Abstract
Equity is an important criterion in evaluating health system performance. Developing a framework for equitable and effective resource allocation for health depends upon knowledge of service providers and their location in relation to the population they should serve. The last available map of health service providers in Kenya was developed in 1959. We have built a health service provider database from a variety of traditional government and opportunistic non-government sources and positioned spatially these facilities using global positioning systems, hand-drawn maps, topographical maps and other sources. Of 6674 identified service providers 3355 (50%) were private sector, employer-provided or specialist facilities and only 39% were registered in the Kenyan Ministry of Health database during 2001. Of 3319 public service facilities supported by the Ministry of Health, missions, not-for-profit organizations and local authorities, 84% were registered on a Ministry of Health database and we were able to acquire co-ordinates for 92% of these. The ratio of public health services to population changed from 1:26,000 in 1959 to 1:9,300 in 1999-2002.
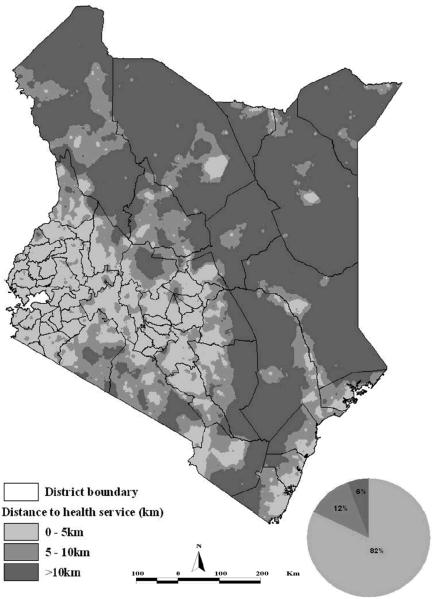
There were 82% of the population within 5km of a public health facility and resident in 20% of the country. Our efforts to recreate a comprehensive, spatially defined list of health service providers has identified a number of weaknesses in existing national health management information systems which with an increased commitment and minimal costs can be redressed. This will enable geographic information systems to exploit more fully facility-based morbidity data, population distribution and health access models to target resources and monitor the ability of health sector reforms to achieve equity in service provision.
Keywords: health management information systems, geographic information systems, health reform, health resource allocation, equity, access, health services, Kenya
1 Introduction
There has been a resurgence of interest in the geographic inequalities in health among countries of Western Europe and North America linked to atlases of risk and analyses of the economic, social, service and environmental causes for disparities in health outcomes (Macintyre et al., 1986; Kunst and Mackenbach, 1994; Bartley et al., 1997; Kennedy et al., 1998; Gilson, 1998; Braveman and Tarimo, 2002). By contrast, our understanding of spatial determinants of risk, health and access to services in the low-income tropics is limited.
While high-income countries are able to fund and integrate new information tools to guide national health policy, low-income countries who bear the majority of the global burden of disease, have inadequate and poorly performing health management information systems (HMIS). Many countries in sub-Saharan Africa (SSA) have embraced the need to develop broad health sector reforms linked to poverty reduction strategies (Owino, 1997; Bossert, 1998; Agyepong, 1999). Targets are established by national governments to reach specific goals of mortality reduction through equitable access to services. The strategies adopted to achieve these goals should be based upon knowledge of existing services, disease burden and equity. In practice, the extent to which the evidence-base for these decisions can be developed is often limited (Murray, 1995; Owino and Munga, 1997; WHO, 2000; Niessen et al., 2000).
Geographical information systems (GIS), with their capacity for spatial data input, data storage, multi-factor analysis and output have been identified as an important tool in setting public health agendas and understanding the levels of inequalities in access to health care (Twigg, 1990; Scholten and Lepper, 1991; Fotheringham and Rogerson, 1994; Loslier, 1995; Snow et al., 1998; Hay et al., 2000; Higgs and Gould, 2001). In this paper, we describe efforts to reconstruct the national map of health service providers in Kenya using all available information. We use this to highlight the current HMIS problems facing Kenya and similar countries in the region. We also explore how these might be resolved through coordinated efforts using GIS applications. We demonstrate the simple use of GIS data to highlight disparity in physical access to health service.
2 Methodology
The Kenya Context
Since independence in Kenya (1963) continuous attempts have been made to create an equitable health care system. It was clear that access to formal health services was a major problem to the bulk of the population, 95% of who were listed as rural in the 1962 census (Mburu, 1980). Despite declining economic growth, high population growth rates and an increasingly overwhelmed and under-resourced health system, Kenya was able to realise precipitous and sustained declines in infant and child mortality between 1960 and the early 1990s (Mburu, 1980; Owino, 1997). In 1994 the Government of Kenya (GoK) launched its proposal for health sector reform placing greater emphasis upon decentralized priority setting and equitable allocation of resources (MoH, 1994). The health sector reform required a combined epidemiological and micro-economic framework to develop standard geographic criteria for resource allocation (MoH, 1994).
Kenya's formal public clinical services are structured at three administrative levels: central headquarters, provincial and district levels in a hierarchical system. Clinical services are provided by a number of partners including the GoK, missions, non-governmental organizations (NGOs), local authorities (LA) and the private-for-profit (MoH, 1994; GoK, 1998; MoH, 2002). Clinical facilities at district-levels are organized according to the types of services they provide. From the most common least complex, to the larger and more complex clinical facilities are dispensaries networked to sub-health centres and health centres through to rural health training centres, sub-district hospitals and district hospitals. Provincial general hospitals and the Kenyatta National Hospital provide the major secondary and tertiary referral levels for the government health services. While all service types provide out-patient clinical services only the dispensaries and sub-health centres do not provide in-patient services. In addition, both at district and provincial levels, specialist hospitals, for example, for tuberculosis or leprosy, and maternity homes provide additional support. In reality there are difficulties distinguishing between middle levels of the service (dispensaries vs. clinics, sub-health centres vs. health centres and rural health training centres vs. sub-district hospitals) owing to decisions made by district health management teams (DHMTs) to provide staffing based upon patient loads rather than infrastructure criteria.
Developing a national clinical service provider list
We anticipated a single, definitive list of all service providers nationwide held centrally by the Ministry of Health (MoH). Four principal lists existed, however, created at different times over the last six years. These included a list held by the MoH-HMIS division (last updated in April 2001), an independent list created by the Family Planning and Logistics Management (FPLM) program supporting the supply of commodities for the Ministry of Health's Division of Reproductive Health (developed in October 1998), the Kenyan Government's Gazette (KG) notice of officially recognized health service providers posted in August 1998 and the Kenya Service Providers Assessment (KSPA) report which was conducted in 1999 by the MoH and the National Council for Population and Development. Careful matching of these lists for names and district location revealed considerable differences in their coverage and completeness, particularly with respect to the private sector providers.
By retaining the original HMIS codes we reconstructed a unique listing of health facilities including facilities found on the other key lists but not the HMIS list. This list was then updated through a number of different information sources and correspondence. First, the Central Bureau of Statistics of the Ministry of Finance and Planning were contacted to source District Development Plans for 57 districts. These often provided hand-drawn maps and lists of facilities located in each district (52 districts). Second, we obtained additional non-GoK lists of service providers from the Christian Health Association of Kenya (CHAK) developed in September 2000, who provide umbrella support to the mission health sector in Kenya. Likewise the Kenya Medical Association provided the Kenya Medical Directory (KMD) 2000 edition, which contained a list and addresses of their national members practicing care within the public and private sectors. Telephone directories were checked for each of the eight provinces to identify listed private practitioners. NGOs and research organizations were contacted to provide any annual reports or publications which might contain health facility lists and maps. Data on facility name, district, address and telephone numbers were listed in an MS Excel 2000 spreadsheet. Lists of health facilities run by MoH, mission, NGO and LA were abstracted from the main data and used as provisional lists that were checked in April 2003 by Provincial Health Information Officers to identify omissions, duplications and correct facility status. The Coastal and North Eastern provinces were consulted more extensively during 2002.
Developing spatial coordinates for health service providers
A number of methods were used to provide a longitude and latitude for each health service provider identified during the process described above. These included the use of global positioning systems (GPS) by various NGO and research groups (including ours); extraction and triangulation of coordinates from hand-drawn maps against GIS data on administrative boundaries and roads through a process of on- screen digitizing using Arcview GIS (Version 3.2); the use of 1:50,000 topographical maps; matching names of facilities to digital databases of village names and market centres created in 2001 by the International Livestock Research Institute, Kenya; and finally matching facility names to fifth-level administrative boundary units where these units were small by extracting a centroid position.
Handheld GPS units used from 01 May 2000, when selective availability was removed, to position facilities as part of specialized survey work will have had an estimated mean accuracy of +/− 15 m (http://www.garmin.com, http://www.trimble.com). We have regarded our GPS co-ordinates as the ‘gold-standard’. While we have ensured that there are no gross errors in our readings, we did not perform differential corrections of the GPS results. One hundred and thirty seven on-screen digitized coordinates from hand-drawn maps and 125 extracted from grid references on 1:50,000 were subsequently or coincidentally positioned with a GPS unit. To examine the error margins in extracting data from either on-screen digitizing of hand-drawn maps or from 1:50,000 maps we used a Root-Mean Square Error (RMSE) analysis.
Population distributions map for health care planning
The most recent MoH's Resource Allocation Criteria (MoH- RAC) document, which advises on methods of resource allocation, includes as one of its criteria the distribution and characteristics of the population (MoH, Personal Communication) including the total population in the district, population under five years, females between 15-44 years, poverty and prevalence of diseases (HIV/AIDS, malaria, respiratory infections and communicable diseases). The latest Kenya population and housing census was undertaken in 1999 (CBS, 2001). The highest spatial resolution data readily accessible in the public domain were at the sub-location, fifth-level administrative unit (circa 4250 people). The sub-location population data were entered in MS Excel 2000 and sub-location maps were digitized by the Central Bureau of Statistics using ArcInfo (Version 3.5) (minimum area and population 0.059 sq. km and 46 people, maximum is 5022 sq. km and 108, 234 people). This national sub-location digital map and attribute population data were exported and linked into ArcView GIS (Version 3.2).
Access to health facilities
Using ArcView GIS (Version3.2), Euclidean distances (in kilometers) between centroid of each sub-location and the nearest public health facility were computed. We divided the sub-locations into three distance categories to public health facilities-within 5km, 10km and >10km distances. We interpolated the distance at each sub-location and created a national map of physical access to public health facilities.
3 Results
Following 2 years of compiling various facility lists and checking on completeness, duplications and positions, the final database contained a total of 6674 health service providers (Table 1). We did not include mobile clinics, community pharmacies or village health posts, which represent a dynamic and transient grouping of lowest level providers subject to NGO or DHMT resources and support. The list did attempt to include private sector providers, a large grouping of health facilities widely used by the community but difficult to regulate by the MoH. Two thousand nine hundred and fifty one private sector facilities were identified, representing 45% of all service providers. These were identified principally through the KMD (20%), the FPLM list (19%) and telephone directories (17%) and only 38% were found on the MoH-HMIS list. Among four districts studied intensively for health service providers (Noor et al., 2003), 50% of private sector providers were not recorded on any official list and identified only through district-level investigation.
Table 1. 6674 identified health facilities in Kenya by type and service providera (Shaded facilities used in Figure 2 and Tables 2 & 3).
| MoH | Mission/NGO | Local Authority |
Employers and other ministries |
Private | Total | |
|---|---|---|---|---|---|---|
| Hospitalsb | 125 | 96 | 11 | 107 | 339 | |
| Health centresc | 473 | 157 | 50 | 24 | 26 | 730 |
| Dispensaries | 1471 | 907 | 40 | 252 | 289 | 2958 |
| Unspecified clinicsd | 45 | 2179 | 2225 | |||
| Specialist facilitiese | 8 | 54 | 5 | 5 | 350 | 422 |
|
| ||||||
| Total |
2077 (31.1%) |
1214 (18.2%) |
95 (1.4%) |
337 (5.1%) |
2951 (44.2%) |
6674 |
A total of 41 facilities were identified on the national HMIS list but could not be identified according to service provider and/or facility-type.
Includes provincial, district, sub-district hospitals or unspecified private hospitals offering general in-patient clinical services.
Includes all health centres, sub-health centres and rural health training centres as specified on national databases.
Includes all clinics that were not classified in the private or employer sectors that provide generalized health services but were not classed as dispensaries or health centres.
Includes all hospitals that provide treatment for only special diseases such as leprosy, tuberculosis, cancer, ophthalmology, spinal injury etc and the large number of maternity and nursing homes.
In the following descriptive analysis of the completeness and coverage of facility locations we have focused on formal health facilities that provide in- and out-patient clinical services to the general public and are run by the MoH, missions, NGOs or local authorities. We have excluded specialist services such as maternity and nursing homes, ophthalmic centres, tuberculosis, oncology and other specialist investigation centres. Furthermore, we have excluded 337 service providers located among the industrial, agricultural and education sectors, and those run by or on behalf of the armed, prison and other Government services. These services are provided to targeted employed populations and their immediate families and not accessible to the general public. The final public sector general clinical service provider list contained 2069 facilities run by the MoH, 1160 mission/NGO facilities and 90 LA services (Table 1).
The HMIS list of facilities, which was the primary MoH list that we used as the basis on which we built the comprehensive national database of facilities, contained 2774 health facilities of which 1812 were run by the MoH, 873 by Mission/NGO and 89 by LAs (Table 2). The other lists that we used to update the HMIS database contained varied numbers of facilities in the decreasing order of FPLM (2244), KG (2183), KSPA survey list (1602), telephone directories (294), KMD (165), Division of Primary Health Care list (218) and the mission sector lists from CHAK (212). As mentioned earlier most of the facilities not in the MoH-HMIS were private facilities (1838). However, 257 MoH, mission/NGO and LA facilities were also not on this list.
Table 2. Number of general public health facilities in each nationally available public domain list by service provider.
| Number of facilities |
||||||||
|---|---|---|---|---|---|---|---|---|
| Agency | HMIS | FPLM | KG | KSPA | TD | KMD | DPHC | CHAK |
| MoH | 1812 | 1575 | 1538 | 1140 | 232 | 79 | 136 | |
| Mission/NGO | 873 | 611 | 576 | 406 | 61 | 50 | 81 | 212 |
| Local Authority |
89 | 58 | 69 | 56 | 1 | 36 | 1 | |
|
| ||||||||
| Total | 2774 | 2244 | 2183 | 1602 | 294 | 165 | 218 | 212 |
HMIS = Health Management Information Systems (2001); FPLM = Family Planning and Logistics Management (1998); KG = Kenya Gazette (1998) ; KSPA =Kenya Service Provision Assessment (1999); TD= Telephone Directory (2002); KMD= Kenya Medical Directory (2000); DPHC= Division of Primary Health Care (2002); CHAK= Christian Health Association of Kenya (2000).
Special surveys by donors, NGOs or research groups in selected districts provided an opportunity to examine the likelihood that the centrally available listings of service providers would not identify a service provider at the district level. We have focused on five districts (Kilifi, Kwale, Makeuni, Kisii/Gucha, and Bondo) that formed part of detailed GIS studies between 2000 and 2002 (Noor et al., 2003; KEMRI-Kilifi-unpublished data). Among these districts a total of 25 out of 274 MoH, Mission/NGO and LA facilities were identified in collaboration with district health management teams that were not on centrally-held lists and databases, representing an average of 5 facilities per district that were not on any published list.
It was possible, through a combination of approaches, to position spatially 1993 (96%) of the MoH, 979 (81%) of the Mission/NGO and 80 (84%) of the LA service providers (Table 3). The majority of the combined facility positions (46%) were identified through the use of on-screen digitizing from hand drawn maps provided by various partners and MoH initiatives. Additional locations were positioned directly using GPS coordinates (23%), 14.5% from 1:50,000 maps, 10% from International Livestock Research Institute (ILRI) village databases and 6.5% from centroid positions of small sub-location areas (Table 3). Overall 8% (267) of general clinical service providers within the Government, mission or NGO sectors could not be positioned by any approach available outside of direct consultation with district health management teams.
Table 3. Numbers (%) of facilities spatially positioned using different methods.
| Source of co-ordinates |
|||||||
|---|---|---|---|---|---|---|---|
| Agency | GPS | 1:50000 maps |
Hand drawn maps |
Village digital database |
Centroids of sublocations |
Not positioned |
Total |
| MoH | 503 | 342 | 1012 | 42 | 94 | 76 | 2069 |
| Mission/NGO | 140 | 99 | 396 | 252 | 92 | 181 | 1160 |
| Local Authority |
50 | 2 | 10 | 6 | 12 | 10 | 90 |
|
| |||||||
| Total |
693 (21%) |
443 (13%) |
1418 (43%) |
300 (9%) |
198 (6%) |
267 (8%) |
3319 |
Coincidental GPS versus on-screen digitizing or 1:50,000 topographic map referencing was available for 262 MoH, Mission/NGO, LA or private facilities, largely from 29 intensively studied districts. The accuracies of the various non-GPS approaches to positioning facilities were examined revealing accuracy values of about 1.9 km for on-screen digitizing (n = 137) and 1.4 km for 1:50,000 topographic maps (n= 125). Overall 31% of on-screen digitizing coordinates were within 1 km of GPS readings and 70% were within 1 km of 1:50,000 map references (Table 4).
Table 4. Accuracy assessment of on-screen digitizing from hand-drawn maps and use of 1:50,000 topographical maps against GPS positioning.
| Method | No. of facilities (n) | Σ(r)= Σ√(x2 + y2) | RMSE= √[ Σ(r) /n] |
|---|---|---|---|
| 1: 50000 | 125 | 240.4914 | 1.387058 |
| On-Screen digitizing (OSD) | 137 | 478.2284 | 1.868346 |
Footnote: The difference in longitude (X) and latitude (Y) for each point was computed from each pair of coordinates of a point by treating the GPS coordinates as the known and the on-screen digitized and 1:50000 coordinates as the observed. The shift at each point was then computed as the square root of the sum of the square of X and Y. This shift was considered to be the difference between the known and observed position of the point. The RMSE was then computed by RMSE=√ [Σ√(x2 + y2)/n]. Where n= is the number of points positioned through on-screen digitizing or from the topographic maps.
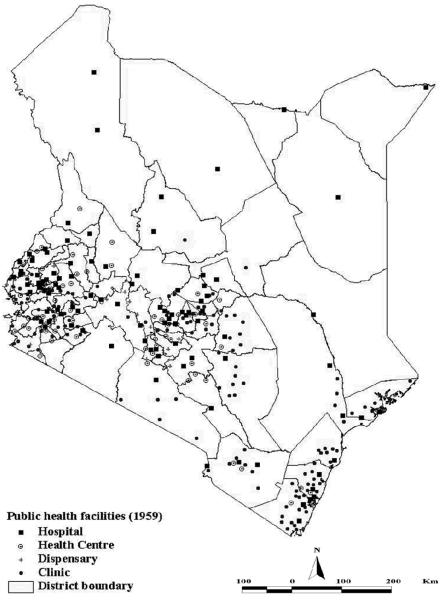
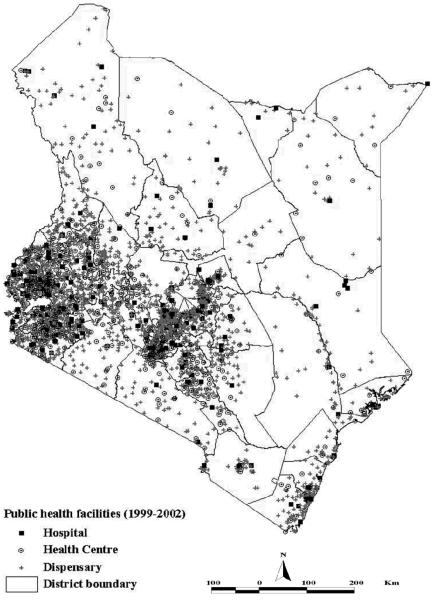
Figure 1 shows 308 public clinical services run by the MoH, mission/NGO or local authorities which we extracted digitally from the last known map of service providers developed in 1959 (Butler, 1959), at a time when Kenya's population was estimated to be 8 million (World Population Prospects, http://esa.un.org/unpp). Figure 2 shows the distribution of the current 3052 (92%) of the public clinical service providers that we were able to position. Figure 3 is a sub-location population distribution map based on the 1999 Kenya census. Overall the formal clinical service-to-population ratio in 1959 was approximately 1:26,000 compared to the 3319 general clinical services provided by the MoH, mission, NGO and LA to approximately 29 million people in 1999-2002 (1:9,300).
Figure 1.
A map of Kenya showing the distribution of health facilities in 1959. This map was digitized from Butler's map in the Atlas of Kenya, 1959'(Butler, 1959). The map shows a total of 308 health facilities (89 MoH and Mission hospitals; 114 MoH, Mission and LA dispensaries; and 105 LA health centres.
Figure 2.
A district map of Kenya showing the distribution of 3052 public health service facilities (hospitals, health centres and dispensaries) supported by the MoH (1993), Missions or NGOs (979) and LA (80) as identified as operational between 1999 and 2002 (Table 1).
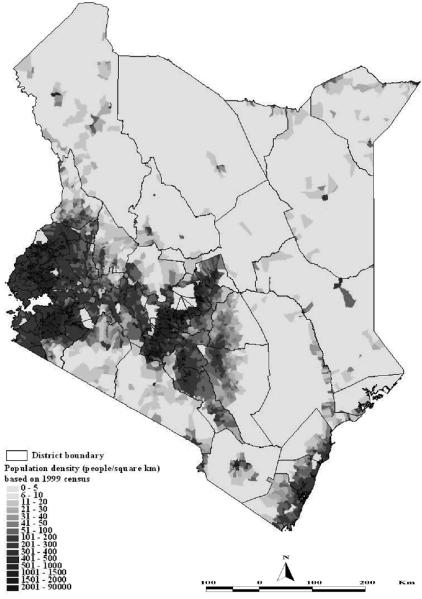
Figure 3.
A sub-location level population distribution map of Kenya based on the 1999 census of circa 29 million people (CBS, 2001).
Figure 4 is a map of population's distance to public health facilities based on those that we positioned. The 267 health facilities that we were unable to position are not represented in this figure. Eighty-two percent of the populations live within 5km of a public health facility. Twelve percent are between 5-10km and the remaining six percent live at > 10km to a health facility. While most of the people live within 5km of a health facility, they occupy only 20% of the country's land surface.
Figure 4.
A Kenya district map and pie chart of population within 5, 10 and >10km of a public health facility providing out-patient clinical services. Pie chart represents the proportions of the population residing in each of the three distance categories (shaded as per map figure).
4 Discussion
The last available map of health service providers in Kenya was developed in 1959 (Butler, 1959; Figure 3). Forty years on we have attempted to reconstruct the national health facility map. We have identified 3319 general health service providers supported by the MoH or their mission, NGO or LA partners providing services to 29 million people in 1999. Since 1959, the services-to-population ratio changed from 1:26,000 people to 1:9,300 people in 1999. At an initial glance (figures 2 and 3) the location of these services appears coincidental with the distributions of population. While most of the population lives within five kilometers of a public health facility, there are still inter- and intra- district disparities (figure 4). This is most notable in the semi-arid areas of north and north-east of Kenya with the largest proportion of population residing outside the five-kilometre zone. This figure does not represent the 267 facilities that were not positioned. Although there are discrepancies between Euclidean distances and the actual routes used by people to get to health facilities, nonetheless, this example demonstrates the potential of GIS in health planning. More detailed approaches to examining physical access to health services based on transport network, topography and land-use will be presented elsewhere (Noor et al., in preparation).
We began this exercise under an assumption that a single definitive list of clinical service providers would be available within the MoH and were surprised by the early realisation that more than one list was available, there was a lack of correspondence between the lists and they did not contain all the facilities that were likely to be present at the district-level. It is possible that Kenya's HMIS system is unique but we suspect that it is broadly similar to many countries of the region. In Kenya, the most comprehensive list of all clinical service providers was produced by the MoH-HMIS. Despite these being updated as recently as 3 years ago and capturing most of the public health facilities, it still did not contain the names of 257 (12%) MoH health facilities. In addition, it did not contain 288 (23%) of the facilities of the clinical services provided by the mission, NGO and LA sectors. More detailed district-level surveys of five districts revealed approximately 9% of all the health facilities supported by the MoH, Mission/NGO and LA sectors that were not identified on any nationally available listings. The least well represented on national databases were the private sector, the majority of which were identified through unofficial listings such as telephone directories and the KMD. The Private sector is hard to regulate and track at the peripheral, district-levels of the health sector. During more detailed investigations of five districts we identified 117 (50%) private sector providers not registered on official or unofficial lists held centrally. The existence of some of these facilities was not even known by the local DHMTs and is indicative of how unregulated this sector remains.
The location of facilities in relation to population, other services and poverty or disease vulnerability underpins all efforts to achieve an equitable health service reform. We were able to position spatially 92% of the general health service providers from the MoH, mission, NGO and LA sectors using a variety of techniques. Allowing for a degree of inaccuracy (Table 4), the 1:50,000 topographic and hand-drawn maps can be used to develop spatial platforms. Ideally, GPS coordinates would provide the gold-standard for positioning service providers. Developing high-resolution district-level spatial maps is expensive. We estimate that a two-week GPS level exercise in a medium sized district in Kenya, including transportation and field assistance, costs approximately US $3,000. Nationally, this would cost US $200,000. We argue that this is a small price to pay to establish a comprehensive (including private sector) national GIS database.
Without a nationally accurate spatial infrastructure of health service providers, health sector planning and monitoring is limited in a number of important ways. In the absence of an updated and comprehensive listing of service providers, MoHs are limited in their ability to reliably define drug and clinical commodity needs, staffing levels, interpret the geographic coverage of disease burdens reported by facilities or target information packages on new drug regimens or national recommendations for case-management or disease prevention. All the parameters proposed by the Kenyan MoH to guide resource allocation depend largely on a robust HMIS with a high reporting rate that incorporates the relevant ancillary data. For instance, the latest HMIS report 1996-99, published in 2001, presents details of out-patient and in-patient statistics, immunization coverage, health facilities distribution and workload service statistics which form the basis of the MoH and donors budgetary allocations for health care. Further, the report gives a health facility reporting rate of between 6-59%. However, the number of health facilities in the HMIS database, which is the key denominator for the reporting rates, is 84% percent of all facilities, implying that the reporting rate is much lower than indicated, resulting in overestimation of health service coverage and underestimation of disease rates, workload statistics and resource needs. In the presence of such low reporting rates and clear deficiencies in Kenya's HMIS, it is impossible to correctly determine the parameters for resource allocation.
Health care provision has a supply side represented by the health service centres and a demand side represented by the target population. Therefore, to produce an evidence base for decision-making, information on the nature and distribution of services in relation to population needs and methodologies of linking the two is imperative. The potential of GIS to link the demand and supply sides of health care has led to its emergence as an important tool in equitable health resource allocation in many parts of the world (Twigg 1990; Scholten and Lepper, 1991; Fotheringham and Rogerson, 1994; Loslier, 1995; Snow et al., 1998; Hay et al., 2000; Higgs and Gould, 2001). This has come with new sets of challenges to health information systems (Gatrell and Loytonen, 1998; Boelaert et al., 1998; Gatrell and Senior, 1999) particularly in areas of the world where traditional HMIS are weak. For a health GIS to function to full capacity, the health and population data contained in traditional relational databases must be assigned to a definite spatial position.
To address the above challenges, many high-income countries have established accessible national and regional GIS resources (UK Association for Geographic Information, US TIGER and National Spatial Data Infrastructure, the EC INSPIRE-Infrastructure for Spatial Information in Europe) which have provided a solid foundation on which many uses of GIS in public health are based. In most low-income countries, particularly those of the African continent, there is an urgent need to build such an infrastructure (Rockefeller Foundation, 2002). Currently, relatively few applications of GIS for public health exist in sub-Saharan Africa (Zwarenstein et al., 1991; Tanser, 1999; Booman et al., 2000; WHO, 2003). For the most part, these applications have been specific small area studies not built within a national HMIS framework.
In an effort to reduce the technology gap, the World Health Organisation's public health mapping group developed HealthMapper, a free, easy to use GIS software proposed as a standard tool for developing countries (WHO, 2002). However, in the absence of organised and accurate spatial health information, full utility of this software cannot be realised. This requires a concerted effort among all national stakeholders under the leadership of ministries of health. As we have demonstrated this will not be an easy task but the production and utilisation of a comprehensive, spatially defined infrastructure of health service providers linked to vulnerability (disease or economic), we believe, is both possible and fundamental to any health sector reform process.
Acknowledgments
This study received financial support from The Wellcome Trust, UK (#058922), Roll Back Malaria Initiative, AFRO (AFRO/WHO/RBM # AF/ICP/CPC/400/XA/00) and the Kenya Medical Research Institute. SIH is currently supported by the Wellcome Trust as a Research Career Development Fellow (#069045) and RWS is supported by the Wellcome Trust as Senior Fellow (#058992). The authors are grateful to a large number of contributors to the location and checking of information used to create the National Health Service GIS database described in this paper, these include: Henri Van Den Homberg and Mark Ayalo (GTZ), Michael Hansen (DANIDA), Al Henn and Linda Archer (AMKENI project), Francis Echessa (CHAK), Dr John Gimnig (CDC-KEMRI), Helen Guyatt, Lydiah Mwangi, Lucy Muhonyo, Abdinassir Amin & Judy Omumbo (Oxford-KEMRI), Kipruto Chesang (Provincial Medical Office, Rift Valley), Sammy Kagoiyo (Provincial Medical Office, Central), Pepela Wanjala (Provincial Medical Office, Nyanza), Peter Wainaina (District Medical Office, Nakuru), Jonathan Mutinda (District Medical Office, Kericho), Mutile Wanyee (District Medical Office, Kiambu), Dominic Mutua (HMIS, MoH), Gordon Wayumba (University of Nairobi), Julius Munyao (Family Health International), Bill Powell (University of North Carolina), the DHMTs and the several other health officers who helped during district visits and through correspondence. We also wish to express our gratitude to Dr Sam Ochola (DOMC, Ministry for Health) and Mr David Nalo (Central Bureau of Statistics, Ministry for Finance & Planning) for their continued support for this project. We are also grateful to Peter Atkinson and Mike English for their comments on the manuscript. This paper is published with the permission of the director KEMRI.
References
- Agyepong AI. Reforming health service delivery at district level in Ghana: The perspective of a District Medical Officer. Health Policy Plann. 1999;14:59–69. doi: 10.1093/heapol/14.1.59. [DOI] [PubMed] [Google Scholar]
- Butler RJ. Atlas of Kenya: A comprehensive series of new and authenticated maps prepared from the national survey and other government sources with gazetteer and notes on pronunciation and spelling. The Survey of Kenya; Nairobi, Kenya: 1959. [Google Scholar]
- Bartley M, Blane D, Montgomery S. Health and the life course: Why safety nets matter. Brit. Med. J. 1997;314:1194–1196. doi: 10.1136/bmj.314.7088.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelaert M, Arbyn M, Van der Stuyft P. Geographical Information Systems (GIS), gimmick or tool for health district management. Trop. Med. Int. Health. 1998;3:163–165. doi: 10.1046/j.1365-3156.1998.00221.x. [DOI] [PubMed] [Google Scholar]
- Booman M, Dave ND, La Grange K, Martin C, Mabuza FM, Zitha A, Fraser C, Sharp BL. Using geographic information systems to plan a malaria control programme in South Africa. B. World Health Organ. 2000;78:1438–1444. [PMC free article] [PubMed] [Google Scholar]
- Bossert T. Analyzing the decentralization of health systems in developing countries: Decision space, innovation and performance. Soc. Sci. Med. 1998;47:1513–1527. doi: 10.1016/s0277-9536(98)00234-2. [DOI] [PubMed] [Google Scholar]
- Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc. Sci. Med. 2002;54:1621–1635. doi: 10.1016/s0277-9536(01)00331-8. [DOI] [PubMed] [Google Scholar]
- Central Bureau of Statistics . 1999 population and housing census: counting our people for development. Volume 1: Population distribution by administrative areas and urban centres. Central Bureau of Statistics, Ministry of Finance & Planning, GoK; Jan, 2001. p. 415. 2001. [Google Scholar]
- Fotheringham S, Rogerson P. Spatial Analysis & GIS. Taylor & Francis Ltd.; 1994. 1994. [Google Scholar]
- Gatrell A, Senior M. Health and health care applications. In: Longley PA, Maguire DJ, Goodchild MF, Rhind DW, editors. Geographical Information Systems Volume 2: Management Issues and Applications. John Wiley & Sons; New York, NY: 1999. pp. 925–938. [Google Scholar]
- Gatrell AC, Markku L. In: GIS and Health. Gatrell Anthony C., Loytonen Markku., editors. Taylor and Francis; London: 1998. pp. 3–16. [Google Scholar]
- Government of Kenya (GoK) The Kenya Gazette. The Government Printers; 1998. [Google Scholar]
- Gilson L. In defense and pursuit of equity. Soc. Sci. Med. 1998;47:1891–1896. doi: 10.1016/s0277-9536(98)00217-2. [DOI] [PubMed] [Google Scholar]
- Hay SI. An overview of remote sensing and geodesy for epidemiology and public health application. Adv. Parasit. 2000;47:1–35. doi: 10.1016/s0065-308x(00)47005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay SI, Omumbo JA, Craig MH, Snow RW. Earth observation, geographic information systems and Plasmodium Falciparum Malaria in Sub-Saharan Africa. Adv.Parasit. 2000;47:174–206. doi: 10.1016/s0065-308x(00)47009-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgs G, Gould M. Is there a role for GIS in the ‘new NHS’? Health Place. 2001;7:247–259. doi: 10.1016/s1353-8292(01)00014-4. [DOI] [PubMed] [Google Scholar]
- Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: Multilevel analysis. Brit. Med. J. 1998;317:917–921. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunst AE, Mackenbach JP. The size of mortality differences associated with educational level in nine industrialized countries. Am. J. Public Health. 1994;84:932–937. doi: 10.2105/ajph.84.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loslier L. In: Don de Savigny, Wijeyaratne P., editors. GIS for Health and the Environment; Proceedings of an international workshop held in Colombo, Sri Lanka; 5-10, September 1994; IDRC; 1995. 1994. [Google Scholar]
- Macintyre S. The patterning of health by social position in contemporary Britain: Directions for sociological research. Soc. Sci. Med. 1986;23:393–415. doi: 10.1016/0277-9536(86)90082-1. [DOI] [PubMed] [Google Scholar]
- Mburu FM. Health Development in Kenya, 1964-1978: Issues of relevance and priority. Department of Community Health, University of Nairobi; 1980. [Google Scholar]
- Ministry of Health (MoH) Health Policy Framework. Government of Kenya; 1994. reprinted 1997. [Google Scholar]
- Ministry of Health (MoH) Guidelines for the District Health Management Boards & Health Centre Management Committees. Government of Kenya; 2002. [Google Scholar]
- Murray CJ. Toward an analytical approach to health sector reform. Health Policy. 1995;32:93–109. doi: 10.1016/0168-8510(95)00729-c. [DOI] [PubMed] [Google Scholar]
- Niessen LW, Grisjeels EWM, Rutten FFH. The evidence-based approach in health policy and health care delivery. Soc. Sci. Med. 2000;51:859–869. doi: 10.1016/s0277-9536(00)00066-6. [DOI] [PubMed] [Google Scholar]
- Noor AM, Zurovac D, Hay SI, Ochola SA, Snow RW. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Trop. Med. Int. Health. 2003;8:917–926. doi: 10.1046/j.1365-3156.2003.01112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omumbo JA, Hay SI, Goetz SJ, Snow RW, Rogers DJ. Updating historical maps of malaria transmission intensity in East Africa using remote sensing. Photogramm. Eng. Rem. S. 2002;68:161–166. [PMC free article] [PubMed] [Google Scholar]
- Owino W, Munga S. Decentralization of financial management systems: Its implementation and impact on Kenya health care delivery. Institute of Analysis and Research; Nairobi: 1997. pp. 1–42. DP No. 006/1997. [Google Scholar]
- Owino W. Delivery and financing of health care services in Kenya: Critical issues and research gaps. Institute of Analysis and Research; Nairobi: 1997. p. 27. DP No. 002/1997. [Google Scholar]
- Rockefeller Foundation . Geographic Information Systems & Health in East Africa: Applications for Integrated Disease Surveillance. Rockefeller Foundation, Health Equity Theme; New York: 2002. pp. 1–94. [Google Scholar]
- Scholten HJ, de Lepper MJC. The benefits of the application of geographical information systems in public and environmental health. World Health Quarterly. 1991;44:160–169. [PubMed] [Google Scholar]
- Snow RW, Gouws E, Omumbo J, Rapuoda B, Craig MH, Tanser FC, le Sueur D, Ouma J. Models to predict the intensity of Plasmodium falciparum transmission: applications to the burden of disease in Kenya. T. Roy. Soc. Trop. Med. H. 1998;92:601–606. doi: 10.1016/s0035-9203(98)90781-7. [DOI] [PubMed] [Google Scholar]
- Tanser FC. The application of geographical information systems to infectious diseases and health systems in Africa. Faculty of Medicine, University of Natal; 2000. Phd Thesis. [Google Scholar]
- Twigg L. Health based geographical information systems: Their potential in the light of existing data sources. Soc. Sci. Med. 1990;30:143–155. doi: 10.1016/0277-9536(90)90337-r. [DOI] [PubMed] [Google Scholar]
- W.H.O. Health Systems: Improving Health Performance. World Health Organization; Geneva: 2000. pp. 1–206. [Google Scholar]
- W.H.O. The HealthMapper: Integrated Information and Mapping system for Public Health. 2002. http://bbs.wpro.who.int/components3.htm.
- W.H.O. Success in Africa: The Onchocerciasis Control Programme in West Africa, 1974-2002. World Health Organization; Geneva: 2003. pp. 1–79. [Google Scholar]
- Zwarenstein M, Krige D, Wolf B. The use of a geographical information system for hospital catchment area research in Natal/KwaZulu. S. Afr. Med. J. 1991;80:497–500. [PubMed] [Google Scholar]