Pigmented villonodular synovitis (PVNS) is a proliferation of the synovium that leads to villous or nodular changes of synovial-lined joints, bursae and tendon sheaths.1 It is rare and likely caused by either an inflammatory response or neoplastic formation of the synovium. Both the extra-and the intra-articular types appear in a nodular-localized and villous-diffuse variant. It usually affects single joints only, and bilateral involvement is extremely rare.2
CASE REPORT
A 30-year-old woman was referred to us because of a small lump that she had noted at her right lateral malleolus following an ankle sprain. The lump had enlarged over time and was painful on physical activity. The patient stated that the ankle was unstable.
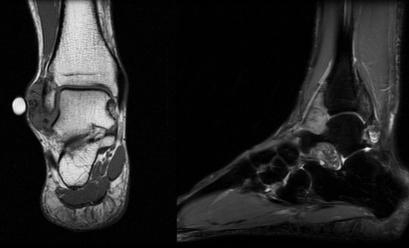
A nontender mass, 2 × 3 cm in size, at the lateral border of her right fibula was the only abnormal clinical finding. Plain radiographs showed no bony abnormalities, but magnetic resonance imaging (MRI) established an intra-articular well-defined mass in the right anterolateral ankle joint (Fig. 1).
Fig. 1. The magnetic resonance image (coronal and sagittal T1 and fast short-tau inversion-recovery [FSTIR] images) of the patient's right ankle shows an intra-articular well-defined localized mass in the anterolateral ankle joint and sinus tarsi without bony infiltration. The mass has an intermediate density T1 signal and a mildly high FSTIR signal, and it distends the ankle joint locally. On the gradient-echo images, blooming indicated hemorrhage and iron deposition.
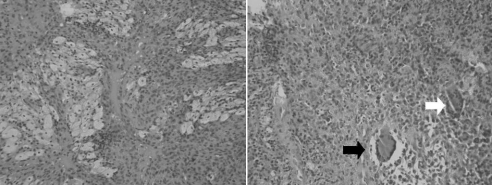
Surgery included ankle arthroscopy, open excision of the mass and repair of the lateral anterior talofibular ligament. Arthroscopy confirmed the PVNS, and this finding led to an arthroscopic synovectomy. Through a lateral arthrotomy we were able to enucleate the encapsulated tumour completely. We repaired the torn anterior talofibular ligament with use of nonabsorbable sutures. The patient had an uncomplicated postoperative course. The pathology report confirmed an intra-articular PVNS (Fig. 2).
Fig. 2. Characteristic photographs were taken from histologic findings of the bilateral pigmented villonodular synovitis. Left: There is a proliferation of histiocytes, with some (the light coloured cells) showing a lipid-filled cytoplasm (so-called “foamy macrophages”) (hematoxylin and eosin stain, original magnification × 100). Right. A field of histiocytes contains 2 reactive multinucleated histiocytic giant cells. The one on the right (white arrow) has a scattered arrangement of nuclei (a “foreign body” type giant cell), whereas that on the left (black arrow) has clear lipid in its cytoplasm and a wreath-like arrangement of nuclei (a Touton type giant cell) (hematoxylin and eosin stain, original magnification × 200).
Three years later at follow-up, the patient reported increasing deep discomfort in both ankles. A new mass had appeared on the left side but not on the right. According to the patient, both ankle joints were stable. Clinical examination revealed a mobile mass, about 2 × 2 cm in dimension, in the left sinus tarsi. Again, plain radiographs revealed no bony abnormality. Magnetic resonance images suggested a recurrence of the PVNS on the right side and confirmed the PVNS on the left side.
We excised the PVNS on the left side through a longitudinal incision above the sinus tarsi. The tumour extended throughout the sinus tarsi, underneath the extensor digitorum brevis muscle and medially through to the medial facet of the subtalar joint. The tumour infiltrated the interosseous ligament and the superior centimetre of the calcaneus bone. We carried out an intralesional excision as extensively as possible. Her postoperative course was uncomplicated. The pathology report confirmed PVNS.
A repeat exploration of the right ankle for the assumed PVNS recurrence demonstrated by the repeat MRI failed to identify any mass. The radiologist responsible noted that the recurrence was seen in the area where nonabsorbable stitches were placed to repair the lateral ligaments previously, giving an MRI signal similar to PVNS. Pathological examination of the tissue showed benign fibrofatty material with stitch granuloma.
A clinical and radiographic follow-up 17 months after the second surgery with bilateral repeat MRI demonstrated no recurrence of the PVNS. A further clinical and radiographic follow-up with repeat MRI was planned for the following year; however, the patient did not follow up.
DISCUSSION
The villous-diffuse variant of either extra-or intra-articular PVNS infiltrates aggressively into surrounding tissues such as the joint capsules and bone. Therefore, wide resection of the tumour is difficult and recurrence is more likely for the villous-diffuse variant, whereas the nodular-localized variant is episodic and seldom recurs after excision.3 Early diagnosis of PVNS is advised because delay may lead to significant local bony and soft-tissue destruction.4
The proposed treatment for primary disease is local excision for nodular-localized PVNS and extralesional excision including complete synovectomy or excision of the tendon sheath, capsulectomy and excision of affected bone for the villous-diffuse variant.3 Supportive treatment such as cryosurgery, phenol or hydrogen peroxide application is suggested to reduce the risk of recurrence. For recurrent lesions, postoperative radiotherapy is recommended. Arthrodeses and joint replacements are used to treat advanced arthritis secondary to PVNS.
Our patient's case shows a temporally independent bilateral onset of an intra-articular nodular-located and an extra-articular villous-diffuse PVNS in the hindfeet. Whereas the tumour on the right side had developed within more than 3 years and at the time of excision was fairly encapsulated, the tumour on the left side occurred more rapidly and infiltrated the surrounding tissues. This indicates 2 PVNS tumours with different degrees of aggressiveness in a single patient. Although the desired extralesional excision of the extra-articular villous-diffuse PVNS on the left side was not feasible in many areas, excision of the bilateral PVNS tumours, with additional bony curettage on the left, but without supportive therapy, has been sufficient to prevent tumour recurrence so far. As no PVNS was detected in the recent MRIs, a recurrence is highly unlikely. Magnetic resonance imaging for assumed PVNS recurrence may be misleading with respect to postoperative scar formation, but it remains the most accurate radiologic investigation for this condition.
Involvement of the foot and ankle occurs in fewer than 10% of patients with PVNS,3 and extra-articular localized nodular synovitis attached unilaterally to the subtalar joint has been reported.5 However, our patient's case of a bilateral symmetric PVNS of the ankle joint and the sinus tarsi is unique and, to our knowledge, is reported here for the first time.
Acknowledgments
We thank Enid Edwards, MD, Department of Pathology, St. Paul's Hospital, Vancouver, for contribution to the pathology reports.
Competing interests: None declared.
Correspondence to: Dr. A.S.E. Younger Department of Orthopaedics University of British Columbia 1144 Burrard St., #560 Vancouver BC V6Z 2A5 fax 604 683-3464 asyounger@shaw.ca
References
- 1.Goldman AB, DiCarlo EF. Pigmented villonodular synovitis: diagnosis and differential diagnosis. Radiol Clin North Am 1988;26: 1327-47. [PubMed]
- 2.Schwartz HS, Unni KK, Pritchard DJ. Pigmented villonodular synovitis. Clin Orthop Relat Res 1989;247:243-55. [PubMed]
- 3.Flandry F, Hughston JC. Pigmented villonodular synovitis. J Bone Joint Surg Am 1987;69:942-9. [PubMed]
- 4.Saxena A, Perez H. Pigmented villonodular synovitis about the ankle: a review of the literature and presentation in 10 athletic patients. Foot Ankle Int 2004;25:819-26. [DOI] [PubMed]
- 5.Villani C, Tucci G, Di Mille M, et al. Extra-articular localized nodular synovitis (giant cell tumor of tendon sheath origin) attached to the subtalar joint. Foot Ankle Int 1996;17:413-6. [DOI] [PubMed]