GH ambulatory medical record includes notes from primary care and specialty physician visits, emergency department notes, discharge summaries, information from telephone contacts, electrocardiograms, Holter monitor reports, and laboratory and diagnostic test reports. Trained abstractors reviewed the entire medical record for each subject, covering a mean of 22 years of enrollment, to gather data on the following covariates, which were assessed prior to the index date: the most recent measured height, weight, and blood pressure, diabetes mellitus, valvular heart disease, angina, presence and duration of hypertension, and history of MI, stroke, peripheral vascular disease, or revascularization procedure. Subjects were asked about race and smoking status in telephone interviews. For subjects who did not complete a telephone interview, these data were obtained from medical record review.
Medication use
The GH pharmacy database was the primary source of information about medication use. Since 1977, the pharmacy database has included a record for each prescription dispensed to GH enrollees from a GH pharmacy. Among patients in this age group, 96% of GH members report filling all or almost all prescriptions through GH pharmacies 10. Each pharmacy record includes the drug type and dose, quantity dispensed, and intended days supply of the prescription. To determine current use of a particular drug at the index date, we searched the pharmacy data for the prescription immediately preceding the index date. If the patient received enough pills to last until the index date, assuming 80% compliance with prescribing instructions, then the patient was considered a user of the drug on the index date. If so, and if the subject was also a user at 30 and/or 60 days prior to the index date, the subject was classified as a current user. Because only 5% of control subjects and 8% of AF cases currently used ARBs at the index date, ARB use was classified together with ACE inhibitor use in a single group (“ACE inhibitor/ARB”) in all analyses.
Covariates: variable definitions
Diabetes was defined as present if a physician diagnosis was found in the medical record and the subject was receiving insulin or oral hypoglycemic medication at the index date. Atherosclerotic disease was defined as a history of MI, angina, coronary revascularization, ischemic stroke, carotid endarterectomy, or peripheral vascular disease before the index date. Duration of hypertension was defined as the interval from the date of first hypertension treatment until the index date.
Statistical analyses
We performed descriptive analyses to examine the characteristics of AF case and control subjects, and the characteristics associated with use of various classes of antihypertensive medication among control subjects. Multivariate logistic regression was used to examine the adjusted risk of new-onset AF associated with the most common one-drug and two-drug antihypertensive regimens. Single-drug users of a diuretic were the reference group for all analyses because diuretic alone was one of the most common regimens, and because diuretics are recommended as the initial drug of choice for the treatment of hypertension 11. In a secondary analysis, the association of antihypertensive regimen with AF risk was examined in subgroups of subjects with and without underlying atherosclerotic disease or diabetes. All models were adjusted for the matching variables of age (as a continuous variable), sex, and calendar year, and for atherosclerotic disease and diabetes. Goodness of fit of the models was evaluated with the Hosmer-Lemeshow goodness-of-fit test, and could not be rejected for any of the estimated models shown. Results from analyses that assumed 100% compliance with medication instructions yielded results similar to those that assumed 80% compliance; therefore, only the results for the latter are presented.
In analyses restricted to users of single-drug antihypertensive regimens, we examined AF risk according to daily dose of antihypertensive medication. We categorized the daily drug dose at the index date into 3 groups. Daily doses equal to the modal daily dose for each generic drug were considered medium, daily doses below the modal dose were considered low, and daily doses above the modal dose were considered high. Duration of use of each drug was estimated for users of single-drug antihypertensive regimens by counting the number of prescriptions filled in each drug class and multiplying by the median days supply provided for drugs in that class. Duration of use was classified into two categories, below and above the median of 4 years of use.
All analyses were conducted using Stata 10 (Stata Corporation, College Station, TX).
Results
During the study period, 946 AF cases and 1,707 control subjects with treated hypertension were identified. Of these, 810 (86%) AF cases and 1,512 (89%) control subjects were sufficiently compliant with their antihypertensive medication to be classified as current users at the index date and were included in the analysis. As expected, patients with AF had a higher prevalence of angina, myocardial infarction, valvular heart disease, and diabetes, compared with control subjects (Table 1). AF cases also had slightly longer GH enrollment and duration of hypertension, slightly higher systolic blood pressure, and used on average a larger number of antihypertensive medications than control subjects.
Table 1.
Characteristics of atrial fibrillation case and control subjects
| Characteristic | AF case subjects N = 810 | Control subjects N = 1,512 | P-value, controls vs. cases |
|---|---|---|---|
| Age, mean (SD) | 73 (9) | 67 (11) | * |
| Male, % | 46 | 58 | * |
| Black, % | 3 | 5 | 0.06 |
| Years enrolled at GH, mean (SD) | 23 (13) | 21 (13) | <0.01 |
| Duration of hypertension, yrs, mean (SD) | 12 (9) | 11 (9) | <0.001 |
| Current smoking, % | 6 | 7 | 0.29 |
| Body mass index (kg/m2), mean (SD) | 30 (7) | 30 (6) | 0.93 |
| Angina, % | 18 | 11 | <0.001 |
| Myocardial infarction, % | 11 | 7 | <0.01 |
| Atherosclerotic disease**, % | 40 | 26 | <0.001 |
| Valvular heart disease, % | 6 | 2 | <0.001 |
| Diabetes mellitus, % | 19 | 16 | <0.05 |
| Systolic blood pressure, mmHg, mean (SD) | 140 (21) | 138 (18) | <0.01 |
| Diastolic blood pressure, mmHg, mean (SD) | 77 (12) | 78 (11) | 0.06 |
| Controlled hypertension (SBP<140 and DBP<90), % | 46 | 48 | 0.22 |
| Number of antihypertensive medications at index date, % | <0.001 | ||
| 1 | 42 | 49 | |
| 2 | 36 | 35 | |
| ≥3 | 22 | 16 | |
| Antihypertensives used at index date, % † | |||
| Diuretic | 55 | 49 | <0.01 |
| Beta-blocker | 48 | 43 | <0.05 |
| Calcium channel blocker | 23 | 19 | <0.05 |
| ACE inhibitor/ARB | 51 | 53 | 0.59 |
| Other ‡ | 9 | 6 | <0.05 |
AF = atrial fibrillation, GH = Group Health, SD = standard deviation, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker
Age and sex were frequency-matching variables
Atherosclerotic disease was defined as a history of myocardial infarction, angina, coronary revascularization, ischemic stroke, carotid endarterectomy, or peripheral vascular disease.
Patients could be on more than one antihypertensive drug
Other drug classes include peripheral vasodilators and centrally and peripherally-acting antiadrenergic agents
Race was missing in 5 cases and 35 control subjects; years enrolled in GH in 6 cases and 9 control subjects; BMI in 6 cases and 34 control subjects; and duration of hypertension in 27 cases and 46 control subjects.
The four antihypertensive drug classes most commonly used by both AF cases and control subjects were diuretics, beta-blockers, calcium channel blockers, and ACE inhibitors/ARBs. Preferred drugs on the GH formulary during the period of the study included hydrochlorothiazide, which accounted for 84% of drugs in its therapeutic class in current use at the index date; atenolol, 87%; felodipine, 34%; and lisinopril, 86%. Drugs in all other therapeutic classes, including peripheral vasodilators and centrally and peripherally-acting antiadrenergic agents, were used by few AF cases and control subjects (Table 1), and were not considered further in this analysis.
Among the 1,512 control subjects, the choice of antihypertensive agent was related to the presence or absence of atherosclerotic disease and diabetes (Table 2). For example, beta-blockers were used by 39% of control subjects without atherosclerotic disease, and by 54% of those with atherosclerotic disease, after adjustment for age and sex. Beta-blockers, calcium channel blockers, and ACE inhibitors/ARBs were more commonly used in patients with atherosclerotic disease than in those without, and diuretics were less commonly used. Calcium channel blockers and ACE inhibitors/ARBs were more commonly used in patients with diabetes than in those without.
Table 2.
Percentage (95% CI) of current users of various drugs among 1,512 control subjects with and without indications for specific antihypertensive therapies (adjusted for age and sex)
| Characteristic | N | Diuretic | Beta-blocker | Calcium channel blocker | ACE inhibitor/ARB |
|---|---|---|---|---|---|
| Atherosclerotic disease | |||||
| No | 1,121 | 52 (49, 55) | 39 (36, 42) | 17 (14, 19) | 48 (45, 51) |
| Yes | 391 | 37 (31, 42) | 54 (49, 59) | 29 (24, 34) | 66 (61, 72) |
| P<0.001 | P<0.001 | P<0.001 | P<0.001 | ||
| Diabetes mellitus | |||||
| No | 1,275 | 50 (47, 52) | 44 (41, 46) | 18 (16, 20) | 47 (45, 50) |
| Yes | 237 | 44 (37, 50) | 37 (31, 44) | 25 (19, 31) | 82 (77, 87) |
| P=0.10 | P=0.09 | P<0.05 | P<0.001 | ||
ACE = angiotensin-converting enzyme, ARB = angiotensin receptor blocker
Among the 810 AF cases and 1,512 control subjects studied, 576 (71%) cases and 1,162 (77%) control subjects used one of the most common single-drug and two-drug antihypertensive regimens at the index date: single-drug treatment with a diuretic, a beta-blocker, a calcium channel blocker, or an ACE inhibitor/ARB, or two-drug treatment with various combinations of these drugs (Figure 1). Compared with single-drug users of a diuretic, only single-drug users of an ACE inhibitor/ARB had a lower risk of incident AF. In particular, single-drug use of beta-blockers was not significantly associated with lower risk of AF, and none of the two-drug regimens was significantly associated with AF risk, compared with single-drug use of diuretic. Risks were similar after further adjustment for duration of treated hypertension, body mass index, achieved systolic blood pressure, or statin use, after excluding the 32 AF cases and 21 control subjects with valvular heart disease, or after excluding the 61 AF cases and 34 control subjects who used furosemide as part of any regimen.
Figure 1. Association of antihypertensive drug therapies with AF risk among 1,738 treated hypertensives using the most common one and two-drug regimens at the index date.
AF = atrial fibrillation, OR = odds ratio, CI = confidence interval, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker, CCB = calcium channel blocker
ORs adjusted for the matching variables of age, sex, and calendar year, and for atherosclerotic disease and diabetes mellitus
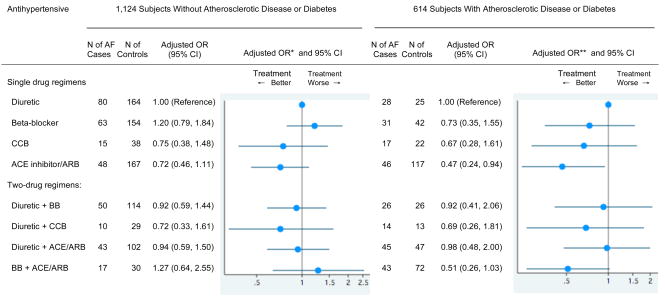
We conducted a secondary analysis in subgroups with and without atherosclerotic disease or diabetes (Figure 2). Among 1,124 subjects without either condition, ACE inhibitor/ARB use was associated with lower AF risk compared with diuretic use, but this difference did not reach statistical significance. Among the 614 subjects with atherosclerotic disease or diabetes, ACE inhibitor/ARB use remained significantly associated with a lower risk of incident AF. Compared with diuretic use, beta-blocker use was associated with slightly higher AF risk in subjects without atherosclerotic disease or diabetes, and with a slightly lower AF risk in those without, but confidence intervals included unity and these differences were not statistically significant. None of the other antihypertensive regimens was significantly associated with AF risk in either subgroup, although there was a suggestion of reduced AF risk associated with use of beta-blocker plus ACE inhibitor/ARB in the subgroup with atherosclerotic disease or diabetes. Statistical evidence was lacking for heterogeneity in the drug regimen-AF associations in these two subgroups (interaction p=0.64).
Figure 2. Association of antihypertensive drug therapies with AF risk in subjects with or without a history of atherosclerotic disease or diabetes, among 1,738 hypertensives using the most common one and two-drug regimens at the index date.
AF = atrial fibrillation, OR = odds ratio, CI = confidence interval, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker, BB = beta-blocker, CCB = calcium channel blocker
* Adjusted for age, sex, and calendar year
** Adjusted for age, sex, calendar year, atherosclerotic disease, and diabetes mellitus
Subjects on a single-drug antihypertensive regimen tended to receive a drug from a single therapeutic class for long periods of time and received few or no drugs from the other classes during their GH enrollment (Table 3). For example, users of an ACE inhibitor/ARB at the index date had filled a median of 19 prescriptions for ACE inhibitors/ARBs, one prescription for a diuretic, and zero prescriptions for calcium channel blockers or beta-blockers during a median enrollment of 22 years.
Table 3.
Median (interquartile range [IQR]) number of diuretic, beta-blocker, calcium channel blocker, and ACE inhibitor/ARB prescriptions dispensed during enrollment at GH among 1,057 hypertensives using single-drug therapy at the index date
| Median (IQR) number of prescriptions |
|||||
|---|---|---|---|---|---|
| Antihypertensive used at index date | Number of AF cases & control subjects | Diuretic | Beta-blocker | Calcium channel blocker | ACE inhibitor/ARB |
| Diuretic | 297 | 16 (7, 35) | 0 (0, 1) | 0 (0, 0) | 0 (0,1) |
| Beta-blocker | 290 | 1 (0, 7) | 20 (9, 35) | 0 (0, 0) | 0 (0, 1) |
| Calcium channel blocker | 92 | 8 (0, 24) | 1 (0, 11) | 34 (15, 49) | 1 (0, 7) |
| ACE inhibitor/ARB | 378 | 1 (0, 8) | 0 (0, 4) | 0 (0, 0) | 19 (9, 38) |
ACE = angiotensin-converting enzyme, ARB = angiotensin receptor blocker
Among single-drug users of diuretics, beta-blockers, calcium channel blockers, or ACE inhibitors/ARBs, the risk of AF did not differ according to the daily dose of the drug at the index date (below, at, or above the modal dose for their drug) compared with low dose diuretic use, or by duration of use of that drug (< or ≥ 4 years), compared with diuretic use for < 4 years.
Discussion
In this population-based study of patients with treated hypertension, single-drug users of ACE inhibitors or ARBs had a lower risk of incident AF than single-drug users of diuretics. The association was similar in subgroups with and without underlying atherosclerotic disease or diabetes. The risk of AF in users of beta-blockers alone or in users of two-drug regimens that included ACE inhibitors/ARBs was not significantly different from that of diuretic users.
Strengths of our study include the population-based design, the study of a general population of treated hypertensives, the ability to study patients on single-drug antihypertensive regimens, the large number of carefully-validated AF cases, ascertainment of AF presenting in both the inpatient and outpatient setting, and the comparable ascertainment of potential confounding factors in AF cases and control subjects. The use of the GH pharmacy database permitted assessment of antihypertensive use in an unbiased fashion, and the presence of a drug formulary tended to limit prescribing to a few agents. Patients on single-drug regimens tended to stay on a drug from the same class for a long period of time. We used restriction, stratification, and adjustment to minimize the possibility of confounding. All subjects were enrollees of a health maintenance organization and thus had similar access to health care.
Nonetheless, our study was observational and antihypertensive drugs were not assigned at random. Unknown or unmeasured confounding factors may exist for which adjustment was not possible. Measurement error in the assessment or estimation of covariates and their severity may have resulted in incomplete adjustment and residual confounding. In particular, in analyses that compared AF risk for users of two-drug regimens versus a diuretic alone, residual confounding by hypertension severity or sequelae may have obscured differences in AF risk. Ascertainment of AF may not have been complete, as we were only able to identify AF cases that came to clinical attention.
Angiotensin II has been shown to mediate atrial remodeling by promoting myocyte hypertrophy, fibroblast proliferation, collagen accumulation, inflammatory cell infiltration, and apoptosis, and by interfering with atrial electrophysiology (reviewed in 12 and 13). In small studies with careful measurement of left atrial size and function, ACE inhibitor and ARB treatment have been shown to reverse left atrial remodeling in the setting of diastolic dysfunction and left atrial enlargement in humans 14, and in the setting of pacing-induced AF in a canine model 15. Consistent with these findings, in secondary analyses of incident AF from several heart failure trials, ACE inhibitor or ARB use has been uniformly associated with lower AF risk 4, 5.
The findings for AF risk in patients with hypertension but not heart failure have been less clear. In analyses of incident AF as a secondary endpoint over 5–6 years’ follow-up in the Captopril Prevention Project (CAPPP) 16 and Swedish Trial in Old Patients with Hypertension-2 (STOP-H-2)17, neither study found ACE inhibitors to be associated with AF risk. In CAPPP, captopril was compared with a thiazide or a beta-blocker in hypertensive subjects 25–66 years of age; in STOP-H-2, enalapril or lisinopril were compared with a beta-blocker or a diuretic or both in subjects 70–84 years of age. On the other hand, in two trials in hypertensive subjects selected for high cardiovascular risk, ARB use was associated with lower AF risk in secondary analyses. In the Losartan Intervention for End Point Reduction in Hypertension (LIFE) trial 18, which studied losartan versus atenolol in hypertensive patients with left ventricular hypertrophy by electrocardiogram, losartan was associated with a 33% reduction in AF incidence over 4.8 years.
In the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial 19, which studied valsartan versus amlodipine in high-risk patients with diabetes, current smoking, elevated cholesterol, left ventricular hypertrophy, renal impairment, or clinically recognized cardiovascular disease, valsartan use was associated with a 16% reduction in AF incidence. Our findings add to this evidence by demonstrating lower AF risk with single-drug ACE inhibitor/ARB compared with diuretics in a general hypertensive population without heart failure. Differences in findings between studies may be due to the inclusion of subjects at different underlying risk of AF, due to incomplete ascertainment of AF events, or due to simultaneous use of antihypertensive agents from more than one therapeutic class, which makes it difficult to ascertain the effects of individual classes of drugs.
Beta-blockers may interfere with the recognition of AF symptoms by the patient due to slowed ventricular rates 20, and may decrease AF risk by several mechanisms. Beta-blockers inhibit renin secretion and may reduce atrial remodeling; they reduce sympathetically-mediated effects on automaticity and conduction, including shortening of the atrial refractory period; and they decrease the magnitude of potassium currents 6. In the perioperative setting, and particularly in the setting of cardiac surgery, beta-blockers reduce the risk of AF 21, and withdrawal of beta-blockers before surgery is associated with postoperative atrial arrhythmias 22. In patients with heart failure, most studies have found lower AF risk in beta-blocker recipients versus placebo 6. But despite several theoretical pathways by which beta-blockers might decrease the risk or recognition of incident AF, our findings do not suggest that they have this net effect in hypertensive patients without clinically recognized heart failure.
Hypertension, left ventricular hypertrophy, and heart failure increase the risk of incident AF 23–25. Existing evidence suggests that ACE inhibitor/ARB therapy reduces AF risk in patients with heart failure, hypertrophy, or other markers of high cardiovascular risk. The results of our study suggest that this benefit applies to single-drug users of ACE inhibitors/ARBs in the general hypertensive population as well.
Acknowledgments
Supported by grants HL068986, HL043201, HL073410, and HL068639 from the National Heart, Lung and Blood Institute, Bethesda, MD. Dr. Dublin was supported by grant AG028954 from the National Institute on Aging.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995;155:469–73. [PubMed] [Google Scholar]
- 2.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 3.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 4.Healey JS, Baranchuk A, Crystal E, Morillo CA, Garfinkle M, Yusuf S, Connolly SJ. Prevention of atrial fibrillation with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysis. J Am Coll Cardiol. 2005;45:1832–9. doi: 10.1016/j.jacc.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 5.Anand K, Mooss AN, Hee TT, Mohiuddin SM. Meta-analysis: inhibition of renin-angiotensin system prevents new-onset atrial fibrillation. Am Heart J. 2006;152:217–22. doi: 10.1016/j.ahj.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Nasr IA, Bouzamondo A, Hulot JS, Dubourg O, Le Heuzey JY, Lechat P. Prevention of atrial fibrillation onset by beta-blocker treatment in heart failure: a meta-analysis. Eur Heart J. 2007;28:457–62. doi: 10.1093/eurheartj/ehl484. [DOI] [PubMed] [Google Scholar]
- 7.Psaty BM, Heckbert SR, Koepsell TD, Siscovick DS, Raghunathan TE, Weiss NS, Rosendaal FR, Lemaitre RN, Smith NL, Wahl PW, Wagner EH, Furberg CD. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA. 1995;274:620–25. [PubMed] [Google Scholar]
- 8.Lemaitre RN, Psaty BM, Heckbert SR, Smith NL, Longstreth WT, Jr, Rosendaal FR. Hormone replacement therapy, prothrombotic mutations, and the risk of incident nonfatal ischemic stroke in postmenopausal women. Arterioscler Thromb Vasc Biol. 2002;22:1051–2. [PubMed] [Google Scholar]
- 9.Smith NL, Heckbert SR, Lemaitre RN, Reiner AP, Lumley T, Weiss NS, Larson EB, Rosendaal FR, Psaty BM. Esterified estrogens and conjugated equine estrogens and the risk of venous thrombosis. JAMA. 2004;292:1581–1587. doi: 10.1001/jama.292.13.1581. [DOI] [PubMed] [Google Scholar]
- 10.Saunders KW, Davis RL, Stergachis A. Group Health Cooperative. In: Strom BL, editor. Pharmacoepidemiology. 4. Chichester: John Wiley & Sons, Ltd; 2005. p. 234. [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.Savelieva I, Camm J. Is there any hope for angiotensin-converting enzyme inhibitors in atrial fibrillation? Am Heart J. 2007;154:403–6. doi: 10.1016/j.ahj.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Casaclang-Verzosa G, Gersh BJ, Tsang TS. Structural and functional remodeling of the left atrium: clinical and therapeutic implications for atrial fibrillation. J Am Coll Cardiol. 2008;51:1–11. doi: 10.1016/j.jacc.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 14.Tsang TS, Barnes ME, Abhayaratna WP, Cha SS, Gersh BJ, Langins AP, Green TD, Bailey KR, Miyasaka Y, Seward JB. Effects of quinapril on left atrial structural remodeling and arterial stiffness. Am J Cardiol. 2006;97:916–20. doi: 10.1016/j.amjcard.2005.09.143. [DOI] [PubMed] [Google Scholar]
- 15.Kumagai K, Nakashima H, Urata H, Gondo N, Arakawa K, Saku K. Effects of angiotensin II type 1 receptor antagonist on electrical and structural remodeling in atrial fibrillation. J Am Coll Cardiol. 2003;41:2197–204. doi: 10.1016/s0735-1097(03)00464-9. [DOI] [PubMed] [Google Scholar]
- 16.Hansson L, Lindholm LH, Niskanen L, Lanke J, Hedner T, Niklason A, Luomanmaki K, Dahlof B, de Faire U, Morlin C, Karlberg BE, Wester PO, Bjorck JE. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet. 1999;353:611–6. doi: 10.1016/s0140-6736(98)05012-0. [DOI] [PubMed] [Google Scholar]
- 17.Hansson L, Lindholm LH, Ekbom T, Dahlof B, Lanke J, Schersten B, Wester PO, Hedner T, de Faire U. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354:1751–6. doi: 10.1016/s0140-6736(99)10327-1. [DOI] [PubMed] [Google Scholar]
- 18.Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlof B, Ibsen H, Julius S, Kjeldsen SE, Lindholm LH, Nieminen MS, Devereux RB. Angiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol. 2005;45:712–9. doi: 10.1016/j.jacc.2004.10.068. [DOI] [PubMed] [Google Scholar]
- 19.Schmieder RE, Kjeldsen SE, Julius S, McInnes GT, Zanchetti A, Hua TA. Reduced incidence of new-onset atrial fibrillation with angiotensin II receptor blockade: the VALUE trial. J Hypertens. 2008;26:403–11. doi: 10.1097/HJH.0b013e3282f35c67. [DOI] [PubMed] [Google Scholar]
- 20.Page RL. Clinical practice. Newly diagnosed atrial fibrillation. N Engl J Med. 2004;351:2408–16. doi: 10.1056/NEJMcp041956. [DOI] [PubMed] [Google Scholar]
- 21.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 22.Bharucha DB, Kowey PR. Management and prevention of atrial fibrillation after cardiovascular surgery. Am J Cardiol. 2000;85:20D–24D. doi: 10.1016/s0002-9149(00)00903-6. [DOI] [PubMed] [Google Scholar]
- 23.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–4. [PubMed] [Google Scholar]
- 24.Psaty BM, Manolio TA, Kuller LH, Kronmal RA, Cushman M, Fried LP, White R, Furberg CD, Rautaharju PM. Incidence of and risk factors for atrial fibrillation in older adults. Circulation. 1997;96:2455–2461. doi: 10.1161/01.cir.96.7.2455. [DOI] [PubMed] [Google Scholar]
- 25.Verdecchia P, Reboldi G, Gattobigio R, Bentivoglio M, Borgioni C, Angeli F, Carluccio E, Sardone MG, Porcellati C. Atrial fibrillation in hypertension: predictors and outcome. Hypertension. 2003;41:218–23. doi: 10.1161/01.hyp.0000052830.02773.e4. [DOI] [PubMed] [Google Scholar]