Abstract
For successful TKA, good soft tissue balance is one of the most important factors; however, it is unknown whether the coronal balance immediately after surgery is maintained with time. We hypothesized, if neutral mechanical alignment was achieved at the time of TKA, some degree of lateral ligamentous laxity could be accepted and the laxity would diminish with time. To confirm this hypothesis, we posed two scientific questions: (1) Does the coronal ligament balance measured immediately after TKA change with time? (2) Does the degree of preoperative varus alignment correlate with the lateral or medial ligamentous laxity observed after TKA? We measured coronal lateral or medial ligamentous laxity in 71 knees with varus deformities immediately after surgery and at 3, 6, and 12 months thereafter. The mean mechanical axis was 15.9° varus preoperatively and 0.4° varus postoperatively. The mean medial ligamentous laxity was relatively constant postoperatively from immediately after surgery to 12 months. However, the mean lateral ligamentous laxity was as much as 8.6° immediately after surgery and decreased to 5.1° at 3 months. The lateral ligamentous laxity immediately after surgery correlated with the preoperative varus mechanical axis. Our data show residual lateral ligamentous laxity observed in preoperative varus deformity may be corrected spontaneously after TKA.
Introduction
Since the mid1970s, obtaining proper soft tissue balance has been recognized as one of the most important considerations in successful TKA [6, 9] because abnormal motion after TKA leads to increased early wear of polyethylene and a poor prognosis. In knees with little varus or valgus deformity, it is possible to create balance. However, in knees with a large deformity, achieving balance has been a challenging problem [25]. Also, even in normal knees, lateral ligamentous laxity and medial ligamentous laxity are not balanced. More lateral ligamentous laxity than medial ligamentous laxity has been observed [18, 23].
In general, Japanese people have a greater tendency for varus knee deformity than people in the United States and Europe [17]. Furthermore, owing to their reluctance to undergo surgery at an early stage, severe varus deformity is common by the time they visit the hospital.
In varus knees, the medial soft tissues, including the medial collateral ligament, generally are shortened, whereas the lateral soft tissues generally are lax and stretched preoperatively [7]. Therefore, to achieve equal soft tissue balance between the medial and lateral sides, one must release the medial soft tissue equal to the level of the lateral side. This large amount of medial release results in potential widening of the joint gap with elongation of the extremity and consequently patella baja. There are two strategies for adjusting the soft tissue balance in varus knees: (1) create equal medial and lateral gaps even for varus-deformed knees [7, 21, 24] and (2) accept some degree of lateral side laxity as long as proper valgus alignment is maintained [13, 19]. With the latter strategy, there is a possibility of residual lateral ligamentous laxity after surgery. We have observed many varus knees treated using the latter strategy exhibited lateral ligamentous laxity during and immediately after surgery. However, we typically observed no objective abnormal coronal laxity or subjective instability of the knee 1 year after surgery.
From these experiences, we hypothesized, if proper alignment was achieved by TKA, we could accept some degree of lateral ligamentous laxity at surgery, and the laxity would diminish with time. To confirm our hypothesis, we attempted to answer two questions: (1) Does coronal ligament balance measured immediately after TKA change with time? (2) Does the degree of preoperative varus alignment correlate with the lateral or medial ligamentous laxity observed after TKA?
Materials and Methods
We prospectively followed 71 patients (71 varus knees) undergoing primary TKA between July 2003 and December 2006. Among these, 55 patients had osteoarthritis (OA) and 16 had rheumatoid arthritis (RA). The patients ranged in age from 47 to 86 years (mean, 71 years). The mean weight, height, and body mass index of the patients were 57.4 kg (range, 41–88 kg), 150 cm (range, 136–167 cm), and 23.9 kg/m2 (range, 16.9–36.6 kg/m2), respectively. Ten of the 71 patients had body mass indices greater than 30 kg/m2. The minimum followup was 18 months (mean, 40 months; range, 18–57 months), and none was lost to followup.
The mechanical axis of the knee was determined on a preoperative standing weightbearing anteroposterior radiograph of the knee. The mean preoperative mechanical axis was 15.9° ± 6.5° varus (range, 5°–39° varus). The mean preoperative maximum flexion angle was 120° (range, 10°–150°). The mean preoperative flexion contracture was 14° (range, 0°–50°). The mean preoperative Knee Society score [8] was 56 points (range, 37–70 points). We used a Scorpio® NRG® (Stryker Howmedica Osteonics, Allendale, NJ) posterior-stabilized type of prosthesis in all knees. After bone cuts were made with an independent cut method, a 40-lb tensor was used in extension and 90° flexion, and release of the medial side soft tissue was conducted step by step. However, in varus knees, the lateral gap was far larger than the medial gap in many cases. In these cases, the medial release was terminated at the point when the medial gap reached 20 mm in extension and 90° flexion, thereby allowing residual lateral laxity.
Postoperative coronal laxity was assessed by stress radiographs of the knees using a Telos SE arthrometer (Fa Telos; Medizinisch-Technische, Greisheim, Germany) following a previously reported method [10, 11, 14, 25]. Anteroposterior radiographs were taken while the device was used. Valgus or varus forces of 7 kg to the knees were applied just above the joint on the lateral or medial femoral condyle, whereas the proximal thigh and middle leg were held by the counter supports at 15° flexion. On the stress radiographs, the angle between a line in contact with the bottom of the femoral prosthesis and a line in contact with the upper surface of the tibial prosthesis was measured. We defined this as the valgus angle or varus angle according to the description by Yagishita et al. [25]. These angles indicated the values of medial ligamentous laxity or lateral ligamentous laxity, respectively.
All measurements were taken in the operating room immediately after surgery and again at 3, 6, and 12 months postoperatively. We evaluated the differences between the varus/valgus angles immediately after surgery and at other postoperative times and also compared the differences between the values for knees with OA and RA. All data concerning the angles are presented as the mean ± standard deviation. To ascertain differences in the varus/valgus angles with stress tests (ie, laxity) among the various postoperative times, we used one-way repeated-measures ANOVA. The Bonferroni/Dunn test was used as the post hoc test. To evaluate the differences of the valgus or varus angle between knees with OA and those with RA, we used Student’s t test. In addition, we analyzed the correlations between the preoperative mechanical axis and the varus/valgus angles at the postoperative times. For analysis of the correlations, we used Pearson’s correlation coefficient test. For all analyses, we used SPSS® 12.0 (SPSS Inc, Chicago, IL).
Results
The mean postoperative flexion angle was 120° (range, 75°–145°), and the mean flexion contracture was 1.9° (range, 0°–30°). The mean postoperative mechanical axis was 0.4° ± 1.8° varus (range, 4° varus–4° valgus). The mean postoperative Knee Society score was 91.5 points (range, 78–99 points).
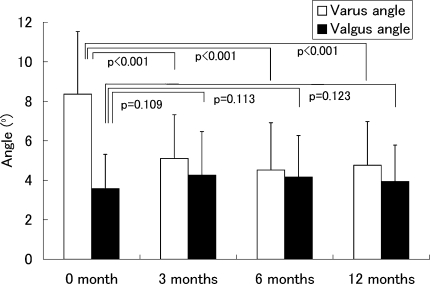
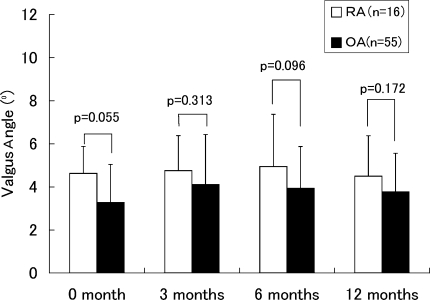
We observed no differences in the valgus angle among the various postoperative times (Fig. 1). The varus angle measured immediately after surgery was larger (p < 0.001) than those at other postoperative times (Fig. 1). No differences in valgus and varus angles were observed between knees with OA and those with RA at any of the postoperative times (Figs. 2, 3).
Fig. 1.
Mean values are shown for varus and valgus angles at various postoperative times. The errors bars represent one standard deviation. The varus angle immediately after surgery was greater than at 3, 6, and 12 months postoperatively. We found no difference between 3 months and 6 months, 6 months and 12 months, and 3 months and 12 months in varus or valgus angle.
Fig. 2.
Mean values are shown for the varus angle in RA and OA. The errors bars represent one standard deviation. We observed no differences between OA and RA at any of the times.
Fig. 3.
Mean values are shown for the valgus angle in RA and OA. The errors bars represent one standard deviation. We observed no differences between OA and RA at any of the times.
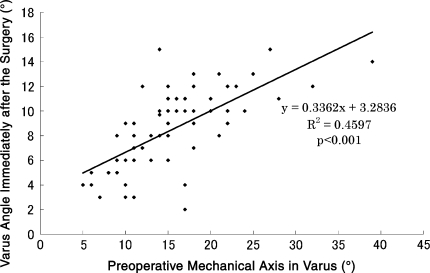
The varus angle immediately after surgery correlated (p < 0.001) with the preoperative mechanical axis (Fig. 4). We observed no correlations between the preoperative mechanical axis and the varus/valgus angles at the other postoperative times (data not shown).
Fig. 4.
This graph shows a comparison of the varus angle immediately after surgery and the preoperative mechanical axis in varus on a standing radiograph. We found a correlation between the degree of the preoperative varus deformity and the varus angle immediately after surgery.
Discussion
We have observed that many varus knees treated by TKA allowing residual lateral ligamentous laxity during the surgery had lateral ligamentous laxity immediately after TKA but had no objective abnormal coronal laxity or subjective instability of the knee 1 year after surgery. We hypothesized, if neutral mechanical alignment was achieved during TKA, some degree of lateral ligamentous laxity could be accepted and the laxity would diminish with time. To confirm this hypothesis, we posed two questions: (1) Does the coronal ligament balance measured immediately after TKA change with time? (2) Does the degree of preoperative varus alignment correlate with the lateral or medial ligamentous laxity observed after TKA?
We note several limitations. First, it is possible there was an influence of the anesthesia on the value of the varus or valgus angle measured immediately after surgery. Highgenboten et al. [4] reported the difference of anteroposterior laxity in normal knees and anterior cruciate ligament-disrupted knees using a KT-1000 arthrometer. In both knees, the values measured under an unconscious state were greater than values measured under a conscious state [4]. From their results, it seemed difficult to compare the value of angles measured immediately after surgery with the values measured after periods in an absolute manner. However, the fact that the valgus angle measured in our study was relatively constant from immediately after surgery to the following times indicated we at least could compare the value in a relative manner.
The measurement technique for coronal laxity has additional limitations. Numerous authors [10, 11, 14, 25] have measured coronal laxity by adding 15 kg of force to knees flexed somewhere between 0° and 20°. We selected 7 kg instead of 15 kg as the amount of force to be applied to the knees because 15 kg caused intolerable pain in some patients. The varus and valgus angles we obtained 12 months after surgery were approximately 4°, consistent with the values reported in other studies [10, 11, 14, 25].
We measured the coronal balance only at 15° flexion. The degree was fairly close to the extension. To evaluate the coronal balance in flexion, we should use further methods [12, 22, 23].
We found postoperative lateral ligamentous laxity closely related to the preoperative mechanical axis, meaning larger preoperative varus deformities were associated with greater lateral ligamentous laxity immediately after surgery, but we found no correlation between preoperative varus deformity and medial ligamentous laxity immediately after surgery. This close correlation between preoperative varus deformity and postoperative lateral ligamentous laxity was reasonable because we emphasized the importance of maintaining correct alignment rather than keeping the coronary soft tissue balance in varus knees. If we aimed to equalize the coronary balance, the result concerning the correlation could be altered.
We observed no remarkable change in medial ligamentous laxity between immediately after surgery and other postoperative periods. In contrast to the change in medial ligamentous laxity, a marked decrease was observed in lateral ligamentous laxity from immediately after surgery to 3 months after surgery. Yagishita et al. [25] reported, in 44 posterior cruciate ligament-retaining TKAs, the degree of preoperative varus deformity had a close correlation to postoperative lateral ligamentous laxity at an average of 32 months postoperatively. Their results are strikingly different from our results. We do not know the reason for the difference, but the difference in treatment of the posterior cruciate ligament might have some effect on the result.
Why was the large lateral ligamentous laxity observed immediately after surgery so dramatically decreased at 3 months after surgery in our study? Goradia and Van Allen [3] reported the case of a 22-year-old woman with chronic lateral instability of her right varus-deformed knee who was treated successfully with a high tibial osteotomy with no surgical intervention to the stretched lateral collateral ligament. After surgery, she had no lateral instability and successfully returned to all her recreational sports activities. In the varus-deformed knee, the soft tissue at the lateral side of the knee, including the lateral collateral ligament, is always under stretching stress in weightbearing conditions, including walking. A change in alignment from varus to valgus would decrease the stretching stress on the soft tissue at the lateral side of the knee. Therefore, the lateral instability presented preoperatively diminished after the high tibial osteotomy. In addition, many varus knees with OA or RA have some extent of bony defects at the medial tibial condyle. Because of these defects, the congruity of the distal femur and proximal tibia inevitably is decreased compared with normal knees. In TKA, the deformed surfaces of the femur and tibia are replaced with highly congruous components. These changes in congruity and alignment could have a synergic effect to decrease the stretching stress on the lateral soft tissue.
Yamamoto et al. [26] reported approximately 10% shortening of the length and a marked decrease in the tensile strength of the patellar tendon in rabbits 2 weeks after stress shielding of the patellar tendon. They reported an increase in the number of fibroblasts in the patellar tendon and in the diameter of the tendon after stress shielding but made no comments regarding the mechanism of the tendon shortening.
Coronal alignment of the lower extremity in normal subjects has been described in numerous reports [1, 2, 5, 15, 16, 20]. The tibiofemoral mechanical axis is slightly varus from 1.2° to 2.9° [1, 5, 20]. The coronal mechanical axis passes through a relatively medial part of the knee in normal subjects. Minoda et al. [15] reported the coronal mechanical axis passed through 33.9% medial to the proximal tibial articulating surface in normal Japanese subjects. Hsu et al. [5] reported 75% of the knee load passed through the medial tibial plateau, not the center of the knee, in normal subjects. Compared with normal subjects, the knees of patients after TKA could be deemed as having a valgus condition. In the valgus knee, the medial soft tissue should be tight, whereas the lateral soft tissue could be lax under weightbearing conditions. In such conditions, similar shortening of the soft tissue on the lateral side, as that observed by Yamamoto et al. [26], may occur as a result of loss of tension through postoperative changes in alignment.
In varus knees, the values of medial ligamentous laxity immediately after TKA were relatively constant for 1 year. However, the lateral ligamentous laxity was large immediately after surgery but decreased at 3 months. Our findings show, in varus knees, large lateral ligamentous laxity immediately after surgery will diminish to a normal level by 3 months after surgery. When we treat varus knees by TKA, some degree of residual lateral side laxity can be allowed as long as proper valgus alignment is maintained.
Acknowledgments
We thank Dr. Yusei Kariya from the Oyama Municipal Hospital and Dr. Yuichi Hoshino and Atsushi Seichi from Jichi Medical University for assistance.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
References
- 1.Andrews M, Noyes FR, Hewett TE, Andriacchi TP. Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. J Orthop Res. 1996;14:289–295. [DOI] [PubMed]
- 2.Cooke TD, Li J, Scudamore RA. Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am. 1994;25:387–393. [PubMed]
- 3.Goradia VK, Van Allen J. Chronic lateral knee instability treated with a high tibial osteotomy. Arthroscopy. 2002;18:807–811. [DOI] [PubMed]
- 4.Highgenboten CL, Jackson AW, Jansson KA, Meske NB. KT-1000 arthrometer: conscious and unconscious test results using 15, 20, and 30 pounds of force. Am J Sports Med. 1992;20:450–454. [DOI] [PubMed]
- 5.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed]
- 6.Insall JN. Presidential address to the Knee Society. Choices and compromises in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:43–48. [PubMed]
- 7.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed]
- 8.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 9.Insall JN, Ranawat CS, Scott WN. Total condylar knee replacement: preliminary report. Clin Orthop Relat Res. 1976;120:149–154. [PubMed]
- 10.Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G. Coronal laxity in extension in vivo after total knee arthroplasty. J Orthop Sci. 2003;8:538–542. [DOI] [PubMed]
- 11.Ishii Y, Matsuda Y, Noguchi H, Kiga H. Effect of soft tissue tension on measurements of coronal laxity in mobile-bearing total knee arthroplasty. J Orthop Sci. 2005;10:496–500. [DOI] [PubMed]
- 12.Kanekasu K, Kondo M, Kadoya Y. Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2005;434:193–197. [DOI] [PubMed]
- 13.Lotke PA. Primary total knees: standard principles and techniques. In: Lotke PA, Lonner JH, eds. Knee Arthroplasty. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:49–72.
- 14.Matsuda Y, Ishii Y. In vivo laxity of low contact stress mobile-bearing prostheses. Clin Orthop Relat Res. 2004;419:138–143. [DOI] [PubMed]
- 15.Minoda Y, Kobayashi A, Iwaki H, Sugama R, Iwakiri K, Kadoya Y, Ohashi H, Takaoka K. Sagittal alignment of the lower extremity while standing in Japanese male. Arch Orthop Trauma Surg. 2008;128:435–442. [DOI] [PubMed]
- 16.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed]
- 17.Nagamine R, Miura H, Bravo CV, Urabe K, Matsuda S, Miyanishi K, Hirata G, Iwamoto Y. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci. 2000;5:232–237. [DOI] [PubMed]
- 18.Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y. Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci. 2006;11:264–266. [DOI] [PubMed]
- 19.Sculco TP. Soft tissue balancing in total knee arthroplasty. In: Goldberg VM, ed. Controversies of Total Knee Replacement. New York, NY: Raven Press; 1991:167–174.
- 20.Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000;82:1603–1608. [DOI] [PubMed]
- 21.Teeny SM, Krackow KA., Hungerford DS, Jones M. Primary total knee arthroplasty in patients with severe varus deformity: a comparative study. Clin Orthop Relat Res. 1991;273:19–31. [PubMed]
- 22.Tokuhara Y, Kadoya Y, Kanekasu K, Kondo M, Kobayashi A, Takaoka K. Evaluation of the flexion gap by axial radiography of the distal femur. J Bone Joint Surg Br. 2006;88:1327–1330. [DOI] [PubMed]
- 23.Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K. The flexion gap in normal knees: an MRI study. J Bone Joint Surg Br. 2004;86:1133–1136. [DOI] [PubMed]
- 24.Winemaker MJ. Perfect balance in total knee arthroplasty: the elusive compromise. J Arthroplasty. 2002;17:2–10. [DOI] [PubMed]
- 25.Yagishita K, Muneta T, Yamamoto H, Shinomiya K. The relationship between postoperative ligament balance and preoperative varus deformity in total knee arthroplasty. Bull Hosp Jt Dis. 2001;60:23–28. [PubMed]
- 26.Yamamoto N, Ohno K, Hayashi K. Effects of stress shielding on the mechanical properties of rabbit patellar tendon. J Biomech Eng. 1993;115:23–28. [DOI] [PubMed]