Abstract
One-stage hip arthroplasty and contralateral core decompression with bone grafting were performed for 30 patients with bilateral femoral head osteonecrosis between April 2002 and June 2005. The treatment course, clinical and radiographic outcomes, and medical costs were compared with another 30 age-, gender-, etiology-, and disease extent-matched patients undergoing two-stage treatment during the same period. The two groups had similar clinical data and few complications. Total hospital stay and associated costs were reduced for patients who had one-stage treatment. These patients also returned to work faster (6.0 versus 10.8 months). At an average followup of 46 months, progression to greater than 2 mm of collapse of the salvaged femoral head was observed in seven patients (23%) who had one-stage treatment and 14 patients (47%) who had two-stage treatment. Conversion to hip arthroplasty was performed in five patients (17%) in the one-stage group and 12 patients (40%) in the two-stage group. A special group of patients with bilateral osteonecrosis of the femoral head seemed to benefit from one-stage hip arthroplasty and contralateral core decompression with bone grafting and had better survival of the salvaged femoral head. One-stage hip arthroplasty and core decompression with bone grafting proved to be a cost-effective method that did not increase perioperative morbidity.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Osteonecrosis of the femoral head (ONFH) often is diagnosed in young patients [14]. It is known to have a natural history of progressive necrosis leading to subchondral fracture and collapse of the femoral head, and subsequent degenerative arthritis of the hip [10, 17]. The main goal in treating ONFH is to preserve the femoral head. Unfortunately, most patients with ONFH first present to an orthopaedic surgeon after the disease already is advanced. Once the femoral head has collapsed, hip arthroplasty (HA) is the procedure with the highest likelihood of success [9, 14]. Various procedures have been used to preserve the femoral head, including core decompression [4, 24], osteotomies [27], and various forms of free vascularized [1, 28, 29] or nonvascularized bone grafting (BG) [2, 3, 15, 19–23]. Most treatment modalities have difficulty in successfully preserving the femoral head.
Osteonecrosis of the femoral head often occurs bilaterally. Prevalence of bilateral involvement has been reported to be as much as 78% [13, 26]. An unusual situation occurs when the patient presents with ONFH on one side that may require HA (Stage IV according to Steinberg et al. [25] with greater than 2 mm collapse), whereas the other less symptomatic or asymptomatic side also has ONFH that may be saved via a femoral head-preserving procedure (≤ Stage III). Theoretically, treatment for the less symptomatic or asymptomatic side (head-preserving procedure) should be prioritized over the advanced side (HA), or at least, bilateral surgery should be performed simultaneously. However, patients often query why the orthopaedic surgeon does not perform surgery on the symptomatic side first or are concerned by the surgical risk of one-stage bilateral surgery, and some patients refuse surgery on the asymptomatic side.
Despite interest in surgical outcomes for patients with ONFH, we are not aware of any report in the English literature estimating surgical risks and outcomes of this group of patients after one-stage HA and contralateral side femoral head-preserving procedures (core decompression with BG). We hypothesized bilateral hip surgery during one anesthesia would benefit these patients. To determine the effectiveness and safety of one-stage bilateral surgery, the specific questions addressed in this investigation included whether one-stage bilateral hip surgery decreased risk of disease progression, increased surgical risk for the patient, reduced medical costs and shortened rehabilitation time, enhanced the healing process of the femoral head-preserving procedure, and had better functional results compared with those of patients undergoing two-stage surgery.
Materials and Methods
During a preliminary study, only two of 10 patients who had one-stage surgery had greater than 2 mm collapse at followup. Our previous experience showed that greater than 50% of patients having core decompression and allografting had greater than 2 mm collapse at followup. A power calculation was performed using a confidence level of 95% and power (1 – β) of 90%. It was calculated that 52 subjects (26 patients in each group) were needed for this study. We thus prospectively followed 30 patients with simultaneous bilateral ONFH undergoing one-stage HA on one side and core decompression with BG on the contralateral hip between April 2002 and June 2005. The etiology was alcohol-induced in 17 patients (57%), steroid-induced in nine patients (30%), and idiopathic in four patients (13%). Another 30 age-, gender-, etiology-, and disease extent-matched patients undergoing two-stage surgery during this period comprised the comparison group. The intervals between each stage of surgery ranged from 6 weeks to 4 months (mean, 9 weeks) in the two-stage group. Data collected included age, gender, body weight and height, etiology, stage and extent of ONFH, American Society of Anesthesiologists (ASA) classification [12], dates and procedures for the index and subsequent surgeries, operating time, estimated blood loss, length of hospital stay, total costs and their distribution, and complications (Table 1). No statistical difference was found in demographic variables. The patients were followed for a minimum of 2 years, with no patients lost to followup. The mean followup was 45 months (range, 26–64 months) for the one-stage group and 46 months (range, 26–65 months) for the two-stage group.
Table 1.
Comparison of demographic data
| Data | One-stage surgery (n = 30) | Two-stage surgery (n = 30) | p value |
|---|---|---|---|
| Age (years) | 40 ± 9 | 40 ± 11 | 0.99 |
| Gender (male:female) | 23:7 | 23:7 | 1 |
| Body weight (kg) | 66 ± 11 | 67 ± 10 | 0.84 |
| Body height (cm) | 165 ± 8 | 167 ± 9 | 0.80 |
| Blood loss (mL) | 450 ± 130 | 500 ± 145 | 0.15 |
| Operation time (minutes) | 185 ± 36 | 200 ± 22 | 0.07 |
| Hospital stay (days) | 6.9 ± 0.8 | 12.9 ± 1.8 | < 0.001 |
| Complications | 1/30 | 2/30 | 0.38 |
| Costs (USD) | |||
| Total | 3823 ± 107 | 4392 ± 138 | < 0.001 |
| Pharmacy + ward | 389 ± 79 | 710 ± 104 | < 0.001 |
| Laboratory + radiology | 370 ± 15 | 537 ± 6 | < 0.001 |
| Anesthesia | 354 ± 67 | 365 ± 64 | 0.54 |
| Operating room | 2710 ± 40 | 2780 ± 80 | 0.002 |
| Return to work (months) | 6.0 ± 1.6 | 10.8 ± 2.4 | < 0.001 |
| Followup (months) | 45 ± 11 | 46 ± 11 | 0.93 |
Data are expressed as mean ± standard deviation.
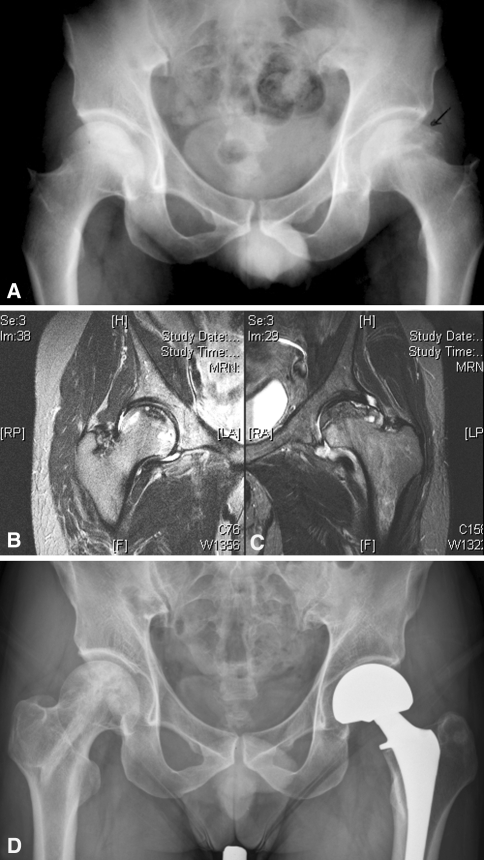
Preoperatively, anteroposterior and frog-leg lateral radiographs of the pelvis were taken (Fig. 1A). In addition, MRI was performed on each patient and used to accurately stage each hip (Fig. 1B). The ONFH stage was classified according to the University of Pennsylvania classification and staging system (Table 2) [25]. The percentage of femoral head involvement on MRI was calculated by approximating the average areas of abnormality seen on serial MRI cuts. All MR images were viewed by an individual (YCW) who was blinded to the results. The extent of femoral head involvement was classified as A (< 15%), B (15%–30%), and C (> 30%). Indications for HA included ONFH at Stage IV with greater than 2 mm collapse of the femoral head or ONFH with degenerative changes in the acetabulum. According to the regulations of the National Health Bureau of Taiwan, bipolar HA was performed for Stage IV ONFH, and THA was chosen for Stage V or VI ONFH. An uncemented technique was used in all HAs. The indication for core decompression with BG was ONFH at Stage III or less.
Fig. 1A–D.
Radiographs are shown for a 32-year-old patient with left hip pain. (A) A preoperative radiograph of the pelvis shows collapse of the right femoral head, and MR images show (B) right and (C) left femoral head involvement. (D) A radiograph taken 49 months after one-stage HA and contralateral side core decompression with BG shows a well-preserved right femoral head and preserved articular space and a well-fixed bipolar prosthesis in the left hip.
Table 2.
Comparison of radiographic staging
| Steinberg stage [25] | Number of patients | |||
|---|---|---|---|---|
| Initial | Followup | |||
| One-stage | Two-stage | One-stage | Two-stage | |
| IB | 2 | 2 (2)* | 2 | 2 |
| IIA | 3 | 3 (2) | 3 | 2 |
| IIB | 6 | 6 (4) | 6 | 3 |
| IIC | 10 | 10 (10) | 7 | 2 |
| IIIC | 9 | 9 (12) | 5 | 7 |
| IV | 5 | 10 | ||
| V | 2 | 4 | ||
*Data are presented as number of patients at diagnosis, with total number of patients at the staged bone-grafting procedure in parentheses.
All surgery was performed by two surgeons (LYS, HNS). For one-stage surgery, the HA was performed first. Autogenous bone was harvested from the resected femoral head, neck, and proximal femur after excising the necrotic bone. Thirty milliliters of bone marrow was aspirated from the ipsilateral iliac crest, mixed with the autograft, and temporarily stored in a sterile culture tube at 4°C. The patient then was placed in a supine position on a fracture table. Core decompression with BG was performed using the technique described by Phemister [19]. Briefly, a guide pin was placed precisely into the osteonecrotic area from the lateral cortex of the femur under fluoroscopic guidance and a core (12–14 mm) was made. Biopsy specimens were obtained to confirm the diagnosis. The necrotic bone was removed thoroughly using an angled curette (Fig. 2A), and the defect was packed tightly with bone marrow-soaked fresh autografts. An allogenous cortical strut then was inserted into the core tract to within 5 to 10 mm of the subchondral area (Fig, 2B). For two-stage surgery, the same procedure was performed except that the defect after débridement was replaced with morselized frozen autografts (if HA was performed first) or allografts (if core decompression with BG was performed first).
Fig. 2A–B.
The technique used for core decompression and bone grafting is shown. (A) An intraoperative fluoroscope shows the angled curette used to remove necrotic bone from the superoanterior femoral head. (B) A postoperative radiograph shows adequate debridement and bone grafting at the superoanterior femoral head and good position of supportive cortical strut.
Postoperatively, the patient was restricted to nonweightbearing on the BG side and partial weightbearing on the HA side for 6 weeks. The patients used crutches with nonweightbearing for another 6 weeks and began gradual weightbearing after 3 to 6 months on the BG side, depending on lesion stage and extent. Patients were evaluated preoperatively, at 6-week intervals for the first 3 months after surgery, at 3-month intervals for 2 years, and annually thereafter. During followup, each patient was examined for range of motion, gait, and pain using the Harris hip scoring system [6], with 90 to 100 points indicating an excellent outcome, 80 to 89 points a good outcome, 70 to 79 points a fair outcome, and less than 70 points a poor outcome. Radiographs, including anteroposterior and frog-leg lateral views of the pelvis, were taken at each visit and evaluated by a radiologist with no information regarding the clinical data, treatment, and outcomes. The degree of collapse was measured using a plastic template with Mose concentric circles [16].
Statistical analysis was performed using the SPSS for Windows statistical package (Version 10.0; SPSS Inc, Chicago, IL). Operating time, estimated blood loss, duration of hospital stay, complications, and outcomes were compared. Hospital expenses, including costs for surgery, anesthesia, laboratory (including radiology), and ward (including pharmacy and nursing) also were calculated. Variables were analyzed using Student’s t test for continuous data, Mann-Whitney U test for nonparametric data, and Fisher’s exact test or chi square test for nominal data. Kaplan-Meier analysis was used to compare radiographic signs of progression to collapse of the femoral head between one-stage and two-stage groups. Significance was defined as p < 0.05.
Results
Two-stage surgery significantly increased (p = 0.026) the risk of worsening the stage or extent of ONFH. Progression of the stage and/or extent of the hips occurred in five patients in the two-stage group owing to a time lag for the femoral head-preserving procedure (HA was performed first because patients initially refused the femoral head-preserving procedure).
One-stage bilateral hip surgery did not increase surgical risk compared with two-stage surgery. Operating time and estimated blood loss did not differ between patients in the two-stage and one-stage groups (Table 1). Overall, there were few complications related to HA or core decompression with BG. One patient in the one-stage group had calcar splitting during insertion of a bipolar prosthesis and was treated successfully using cable wiring. One patient in the two-stage group had atelectasis of the lung, and another patient in the two-stage group had dysuria. Administration of appropriate medical care was successful in both cases. No mortality occurred.
One-stage bilateral surgery significantly reduced medical costs and shortened rehabilitation time compared with two-stage surgery. Patients receiving one-stage surgery had shorter overall hospital stays (p < 0.001) than those undergoing two-stage surgery. Treatment costs also were less (p < 0.001) for patients who had one-stage surgery (mean ± standard deviation, $3823 ± $107 [USD] versus $4392 ± $138 [USD]). Not only were costs related to bed utilization reduced, as might be expected, but laboratory (including radiology), pharmacy, and nursing costs also were reduced (p < 0.001). Patients who had one-stage surgery returned to work at an average of 6.0 months after surgery, which was faster (p < 0.001) than patients who had two-stage surgery (10.8 months).
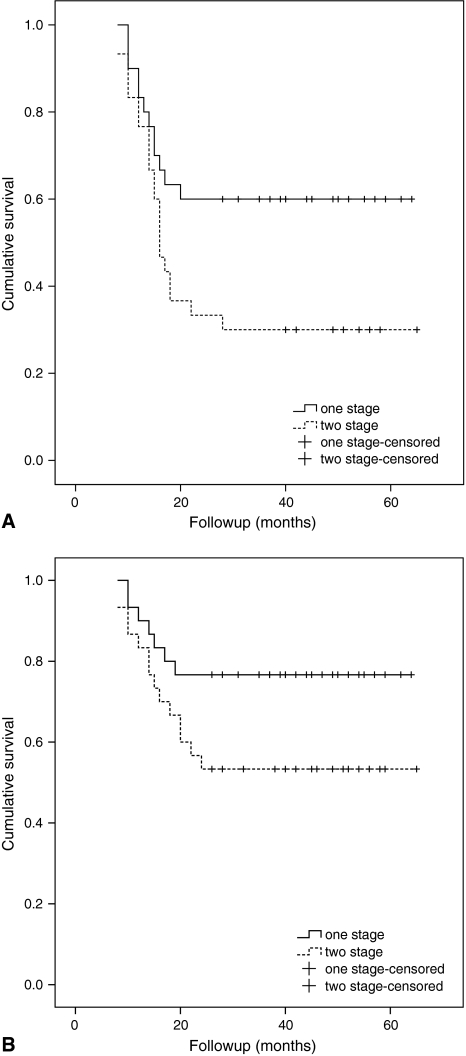
One-stage bilateral surgery enhanced the healing power of the head preserving procedure and had fewer femoral head collapses. At latest followup, radiographic evaluation revealed no progression of ON after core decompression with BG in 18 (60%) patients in the one-stage (Fig. 3A) and nine (30%) patients in the two-stage groups; progression in stage and/or extent (< 2 mm collapse) with minimal or mild symptoms in five (17%) patients in the one-stage and seven (23%) patients in the two-stage groups; and progression to collapse in seven (23%) patients in the one-stage and 14 (47%) patients in the two-stage groups. The rate of greater than 2 mm collapse of the femoral head was higher (p = 0.04) in the two-stage group. Survival analysis with radiographic signs of greater than 2 mm collapse as an end point showed a difference (log-rank test, p = 0.07) (Fig. 3B) between the two groups. The stage and extent of ONFH at surgery were associated with (p < 0.001) the occurrence of radiographic progression to collapse. Overall, 17 (81%) of the 21 patients with Stage IIIC ONFH showed progressive collapse of the femoral head.
Fig. 3A–B.
Survival curves for one-stage (solid line) and two-stage surgery groups (dashed line) show better survival of the head preserving procedure in the one-stage group. (A) Any progression of stage was used as the end point in the survival curve. (B) When greater than 2 mm collapse of the femoral head (Steinberg [25] Stage IV) was used as the end point in the survival analysis, the one stage group exhibited less collapse than the two stage group.
One-stage bilateral surgery had better clinical results of the head preserving procedure. Conversion of the femoral head-preserving procedure to HA was performed in five (17%) patients in the one-stage and 12 (40%) patients in the two-stage groups. The rate of conversion to HA was greater in the two-stage group (p = 0.03). Again, the stage and extent of ONFH at surgery were associated (p < 0.001) with the need for conversion to HA. Overall, 16 of 21 (76%) patients with Stage IIIC osteonecrotic hips had conversion surgery to HA during the study. At most recent followup, no loosening or revision of the hip prostheses in either groups was observed. The clinical outcome showed 20 of 25 (80%) patients in the one-stage and 13 of 18 (72%) patients in the two-stage groups had good to excellent results on the hip that had core decompression with BG. Harris hip scores improved from a mean of 77 points (range, 64–100 points) to 90 points (range, 68–100 points) for the femoral head-preserving side and 51 points (range, 35–62 points) to 94 points (range, 88–98 points) for the HA side in patients in the one-stage group and improved from 75 points (range, 60–100 points) to 88 points (range, 65–100 points) for the femoral head-preserving side and 50 points (range, 37–64 points) to 95 points (range, 89–98 points) for the HA side in patients in the two-stage group.
Discussion
We compared the courses, clinical and radiographic results, complications, and treatment costs for patients treated for bilateral ONFH with one-stage surgery versus two-stage surgery. Our results suggest patients with bilateral ONFH benefit from one-stage HA and contralateral side core decompression with BG, with better survival of the salvaged femoral head. One-stage surgery reduces total costs and shortens the rehabilitation period compared with two-stage surgery, without increasing perioperative morbidity.
Our study has some limitations. First, our study involved a relatively small number of patients. Second, the described techniques are applicable only to a very specific group of patients. The effect of bone marrow implantation (discussed below) also needs to be studied further. The MRI staging was made by a radiologist blinded to the results. Although the reading showed excellent agreement (full agreement, 56/60; 93%) with the clinical staging, no statistical test was done. A minimum followup of 2 years was chosen in this study because collapse of the femoral head generally occurs during this time span [13, 17]. However, a longer followup is required to determine whether one-stage surgery ultimately improves outcomes of the femoral head-preserving procedure.
One-stage bilateral hip surgery is a reasonable alternative to two-stage unilateral surgery provided the benefits are not jeopardized by increased perioperative morbidity. The benefits of one-stage surgery include diminished complication risk related to anesthesia, decreased hospitalization, and reduced costs [11]. However, one-stage bilateral surgery can be expected to produce more blood loss, longer operation time, and more complications compared with a unilateral procedure. Our study confirmed there are few complications related to HA or core decompression with BG, and one-stage bilateral surgery does not increase overall perioperative morbidity compared with two-stage unilateral hip surgery.
Another key advantage of one-stage surgery is cost efficiency. The rationale for one-stage surgery is to improve postoperative rehabilitation and decrease overall hospital stay and associated costs. It has been well established that many patients do not experience functional improvement until both hip problems have been resolved [11]. Although rehabilitation was demanding and difficult, the patients who had one-stage surgery in our study returned to work faster than patients who had two-stage surgery. There was a total cost reduction of $569 (USD) per case. The absolute number is small because of generalized low medical costs in Taiwan. However, this figure represents a 15% reduction of total costs, which is undoubtedly significant. The cost reduction derives from reductions in ward costs, nursing care, pharmacy, and radiographic examination.
The main goals of treating ONFH with a femoral head-preserving procedure are pain relief, maintaining a congruent hip, and delaying the need for HA as long as possible. When ONFH is diagnosed in young patients, it is advisable to perform the most conservative possible surgical procedure, with the knowledge that a future intervention may be necessary [9, 14]. Surgery that involves a high complication rate or morbidity or that compromises subsequent THA should be avoided [9]. Nonvascularized BG through a core decompression tract from the greater trochanter is more appealing than vascularized or nonvascularized BG through the femoral neck or the joint for this group of patients because this procedure is less invasive and requires less technical expertise. This procedure has very low morbidity, requires a mean surgical time less than 1 hour with limited blood loss, and does not increase perioperative morbidity of one-stage surgery.
Managing ON of the contralateral femoral head using the currently reported procedure at one stage is based on the following rationales: (1) decompression of the femoral head, (2) removal of the necrotic bone, (3) replacement with fresh autografts, (4) support of the subchondral bone with a strong bone strut, and (5) enhancement of bone healing and incorporation by use of autogenous bone and marrow graft. The success of the procedure is attributed to the following factors. First, the most symptomatic hip was treated and the femoral head-preserving procedure was performed at the earliest possible time in one stage. As seen for some patients who had two-stage surgery, the stage and/or extent of ONFH progressed during the time between the two stages of surgery when the patient underwent HA first, or there was deterioration of the femoral head attributable to the patient bearing more weight during recovery when the femoral head-preserving procedure was done first. One-stage surgery avoided the unnecessary delay of the head-preserving procedure. Second, fresh cancellous autograft tightly packed into the subchondral area provided support and living cells necessary for bone healing in patients who had one-stage surgery. One-stage surgery offered a distinct advantage over two separate operations in that the femoral neck and proximal femur obtained during the first procedure could be used as fresh autografts. Using autografts instead of allografts or frozen autografts is appealing as fresh cancellous autografts lead to rapid healing and subsequent restoration of structural support for the subchondral plate and overlying cartilage [18]. Finally, the efficacy of fresh autografts might be augmented via the addition of bone marrow. A decrease of osteogenic stem cells in the proximal femur of patients with ONFH has been reported [8]. Bone marrow grafting may provide the osteoprogenitors necessary for bone healing. Hernigou and Beaujean [7] and Gangji et al. [5] reported good results of treating precollapse ON with core decompression and autologous bone marrow grafting. In our study, 30 mL of bone marrow mixed with autologous bone was used to replace the bone defect. Whether the addition of this small amount of bone marrow enhanced bone healing in patients who had one-stage surgery requires further examination. However, it seems logical to add more osteogenic cells to the graft to accelerate bone healing and incorporation.
Our study showed patients with bilateral ONFH appeared to benefit from one-stage HA and contralateral core decompression with BG and had better survival of the salvaged femoral head. One-stage surgery proved to be a cost-effective method that did not increase perioperative morbidity.
Acknowledgment
We thank Ted Knoy for editorial assistance.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:987–993. [DOI] [PubMed]
- 2.Buckley PD, Gearen PF, Petty RW. Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1991;73:1357–1364. [PubMed]
- 3.Dunn AW, Grow T. Aseptic necrosis of the femoral head: treatment with bone grafts of doubtful value. Clin Orthop Relat Res. 1977;122:249–254. [PubMed]
- 4.Fairbank AC, Bhatia D, Jinnah RH, Hungerford DS. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42–49. [PubMed]
- 5.Gangji V, Hauzeur JP, Matos C, De Maertelaer V, Toungouz M, Lambermont M. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells: a pilot study. J Bone Joint Surg Am. 2004;86:1153–1160. [DOI] [PubMed]
- 6.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 7.Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;405:14–23. [DOI] [PubMed]
- 8.Hernigou P, Beaujean F, Lambotte JC. Decrease of mesenchymal stem-cell pool in the proximal femur in corticosteroid-induced osteonecrosis. J Bone Joint Surg Br. 1999;81:349–355. [DOI] [PubMed]
- 9.Hungerford DS. Treatment of osteonecrosis of the femoral head: everything’s new. J Arthroplasty. 2007;22(4 suppl 1):91–94. [DOI] [PubMed]
- 10.Jergesen HE, Khan AS. The natural history of untreated asymptomatic hips in patients who have non-traumatic osteonecrosis. J Bone Joint Surg Am. 1997;79:359–363. [DOI] [PubMed]
- 11.Jergesen HE, Poss R, Sledge CB. Bilateral total hip and knee replacement in adults with rheumatoid arthritis: an evaluation of function. Clin Orthop Relat Res. 1978;137:120–128. [PubMed]
- 12.Keats AS. The ASA classification of physical status: a recapitulation. Anesthesiology. 1978;49:233–236. [DOI] [PubMed]
- 13.Lee MS, Chang YH, Chao EK, Shih CH. Conditions before collapse of the contralateral hip in osteonecrosis of the femoral head. Chang Gung Med J. 2002;25:228–237. [PubMed]
- 14.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, Urbaniak JR. Osteonecrosis of the hip: management in the 21st century. J Bone Joint Surg Am. 2002;84:834–853. [PubMed]
- 15.Mont MA. Einhorn TA, Sponseller PD, Hungerford DS. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br. 1998;80:56–62. [DOI] [PubMed]
- 16.Mose K. Methods of measuring in Legg-Calvé-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;150:103–109. [PubMed]
- 17.Ohzono K, Saito M, Takaoka K, Ono K, Saito S, Nishina T, Kadowaki T. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1991;73:68–72. [DOI] [PubMed]
- 18.Oklund SA, Prolo DJ, Gutierrez RV, King SE. Quantitative comparisons of healing in cranial fresh autografts, frozen autografts and processed autografts, and allografts in canine skull defects. Clin Orthop Relat Res. 1986;205:269–291. [PubMed]
- 19.Phemister DB. Treatment of the necrotic head of the femur in adults. J Bone Joint Surg Am. 1949;31:55–66. [PubMed]
- 20.Plakseychuk AY, Kim SY, Park BC, Varitimidis SE, Rubash HE, Sotereanos DG. Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:589–596. [DOI] [PubMed]
- 21.Rijnen WH, Gardeniers JW, Buma P, Yamano K, Slooff TJ, Schreurs BW. Treatment of femoral head osteonecrosis using bone impaction grafting. Clin Orthop Relat Res. 2003;417:74–83. [DOI] [PubMed]
- 22.Rosenwasser MP, Garino JP, Kiernan HA, Michelsen CB. Long term followup of thorough debridement and cancellous bone grafting of the femoral head for avascular necrosis. Clin Orthop Relat Res. 1994;306:17–27. [PubMed]
- 23.Smith KR, Bonfiglio M, Montgomery WJ. Non-traumatic necrosis of the femoral head treated with tibial bone-grafting: a follow-up note. J Bone Joint Surg Am. 1980;62:845–847. [PubMed]
- 24.Smith SW, Fehring TK, Grifflin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77:674–680. [DOI] [PubMed]
- 25.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41. [PubMed]
- 26.Sugano N, Takaoka K, Ohzono K, Matsui M, Masuhara K, Ono K. Prognostication of nontraumatic avascular necrosis of the femoral head: significance of location and size of the necrotic lesion. Clin Orthop Relat Res. 1994;303:155–164. [PubMed]
- 27.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head: indications and long-term results. Clin Orthop Relat Res. 1992;277:111–120. [PubMed]
- 28.Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting: a long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77:681–694. [DOI] [PubMed]
- 29.Urbaniak JR, Harvey EJ. Revascularization of the femoral head in osteonecrosis. J Am Acad Orthop Surg. 1998;6:44–54. [DOI] [PubMed]