Abstract
Background
Enhancements to current dietary advice to prevent chronic disease are of great clinical and public health importance. The OmniHeart Trial compared 3 diets designed to reduce cardiovascular disease (CVD) risk—one high in carbohydrate and 2 that replaced carbohydrate with either unsaturated fat or protein. The lower carbohydrate diets improved the CVD risk factors. Several popular diets claiming health benefits emphasize carbohydrate, fat, or protein or various combined approaches.
Objective
The objective of this study was to compare the macronutrient contents of the OmniHeart trial diets to those of several popular diets and to evaluate each diet for consistency with national health guidelines.
Design
The macronutrient contents of 7-d menu plans from the OmniHeart Study, Dietary Approaches to Stop Hypertension (DASH), Zone, Atkins, Mediterranean, South Beach, and Ornish diets were evaluated for consistency with the US Food and Nutrition Board's Acceptable Macronutrient Distribution Ranges (AMDRs) and with the dietary recommendations of several health organizations.
Results
The OmniHeart diets fulfilled the major AMDRs, but, of the popular diets, only the Zone diet did. The OmniHeart diets were generally consistent with national guidelines to prevent cancer, diabetes, and heart disease, whereas most popular diets had limitations for fulfilling one or more guidelines.
Conclusions
Although the OmniHeart protein and unsaturated fat diets were superior to the carbohydrate diet in improving CVD risk, all 3 study diets were consistent with national guidelines to reduce chronic disease risk, which suggests that the guidelines might now be fine-tuned to optimize disease prevention. Popular diets vary in their nutritional adequacy and consistency with guidelines for risk reduction.
INTRODUCTION
In 2002, the Institute of Medicine developed Acceptable Macronutrient Distribution Ranges (AMDRs) for total fat, n–6, and n–3 polyunsaturated fatty acids (PUFAs), carbohydrate, dietary fiber, and protein (1). These guidelines were designed to move beyond ensuring adequacy, ie, determining an Adequate Intake (AI) of these nutrients and to address the relation of macronutrients to chronic disease in the context of adequate physical activity and energy expenditure to maintain a healthy weight (1). In 2006, the American Heart Association (AHA) (2), the American Diabetes Association (ADA) (3), and the American Cancer Society (ACS) (4) updated their diet and lifestyle recommendations with guidelines consistent with the IOM's document (Table 1). All of these oganizations recommended a dietary pattern rich in vegetables and fruit and promote the consumption of whole grains instead of refined grains. The AHA and ADA included specific targets for saturated fat and cholesterol (2, 3, 6).
TABLE 1.
Dietary guidelines to reduce chronic disease risk1
| Nutrient | IOM | AHA | ADA | ACS |
|---|---|---|---|---|
| Carbohydrate | 45−65% (≥130 g/d) | 1) Consume a diet rich in vegetables and fruit | 45−65%2,3 (≥130 g/d) | 1) Eat ≥5 servings of a variety of vegetable and fruit each day |
| 2) Choose whole-grain, high-fiber foods | 2) Choose whole grains over refined grains | |||
| 3) Minimize intake of beverages and foods with added sugars | ||||
| Protein | 10−35% (0.8 g/kg) | 1) Use lean cuts of meat and remove skin from poultry | 10−35% (≤20% if diabetic) | 1) Limit consumption of processed and red meats |
| 2) Consume fish, especially oily fish, at least twice a week | 2) Choose fish, poultry, or beans as an alternative to beef, pork, and lamb | |||
| Fat | 20−35% | 25−35%4 | 20−35%3 | NR |
| Linoleic acid | 5−10% | NR | NR | NR |
| α-Linolenic acid | 0.6−1.2% | NR | NR | NR |
| Saturated fat | as low as possible | <7% | Normolipidemic: <10% | NR |
| Hyperlipidemic: <7% | ||||
| trans-Unsaturated fat | as low as possible | <1% | as low as possible | Consume as few trans fats as possible |
| Cholesterol | as low as possible | <300 mg/d | Normolipidemic: <300 mg/d | NR |
| Hyperlipidemic: <200 mg/d | ||||
| Dietary fiber | Women: 25 g/d | Increase fiber intake by eating beans (legumes), whole-grain products, fruit, and vegetables | 14 g/1000 kcal | Increase fiber intake by eating beans (legumes), whole-grain products, fruit, and vegetables |
| Men: 38 g/d |
IOM, Institute of Medicine (1); AHA, American Heart Association (2, 5); ADA, American Diabetes Association (3, 6); ACS, American Cancer Society (4); NR, no specific recommendation.
Whole grains, fruit, vegetables, and low-fat milk as the primary sources.
Carbohydrate + monounsaturated fat should provide 60−70% of energy.
Use liquid vegetable oils in place of solid fats.
Against this background of health guidelines are popular diets with a limited evidence base of randomized trials, several of which have shown a reduction in risk factors for CVD or short-term weight loss (7–12). The macronutrient content of some of these diets diverges markedly from guidelines (13, 14), whereas others appear to be mainly consistent with guidelines (15–17). These popular diets include very-low-fat vegetarian diets (eg, Dean Ornish's diet); Mediterranean dietary patterns characterized by a higher intake of monounsaturated fatty acids (MUFAs); higher-protein, lower-carbohydrate diets that are low in fat (eg, the Zone diet); and higher-protein, lower-carbohydrate diets that are more liberal with fat, such as the South Beach and Atkins diets. The nutritional adequacy, long-term safety, sustainability, and impact of these popular diets on disease risk have not all been evaluated rigorously.
The Dietary Approaches to Stop Hypertension (DASH) eating pattern—a high-carbohydrate diet rich in fruit, vegetables, and low-fat dairy foods—reduced blood pressure and serum lipid risk factors in both average-and high-risk subgroups (18–20). The Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart) extended the approach of the DASH diet to determine the effect of macronutrients on CVD risk factors. Substitution of 10% of energy from carbohydrate with either protein or unsaturated fat enhanced the dietary effects on blood pressure, lipid risk factors, and estimated risk of coronary heart disease (CHD) (21).
The objective of this study was to provide a comparison of the macronutrients in the OmniHeart Diets with those in several popular diets and with national health guidelines. The macronutrient adequacy of the OmniHeart diets, DASH, and 5 popular diets was first evaluated using the AMDR criteria. The consistency of these diets with guidelines to prevent chronic disease issued by the AHA, ACS, and ADA was then assessed. We then comment on the healthfulness of the 3 OmniHeart Trial diets—high-carbohydrate (Omni-Carb), high-protein (Omni-Protein), and high unsaturated fat (Omni-Unsat) diets—compared with that of the DASH diet and 5 popular diets: the Atkins, Ornish, South Beach, Mediterranean, and Zone diets.
METHODS
Seven-day menu plans were constructed for each diet. The DASH and OmniHeart meal plans used were those previously developed at the time of the primary publications (21, 22), and the popular diets were developed by using Food Processor nutritional analysis software (version 8.0; ESHA Research, Salem, OR) and the guidelines and sample menu plans published in diet books (13–17, 23). How the 7-d menu plans for the Atkins, Zone, Mediterranean, Ornish, and South Beach diets were derived is outlined in Appendix A. Data are presented as means (±SEMs) of the 7-d analysis, obtained by using Microsoft EXCEL XP (Microsoft, Redmond, WA).
RESULTS
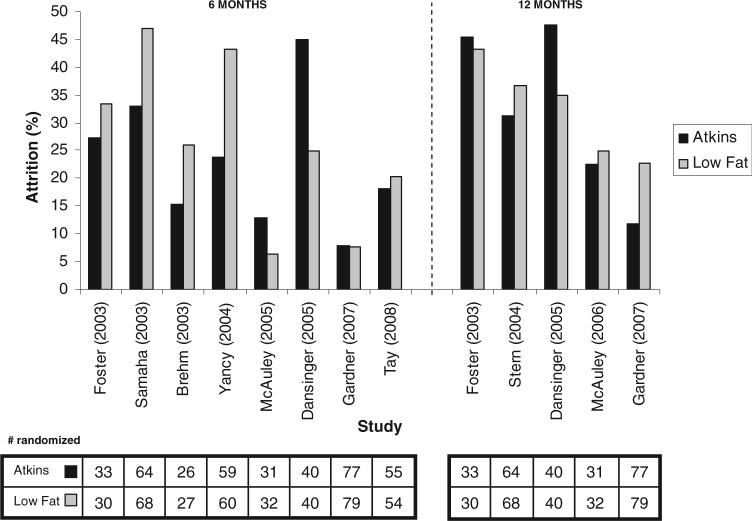
Typical 1-d menus of the evaluated diets are shown in Table 2 (popular diets) and Table 3 (DASH and OmniHeart Diets). The macronutrient profiles of these diets are illustrated, in order of decreasing carbohydrate content, in Figure 1; profiles for the AHA's Therapeutic Lifestyle Changes diet (AHA TLC) (5) and the third National Health and Nutrition Examination Survey (NHANES III) (24) are provided as reference. The Ornish diet was highest in carbohydrate (75% of energy) and dietary fiber (67 g/2000 kcal) and lowest in fat (7%), saturated fat (1%), and cholesterol (6 mg/d); the Atkins diet was the lowest in carbohydrate (9%) and fiber (20 g/2000 kcal) and the highest in fat (62%), saturated fat (23%), and cholesterol (731 mg). Neither diet met national guidelines for macronutrient intake. The Zone diet had the highest protein content (35%) and meets the national guidelines for intakes of fat and protein, but not for carbohydrate. The other diets analyzed had moderate mixes of protein (16−26%), carbohydrate (33−54%), and fat (28−46%).
TABLE 2.
Sample 1-d menu plans for 5 popular diets
| Atkins | Mediterranean | The Zone | Ornish | South Beach | |
|---|---|---|---|---|---|
| Breakfast | Scrambled eggs, turkey sausages, oatmeal | Sliced peaches, scrambled egg with spinach, whole-grain bread with olive oil, low-fat cappuccino | Poached fruit with cheddar cheese, skim milk, coffee | Apple pancakes with cinnamon, fresh berries, nonfat yogurt, whole-wheat toast with preserves, warm beverage | Fresh orange, sliced tomato and ham, frittata, multigrain toast, low-sugar fruit spread, decaffeinated coffee |
| Lunch | Greek salad with Romaine lettuce, half a tomato, feta cheese, olives, and dill vinaigrette; small can of tuna, lentils, apple | Striped bass (Oreganato); pasta with peas, asparagus, and tomato sauce; grilled zucchini and yellow squash with olive oil and garlic; whole-grain bread with olive oil; strawberries drizzled with balsamic vinegar | Italian style chicken, water | Bruschetta with sun-dried tomatoes and capers; rice, lentil, and spinach pilaf; tossed green salad; fresh fruit | Tuna, cucumber, and red pepper salad; lemony dill dressing; sugar-free gelatin, dessert |
| Dinner | Veal scallops with white wine caper sauce, sautéed spinach, gelatin dessert made with sucralose topped with heavy whipping cream, carrots | Broiled lamb chops, spaghetti with tomato sauce and arugula, mixed green salad with champagne dressing, whole-grain bread with olive oil, melon slices | Deviled steak, tossed salad with olive oil, and water | Tofu gumbo, Basmati rice with peas, black-eyed pea salad, grilled asparagus with vegetables, green salad, figs and blueberries in citrus broth | Apricot-glazed Cornish Hen, couscous, Bibb lettuce salad with olive oil and balsamic vinegar, chocolate sponge cake |
| Snacks | Controlled-carbohydrate strawberry shake, walnuts | Low-fat yogurt, raisins, and walnuts | Cottage cheese, nuts, 1/2 piece of fruit | Fruit | Baba Ghannouj (eggplant purée) |
TABLE 3.
Sample 1-d menu plans for the Dietary Approaches to Stop Hypertension (DASH) and OmniHeart diets
| Diet | DASH | Omni-Carb | Omni-Protein | Omni-Unsat |
|---|---|---|---|---|
| Breakfast | Bran flakes cereal, medium banana, low-fat milk, whole-wheat bread, soft (tub) margarine, orange juice | Grapefruit juice, multibran cereal, skim milk, banana | Tomato juice, scrambled egg substitute with low-fat shredded cheese; hot cereal: bulgur wheat with soy, olive oil, margarine, raisins, sugar; skim milk | Orange juice, cereal with raisins, skim milk, white bread with olive oil margarine, jelly |
| Lunch | Chicken salad, whole-wheat bread, Dijon mustard, salad: fresh cucumber slices, tomato wedges, sunflower seeds, Italian dressing, low-calorie fruit cocktail juice pack | Chicken sandwich: whole-wheat bread, chicken breast, mayonnaise; salad: lettuce with olive oil; trail mix: almonds, dried apricots | Vegetarian burger: hamburger roll, vegetarian patty, barbecue sauce, lettuce with tomato slices; broccoli salad; unsalted potato chips; chocolate pudding | Chicken sandwich: white bread, chicken breast, barbecue sauce, olive oil margarine; olive oil potato chips, spinach salad with tomato and olive oil balsamic dressing; broccoli salad with safflower oil; tomato juice |
| Dinner | Beef, eye of the round, beef gravy, fat-free green beans sautéed with canola oil, small baked potato: sour cream, fat-free grated cheddar cheese, reduced-fat chopped scallions; whole wheat roll, soft (tub) margarine, small apple, low-fat milk | Penne bean pasta with spinach, tomato, olive oil, beef meatballs, parmesan cheese; tossed salad: Romaine lettuce, cherry tomatoes, Italian dressing with safflower oil; fresh grapes; peppermint patty | Black bean taco: black beans and wheat protein with vegetables; 3-grain salad with olive oil; tortilla chips; chicken breast; fresh orange; skim milk | Black bean taco: black beans with vegetables; 3-grain pilaf with olive oil; tortilla chips; carrots (cooked); pecan cookie; skim milk |
| Snacks | Almonds; unsalted raisins; fat-free, no-sugar added fruit yogurt; walnuts | Small fresh apple, yogurt | Fat-free cottage cheese, mandarin oranges, almonds | Mandarin oranges, almonds |
FIGURE 1.
Macronutrient profiles of popular diets, the OmniHeart and Dietary Approaches to Stop Hypertension (DASH) study diets, the American Heart Association Therapeutic Lifestyle (AHA TLC) guidelines (5), and typical US macronutrient intakes as reported in the third Health and Nutrition Examination Survey (NHANES III; 24). The eating patterns are ordered with the highest-carbohydrate diet starting on the left and the lowest on the right. The Atkins diet profile is for the life-long maintenance phase, and the South Beach diet profile is for phase 3. Small amounts of alcohol (0.2−0.8% of energy) were also present in the Ornish, Mediterranean, Atkins, Zone, and South Beach diets. Percentages may not add up to 100% because of rounding.
Carbohydrate
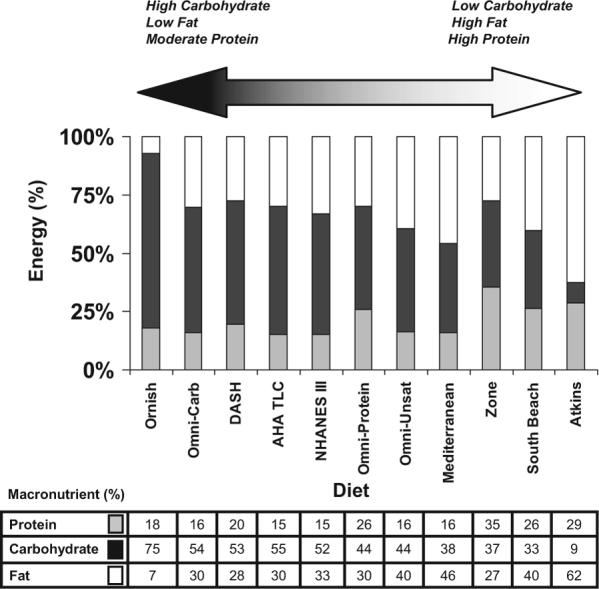
Each OmniHeart diet and the DASH diet were consistent with the AMDR (45−65%) for available carbohydrate (total carbohydrate minus dietary fiber) (Figure 2). The Atkins (9 ± 1%), South Beach (33 ± 4%), Zone (37 ± 1%), and Mediterranean (38 ± 2%) diets all provided <45% of energy from carbohydrate, and the Ornish diet exceeded the recommended intake of carbohydrates (75 ± 1%).
FIGURE 2.
Comparison of the calculated macronutrient profiles (mean ± SEM) of various diet plans with the Institute of Medicine's Acceptable Macronutrient Distribution Ranges (AMDR). Solid horizontal lines represent the upper and lower limits of the AMDR for the macronutrient. ■, exceeds the AMDR;  , meets the AMDR; □, failed to reach the minimum AMDR. DASH, Dietary Approaches to Stop Hypertension.
, meets the AMDR; □, failed to reach the minimum AMDR. DASH, Dietary Approaches to Stop Hypertension.
The OmniHeart and DASH diets provided carbohydrate from whole grains, fruit, and vegetables at levels well above the Recommended Dietary Allowance (RDA) and the ADA recommendation of 130 g/d (226 ± 2to283 ± 2 g/d), as did the Ornish (278 ± 16 g/d) and Mediterranean (235 ± 10 g/d) diets. Both moderately carbohydrate-restricted diets, the South Beach (129 ± 17) and the Zone (120 ± 7) diets, fell slightly below the RDA and ADA recommendations and featured a variety of fruit, vegetables, and whole grains. The Atkins diet severely restricted the intake of fruit, vegetables, and whole grains and provided only 47 ± 2 g carbohydrate/d, a level below the RDA and ADA guidelines.
Dietary fiber
The Omni (33 ± 1 g/2000 kcal) and DASH (29 ± 1 g/2000 kcal) diets provided dietary fiber at a level consistent with the IOM/ADA target of 28 g. Of the popular diet plans, only the Atkins diet failed to provide fiber at the recommended level (20 ± 1 g). Both the Mediterranean and South Beach diets provided ≈28 g/2000 kcal. The diets with the highest fiber contents were the Zone and the Ornish diets, which provided about twice the IOM/ADA target per 2000 kcal: 52 ± 1 and 67 ± 3 g/2000 kcal, respectively.
Protein
The Omni-Protein (26 ± 0% of energy from protein), Atkins (29 ± 3%), Zone (35 ± 2%), and South Beach (26 ± 2%) diets fell toward the upper range of the AMDR, whereas the Ornish (18 ± 0%), Mediterranean (16 ± 1%), DASH (20 ± 1%), Omni-Unsat (16 ± 0%), and Omni-Carb (16 ± 0%) diets were closer to the lower limit. Because the ADA discourages diets with >20% protein for individuals with diabetes and because the long-term safety of these diets has not been established (3, 6), the Omni-Protein, Atkins, Zone, and South Beach diets would not meet ADA guidelines for this group. All 9 diets meet the RDA for protein for the average 90-kg male (0.8 g/kg), with the exception of the Ornish diet, which falls marginally below this level (0.72 ± 0.03 g/kg). All 9 diets fall within the AMDR for protein (Figure 2).
The AHA recommends that protein comes from fat-free or low-fat milk and milk products, lean meats, poultry, fish, nuts, seeds, and legumes (2). The ACS specifically recommends limiting the consumption of processed and red meats (4).
All 3 OmniHeart diets and the DASH, Mediterranean, Zone, and South Beach diets provided a mix of lean animal and plant proteins from recommended sources (Table 4). The predominant sources of protein in the Atkins diet were of animal origin, such as fish, cheese, beefsteak, pork, chicken, and egg. In contrast, the Ornish diet derived all of its protein from plant sources, such as legumes, tofu, buckwheat, and oatmeal, with small amounts of dairy protein from low-fat yogurt and cottage cheese.
TABLE 4.
Protein sources in the OmniHeart, the Dietary Approaches to Stop Hypertension (DASH), Ornish, South Beach, Mediterranean, Zone, and Atkins diets1
| OmniHeart/DASH (85−100 g) | Ornish (65 g) | South Beach (98 g) | Mediterranean (101 g) | Zone (113 g) | Atkins (160 g) |
|---|---|---|---|---|---|
| Low-fat dairy (14.6%) | Legumes/soy (44.5%) | Fish (15.2%) | Fish (23.1%) | Chicken (17.6%) | Fish (13.3%) |
| Fish (10.9%) | Grains (24.5%) | Chicken (13.2%) | Grains (11.7%) | Legumes/soy (17.3%) | Hard cheese (10.4%) |
| Chicken (10.7%) | Vegetables (23.6%) | Red meat (13.0%) | Vegetables (10.0%) | Vegetables (15.6%) | Red meat (9.3%) |
| Legumes/soy (10.3%) | Fruit (5.3%) | Egg (11.6%) | Low-fat dairy (9.2%) | Low-fat dairy (9.1%) | Sausage/pork (9.3%) |
| Turkey (8.8%) | Hard cheese (11.3%) | Red meat (8.4%) | Red meat (8.3%) | Chicken (8.5%) | |
| Grains (8.0%) | Low-fat dairy (7.0%) | Egg (7.3%) | Egg (7.6%) | Egg (8.0%) | |
| Red meat (8.0%) | Grains (6.3%) | Shellfish (6.4%) | Turkey (5.6%) | Low-fat dairy (7.7%) | |
| Nuts (6.5%) | Turkey/hen (5.0%) | Chicken (6.0%) | Shellfish (4.5%) | Turkey (6.7%) | |
| Hard cheese (4.5%) | Shellfish (4.4%) | Nuts (4.0%) | Sausage/pork (4.2%) | Vegetables (5.3%) | |
| Nuts (5.2%) | |||||
| Other (17.8%) | Other (2.1%) | Other (14.3%) | Other (14.0%) | Other (12.0%) | Other (16.3%) |
Foods listed provided ≈80% of the total protein for each diet. Foods at the top of each list provided the most protein and foods at the bottom the least. Average grams of protein per day are listed in parentheses in the column headings.
Total fat
The AMDR for total fat was set at 20−35% of energy (1), a range supported by the ADA (3). The AHA guidelines recommend from 25% to 35% of energy from fat (2, 5). The ACS claims that there is little evidence that total fat increases cancer risk, as long as it does not lead to weight gain (4). All 3 OmniHeart study diets and the DASH diet provide between 28 ± 1% and 40 ± 1% fat (Figure 2).
Of the popular diets, only the Zone diet fell within the AMDR, ADA, and AHA guidelines for total fat (27 ± 2%). The Mediterranean (46 ± 2%), Atkins (62 ± 3%), and South Beach (40 ± 2%) diets all provided >35% of energy from fat, and the Ornish diet provided <10% fat (7 ± 1%). However, the fatty acid profiles were very different between the diets.
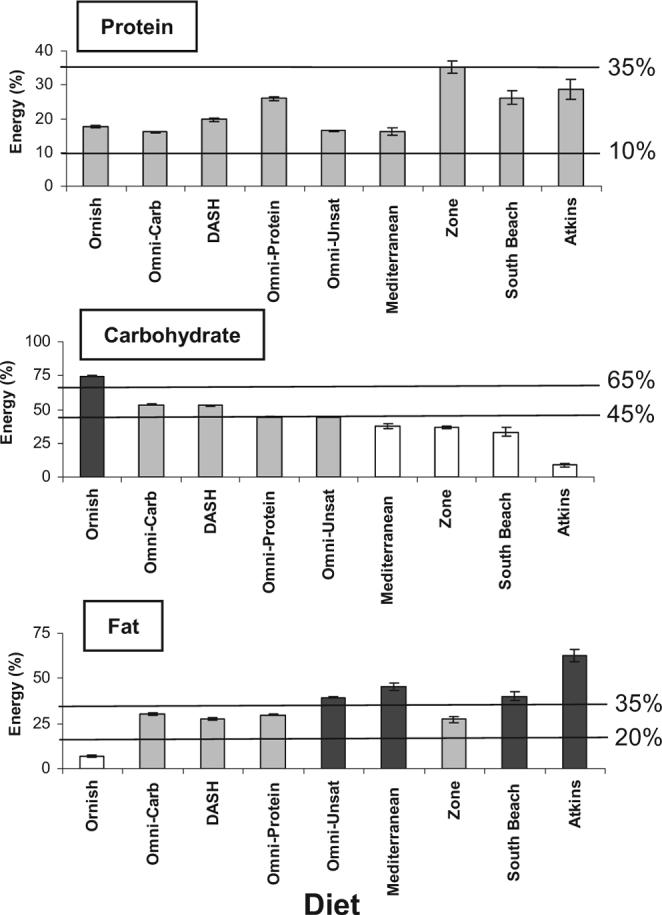
Saturated fat
The fatty acid profile and relative fat content of the various diets is shown in Figure 3. The IOM concluded that an increased risk of adverse events begins at saturated fat intakes >0 and therefore recommended that individuals “eat as little as possible while consuming a diet adequate in important other essential nutrients” (25). The AHA set an upper limit of 7% of energy from saturated fat for the general population (2), whereas the ADA recommends <10% for the general population and <7% for those with an LDL-cholesterol concentration >100 mg/dL (3).
FIGURE 3.
Typical fatty acid profiles of popular diets, the OmniHeart and Dietary Approaches to Stop Hypertension (DASH) study diets, the American Heart Association Therapeutic Lifestyle (AHA TLC) guidelines (5), and typical US macronutrient intakes as reported in the third Health and Nutrition Examination Survey (NHANES III; 24) as “reference points.” Solid horizontal line represents the 7% upper level of intake for saturated fat proposed by the AHA; diets to the right of the vertical dashed line provided >35% of energy from total fat. The Ornish, Zone, DASH, and OmniHeart study diets provided ≤7% of energy from saturated fat; the South Beach (phase 3) and Mediterranean diets provided ≤11% of total energy from saturated fat. The Atkins profile is for the life-long maintenance phase and provided >20% of energy from saturated fat. Note that the sum of fatty acid classes may not add up to the total amount of fat, because total fat may include some non-fatty acid material, such as glycerol, phosphate, sugar, or sterol not analyzed in the foods.
The OmniHeart (6 ± 0 to 7 ± 0%), DASH (6 ± 0%), Ornish (1 ± 0%), the Zone (6 ± 1%), and Mediterranean (8 ± 1%) diets provided close to or <7% of energy from saturated fat. Both the South Beach (11 ± 1%) and Atkins (23 ± 2%) diets provide saturated fat at a level that exceeds the AHA and ADA guidelines.
Polyunsaturated fat
The IOM suggests an intake of 5−10% of total energy from linoleic acid, 0.6−1.2% for α-linolenic acid (25), but no AMDR for total PUFA. The AHA and ADA do not set a specific target for PUFAs, but recommend consuming oily fish at least twice per week (2, 3). Our data were only sufficient to examine total PUFAs, not individual essential fatty acids. The Omni-Protein and Omni-Carb diets provided 8 ± 0% to 9 ± 0% of energy from PUFAs, the Omni-Unsat provided 10 ± 0%, and DASH provided 7 ± 0%. The Ornish plan provided the least amount of PUFAs (2 ± 0% of energy, or 4 ± 0 g) of the diets considered, and the Atkins diet provided the most (12 ± 1%, or 31 ± 5 g). The South Beach (8 ± 1%) and Mediterranean (7 ± 1%) diets provided a similar fraction of energy from PUFAs, whereas the Zone diet provided 6 ± 1% (Figure 3). Fish (though not necessarily oily fish), nuts, and vegetable oils were a part of all meal plans, except the Ornish diet.
Monounsaturated fat
No specific recommendations for total MUFAs have been made by the IOM, AHA, ADA, or ACS (2–4, 25); however, the AHA and ADA suggest that MUFAs can be part of a healthy eating plan that provides 20−35% of energy from fat (2, 3). The Omni-Unsat diet provided 20 ± 0% of energy from MUFAs, whereas the DASH, Omni-Protein, and Omni-Carb diets each provided 12 ± 0% to 13 ± 0% of energy from MUFAs. The Mediterranean diet provided 28 ± 2% of energy from MUFAs, the Atkins diet 23 ± 2%, the South Beach diet 18 ± 1%, the Zone diet 13 ± 1%, and the Ornish diet 2 ± 0% (Figure 3).
trans-Unsaturated fat
The IOM concluded that an increased risk of adverse events begins at trans-unsaturated fat (trans fat) intakes >0 and therefore recommends that individuals “eat as little as possible while consuming a diet adequate in important other essential nutrients” (25). The American Heart Association has set an upper limit of 1% energy from trans fat (2), and the ADA (3) and ACS (4) suggest that the intake of trans fat be minimized. Despite divergent macronutrient and food recommendations, all authors of these popular diet plans shunned processed foods and fast food items high in trans fats. Therefore, these diets provided ≤1% of energy from trans fats, as analyzed.
Cholesterol
Although the IOM set no AI or RDA for dietary cholesterol because of its endogenous synthesis, they recommend that its dietary intake be kept as low as possible because of the direct, progressive association between cholesterol intake and LDL cholesterol (26). The AHA and ADA recommend that the intake of dietary cholesterol be <300 mg/d for adults without diabetes and the intake of LDL cholesterol be <100 mg/dL (2, 3). The ADA set a target of <200 mg/d for those with diabetes or whose LDL is ≥100 mg/dL (6). No target was set for dietary cholesterol by the ACS, specifically for cancer prevention (4).
All of the OmniHeart diets and the DASH diet provided <150 mg cholesterol at the 2100-kcal level (<136 mg/2000 kcal), which would conform to AHA and ADA guidelines. Other popular diets varied widely with respect to cholesterol content. The Ornish diet was very low in cholesterol (6 ± 1 mg/d). The Zone (208 ± 49 mg/d) and South Beach (221 ± 26 mg/d) diets met the AHA and ADA recommendations for individuals without diabetes and/or without elevated LDL cholesterol. The Atkins (731 ± 81 mg/d) and Mediterranean (337 ± 91 mg/d) diets exceeded these cholesterol targets.
DISCUSSION
The intent of this analysis was to evaluate the healthfulness of several popular diets and the OmniHeart diets; to do this, we evaluated each diet's consistency with national dietary guidelines. We found that all diets met the AMDR for protein; the Atkins, Mediterranean, Omni-Unsat, and South Beach diets exceeded the AMDR for total fat (40−62%); and the Atkins, South Beach, Mediterranean (9−38%), and Ornish (75%) diets fell outside the AMDR for carbohydrate. Each diet varied with respect to its compliance with national guidelines from the AHA, ACS, and ADA.
Whether or not a diet that falls outside the AMDR for a given macronutrient is necessarily “unhealthy” depends on the food choices that cause a diet to exceed the macronutrient target. A diet that is 30% fat, 50% carbohydrate, and 20% protein might meet the AMDR, but could still contain 15% saturated fat, carbohydrates from refined grains, and high amounts of processed meat (ie, a typical “Western” dietary pattern). However, the Omni-Unsat, Mediterranean, and South Beach diets exceeded the upper AMDR for total fat, but were high-fiber diets low in saturated fats that included ample unsaturated fats, whole grains, fruit, and vegetables. In contrast, the very-low-fat content of the Ornish diet did not meet the minimum fat requirements of national organizations, yet provided healthful sources of protein (eg, legumes and nuts), ample fruit and vegetables, and low amounts of saturated fat. These exceptions indicate that compliance with the AMDR should not be the only criterion by which to assess a diet.
The possible health effects of popular diets, though numerous in theory, have not been tested in controlled feeding studies with hard endpoints (eg, CHD or cancer), likely because large randomized controlled trials of diet are subject to ethical, financial, logistical, and methodologic constraints. Therefore, a discussion of the impact of various macronutrient combinations on chronic disease risk must draw on literature exploring the relation between macronutrients and biologic intermediates (eg, LDL cholesterol). To provide some context for our evaluation of the diets, we discuss and comment on the potential impact of these diets on disease risk in light of the best available evidence for outcomes; and, in the absence of data on hard endpoints, we discuss the effects of the diets and their components on intermediates such as blood lipids, blood pressure, and insulin sensitivity.
Higher-protein diets
The Omni-Protein, South Beach, and Zone diets were higher-protein diets generally consistent with national recommendations for intakes of saturated fat, fiber, and cholesterol; however, several aspects of the higher-protein, higher-fat Atkins approach raise concerns for general health. Unlike the healthful higher-protein diets mentioned above, the Atkins diet severely restricts the intake of fruit, vegetables, and whole grains, which results in a lower fiber intake than all other higher-protein diet. Randomized trials suggest the actual fiber intake with the Atkins diet is likely 10−15 g/d, and participants frequently report constipation while following this diet (8, 27, 28). This low fiber intake may increase the risk of diverticular diseases (29). A meta-analysis of controlled trials reported that Atkins-type diets raise LDL-cholesterol concentrations slightly, even in the setting of weight loss (30), and, the liberal intake of red and processed meats advocated by this diet may increase the risk of colon, rectum (31–33), and prostate (34) cancers. For these reasons, the high-protein food sources associated with an Atkins diet are not prudent for overall health.
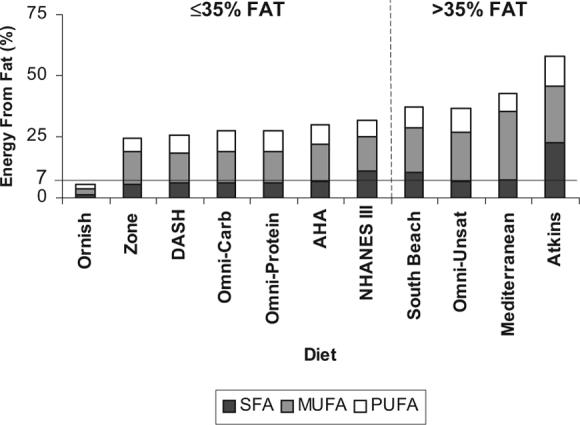
The IOM, AHA, ADA, and ACS emphasize balancing physical activity with energy intake to achieve and maintain a healthy body weight (1–4). Although we lack long-term controlled studies with large samples comparing diets with different macronutrient contents designed for weight loss, 6 randomized controlled trials conducted between 2003 and 2007 found Atkins-type diets superior to high-carbohydrate, low-fat diets for weight loss at 6 mo (7, 27, 28, 35–37) in overweight individuals with or without components of the metabolic syndrome. In these trials, Atkins diets also preserved HDL cholesterol (7, 27, 28, 35–37) and reduced triacylglycerols (27, 36, 37). When follow-up in 4 of these cohorts was extended to 1 y, however, the Atkins weight-loss advantage did not persist, and improvements in serum lipids were attenuated (7, 28, 38, 39).
Studies of high-protein diets have consistently reported high dietary adherence early in the trials, when contact between participants and the research team was frequent, and reduced compliance at later time points, when participants were not as closely monitored. Although this “real-world” condition improves generalizability, it likely resulted in smaller than expected contrasts between macronutrient profiles at the end of follow-up (8, 28, 35, 39). Attrition rates in 6-mo trials were high in Atkins and in low-fat arms (Figure 4), averaging 8−45% for Atkins and 6−47% for low fat (7, 8, 27, 28, 35–37, 40); for 12-mo trials, the dropout rate ranged from 12% to 48% in Atkins and from 23% to 43% in low fat (7, 8, 28, 38, 39). The proportion of participants that cited a dislike of the diet as the main reason for discontinuation was similar for both diets (8, 28, 35, 37, 40). Notably, in the one large trial that collected a detailed symptom diary, those in the Atkins trial arm reported more episodes of constipation, headache, halitosis, muscle cramps, diarrhea, and general weakness than did those in the low-fat arm (27), which may limit the general applicability of such a diet in clinical practice.
FIGURE 4.
Comparison between attrition rates in studies of the Atkins diets and in low-fat diets. Although early studies compared Atkins diets only to low-fat diets, later studies included other popular diets (7, 8, 27, 28, 35–40). For studies that included other popular diets, we present the attrition rates in only the Atkins and low-fat (≤30% of energy) arms. The number of subjects randomly assigned to begin each diet is shown in the chart.
Evidence is emerging that higher-protein diets, even in the absence of weight loss, may be beneficial for health. A large prospective cohort study with 20 y of follow-up found low-carbohydrate, higher protein diets compared with low-fat diets are not associated with increased risk of CHD in women, and diets rich in vegetable protein and fat were found to be protective against CHD (41). Vegetable protein, but not animal protein, was found to have an inverse relation with blood pressure in the INTERMAP study (42), consistent with the blood pressure–lowering effect of the Omni-Protein diet. Compared with a typical diet, all Omni diets lowered LDL cholesterol, but the Omni-Protein diet showed a greater reduction than did the Omni-Carb diet, and the triacylglycerol-lowering effect was stronger for protein than for unsaturated fat, which suggested that a specific beneficial effect of protein on lipid risk factors (21). In addition to these benefits, higher-protein diets may offer better protection against the progression of insulin resistance to type 2 diabetes (43), by reducing circulating free fatty acid concentrations, than higher-fat, low-carbohydrate diets (44).
Whether a higher protein intake (26−35% of energy) is un-healthful remains controversial. The upper limit of the AMDR was set to mitigate against osteoporosis, kidney stones, and renal failure that might accompany chronically high protein intakes (45). Two small 12-wk intervention trials of high-protein diets in healthy adults showed either an adverse effect (46) or no effect (47) on markers of bone turnover or risk of nephrolithiasis, and other trials suggested beneficial effects of a high protein intake on bone health (48, 49). Observational studies in the general population did not find a relation between a high animal protein content in the diet and the development of renal stones (50, 51) and suggest that high-protein diets may only be detrimental in those with existing renal insufficiency (52). This may be of concern to individuals with hypertension or diabetes, because they may have impaired renal function. Further research is needed to better understand the potential adverse effects of chronic high protein intakes.
Higher-fat diets
Although the Omni-Unsat diet exceeded the IOM's target for total fat, it remained within recommended intakes of carbohydrate, saturated fat, cholesterol, and fiber. Furthermore, this diet was rich in whole grains, fruit, and vegetables and thus might be expected to improve CVD risk factors, as it indeed did, and to possibly provide protection against several cancers and type 2 diabetes. Other higher-fat diets, such as the South Beach and the Mediterranean diets, had a slightly higher total fat content than did the Omni-Unsat diet (40−45% of energy), and all of these diets exceeded the AMDR upper limit for total fat, but, similarly to the Omni-Unsat diet, were low in saturated fat and cholesterol because of the inclusion of oils and nuts rich in MUFAs. The South Beach and Mediterranean diets also encourage the consumption of whole-grains, which enhances the potential health benefit. In contrast, the Atkins diet provided considerably more fat (62%) than did the other higher-fat diets, provided excessive amounts of saturated fat (23%) and cholesterol (731 mg/d), and provided carbohydrate and fiber in amounts below the RDA. The different fatty acid profiles of these diets are also important determinants of their healthfulness and likely are of much greater importance than the total fat content.
Despite their claim that insufficient data were available to determine a defined total fat intake at which there is a risk of chronic disease (25), the IOM arrived at an upper limit of 35% for total fat intake largely on the basis of 2 theoretical concerns—the risk of excessive energy intake and weight gain associated with very-high-fat diets and the correlation of saturated fat intake with total fat intake (1). These lines of reasoning are controversial (53).
With respect to the first concern, although fat is the most energy-dense nutrient, in 2 small randomized trials of weight loss, Mediterranean-style diets that exceeded 35% of energy from fat, were high in MUFAs, low in saturated fat, and rich in fruit, vegetables, legumes, whole grains, and fish, resulted in greater weight loss and more improvement in cardiovascular disease (CVD) risk factors than did low-fat, high-carbohydrate diets (11, 54). Furthermore, in the classic Seven Countries Study, the population of Crete had the lowest rates of CVD and cancer, despite a 43% total fat intake. The Cretan diet was low in saturated fat (<8%), high in MUFAs (27%) (55), and rich in fruit, nuts, legumes, and meat of grazing animals, which contained n–3 fats.
The Women's Health Initiative found that a 29%-fat diet was not superior to a 38%-fat diet for long-term weight maintenance in postmenopausal women (56), nor did the lower-fat diet significantly reduce the risk of CHD, stroke, CVD (57), or several cancers (58–60) A major criticism of the study is that the targeted fat reduction of 20% was not met, which calls into question the sustainability of a low-fat approach to reduce the risk of heart disease and cancers.
Second, a diet high in total fat that is low in saturated fat and does not lead to weight gain (or promotes weight loss in the setting of a caloric deficit) does not appear to contribute to the development of insulin resistance, type 2 diabetes, or certain forms of cancer. Although early epidemiologic studies have linked high-fat diets to insulin resistance (61, 62) and cancer, these correlations were confounded by obesity (63), a lack of physical activity (64), and other dietary factors. MUFAs do not appear to increase the risk of type 2 diabetes (65), and, when substituted for high-glycemic index foods, high-MUFA foods improve the postprandial glucose and insulin response (66). An inverse association between MUFA (67) or olive oil (68) intake and breast cancer has been shown in several studies; others showed no increased risk with increasing MUFA consumption (69). Similar results were found for diets high in MUFA-rich vegetable oils and prostate cancer (70, 71). These findings suggest that the benefits of a high MUFA intake as part of an Omni-Unsat diet or a Mediterranean dietary pattern may outweigh concerns related to a higher total fat intake.
Higher-carbohydrate diets
The Omni-Carb diet conformed to the IOM's AMDR and national guidelines in all respects, providing 54% of energy from carbohydrate and acceptable amounts of saturated fat, cholesterol, and fiber. However, replacement of 10% of the energy from carbohydrate with either protein or unsaturated fat reduced blood pressure, triglycerides, and non-HDL cholesterol in the OmniHeart trial (21). The AMDR for carbohydrate took into consideration the adverse effects on triglycerides and HDL cholesterol seen when higher-carbohydrate, low-fat diets are adopted by a sedentary population (72). An emerging concern is that low-fat diets may not be effective for weight management (56). However, these effects may be avoided if low-glycemic-index carbohydrates are the predominant foods in the diet (1) and individuals adopt an active lifestyle.
The Ornish diet exceeded the upper limit of the AMDR for carbohydrates (75%); however, it was high in fiber and provided generous amounts of low-glycemic-index whole grains, such as brown rice, buckwheat, and whole-grain flour. These are choices consistent with AHA guidelines. The most impressive support for the health benefits of this diet come from the Lifestyle Heart Trial (12, 73), which randomly assigned patients with angio-graphically documented CHD to either usual care or an intensive lifestyle change that included a very-low-fat, vegetarian diet; smoking cessation; and an exercise and meditation program. Patients in the treatment arm (n = 22) were highly compliant with the lifestyle changes, lost 20 lb (≈9 kg), and reduced LDL cholesterol by 40% after 1 y (73). These patients had a significant regression in atherosclerosis and had less than half as many cardiac events than did the usual care group at 5 y (12). However, because diet was not the only lifestyle factor modified, it is difficult to ascribe these benefits solely to diet. Subsequent trials found a less impressive reduction in risk factors when larger groups of less motivated individuals free of CHD adopted the same diet principles without intensive lifestyle modification (8, 28). Furthermore, very-low-fat diets may result in suboptimal concentrations of essential long-chain polyunsaturated fatty acids if food products are not carefully chosen (74). In addition, such a high-carbohydrate, low-fat diet may have both health-promoting (eg, reductions in LDL cholesterol and blood pressure) and possibly harmful (eg, reductions in HDL cholesterol and increases in triglycerides) effects.
Implications for practice
Although the optimal macronutrient profile of the diet remains unknown, data are emerging that compliance, rather than a specific macronutrient distribution, may be the most important determinant of whether or not a diet achieves its intended effect (eg, weight loss and chronic disease risk reduction) (8). To maximize adherence to any diet plan, it is imperative to consider an individual's food preferences, culture, lifestyle, and religious beliefs. Advocating a single dietary pattern to reduce chronic disease risk for a diverse population is unlikely to be an effective approach to promote health.
To this aim, the OmniHeart trial provided 2 alternatives to the conventional low-fat, high-carbohydrate DASH approach to maintaining health and reducing CVD risk. The OmniHeart trial showed that a modest redistribution in macronutrient composition from carbohydrate to protein or unsaturated fat can reduce the CVD risk according to the Framingham criteria by 16% to 21% (21). Of great interest is that these modifications in CVD risk were achieved in overweight subjects who did not lose weight. Both Omni-Protein and Omni-Unsat diets may be more sustainable than a high-carbohydrate diet and appear to have health advantages over extreme diets, such as the Atkins (which may increase the risk of CVD, cancer, and diabetes) and the Ornish (which may lower HDL cholesterol, increase triglycerides, and have inadequate polyunsaturated fatty acids) diets.
All 3 OmniHeart diets provided adequate amounts of macronutrients. In practice, the Zone, South Beach, and Mediterranean diets are all generally acceptable options that might be helpful for individuals looking for similar benefits for heart disease, cancer, and diabetes risk. These diets replace carbohydrate with protein and/or fat, are similar in concept to the OmniHeart trial, and may also have several salutary effects on chronic disease risk (9, 11, 37, 54).
Implications for research and policy
This article raises several important issues that are pertinent to research and policy recommendations on macronutrient intake. First, although the IOM recommends a wide range of macronutrient intakes, termed the AMDR, it is likely that some portion of this range is optimal. For instance, in the OmniHeart trial, a carbohydrate intake of 48% of energy was associated with a greater improvement in CVD risk factors than was a carbohydrate intake of 58% of energy, although both values fell within the AMDR for carbohydrate (21). Second, the AMDR limits should be reconsidered. The percentage of energy from fat tested in the Omni-Unsat arm (37%) exceeds the AMDR upper limit for fat of 35%. Third, considerable research is needed to understand the optimal sources and types of macronutrients. For example, types (eg, fructose) and food sources (eg, low-glycemic-index foods) of carbohydrate may have an even greater impact on health than the absolute amount of carbohydrate. Fourth, isocaloric feeding studies with 3 or more arms are an especially powerful type of study design to test the effects of diets with different macronutrient profiles.
As an isocaloric study, OmniHeart tested the effects of the diets without the confounding effects of weight loss. Also, the 3-group design made it possible to draw inferences about the macronutrient responsible for the observed effects. For instance, the Omni-Protein diet lowered blood pressure compared with the Omni-Carb diet (21). Without a third arm, it would be difficult to attribute the blood pressure reduction to lower carbohydrate or increased protein. However, the concurrent finding that the Omni-Unsat diet relative to the Omni-Carb diet also lowered blood pressure provides a parsimonious explanation—lower carbohydrate, rather than increased protein or unsaturated fat, reduced blood pressure. The public health implications of these findings warrant further attention.
Acknowledgments
We express our deep gratitude to the DASH and OmniHeart participants for their enthusiasm and willingness to participate in the studies and to the DASH and OmniHeart staff for their dedicated efforts in conducting the studies. Special thanks to Karen Yee for her assistance with creating and analyzing the menu plans.
The authors' responsibilities were as follows—FMS and LJA: conceived the idea for the manuscript; RJdS: analyzed and interpreted the data and wrote the manuscript; and JFS, RJdS, LJA, and FMS: contributed to the review and revision of the draft and approved the final version of the manuscript. None of the authors had a personal or financial conflict of interest.
APPENDIX
Creating 7-d menu plans
ATKINS
To create the Atkins “Maintenance” phase diet, the induction diet was first created by using a sample 1-wk menu from Dr Atkins's book (1) with the goal of keeping “net carbohydrates” (total carbohydrate minus total dietary fiber) to <20 g and to include 3 cups of salad or other vegetables daily. The “Maintenance” plan used this induction phase diet as a base, and foods providing ≈30 g net carbohydrates were added to this meal plan to attain a level of ≈50 g net carbohydrates/d.
ZONE
An individual's Zone diet plan depends on sex, weight, activity level, and approximate percentage body fat. For the purpose of this study, we chose to design a menu plan for a typical average middle-aged sedentary American male, because this would allow us to examine the impact of larger intakes of nutrients (though the macronutrient profile of a “Zone-perfect” diet would not differ appreciably between men and women). Using data from the NHANES III survey, the average weight of men aged 50−59 y was 89 kg, and the average height was 176 cm (BMI = 28.7) (2). These values, along with a percentage body fat of 18% (3) was used to determine a protein requirement using the formula of Sears (lean body mass in pounds × 0.5; 4). This resulted in a daily protein requirement of 80 g. We attempted to maintain a protein: carbohydrate ratio of 0.75, and we achieved a ratio of 0.75 ± 0.04. If we had used a woman, the ratio of carbohydrate to protein, and therefore the macronutrient composition, would have been almost identical, but the gram weight of nutrients and energy provided would be lower because our reference female would have been smaller (eg, height of 162 cm, weight of 64 kg, and BMI of 29.2 (2) and had a higher percentage body fat (32%) (3).
ORNISH, SOUTH BEACH, AND MEDITERRANEAN DIETS
Nutrient intakes from the Ornish and South Beach diets were computed directly from published 7-d menu plans for the Ornish (5) and phase 3 (Maintenance) South Beach (6) diets. A version of the Mediterranean diet was adapted from Acquista's book (7), based on the results of the Lyon Diet Heart Study.
Footnotes
Supported by grants HL67098, DK63214, HL68712, and RR02635 from the National Institutes of Health.
REFERENCES
- 1.Atkins R., Dr. Atkins' new diet revolution. Quill; New York: 2002. pp. 232–5. [Google Scholar]
- 2.Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index. United States 1960−2002. 2004:1–17. Adv Data. [PubMed] [Google Scholar]
- 3.Owens TA. MedLine Plus: Medical encyclopedia–Weight Loss. 2005.
- 4.Sears B. The zone: a revolutionary life plan to put your body in total balance for permanent weight loss. HarperCollins; New York, NY: 1995. p. 80. [Google Scholar]
- 5.Ornish D. Eat More, Weigh Less Dr. Dean Ornish's life choice program for losing weight safely while eating abundantly. 1 ed. Quill; New York, NY: 2001. pp. 106–11. [Google Scholar]
- 6.Agatston A. The South Beach diet: the delicious, doctor-designed, foolproof plan for fast and healthy weight loss. Random House; New York, NY: 2003. pp. 243–57. [Google Scholar]
- 7.Acquista A, Vandermolen LA. The Mediterranean Prescription: meal plans and recipes to help you stay slim and healthy for the rest of your life. Ballantine Books; New York, NY: 2006. pp. 115–8. [Google Scholar]
REFERENCES
- 1.Institute of Medicine . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academies Press; Washington, DC: 2002. Panel on Macronutrients and Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Macronutrients and healthful diets. pp. 769–879. 2005. [Google Scholar]
- 2.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 3.Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes–2006: a position statement of the American Diabetes Association. Diabetes Care. 2006;29:2140–57. doi: 10.2337/dc06-9914. [DOI] [PubMed] [Google Scholar]
- 4.Kushi LH, Byers T, Doyle C, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006;56:254–81. doi: 10.3322/canjclin.56.5.254. quiz 313−4. [DOI] [PubMed] [Google Scholar]
- 5.American Heart Association Step I, Step II, and TLC diets. 2007. [20 December 2007]. Internet: http://www.americanheart.org/presenter.jhtml?identifier=4764.
- 6.Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148–98. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- 7.Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082–90. doi: 10.1056/NEJMoa022207. [DOI] [PubMed] [Google Scholar]
- 8.Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293:43–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 9.Aude YW, Agatston AS, Lopez-Jimenez F, et al. The national cholesterol education program diet vs a diet lower in carbohydrates and higher in protein and monounsaturated fat: a randomized trial. Arch Intern Med. 2004;164:2141–6. doi: 10.1001/archinte.164.19.2141. [DOI] [PubMed] [Google Scholar]
- 10.Westman EC, Yancy WS, Edman JS, Tomlin KF, Perkins CE. Effect of 6-month adherence to a very low carbohydrate diet program. Am J Med. 2002;113:30–6. doi: 10.1016/s0002-9343(02)01129-4. [DOI] [PubMed] [Google Scholar]
- 11.McManus K, Antinoro L, Sacks F. A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, low-energy diet for weight loss in overweight adults. Int J Obes Relat Metab Disord. 2001;25:1503–11. doi: 10.1038/sj.ijo.0801796. [DOI] [PubMed] [Google Scholar]
- 12.Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–7. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- 13.Atkins R. Dr. Atkins' new diet revolution. Quill; New York, NY: 2002. [Google Scholar]
- 14.Ornish D. Eat More, Weigh Less: Dr. Dean Ornish's life choice program for losing weight safely while eating abundantly. 1st ed Quill; New York, NY: 2001. [Google Scholar]
- 15.Acquista A, Vandermolen LA. The Mediterranean prescription: meal plans and recipes to help you stay slim and healthy for the rest of your life. Ballantine Books; New York, NY: 2006. [Google Scholar]
- 16.Agatston A. The South Beach diet: the delicious, doctor-designed, foolproof plan for fast and healthy weight loss. Random House; New York, NY: 2003. [Google Scholar]
- 17.Sears B. The zone: a revolutionary life plan to put your body in total balance for permanent weight loss. HarperCollins; New York, NY: 1995. [Google Scholar]
- 18.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159:285–93. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 19.Obarzanek E, Sacks FM, Vollmer WM, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hyper-tension (DASH) Trial. Am J Clin Nutr. 2001;74:80–9. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- 20.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 21.Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsatu-rated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–64. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 22.Karanja NM, Obarzanek E, Lin PH, et al. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc. 1999;99(suppl):S19–27. doi: 10.1016/s0002-8223(99)00412-5. [DOI] [PubMed] [Google Scholar]
- 23.Sears B. Zone-perfect meals in minutes. HarperCollins; New York, NY: 1997. [Google Scholar]
- 24.Wright JD, Wang CY, Kennedy-Stephenson J, Ervin RB. Dietary intake of ten key nutrients for public health, United States: 1999−2000. Adv Data. 2003;334:1–4. [PubMed] [Google Scholar]
- 25.Institute of Medicine . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academies Press; Washington, DC: 2002/2005. Panel on Macronutrients and Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary fats: total fat and fatty acids. pp. 542–88. [Google Scholar]
- 26.Institute of Medicine . Dietary reference intakes for energy, carboyhdrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academies Press; Washington, DC: 2002/2005. Panel on Macronutrients and Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Cholesterol. pp. 589–768. [Google Scholar]
- 27.Yancy WS, Jr, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. 2004;140:769–77. doi: 10.7326/0003-4819-140-10-200405180-00006. [DOI] [PubMed] [Google Scholar]
- 28.Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA. 2007;297:969–77. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 29.Korzenik JR. Case closed? Diverticulitis: epidemiology and fiber. J Clin Gastroenterol. 2006;40(suppl):S112–6. doi: 10.1097/01.mcg.0000225503.59923.6c. [DOI] [PubMed] [Google Scholar]
- 30.Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166:285–93. doi: 10.1001/archinte.166.3.285. [DOI] [PubMed] [Google Scholar]
- 31.Willett WC, Stampfer MJ, Colditz GA, Rosner BA, Speizer FE. Relation of meat, fat, and fiber intake to the risk of colon cancer in a prospective study among women. N Engl J Med. 1990;323:1664–72. doi: 10.1056/NEJM199012133232404. [DOI] [PubMed] [Google Scholar]
- 32.Norat T, Bingham S, Ferrari P, et al. Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst. 2005;97:906–16. doi: 10.1093/jnci/dji164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao A, Thun MJ, Connell CJ, et al. Meat consumption and risk of colorectal cancer. JAMA. 2005;293:172–82. doi: 10.1001/jama.293.2.172. [DOI] [PubMed] [Google Scholar]
- 34.World Cancer Research Fund/American Institute for Cancer Research . Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR; Washington, DC: 2007. p. 537. [Google Scholar]
- 35.Brehm BJ, Seeley RJ, Daniels SR, D'Alessio DA. A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. J Clin Endocrinol Metab. 2003;88:1617–23. doi: 10.1210/jc.2002-021480. [DOI] [PubMed] [Google Scholar]
- 36.Samaha FF, Iqbal N, Seshadri P, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003;348:2074–81. doi: 10.1056/NEJMoa022637. [DOI] [PubMed] [Google Scholar]
- 37.McAuley KA, Hopkins CM, Smith KJ, et al. Comparison of high-fat and high-protein diets with a high-carbohydrate diet in insulin-resistant obese women. Diabetologia. 2005;48:8–16. doi: 10.1007/s00125-004-1603-4. [DOI] [PubMed] [Google Scholar]
- 38.Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. 2004;140:778–85. doi: 10.7326/0003-4819-140-10-200405180-00007. [DOI] [PubMed] [Google Scholar]
- 39.McAuley KA, Smith KJ, Taylor RW, McLay RT, Williams SM, Mann JI. Long-term effects of popular dietary approaches on weight loss and features of insulin resistance. Int J Obes (Lond) 2006;30:342–9. doi: 10.1038/sj.ijo.0803075. [DOI] [PubMed] [Google Scholar]
- 40.Tay J, Brinkworth GD, Noakes M, Keogh J, Clifton PM. Metabolic effects of weight loss on a very-low-carbohydrate diet compared with an isocaloric high-carbohydrate diet in abdominally obese subjects. J Am Coll Cardiol. 2008;51:59–67. doi: 10.1016/j.jacc.2007.08.050. [DOI] [PubMed] [Google Scholar]
- 41.Halton TL, Willett WC, Liu S, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med. 2006;355:1991–2002. doi: 10.1056/NEJMoa055317. [DOI] [PubMed] [Google Scholar]
- 42.Elliott P, Stamler J, Dyer AR, et al. Association between protein intake and blood pressure: the INTERMAP Study. Arch Intern Med. 2006;166:79–87. doi: 10.1001/archinte.166.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boden G, Chen X, Ruiz J, White JV, Rossetti L. Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest. 1994;93:2438–46. doi: 10.1172/JCI117252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Due A, Toubro S, Skov AR, Astrup A. Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord. 2004;28:1283–90. doi: 10.1038/sj.ijo.0802767. [DOI] [PubMed] [Google Scholar]
- 45.Institute of Medicine . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academies Press; Washington, DC: 2002/2005. Panel on Macronutrients and Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Protein and amino acids. [Google Scholar]
- 46.Reddy ST, Wang CY, Sakhaee K, Brinkley L, Pak CY. Effect of low-carbohydrate high-protein diets on acid-base balance, stone-forming propensity, and calcium metabolism. Am J Kidney Dis. 2002;40:265–74. doi: 10.1053/ajkd.2002.34504. [DOI] [PubMed] [Google Scholar]
- 47.Carter JD, Vasey FB, Valeriano J. The effect of a low-carbohydrate diet on bone turnover. Osteoporos Int. 2006;17:1398–403. doi: 10.1007/s00198-006-0134-x. [DOI] [PubMed] [Google Scholar]
- 48.Kerstetter JE, O'Brien KO, Caseria DM, Wall DE, Insogna KL. The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab. 2005;90:26–31. doi: 10.1210/jc.2004-0179. [DOI] [PubMed] [Google Scholar]
- 49.Dawson-Hughes B, Harris SS, Rasmussen H, Song L, Dallal GE. Effect of dietary protein supplements on calcium excretion in healthy older men and women. J Clin Endocrinol Metab. 2004;89:1169–73. doi: 10.1210/jc.2003-031466. [DOI] [PubMed] [Google Scholar]
- 50.Curhan GC, Willett WC, Knight EL, Stampfer MJ. Dietary factors and the risk of incident kidney stones in younger women: Nurses' Health Study II. Arch Intern Med. 2004;164:885–91. doi: 10.1001/archinte.164.8.885. [DOI] [PubMed] [Google Scholar]
- 51.Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. 2004;15:3225–32. doi: 10.1097/01.ASN.0000146012.44570.20. [DOI] [PubMed] [Google Scholar]
- 52.Knight EL, Stampfer MJ, Hankinson SE, Spiegelman D, Curhan GC. The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med. 2003;138:460–7. doi: 10.7326/0003-4819-138-6-200303180-00009. [DOI] [PubMed] [Google Scholar]
- 53.Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med. 2002;113(suppl 9B):47S–59S. doi: 10.1016/s0002-9343(01)00992-5. [DOI] [PubMed] [Google Scholar]
- 54.Estruch R, Martinez-Gonzalez MA, Corella D, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 55.Keys A, Menotti A, Karvonen MJ, et al. The diet and 15-year death rate in the seven countries study. Am J Epidemiol. 1986;124:903–15. doi: 10.1093/oxfordjournals.aje.a114480. [DOI] [PubMed] [Google Scholar]
- 56.Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: the Women's Health Initiative Dietary Modification Trial. JAMA. 2006;295:39–49. doi: 10.1001/jama.295.1.39. [DOI] [PubMed] [Google Scholar]
- 57.Howard BV, Van Horn L, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–66. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 58.Prentice RL, Thomson CA, Caan B, et al. Low-fat dietary pattern and cancer incidence in the Women's Health Initiative Dietary Modification Randomized Controlled Trial. J Natl Cancer Inst. 2007;99:1534–43. doi: 10.1093/jnci/djm159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prentice RL, Caan B, Chlebowski RT, et al. Low-fat dietary pattern and risk of invasive breast cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:629–42. doi: 10.1001/jama.295.6.629. [DOI] [PubMed] [Google Scholar]
- 60.Beresford SA, Johnson KC, Ritenbaugh C, et al. Low-fat dietary pattern and risk of colorectal cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:643–54. doi: 10.1001/jama.295.6.643. [DOI] [PubMed] [Google Scholar]
- 61.Marshall JA, Bessesen DH, Hamman RF. High saturated fat and low starch and fibre are associated with hyperinsulinaemia in a non-diabetic population: the San Luis Valley Diabetes Study. Diabetologia. 1997;40:430–8. doi: 10.1007/s001250050697. [DOI] [PubMed] [Google Scholar]
- 62.Mayer-Davis EJ, Monaco JH, Hoen HM, et al. Dietary fat and insulin sensitivity in a triethnic population: the role of obesity. The Insulin Resistance Atherosclerosis Study (IRAS). Am J Clin Nutr. 1997;65:79–87. doi: 10.1093/ajcn/65.1.79. [DOI] [PubMed] [Google Scholar]
- 63.Vessby B, Karlstrom B, Ohrvall M, Jarvi A, Andersson A, Basu S. Diet, nutrition and diabetes mellitus. Ups J Med Sci. 2000;105:151–60. doi: 10.1517/03009734000000061. [DOI] [PubMed] [Google Scholar]
- 64.Feskens EJ, Loeber JG, Kromhout D. Diet and physical activity as determinants of hyperinsulinemia: the Zutphen Elderly Study. Am J Epidemiol. 1994;140:350–60. doi: 10.1093/oxfordjournals.aje.a117257. [DOI] [PubMed] [Google Scholar]
- 65.van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB. Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care. 2002;25:417–24. doi: 10.2337/diacare.25.3.417. [DOI] [PubMed] [Google Scholar]
- 66.Wolever TM, Mehling C. Long-term effect of varying the source or amount of dietary carbohydrate on postprandial plasma glucose, insulin, triacylglycerol, and free fatty acid concentrations in subjects with impaired glucose tolerance. Am J Clin Nutr. 2003;77:612–21. doi: 10.1093/ajcn/77.3.612. [DOI] [PubMed] [Google Scholar]
- 67.Wolk A, Bergstrom R, Hunter D, et al. A prospective study of association of monounsaturated fat and other types of fat with risk of breast cancer. Arch Intern Med. 1998;158:41–5. doi: 10.1001/archinte.158.1.41. [DOI] [PubMed] [Google Scholar]
- 68.Martin-Moreno JM, Willett WC, Gorgojo L, et al. Dietary fat, olive oil intake and breast cancer risk. Int J Cancer. 1994;58:774–80. doi: 10.1002/ijc.2910580604. [DOI] [PubMed] [Google Scholar]
- 69.Holmes MD, Hunter DJ, Colditz GA, et al. Association of dietary intake of fat and fatty acids with risk of breast cancer. JAMA. 1999;281:914–20. doi: 10.1001/jama.281.10.914. [DOI] [PubMed] [Google Scholar]
- 70.Schuurman AG, van den Brandt PA, Dorant E, Brants HA, Goldbohm RA. Association of energy and fat intake with prostate carcinoma risk: results from The Netherlands Cohort Study. Cancer. 1999;86:1019–27. [PubMed] [Google Scholar]
- 71.Veierod MB, Laake P, Thelle DS. Dietary fat intake and risk of prostate cancer: a prospective study of 25,708 Norwegian men. Int J Cancer. 1997;73:634–8. doi: 10.1002/(sici)1097-0215(19971127)73:5<634::aid-ijc4>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 72.Parks EJ, Hellerstein MK. Carbohydrate-induced hypertriacylglycerolemia: historical perspective and review of biological mechanisms. Am J Clin Nutr. 2000;71:412–33. doi: 10.1093/ajcn/71.2.412. [DOI] [PubMed] [Google Scholar]
- 73.Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336:129–33. doi: 10.1016/0140-6736(90)91656-u. [DOI] [PubMed] [Google Scholar]
- 74.Davis BC, Kris-Etherton PM. Achieving optimal essential fatty acid status in vegetarians: current knowledge and practical implications. Am J Clin Nutr. 2003;78(suppl):640S–6S. doi: 10.1093/ajcn/78.3.640S. APPENDIX: Creating 7-d menu plans. [DOI] [PubMed] [Google Scholar]