Abstract
We examined the relation between church attendance, membership in the Church of Jesus Christ of Latter-Day Saints (LDS), and major depressive episode, in a population-based study of aging and dementia in Cache County, Utah. Participants included 2,989 nondemented individuals aged between 65 and 100 years who were interviewed initially in 1995 to 1996 and again in 1998 to 1999. LDS church members reported twice the rate of major depression that non-LDS members did (odds ratio = 2.56, 95% confidence interval = 1.07-6.08). Individuals attending church weekly or more often had a significantly lower risk for major depression. After controlling for demographic and health variables and the strongest predictor of future episodes of depression, a prior depression history, we found that church attendance more often than weekly remained a significant protectant (odds ratio = 0.51, 95% confidence interval = 0.28-0.92). Results suggest that there may be a threshold of church attendance that is necessary for a person to garner long-term protection from depression. We discuss sociological factors relevant to LDS culture.
Keywords: Church Attendance, Depression, Latter Day Saints
LATE-LIFE depression has been estimated as the second major cause of disability among older adults (Judd, Akiskal, & Zeller, 2000), affecting 6.5 million of Americans 65 years of age (Shear, Roose, Lenze, & Alexopoulos, 2005). Incidence rates that include subsyndromal cases vary between 17.1 and 133.5 per 1,000 risk years (Meller, Fichter, & Schroppel, 1996; Palsson, Ostling, & Skoog, 2001), whereas rates of major depression and dysthymia range between 12.5 and 24.0 per 1,000 risk years (Forsell & Winblad, 1999). Further, those with a history of late-life depression exhibit a doubling in risk for dementia (Jorm, 2001). Some studies (Kessler, Foster, Webster, & House, 1992; Palsson, et al.) but not all (Newmann, Engel, & Jensen, 1991; Steffens et al., 2000) have found that rates of depression steadily increase with age, after the age of 65 years. Geriatric depression increases overall public health burden by withdrawal of depressed individuals from social contacts, noncompliance in medication and other health care practices (Katrona, 1994), and mortality (Rozzini, Frisoni, Sabatini, & Trabucchi, 2002). Further, depression in later life is often underdiagnosed (Friedhoff, 1994; Ginsberg, 2005) and undertreated (Mulsant & Ganguli, 1999). As the number of older people with psychiatric needs increases, the current health care system will face a great challenge in meeting the needs of this group (Bartels et al., 2002).
Several factors have been shown to increase risk for new-onset depression in late life, including a prior history of depressive symptoms (Palsson et al., 2001), female gender (Sonnenberg, Beekman, Deeg, & van Tilburg, 2000), functional impairments (Cummings, Neff & Husaini, 2003), and stressful life events (Shear et al., 2005). Some researchers suggest that religious involvement may be associated with lower depression rates by means of the encouragement of coping strategies through spiritual, intellectual, and social avenues (Husaini, Blasi, & Miller, 1999). Still other researchers have found no such effect in both cross-sectional studies (Courtenay, Poon, Martin, Clayton, & Johnson, 1992; Spendlove, West, & Stanish, 1984) and longitudinal studies (Bosworth, Park, McQuoid, Hays, & Steffens, 2003; Braam, Beekman, Deeg, Smit, & van Tilburg, 1997). Church attendance, one aspect of religious practice, helps connect individuals with their social network, conferring a sense of belonging that has been associated with reduction in depression risk in cross-sectional studies (Idler & Kasl, 1997; Parker et al., 2003) and longitudinal studies (Strawbridge, Shema, Cohen, & Kaplan, 2001). Such participation, particularly at the end of life, can help bring about a sense of closure for events that were unexplainable and bring some meaning to the experience of physical and emotional pain (Koenig, Pargament, & Nielson, 1998; Van Ness & Larson, 2002). Religious involvement has been associated with a reduction in depression among functionally disabled (Idler & Kasl) and medically ill (Koenig, George, & Peterson, 1998) older adults. Church attendance often encourages other more private religious behaviors, such as prayer, meditation, scripture reading, and caring for others' needs (Koenig, 1993).
Methodological differences among the published studies on the association between religious involvement and late-life depression may explain the divergent findings. Most studies measure depression as a symptom count, whereas fewer use an approach based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) to categorize major depression (Boey, 2003). The majority of studies are also cross-sectional ones, precluding causal inference. Among longitudinal studies, typically researchers assess only current depression at each interview, ignoring additional depressive episodes with onset during the interval but that resolved prior to the follow-up interview. Further, the association between religious involvement and depression may be stronger in strongly religious communities where the influence of the doctrine pervades the lives of its members (Braam et al., 2001). However, studies are very rare that examine this association in the cultural context of religiously homogeneous populations in which religious behavior may be more salient. Finally, we found no published studies that examined the association between religious practice and subsequent depressive episodes while statistically controlling for prior depression history, health, and functional status, all known to increase risk.
There is one such population-based study that provides an excellent opportunity to examine the effects of religious involvement, specifically church attendance, in a highly religious community, located in Cache County, Utah. Residents of Cache County suffer relatively lower rates of mortality before age 85. They have a conditional life expectancy for men at age 65 that, in the 1990 U.S. Census, was the highest in the country (Murray, Michaud, McKenna, & Marks, 1998), exceeding national norms by almost 10 years (Manton, Stallard, & Tolley, 1991). Older adult residents of this rural county in northern Utah are predominantly members of the Church of Jesus Christ of Latter-Day Saints (LDS; 92%), with more active members reported to have lower rates of mental health problems (Merrill & Salazar, 2002). Some 76% of LDS members (vs 34% of non-LDS members) report church attendance at weekly or greater frequency (Norton, Skoog, Franklin, et al., 2006). Strong LDS prohibitions against use of alcohol and tobacco may at least partially account for the greater longevity of Cache County residents. Additional explanations may include an agricultural past with high levels of activity in midlife and the absence of significant poverty as found also in the upper Midwest, which is another region whose residents show similarly high longevity (Murray et al.).
The prevalence of major depression among those aged 65 and older in this population has been previously reported as 4.3% in women and 3.0% in men (Steffens et al., 2000). This is slightly higher than has typically been reported in North American studies using DSM criteria (Bland, Newman, & Orn, 1998; Regier et al., 1993), but it is much higher than the 1.4% in women and 0.4% in men in the NIMH Epidemiological Catchment Area Study (Koenig, Blazer & Sheikh, 1992). Thus, the somewhat higher rates of depression among older residents in a highly religious community prompt investigation into the nature of the association between church attendance and depression risk in this population. Findings from such research may be informative for studies of late-life mental health in other communities with a predominant religious group.
We have previously reported results from the Cache County Study on Memory Health and Aging. In that community sample of 4,468 older adults, we found that regular church attendance was associated with a reduced prevalence of depression in women but increased prevalence in men, after we controlled for marital status, education, age, health and functional status, and religious affiliation (Norton, Skoog, Franklin, et al., 2006). The study utilized a large community-based sample, without the selection bias typical of clinical studies (van Exel, Stek, Deeg, & Beekman, 2000). It achieved an exceptionally high participation rate (90%); however, the study had a cross-sectional design.
We now present longitudinal data that ascertained depressive episodes during a 3-year interval after measurement of frequency of church attendance. Given the substantially increased risk for depression among older adults with a prior depression history (Norton, Skoog, Toone, et al., 2006; Murphy et al., 2002), we also sought to determine whether the effects of church attendance would be equivalent for those with and without a prior history of depression. We further hypothesized that the inverse association would be robust even after we statistically controlled for medical and functional status.
Methods
Participants
A detailed description of the sample and methods is provided elsewhere (Breitner et al., 1999). Briefly, the Cache County Study on Memory Health and Aging enrolled 5,092 permanent residents of the county aged 65 and older as of January 1, 1995 (90%). The study employed a comprehensive multistage case-ascertainment protocol for dementia in the initial and 3-year follow-up waves of ascertainment. We found that 4,546 (89%) of the residents were nondemented and provided self-report data at the initial interview (356 or 7% had prevalent dementia and 190 or 4% had proxy report at initial interview). Of these, 3,256 (72%) provided self-report and 92 (2%) provided proxy data at the 3-year follow-up; 505 (11%) were deceased; 496 (11%) refused to participate; 166 (3%) had moved out of the area; and 31 (1%) did not participate at follow-up because they had been identified with incident dementia beforehand. Of the 3,256 residents there were 94 (3%) with incident dementia who we therefore excluded from the present study. We included individuals with mild cognitive impairment and normal cognition. We removed participants who had never married because there were so few of them (n = 38 or 1%). Of the remaining 3,124 participants, there were 135 (4%) with some missing data; our final sample size was 2,989. We removed participants with dementia because dementia is an exclusionary criterion in the diagnosis of major depression according to the fourth edition of the DSM (DSM-IV) and because such individuals often exhibit depressive features as a symptom of dementia (Alexopoulos, Meyers, Young, Mattis, & Kakuma, 1993; Kral & Emery, 1989). We also removed those individuals who could not provide their own depression data, necessitating proxy reports.
Interview Procedure
The dementia-ascertainment protocol included the following tests, which were conducted in the participant's home: a cognitive screening test, a semistructured clinical interview with a knowledgeable informant, and then, for those with possible dementia, an in-depth clinical assessment, conducted by nurse and psychometrician. Individuals with a working diagnosis of dementia were examined by a geropsychiatrist and underwent MRI scanning and standard laboratory tests for differential diagnosis. A panel of expert clinicians reviewed all available data and assigned final consensus diagnoses (Breitner et al., 1999).
We obtained all measures from the baseline or follow-up interviews, except for social network, which we collected from a mail-in questionnaire (80% return rate). We obtained informed consent and all procedures received approval by the Institutional Review Boards of Utah State University, Duke University, and the Johns Hopkins University.
To improve data quality, we had a 10% sample of the interviews taped (with consent) and reviewed by the project's field supervisors. Quality Assurance specialists carefully checked responses for consistency and conformity to interview protocols, requiring interviewer clarification for potential errors or ambiguities. We had the data entered in duplicate, with cross-checks for accuracy.
Depression: Prior History at Initial Interview and Subsequent New Onset
A modified version of the NIMH Diagnostic Interview Schedule (DIS; Robins, Helzer, Croughan, & Ratcliff, 1981; also see Helzer & Robins, 1988) was completed at baseline and follow-up interviews. The DIS has been widely used in epidemiologic field studies and its psychometric properties have been well characterized (Helzer et al., 1985; Murphy, 1995). Psychometric properties of the DIS for lifetime mood disorders, comparing lay interviewers' and psychiatrists' ratings, has been shown to be κ = 0.63, sensitivity = 80%, and specificity = 84% overall; sensitivity = 79% and specificity = 81% in current patients; and sensitivity = 82% and specificity = 67% in former patients (Robins et al.). Our modification included three gateway questions with the stem “in your lifetime, have you ever had a period of 2 weeks or more when, nearly every day you…,” which was followed with three question stimuli: “felt sad, blue, or depressed,” “lost all interest and pleasure in the things that you usually cared about or enjoyed,” and “felt unusually cross or irritable” (Norton, 2001; Steffens et al., 2000). Participants endorsing at least one of these were also asked about appetite or weight change, sleep or concentration difficulties, restlessness, diminished energy level, guilt, or suicidal ideation. At baseline we asked for age of onset of first, most recent, and most severe episode. At follow-up we asked for symptoms and the onset and duration of each distinct episode in the interval.
Following the example of Blazer, Hughes, and George (1987) and using DSM-IV criteria when possible (Steffens et al., 2000), we diagnosed prior depressive episodes at baseline and each subsequent new-onset episode. We coded prior depression history as “major” if at least one episode included endorsement of five or more DIS symptoms including sadness or loss of interest, as “minor” if no prior episodes met this criterion, and as “none” if no prior episodes were reported. We coded new-onset major depression as positive if at least one episode in the 3-year follow-up interval met the aforementioned criterion for major depression (with onset after baseline interview date) and negative otherwise.
Church Attendance at Initial Interview
We coded frequency of attendance at religious services and activities as never, less than once per month, one or two times per month, weekly, and more than once per week. We also asked about religious affiliation, with available responses of Catholic, Protestant, LDS, Jewish, other, and no religion. There were 36 participants who indicated no religion, but frequency of church attendance was not queried for these individuals and because such information could not be inferred, we removed them from the sample. We dichotomized religious affiliation into LDS (92%) versus non-LDS.
Medical and Functional Status at Initial Interview
As the Cache County Study's focus was on dementia, the health status interview focused on vascular health conditions and events. For the present study, we utilized these data to create an indirect assessment of overall health status, calculated as the number of the following vascular health problems endorsed: stroke, transient ischemic attack, hypertension, hyperlipidemia, coronary bypass surgery, diabetes mellitus, and heart attack, myocardial infarction, or coronary thrombosis. The vascular health problems score ranged from 0 to 7 (M = 1.20, SD = 1.12). We coded functional impairment as the number of activities of daily living (ADLs) for which the participant reported needing assistance, including both basic and instrumental ADLs. The resulting ADL problems score ranged from 0 to 12 (M = 1.50, SD = 1.20). At initial interview, the number of current medications, another indicator of health (excluding all psychotropic medications), ranged from 0 to 20 (M = 4.82, SD = 3.32).
Demographics and Social Support at Initial Interview
We scored age and reported education as continuous measures, in years. We grouped the reported marital status into married, widowed, and separated or divorced. We measured social support from the mail-in questionnaire (completed immediately after baseline interview) according to the reported frequency of two types of contact—“getting together with family, friends or neighbors” and “attending meetings of social clubs, groups, or organizations such as bridge clubs, book clubs, hospital volunteers, gardening clubs, Rotary club, Kiwanis, and the VFW.” We code each type of contact from 1 (rarely or never) to 6 (usually every day). We combined these two variables into a single measure—social contacts at least twice weekly—which was the median level of contact. This captured social involvement in excess of a single, possibly routine, activity occurring only weekly.
Statistical Analysis
We computed logistic regression models to test for the effect of church attendance on new-onset major depression, both before and after adjustment for other factors known to increase depression risk. To first reexamine the apparently higher depression rate among LDS members that we found in our cross-sectional study (Norton, Skoog, Franklin, et al., 2006), we included religious affiliation (LDS vs non-LDS) in our initial model. Subsequent models added in frequency of church attendance (Model 2), gender (Model 3), marital status, education, age, health status (Model 4), and finally, prior depression history (Model 5). We computed odds ratios by using the fitted logistic regression model parameters, with corresponding 95% Wald confidence intervals. We computed all statistical analyses by using Statistical Package for the Social Sciences, version 13.0.
Results
Sample Description
The final longitudinal sample included 1,270 men (42%) and 1,719 women (58%), with a baseline mean age of 73.8 years (SD=6.3) and mean education of 13.4 years (SD = 2.8). From reports at initial interview, there were 2,166 participants (73%) with no prior depression, 402 (13%) reporting prior minor depression, and 421 (14%) reporting prior major depression. As to religious affiliation, there were 2,804 LDS members (94%), 101 Protestants (3%), 28 Catholics (1%), and 56 participants (2%) from a variety of 18 additional affiliations (each with 12 or fewer adherents).
Attrition
To examine potential attrition bias, we compared those individuals who remained in our final sample with those who dropped out as a result of death, refusal, moving away, or incident dementia. Longitudinal participants were more likely to be LDS members [χ2(1, N = 4,473) = 6.08, p = .014], married [χ2(2, N = 4,473) = 45.6, p < .001], younger by approximately 4 years [t(4471) = 18.6, p < .001], more highly educated by approximately 0.5 years [t(4471) = 5.2, p < .001], report higher frequency of church attendance [χ2(4, N=4,396)=121.8, p < .001], have approximately 0.2 fewer lifetime vascular health problems [t(4471)=5.0, p < .001], and take approximately 0.5 fewer medications [t(4471) = 4.4, p < .001]. There was atrend for female participants to bemore likely than male participants to participate at follow-up [χ2(1, N = 4,473) = 3.29, p = .070], although this did not reach statistical significance. Prior depression history [χ2(2, N = 4,473) = 3.92, p = .141] was not associated with longitudinal participation.
Bivariate Associations
The following categorical variables were significantly associated with major depression in simple bivariate analyses: gender, prior depression history, LDS church affiliation, and frequency of church attendance. However, marital status was not significantly associated with major depression (Table 1). Among the continuous variables that we examined, individuals who experienced major depression over the interval reported more ADL problems, more health problems, and were taking more nonpsychotropic medications at initial interview, compared with those who did not. Age and education level were not significantly related to major depression.
Table 1.
Bivariate Associations with New-Onset Depression in 3-Year Intervals
|
n (row %) |
||||
|---|---|---|---|---|
| Variable | No Major Depression | Major Depression | Row Total | Test Statistic (p Value) |
| Gender | ||||
| Male | 1206 (95) | 64 (5) | 1270 | χ2(1, n = 2,989) = 11.8 (p = .001) |
| Female | 1577 (92) | 142 (8) | 1719 | |
| Prior depression | ||||
| None | 2099 (97) | 67 (3) | 2166 | χ2(2, n = 2,989) = 235.8 (p < .001) |
| Minor | 362 (90) | 40 (10) | 402 | |
| Major | 322 (77) | 99 (23) | 421 | |
| Religious affiliation | ||||
| LDS | 2604 (93) | 200 (7) | 2804 | χ2(1, n = 2,989) = 4.1 (p = .043) |
| Non-LDS | 179 (97) | - | 185 | |
| Church attendance | ||||
| Never | 201 (90) | 22 (10) | 223 | χ2(4, n = 2,989) = 17.0 (p = .002) |
| <1/month | 204 (91) | 21 (9) | 225 | |
| 1-2/month | 187 (89) | 24 (11) | 211 | |
| 1/week | 1336 (93) | 94 (7) | 1430 | |
| >1/week | 855 (95) | 45 (5) | 900 | |
| Marital status | ||||
| Married | 1998 (93) | 152 (7) | 2150 | χ2(2, n = 2,989) = 1.0 (p = .596) |
| Widowed | 698 (94) | 46 (6) | 744 | |
| S-D | 87 (92) | - | 95 | |
| ADL problems | 1.5 (1.1) | 2.1 (1.4) | t(2,987) = 4.8 (p < .001) | |
| Health problems | 1.2 (1.1) | 1.4 (1.1) | t(2,987) = 2.8 (p = .004) | |
| Medications (nonpsychotropic) | 4.7 (3.3) | 6.2 (3.5) | t(2,987) = 6.3 (p < .001) | |
| Age (years) | 73.8 (6.3) | 73.5 (6.2) | t(2,987) = 0.7 (p = .510) | |
| Education (years) | 13.4 (2.9) | 13.1 (2.5) | t(2,987) = 1.6 (p = .112) | |
| Total | 2783 (93) | 206 (7) | 2989 | |
Note: ADL problems, health problems, medications, age, and education are shown as means with standard deviations in parentheses. Em dashes signify that the number was suppressed in compliance with Center for Medicare and Medicaid Services privacy policy. LDS = Church of Jesus Christ of Latter-Day Saints; S-D = separated or divorced; ADL = activity of daily living.
Logistic Regression Models
In Model 1, LDS participants had significantly higher odds of new-onset major depression than non-LDS participants did (Table 2). Model 2 added in frequency of church attendance, which showed that those participants attending weekly and more often than weekly had significantly lower odds of new-onset major depression than those who never attend, whereas those attending less often than weekly did not differ from those who never attend. We next tested a LDS Affiliation × Church attendance interaction, which, at p = .999, was nonsignificant. (We repeated this interaction test with church attendance dichotomized into weekly or greater vs less than weekly, also with a nonsignificant result: p =.394.) Therefore, we removed the interaction term. Controlling for gender had no effect on the association of church attendance with depression, and, at p = .962, a Gender × Church Attendance interaction was not significant (We repeated this interaction test with the dichotomized church attendance variable, also with a nonsignificant result: p =.505.) Therefore we removed it as well. In the fourth model with the addition of age, marital status and education (socioeconomic indicators), ADL problems (an activity level indicator), vascular health problems, and medications (health status indicators), the effect of weekly church attendance was reduced to nonsignificance, whereas attendance more often than weekly remained significant.
Table 2.
Logistic Regression Models for Association of Baseline Church Attendance, Demographic, and Health Variables and Subsequent New-Onset Major Depression (n = 2,989)
| OR (95% CI) |
|||||
|---|---|---|---|---|---|
| Variable | Model 1: LDS | Model 2: Religious Involvement | Model 3: Female Gender | Model 4: Demographics + Health Status | Model 5: Depression Levels |
| LDS affiliation | 2.29 (1.00-5.23) | 2.92 (1.27-6.75) | 2.88 (1.25-6.65) | 2.61 (1.12-6.07) | 2.56 (1.07-6.08) |
| Church attendance | |||||
| <1/month | 0.95 (0.50-1.78) | 0.96 (0.51-1.80) | 1.06 (0.55-2.03) | 1.05 (0.53-2.08) | |
| 1-2/month | 1.10 (0.59-2.04) | 1.08 (0.58-2.00) | 1.25 (0.66-2.37) | 1.20 (0.62-2.36) | |
| 1/week | 0.59 (0.36-0.96) | 0.57 (0.37-0.93) | 0.68 (0.41-1.14) | 0.66 (0.38-1.12) | |
| >1/week | 0.43 (0.25-0.73) | 0.42 (0.25-0.72) | 0.49 (0.28-0.87) | 0.51 (0.28-0.92) | |
| Female gender | 1.72 (1.27-2.34) | 1.59 (1.14-2.22) | 1.20 (0.85-1.70) | ||
| Marital status | |||||
| Widowed | 0.66 (0.48-0.99) | 0.56 (0.37-0.84) | |||
| S-D | 0.72 (0.32-1.62) | 0.60 (0.26-1.37) | |||
| Education: years | 1.00 (0.99-1.06) | 1.02 (0.96-1.08) | |||
| Age: years | 0.98 (0.95-1.00) | 1.00 (0.97-1.03) | |||
| ADL problems (no.) | 1.26 (1.16-1.38) | 1.19 (1.08-1.31) | |||
| Vascular health problems (no.) | 1.04 (0.91-1.18) | 1.02 (0.89-1.17) | |||
| Nonpsychotropic meds (no.) | 1.09 (1.04-1.14) | 1.06 (1.01-1.11) | |||
| Prior depression history | |||||
| Minor | 3.33 (2.18-5.08) | ||||
| Major | 8.19 (5.75-11.67) | ||||
Note: For the variables, the reference categories are married (marital status); never attend (church attendance); none (prior depression history); and all other religious affiliations (LDS affiliation). ORs are adjusted for all other variables in the model. The LR chi-square, degrees of freedom, and p values are as follows: Model 1, χ2 = 4.97, df = 1, p = .026; Model 2, χ2 = 19.58, df = 4, p = .001; Model 3, χ2 = 12.75, df = 1, p < .001; Model 4, χ2 = 57.03, df = 7, p < .001; Model 5, χ2 = 139.98, df = 2, p < .001. OR = odds ratio; CI = confidence interval; LDS = Church of Jesus Christ of Latter-Day Saints; S-D = separated or divorced; ADL = activity of daily living.
In the final step, we added prior depression history to the model, and it was the strongest predictor of new-onset major depression. There was more than a threefold higher rate among those participants with prior minor depression (compared with those with no depression history), and more than an eightfold higher rate among those with prior major depression. However, with its addition to the model, LDS affiliation remained significant, as did church attendance more often than weekly.
We next determined that neither prior depression history nor LDS affiliation moderated the inverse association between church attendance and new-onset major depression (two-way interactions with church attendance: p = .951 and p = .693, respectively). Likewise, three-way LDS Affiliation × Church Attendance × Prior Depression History interaction was nonsignificant (p = .830). We removed all nonsignificant interaction terms.
To explore social networks as a potential mediator, we reran the final model, adjusting for whether the participant reported at least twice weekly in-person social contacts with family or friends (model not shown). Odds ratios (ORs) for weekly church attendance dropped from OR=0.66 to OR=0.59 (95% confidence interval or CI = 0.33-1.07; value change from p = .067 to p = .081), and those for more-than-weekly church attendance increased from OR=0.51 to OR=0.54 (95% CI=0.28-1.02; value change from p=.013 to p=.058), suggesting that at least some of the apparent effect of church attendance is mediated through social network contacts.
Figure 1 demonstrates the higher rates of new-onset major depression among LDS members and among those with a prior depression history, and lower rates among those with church attendance at least weekly. Further, Figure 1 illustrates the nonsignificant interaction effects such that more frequent church attendance is associated with lower new-onset major depression rates within each religious affiliation, and within prior depression history subgroups.
Figure 1.
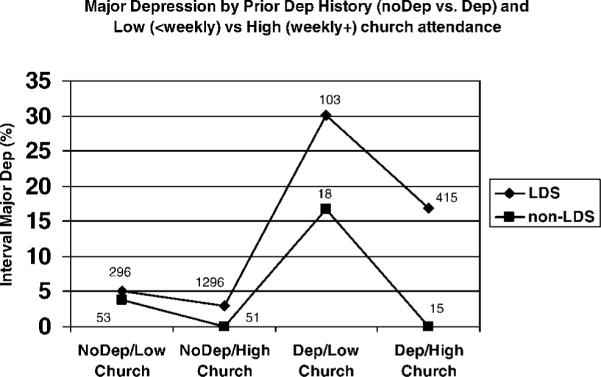
Graphical depiction of nonsignificant (p = .830) three-way interaction between Church of Jesus Christ of Latter-Day Saints (LDS) affiliation, church attendance, and prior depression (Dep) history on interval major depression reported at the 3-year follow-up (sample sizes given with each data point).
Discussion
We examined the association between church attendance and risk for new-onset major depression over a 3-year interval in this community-based sample of older adults, primarily LDS members. Church attendance at least weekly was associated with significantly lower odds of new-onset major depression. Weekly church attendance became nonsignificant after we controlled for demographics and health status, which is consistent with the literature showing increased rates of depression among widowed elderly persons (Umberson, Wortman, & Kessler, 1992) and those with poorer health (Blazer, 2002) and functional impairments (Cummings et al., 2003). Poor health and functional difficulties may also limit church attendance. However, attendance more often than weekly remained significant even after we controlled for these factors and the most powerful predictor—a prior history of depression (Palsson et al., 2001). This effect was diminished to nonsignificance after adjustment for social network (though the trend for lower depression rates among those with frequent attendance persisted), suggesting that some of the apparent beneficial effects of church attendance derive from the increased contact with one's social network. To our knowledge, this is the first study to longitudinally examine the net effect of church attendance after all of these controls.
Church attendance more often than weekly is indicative of a higher level of engagement, including midweek participation in auxiliary organizations and volunteer church callings. Such activities enhance interpersonal attachments through an added exchange of affection, respect, sociability, and companionship between members than what may be afforded by lower levels of involvement (Duke, 1998). Old age and disability often necessitate a shift in focus away from what one produces and accomplishes as the basis for self-worth, which are the typical basis in earlier adult life (Koenig, 1994). Christian theology (including LDS) provides strong assurance that each individual has inherent value and worth, regardless of abilities (Sapp, 1987). Furthermore, other theologies as well as nontheological value systems and ethical codes might encourage adherents to internalize similar beliefs that may reduce depression risk. These data provide some evidence that frequent reinforcement of these notions through high levels of religious participation, regardless of affiliation, may have a beneficial effect on the reduction in depression risk, even for those individuals with a prior history of depression.
New-onset major depression was about 1.6 times as frequent in women as in men, a common finding across many studies (Sonnenberg et al., 2000), though this effect became nonsignificant after we controlled for prior depression history. Consistent with cross-sectional findings (Norton, Skoog, Franklin, et al., 2006), we also found that participants with LDS affiliation reported twice as much new-onset major depression as their non-LDS counterparts, even after we controlled for all other variables. These results are in contrast to lower rates of mental health problems found among younger LDS (vs younger non-LDS) individuals (Judd, 1998). One factor that may contribute to higher rates of depression among older LDS members is feeling guilt or inadequacy at not living up to high expectations for compliance with church doctrine and religious practices (Bergin, Stinchfield, Gaskin, Masters, & Sullivan, 1988).
Older LDS individuals may also experience a more noticeable social role loss in late life as important positions of church leadership are dramatically curtailed, typically given to younger members of the congregation. Older adults who are not of the LDS faith might not have experienced such heavy involvement in organizational power within their respective churches and thus may not have experienced as dramatic a loss of important role(s) within the church upon reaching old age, particularly for men (Cnaan & Helzer, 2004).
LDS individuals may also be somewhat more culturally conditioned to disclose psychological problems, given that they attend monthly testimony meetings where individuals publicly and extemporaneously bear testimony to their religious beliefs, and how these beliefs have helped them cope with life's adversities and make important decisions. “Feelings of profoundest concern are often expressed: appreciation of good family relationships, thanksgiving for blessings…” (Jolley, 1992, p. 502). Through this sharing of very personal psychological feelings, those listening are able “to understand the message both intellectually and spiritually” (Christensen, 1992, p. 1,471). It is speculated that this practice may translate to openness to discuss psychological problems with research interviewers, potentially resulting in apparently higher rates of depression among LDS individuals.
LDS doctrine teaches of an afterlife that includes a perfecting of physical and cognitive abilities, as well as the joy of eternal marriages and families. Thus, many older LDS individuals who feel a degree of worthlessness given their present limitations, and who also have many deceased loved ones, regularly question the purpose for their continued existence in mortality.
Another factor that may affect higher rates of new-onset major depression among LDS members is that non-LDS residents may be particularly resilient. The relatively small number of non-LDS individuals living in Cache County may likely have made a conscious choice to live in a pervasively LDS environment and may not require the levels of social support most people would find desirable. Conversely, LDS members who do not attend church may experience some degree of social isolation given that the community support structure revolves largely around church activity. Additionally, more active LDS churchgoers may be reluctant to try too hard to “reactivate” fellow adherents who have stopped attending church. Generalizability of these findings may therefore be somewhat limited in other religious groups.
Limitations
Because of the population-based nature of the study, depression was not assessed by physicians but by trained lay interviewers, and epidemiologic instruments for such largescale fieldwork may have limits to psychometric stability (Regier et al., 1998). Further, our use of a skip-out interview strategy with the DIS, though common in epidemiological research, has the potential for underdiagnosis, given that depression in late life can appear with a symptom profile that differs from that found in younger adults (Gallo & Rabins, 1999). A study comparing the DIS and the psychiatrist-rated Schedules for Clinical Assessment in Neuropsychiatry revealed a bias toward underreporting (particularly in men), suggesting that associations with risk factors are likely to be conservative (Eaton, Neufeld, Chen, & Cai, 2000).
Frequency of church attendance, though perhaps the most common metric used in studies of religiosity, is but a single aspect of a multidimensional construct (Judd, 1999). Therefore, this study does not offer in-depth explanations for the inverse association with depression in this population. It remains unclear whether the effect has more to do with enhanced understanding of religious doctrine and sense of life purpose through religious study in a group setting, a sense of reconciliation with a higher power, or enhanced social contacts and support from fellow church members (Hoult, 1958).
Although we included statistical controls for social network, health status, and functional limitations, there may be other potential confounders that we omitted as they were unavailable. Those persons who attend church more than once weekly may have higher levels of vitality or energy that allow them to engage in a wide range of activities (church, hobbies, community service). It is conceivable that the lower levels of depression at higher church attendance levels may be largely due to this greater overall vitality rather than church attendance alone.
Several variables were associated with nonresponse at follow-up which may have somewhat biased our results, most notably church affiliation, frequency of church attendance, and marital status. Because our longitudinal sample had a slightly higher proportion of married LDS individuals with high church attendance, compared with our baseline sample, we probably had reduced statistical power to detect associations. However, the strongest predictor of new-onset major depression-prior depression history—was not related to attrition.
The inverse association between church attendance and major depression reported previously in women (Norton, Skoog, Franklin, et al., 2006) was again found in the present longitudinal study. However, the opposite finding of higher rates of depression among men who attended church more often was no longer apparent with longitudinal follow-up. Although not enough for a significant interaction, the effects were somewhat stronger for women who exhibited a 40% and 54% reduction in depression risk for those at weekly and greaterthan-weekly levels of attendance, respectively, relative to depression rates for women attending less often than weekly. Corresponding reductions in risk for men were 25% and 43%, respectively. Additionally, men were more likely to drop out than women, both in general and at higher baseline church attendance levels. This nonrandom attrition may have affected our results (data not shown).
As we already mentioned, these findings may not generalize to all populations of older adults but may be applicable to other populations with a predominant religious group. Although LDS theology includes some unique doctrines, it has many other theological aspects common to other religious groups that may have equal salience in the individual lives of its members. Members of other highly religious communities may exhibit similar cultural influences that place a high value on the application of spiritual coping to life's challenges, successful marriages, and parenting that could place their members at similar risk for depression when such ideals are unmet in the lives of individual members. Generalizability of this predominantly LDS population is enhanced by national studies reporting that LDS members have average socioeconomic status and similar overall happiness, marital happiness, and self-esteem (Heaton, Goodman, & Holman, 1994), and on average “flat” (normal) personality profiles on the Minnesota Multiphasic Personality Inventory (Judd, 1998).
Conclusions
The present study is our second report in a series of studies addressing the association between church attendance and new-onset major depression among members of the Cache County Study cohort, a group exhibiting high levels of church attendance (Norton, Skoog, Franklin, et al., 2006). Noted strengths are that it is a population-based study with a 90% participation rate at in-person interview, conferring significant protection against response bias (Norton, Breitner, Welsh, & Wyse, 1994). Further, our models controlled for potential confounding factors of physical health, functional abilities, marital status, and education. We found rates of new-onset major depression to be twice as high among LDS participants as among non-LDS participants. Further, we established a significant inverse association between frequency of church attendance and new-onset major depression, even net of the effect of the highly predictive risk factor of prior depression history.
Church attendance often encourages private religious behaviors such as prayer, meditation, and scripture reading, as well as public behaviors such as volunteerism (Koenig, 1993). Future studies could expand on the present work by examining these as potential mediators in the church attendance-depression association and the extent to which the effect of these behaviors may be moderated by gender (whereas church attendance was not). The extent to which particular aspects of church attendance may differentially moderate the effect of stressful life events should also be studied.
Acknowledgments
This work was supported by the National Institutes of Health under Grants AG11380 and AG21136. Portions of this article were presented in February, 2002 at the annual conference of the American Association for Geriatric Psychiatry, Orlando, Florida.
We thank the study participants and their families for their generosity in willingness to participate. We also thank Drs. Chiadi Onyike, Curt Canning, and Ronald Munger for their careful reviews of the manuscript. Other Cache County Study investigators involved in the project are as follows (in alphabetic order): James Anthony, PhD; Erin Bigler, PhD; Ron Brookmeyer, PhD; James Burke, MD, MPH; Michelle Carlson, PhD; Eric Christopher, MD; Jane Gagliardi, MD; Robert Green, MD; Andrea Hart, PhD; Kate Hayden, PhD; Christine Hulette, MD; Liz Klein, MPH; Carol Leslie, MA; Constantine Lyketsos, MD, MHS; Richard A. Miech, PhD; John Morris, MD; Ronald Munger, PhD; Chiadi Onyike, MD; Truls Østbye, MD, PhD; Ron Petersen, MD; Roxane Pfister, MS; Carl Pieper, PhD; Kathy Piercy, PhD; Brenda Plassman, PhD; Peter Rabins, MD; Pritham Raj, MD; Russell Ray, MS; Linda Sanders, MPH; Martin Steinberg, MD; Marty Toohill, PhD; Leslie Toone, MS; Jeannette J. Townsend, MD; Heidi Wengreen, PhD; Nancy West, PhD; Michael Williams, MD; and Bonita W. Wyse, PhD.
References
- Alexopoulos GS, Meyers BS, Young RC, Mattis S, Kakuma T. The course of geriatric depression with “reversible dementia”: A controlled study. American Journal of Psychiatry. 1993;150:1693–1699. doi: 10.1176/ajp.150.11.1693. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Dums AR, Oxman TE, Schneider LS, Areán PA, Alexopoulos GS, et al. Evidence-based practices in geriatric mental health care. Psychiatric Services. 2002;53:1419–1431. doi: 10.1176/appi.ps.53.11.1419. [DOI] [PubMed] [Google Scholar]
- Bergin AE, Stinchfield RD, Gaskin TA, Masters KS, Sullivan CE. Religious lifestyles and mental health: An exploratory study. Journal of Counseling Psychology. 1988;35(1):91–98. [Google Scholar]
- Bland RC, Newman SC, Orn H. Prevalence of psychiatric disorders in the elderly in Edmonton. Acta Psychiatrica Scandinavica Supplementum. 1998;77:57–63. doi: 10.1111/j.1600-0447.1988.tb08548.x. [DOI] [PubMed] [Google Scholar]
- Blazer D, Hughes DC, George LK. The epidemiology of depression in an elderly community population. The Gerontologist. 1987;27:2281–2287. doi: 10.1093/geront/27.3.281. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life. 3rd ed. Springer; New York: 2002. [Google Scholar]
- Boey KW. Religiosity and psychological well-being of older women in Hong Kong. International Journal of Psychiatric Nursing Research. 2003;8(2):921–935. [PubMed] [Google Scholar]
- Bosworth HB, Park K-S, McQuoid DR, Hays JC, Steffens DC. The impact of religious practice and religious coping on geriatric depression. International Journal of Geriatric Psychiatry. 2003;18:905–914. doi: 10.1002/gps.945. [DOI] [PubMed] [Google Scholar]
- Braam AW, Beekman ATF, Deeg DJH, Smit JH, van Tilburg W. Religiosity as a protective or prognostic factor of depression in later life; results from a community survey in The Netherlands. Acta Psychiatrica Scandinavica. 1997;96:199–205. doi: 10.1111/j.1600-0447.1997.tb10152.x. [DOI] [PubMed] [Google Scholar]
- Braam AW, Van den Eeden P, Prince MJ, Beekman ATF, Kivelaä SL, Lawlor BA, et al. Religion as a cross-cultural determinant of depression in elderly Europeans: Results from the EURODEP collaboration. Psychological Medicine. 2001;31(5):803–814. doi: 10.1017/s0033291701003956. [DOI] [PubMed] [Google Scholar]
- Breitner JC, Wyse BW, Anthony JC, Welsh-Bohmer KA, Steffens DC, Norton MC, et al. APOE-epsilon4 count predicts age when prevalence of AD increases, then declines: The Cache County Study. Neurology. 1999;53:321–331. doi: 10.1212/wnl.53.2.321. [DOI] [PubMed] [Google Scholar]
- Christensen C. Testimony bearing. In: Ludlow Daniel H., editor. Encyclopedia of Mormonism. Vol. 2. MacMillan; New York: 1992. pp. 1470–1471. [Google Scholar]
- Cnaan RA, Helzer AL. Women in congregations and social service provision: Findings from the Philadelphia census. Social Thought. 2004;23:25–43. [Google Scholar]
- Courtenay BC, Poon LW, Martin P, Clayton GM, Johnson MA. Religiosity and adaptation in the oldest-old. International Journal of Aging and Human Development. 1992;34:47–56. doi: 10.2190/N058-Y7X6-YLGJ-XBGE. [DOI] [PubMed] [Google Scholar]
- Cummings SM, Neff JA, Husaini BA. Functional impairment as a predictor of depressive symptomatology: The role of race, religiosity and social support. Health & Social Work. 2003;28:23–32. doi: 10.1093/hsw/28.1.23. [DOI] [PubMed] [Google Scholar]
- Duke JT. Latter-Day Saint social life: Social research on the LDS church and its members. BYU Religious Studies; Provo, UT: 1998. [Google Scholar]
- Eaton WW, Neufeld K, Chen LS, Cai G. Diagnostic Interview Schedule and schedules for clinical assessment in neuropsychiatry in the Baltimore epidemiologic catchment area follow-up. Archives of General Psychiatry. 2000;57:217–222. doi: 10.1001/archpsyc.57.3.217. [DOI] [PubMed] [Google Scholar]
- Forsell Y, Winblad B. Incidence of major depression in a very elderly population. International Journal of Geriatric Psychiatry. 1999;14:368–372. doi: 10.1002/(sici)1099-1166(199905)14:5<368::aid-gps919>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Friedhoff AJ. Consensus panel report. In: Schneider LS, Reynolds CF, Lebowitz BD, Friedhoff AJ, editors. Diagnosis and treatment of depression in late life: Results of the NIH Consensus Development Conference. American Psychiatric Press; Washington, DC: 1994. pp. 491–512. [Google Scholar]
- Gallo JJ, Rabins PV. Depression without sadness: Alternative presentations of depression in late life. American Family Physician. 1999;60:820–826. [PubMed] [Google Scholar]
- Ginsberg DL. Symposium monograph supplement. Depression in the elderly: The unique features related to diagnosis and treatment. CNS Spectrums. 2005;10:1–2. [Google Scholar]
- Heaton TB, Goodman KL, Holman TB. In search of a peculiar people: Are Mormon families really different? In: Cornwall M, Heaton TB, Young LA, editors. Contemporary Mormonism: Social science perspectives. University of Illinois Press; Urbana, IL: 1994. pp. 87–117. [Google Scholar]
- Helzer JE, Robins LN. The Diagnostic Interview Schedule: Its development, evolution, and use. Social Psychiatry and Psychiatric Epidemiology. 1988;23:6–16. doi: 10.1007/BF01788437. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Robins LN, McEvoy LT, Spitznagel EL, Stoltzman RK, Farmer A, et al. A comparison of clinical and Diagnostic Interview Schedule diagnoses: Physician reexamination of lay-interviewed cases in the general population. Archives of General Psychiatry. 1985;42:657–666. doi: 10.1001/archpsyc.1985.01790300019003. [DOI] [PubMed] [Google Scholar]
- Hoult TF. The sociology of religion. Holt, Rinehart & Winston; New York: 1958. [Google Scholar]
- Husaini BA, Blasi AJ, Miller O. Does public and private religiosity have a moderating effect on depression? A bi-racial study of elders in the American South. International Journal of Aging and Human Development. 1999;48:63–72. doi: 10.2190/F5MT-RTYH-7XR1-TFQU. [DOI] [PubMed] [Google Scholar]
- Idler EL, Kasl SV. Religion among disabled and nondisabled persons. I: Cross-sectional patterns in health practices, social activities, and well-being. Journal of Gerontology: Psychological Sciences. 1997;52B:P294–P305. doi: 10.1093/geronb/52b.6.s294. [DOI] [PubMed] [Google Scholar]
- Jolley M. Fast and testimony meeting. In: Ludlow Daniel H., editor. Encyclopedia of Mormonism. Vol. 2. MacMillan; New York: 1992. p. 502. [Google Scholar]
- Jorm AF. History of depression as a risk factor for dementia: An updated review. Australian and New Zealand Journal of Psychiatry. 2001;35:776–781. doi: 10.1046/j.1440-1614.2001.00967.x. [DOI] [PubMed] [Google Scholar]
- Judd DK. Religiosity, mental health, and the Latter-Day Saints: A preliminary review of literature (1923-1995) In: Duke JT, editor. Latter-Day Saint social life: Social research on the LDS church and its members. Brigham Young University, Religious Studies Center; Provo, UT: 1998. [Google Scholar]
- Judd DK. Religion, mental health and the Latter-Day Saints. Brigham Young University, Religious Studies Center; Provo, UT: 1999. [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ. Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Katrona CL. Depression in old age. Wiley; New York: 1994. [Google Scholar]
- Kessler RC, Foster C, Webster PS, House JS. The relationship between age and depressive symptoms in two national surveys. Psychology and Aging. 1992;7:119–126. doi: 10.1037//0882-7974.7.1.119. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Blazer DG, Sheikh JI. Psychopathology of later life. In: Birren JE, Sloane RB, editors. Handbook of mental health and aging. 2nd ed. Academic Press; San Diego, CA: 1992. pp. 379–599. [Google Scholar]
- Koenig HG. Religion and aging. Reviews in Clinical Gerontology. 1993;3(2):195–203. [Google Scholar]
- Koenig HG. Aging and God: Spiritual pathways to mental health in midlife and later years. Hawthorn Press; Binghamton, NY: 1994. [Google Scholar]
- Koenig HG, George LK, Peterson BL. Religiosity and remission of depression in medically ill older patients. American Journal of Psychiatry. 1998;15:536–542. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Pargament KI, Nielsen J. Religious coping and health status in medically ill hospitalized older adults. Journal of Nervous & Mental Disease. 1998;186:513–521. doi: 10.1097/00005053-199809000-00001. [DOI] [PubMed] [Google Scholar]
- Kral VA, Emery OB. Long-term follow-up of depressive pseudodementia of the aged. Canadian Journal of Psychiatry. 1989;34:445–446. doi: 10.1177/070674378903400515. [DOI] [PubMed] [Google Scholar]
- Manton KG, Stallard E, Tolley HD. Limits to human life expectancy: Evidence, prospects, and implications. Population and Development Review. 1991;17:603–637. [Google Scholar]
- Meller I, Fichter MM, Schroppel H. Incidence of depression in octo- and nonagenerians: Results of an epidemiological follow-up community study. European Archives of Psychiatry and Clinical Neuroscience. 1996;246:93–99. doi: 10.1007/BF02274899. [DOI] [PubMed] [Google Scholar]
- Merrill RM, Salazar RD. Relationship between church attendance and mental health among Mormons and non-Mormons in Utah. Mental Health, Religion and Culture. 2002;5:17–33. [Google Scholar]
- Mulsant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. Journal of Clinical Psychiatry. 1999;60:9–15. [PubMed] [Google Scholar]
- Murphy JM. Diagnostic schedules and rating scales in adult psychiatry. In: Tsuang MT, Tohen M, Zahner GR, editors. Textbook in psychiatric epidemiology. Wiley; New York: 1995. pp. 253–272. [Google Scholar]
- Murphy JM, Nierenberg AA, Laird NM, Monson RR, Sobol AM, Leighton AH. Incidence of major depression: Prediction from subthreshold categories in the Stirling County Study. Journal of Affective Disorders. 2002;68:251–259. doi: 10.1016/s0165-0327(00)00334-7. [DOI] [PubMed] [Google Scholar]
- Murray C, Michaud C, McKenna M, Marks JS. U.S. patterns of mortality by county and race: 1965-1994. Harvard Center for Population and Development Studies; Cambridge, MA: 1998. [Google Scholar]
- Newmann JP, Engel RJ, Jensen JE. Changes in depressive-symptom experiences among older women. Psychology and Aging. 1991;6:212–222. doi: 10.1037//0882-7974.6.2.212. [DOI] [PubMed] [Google Scholar]
- Norton MC. Cross-sectional concordance and longitudinal risk for depression in elderly married couples. Dissertation Abstracts International. 2001 December;62(5B):2495. [Google Scholar]
- Norton MC, Breitner JC, Welsh KA, Wyse BW. Characteristics of nonresponders in a community survey of the elderly. Journal of the American Geriatrics Society. 1994;42:1252–1256. doi: 10.1111/j.1532-5415.1994.tb06506.x. [DOI] [PubMed] [Google Scholar]
- Norton MC, Skoog I, Franklin LM, Corcoran C, Tschanz JT, Zandi PP, et al. Gender differences in the association between religious involvement and depression: The Cache County (Utah) study. Journal of Gerontology: Psychological Sciences. 2006;61B:P129–P136. doi: 10.1093/geronb/61.3.p129. [DOI] [PubMed] [Google Scholar]
- Norton MC, Skoog I, Toone L, Corcoran C, Tschanz JT, Lisota RD, et al. Three-year incidence of first-onset depressive illness in a population sample of older adults. The Cache County Study. American Journal of Geriatric Psychiatry. 2006;14:237–245. doi: 10.1097/01.JGP.0000196626.34881.42. [DOI] [PubMed] [Google Scholar]
- Palsson SP, Ostling S, Skoog I. The incidence of first-onset depression in a population followed from the age of 70 to 85. Psychological Medicine. 2001;31:1159–1168. doi: 10.1017/s0033291701004524. [DOI] [PubMed] [Google Scholar]
- Parker M, Roff LL, Klemmack DL, Koenig HG, Baker P, Allman RM. Religiosity and mental health in southern, community-dwelling older adults. Aging and Mental Health. 2003;7(5):390–397. doi: 10.1080/1360786031000150667. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Myers JK, Kramer M, Robins LN, et al. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: The Epidemiologic Catchment Area study. Acta Psychiatrica Scandinavica. 1993;88:35–47. doi: 10.1111/j.1600-0447.1993.tb03411.x. [DOI] [PubMed] [Google Scholar]
- Regier DA, Kaelber CT, Rae DS, Farmer ME, Knauper B, Kessler RC, et al. Limitations of diagnostic criteria and assessment instruments for mental disorders: Implications for research and policy. Archives of General Psychiatry. 1998;55:109–115. doi: 10.1001/archpsyc.55.2.109. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Rozzini R, Frisoni GB, Sabatini T, Trabucchi M. The association of depression and mortality in elderly persons. Journal of Gerontology: Medical Sciences. 2002;57A:M144–M145. doi: 10.1093/gerona/57.2.m144. [DOI] [PubMed] [Google Scholar]
- Sapp S. An alternative Christian view of aging. Consider aging from the perspective of the cross. Journal of Religion and Aging. 1987;4(1):1–13. [Google Scholar]
- Shear K, Roose SP, Lenze EJ, Alexopoulos GS. Depression in the elderly: The unique features related to diagnosis and treatment. CNS Spectrums. 2005;10:1–13. [Google Scholar]
- Sonnenberg CM, Beekman ATF, Deeg DJH, van Tilburg W. Sex differences in late-life depression. Acta Psychiatrica Scandinavica. 2000;101:286–292. [PubMed] [Google Scholar]
- Spendlove DC, West DW, Stanish WM. Risk factors and the prevalence of depression in Mormon women. Social Science Medicine. 1984;18:491–495. doi: 10.1016/0277-9536(84)90006-6. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Skoog I, Norton MC, Hart AD, Tschanz JT, Plassman BL, et al. Prevalence of depression and its treatment in an elderly population. The Cache County, Utah Study. Archives of General Psychiatry. 2000;57:601–607. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine. 2001;23(1):68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- Umberson D, Wortman CB, Kessler RC. Widowhood and depression: Explaining long-term gender differences in vulnerability. Journal of Health and Social Behavior. 1992;33(1):10–24. [PubMed] [Google Scholar]
- Van Exel E, Stek ML, Deeg DJH, Beekman AT. The implication of selection bias in clinical studies of late life depression: An empirical approach. International Journal of Geriatric Psychiatry. 2000;15:488–492. doi: 10.1002/1099-1166(200006)15:6<488::aid-gps149>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Van Ness PH, Larson DB. Religion, senescence, and mental health: The end of life is not the end of hope. American Journal of Geriatric Psychiatry. 2002;10:386–397. [PMC free article] [PubMed] [Google Scholar]


