Abstract
The relationship between radiographic and functional outcomes in older patients with distal radius fractures is controversial. We explored this relationship by assessing the influence of radiographic displacement and fracture comminution on the functional outcomes of these fractures. We also asked whether operative intervention and demographic factors (age, gender, duration of followup) influenced outcome. We examined 53 patients older than 55 years with distal radius fractures with various functional assessments: range of motion (ROM) and strength measurements, three subjective surveys (Disabilities of the Arm, Shoulder, and Hand; Patient-rated Wrist Evaluation; Modernized Activity Subjective Survey of 2007), a Gartland and Werley score, and an objective, standardized hand performance test (Jebsen-Taylor). We measured angulation, articular gap/stepoff, and radial shortening on final radiographs and fracture comminution of preoperative radiographs. We observed no effect of radiographic displacement on subjective or objective outcome assessments, including standardized hand performance timed testing. Surgically treated fractures were less likely to display residual dorsal angulation and radial shortening, but surgical intervention did not independently predict functional outcome. Fracture comminution, patient gender, and months of followup similarly had no effect on outcome. We found no relationship between anatomic reduction as evidenced by radiographic outcomes and subjective or objective functional outcomes in this older patient cohort.
Level of Evidence: Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Before the plate and screw era for bony fixation, distal radius fractures traditionally were treated by closed reduction and casting or by pins and plaster [11]. Many physicians who used these techniques claimed patients attained functionally good outcomes despite visible wrist deformities, and multiple studies showed minimal or no improvement of functional outcome with improved radiographic reduction [13, 16, 19, 27, 28, 35, 40, 41, 49]. However, with the advent of frequent internal fixation, other studies have suggested radiographic reduction does offer better functional outcomes [1, 9, 14, 21, 23–25, 30, 37, 40, 44]. These data support the trend toward surgical fixation as the definitive treatment of a distal radius fracture with deformity. Despite this shift, in a recent review of the literature it is argued, in the absence of a large, long-term, prospective, randomized, controlled trial, there is no definitive clinical evidence arguing for the superiority of any treatment modality over another, particularly regarding different modalities of surgical intervention [5]. Moreover, age-specific data regarding older patient populations that correlate radiographic and functional outcomes are insufficient, with most data tailored to younger populations [24].
We sought to determine whether (1) anatomic alignment (as measured by radiographic displacement and comminution) after distal radius fracture repair influenced standardized motion and strength measurements, functional outcome assessments, and objective, standardized, timed hand performance testing in an older cohort; and whether (2) operative intervention or (3) demographic information (age, gender, length of followup) influenced either the radiographic or functional outcome.
Materials and Methods
Using the International Classification of Diseases, 9th Revision, codes [18], we identified and contacted by phone 64 potential patients with intraarticular and extraarticular distal radius fracture who initially presented to our center from January 2006 to February 2007. All patients were seen by one of two orthopaedic hand surgeons (CSD, TDR). We included only patients 55 years or older, patients followed at least 6 months after initial treatment, and patients with isolated/unilateral distal radius fractures. We excluded patients with multiple medical comorbidities (precluding them from completing functional tasks; n = 16) or patients who had moved away (n = 17) or were no longer living (n = 5). All remaining (64) participants were called back for a 30-minute visit to measure their outcome parameters. Eleven of the 64 patients (17%) declined to participate. All 53 remaining patients completed the subjective questionnaires and functional outcomes testing in followup. The mean age of our study population (n = 53) was 69 years (range, 55–90 years), and 46 patients (87%) were female. The minimum followup from fracture treatment was 6 months (average, 17 months; range, 6–45 months). Twenty fractures (38%) were of the dominant hand. All treatment decisions were made according to the clinical judgment of the treating surgeon before study enrollment; nonoperative and operative treatments were used. Nonoperative treatment (n = 26) entailed closed reduction and immobilization. Operative treatment (n = 27) included closed reduction percutaneous pinning (n = 4), open reduction and internal fixation (n = 20), and open reduction and internal/external fixation (n = 3). Institutional Review Board approval was granted before initiation of this study, and strict confidentiality guidelines were followed.
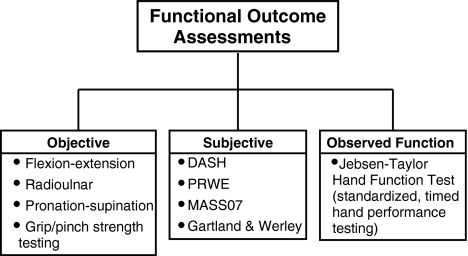
Each patient in this study was assessed according to a battery of functional and radiographic outcomes. Outcomes assessed in the study included radiographic displacement parameters, radiographic comminution assessment, ROM and strength measurements, subjective functional outcome assessments, and objective, standardized hand performance testing (Fig. 1). All of these end points were measured at the time of the study visit. Treatment modality rendered and demographic information (age, gender, duration of followup) also were collected.
Fig. 1.
The different assessments of functional outcome used in this study are shown. These tools can be classified into three general categories: objective, subjective, and observed function assessments.
For each patient, one of the authors (AJS, who was not the treating surgeon) measured three ROM parameters of the affected wrist: the flexion-extension, radioulnar, and supination-pronation arcs with a standard goniometer. All measurements were obtained using the same model goniometer and the same measurement technique. These values were compared with the contralateral, unaffected side and reported as the corresponding percentage of recovery of this unaffected side. Additional bilateral measurements included grip strength (using a Jamar dynamometer) and lateral pinch strength (using a thumb press). These also were reported as a percentage of the contralateral, unaffected side.
We used four subjective assessments/surveys to assess functional outcomes. Two of these were the Disabilities of the Arm, Shoulder, and Hand (DASH) [15] and the Patient-rated Wrist Evaluation (PRWE) [33] surveys. A third survey, the Modernized Activity Subjective Survey of 2007 (MASS07), is a novel, modern wrist and hand functional assessment recently developed and validated by our group [2]. The tasks used in the MASS07 are more technologically applicable to modern daily activities than those found in either the DASH or the PRWE. Examples of these tasks include using a computer mouse, operating a cellular telephone, and so on (Table 1). We also assigned a Gartland and Werley [10] score to each of the affected wrists. This score is an older method of evaluating healed distal radius fractures and assigns points based on criteria including residual deformity, subjective evaluation, objective evaluation, and complications. Based on the number of points accrued, the fracture is classified into four outcomes groups (excellent, good, fair, and poor). The Gartland and Werley score, which is an unvalidated scale and uses somewhat arbitrary classification groups, has been largely supplanted by more modern subjective assessments. However, its inclusion allowed comparisons with previous studies that used this score as a primary end point and thus is of some historical relevance.
Table 1.
The Modernized Activity Subjective Survey of 2007
| Functional task | No difficulty | Unable to do | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Type on a keyboard | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 2. Use a computer mouse | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 3. Dial a cell phone/telephone | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 4. Take a photograph with a camera | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 5. Pull an item from a pocket/purse | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 6. Write a check | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 7. Take a dollar bill out of a wallet | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 8. Plug a cord into a power outlet | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 9. Do laundry/fold clothes | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10. Type on a handheld device | NA | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
NA = not applicable; indicates the patient has never performed the task in question (eg, some people have never typed on a handheld device) and thus is unable to comment on the relative difficulty compared with before the fracture.
(Table modified and reprinted with permission and copyright © of Sage Publications Ltd from Alexander M, Franko OI, Makhni EC, Zurakowski D, Day CS. Validation of a modern activity hand survey with respect to reliability, construct and criterion validity. J Hand Surg Eur. 2008;33:653–660. [2] All material in this table is the exclusive property of the Sage Publications, or its licensors, and is protected by copyright and other intellectual property laws. The download of the file(s) is intended for the User’s personal and noncommercial use. Any other use of the download of the Work is strictly prohibited. User may not modify, publish, transmit, participate in the transfer or sale of, reproduce, create derivative works [including course packs] from, distribute, perform, display, or in any way exploit any of the content of the file(s) in who or in part. Permission may be sought for further use from Sage Publications Ltd, Rights & Permissions Department, 1, Oliver’s Yard, 55, City Road, London EC1Y 1SP, UK. Fax: +44(020) 7324 8600. By downloading the file(s), the User’s acknowledges and agrees to these terms.)
Finally, we assessed each wrist with an objective, standardized, timed performance test, the Jebsen-Taylor hand function test [20], which measured performance through manipulation of everyday items such as spoons, cans, pencils, and paper clips. Each patient completed these tasks with the affected and the unaffected wrists, and results were reported as a ratio (in percent form) of the two values. For this study, we used a modified Jebsen-Taylor test; the writing section was excluded because this task is highly dependent on hand dominance and therefore is difficult to interpret [6]. Because of its ability to assess true functional outcome, we believe the Jebsen-Taylor test of hand function is a particularly representative assessment of the final outcome in our analysis.
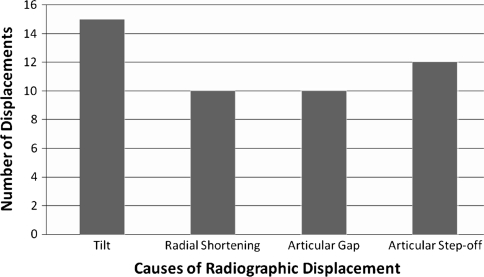
Radiographs were assessed by two study investigators (AJS, ECM). Any disputed radiographs were referred for resolution to the senior author (CSD), who was blinded to all identifying information of the patient (name, demographics, treatment modality, and so on). Radiographs of the healed distal radius fractures were assessed by the investigators and analyzed with respect to five different radiographic displacement parameters: dorsal/volar tilt, radial shortening, and articular gap/stepoff. Fractures were considered radiographically displaced if they contained one or more radiographic parameters in the bounds for dorsal tilt, volar tilt, radial shortening, articular gap, and articular stepoff (Table 2; Fig. 2) [8, 11, 24, 36, 38, 39]. Moreover, comminution was assessed by categorizing as having two, three, and four or more parts. All measurements were made using Centricity® Web software (GE Healthcare, Chalfont St Giles, UK) and the included length and angulation tools packaged in the software.
Table 2.
Criteria for radiographic displacement*
| Parameter | Range |
|---|---|
| Dorsal angulation [8, 11] | > 10° |
| Volar angulation [11, 39] | > 25° |
| Radial shortening [8, 36, 38] | > 5.0 mm |
| Articular gap [24, 36] | > 2.0 mm |
| Articular stepoff [24, 36, 38] | > 2.0 mm |
*Any fracture that healed with any one or more radiographic parameters in this range was considered to have been radiographically displaced.
Fig. 2.
We assessed the radiographic outcome of 53 patients with distal radius fractures. Twenty-six (49%) of the patients in this cohort showed evidence of radiographic displacement in at least one of four general displacement categories: tilt, radial shortening, and articular gap/stepoff. Thirteen (25%) of the fractures showed displacement of two or more parameters.
The statistical analyses were geared to address the questions of our study. Our primary question was the determination of a relationship between anatomic alignment as measured by radiographic displacement and fracture comminution; two-tailed Student’s t tests and analysis of variance were used to compare the means of two or more groups of data (ie, comparing radiographic outcomes data for two groups consisting of displaced and nondisplaced fractures). Multivariate regression analysis was performed when determining the independent predictive value of radiographic data as continuous data on functional, subjective, and objective outcomes. For the analysis of our second question, the influence of operative intervention on the radiographic and functional outcomes, two-tailed Student’s t tests were used to compare the means of two groups (ie, to compare radiographic data of operative and nonoperative groups). Chi square tests were used to compare the proportions of two or more groups (ie, the rate of operative interventions in patients with different numbers of parts for fracture comminution). Finally, multivariate regression analysis was used to determine the independent influence of treatment modality on the functional outcomes data. Our third question examined the influence of demographic factors (age, gender, length of followup) as continuous variables on the radiographic displacement and functional outcome. Multivariate regression analysis was used to evaluate the independent effect of these demographic variables on the functional outcome. For each of these analyses, the majority of the data sets fulfilled the Lilliefors criteria [31] for normality justifying the use of parametric tests; exceptions included the data for articular gap/stepoff and the MASS07 and Gartland and Werley subjective assessments. For data sets that did not meet these criteria for normality, nonparametric testing was used. We conducted all analyses using the SPSS® software package (Version 15.0; SPSS Inc, Chicago, IL).
Results
We observed no influence of anatomic deformity, as measured by radiographic displacement and comminution, on the functional outcomes data. Specifically, we found no differences (all p > 0.11) in the following outcomes between those without and with residual radiographic deformity: flexion-extension, radioulnar deviation, supination-pronation, pinch strength, DASH, PRWE, MASS07, Gartland and Werley score, and Jebsen-Taylor observed and timed hand performance test (Table 3). Percent recovery of grip strength (of the affected side as a percentage of the unaffected side) was greater (p = 0.05) in patients without evidence of radiographic displacement compared with recovery of patients with displacement. When considering severity of displacement as measured by the total number of displaced parameters, only the MASS07 showed an association (p = 0.04) between worsened function and residual radiographic deformity (Table 4). We also found no relationship between the degree of fracture comminution by parts and the functional outcomes data (Table 5). Multivariate linear regression analysis indicated no major multivariate predictors of radiographic displacement on the markers of functional outcome used in this study.
Table 3.
Comparison of functional outcomes between patients with and without evidence of radiographic displacement
| Outcome | Nondisplaced (n = 27) | Displaced (n = 26) | p Value |
|---|---|---|---|
| Range of motion (% recovery) | |||
| Flexion-extension | 83.9 ± 13.8 | 81.0 ± 11.1 | 0.40 |
| Radioulnar | 78.8 ± 18.7 | 85.7 ± 15.8 | 0.15 |
| Supination-pronation | 96.2 ± 10.3 | 96.6 ± 4.1 | 0.85 |
| Strength (% recovery) | |||
| Grip strength | 85.1 ± 21.7 | 74.3 ± 17.7 | 0.05 |
| Pinch strength | 93.5 ± 18.4 | 85.6 ± 16.9 | 0.11 |
| Subjective function (scaled score) | |||
| DASH | 14.3 ± 13.1 | 14.0 ± 11.9 | 0.92 |
| PRWE | 12.8 ± 12.9 | 16.0 ± 15.1 | 0.41 |
| MASS07 | 5.8 ± 9.0 | 7.6 ± 10.2 | 0.50 |
| Gartland and Werley | 3.1 ± 3.5 | 4.0 ± 2.8 | 0.36 |
| Objective hand performance (% recovery) | |||
| Jebsen-Taylor test | 90.9 ± 15.7 | 93.6 ± 13.1 | 0.50 |
Values are expressed as average ± standard deviation; DASH = Disabilities of the Arm, Shoulder, and Hand; PRWE = Patient-rated Wrist Evaluation; MASS07 = Modernized Activity Subjective Survey of 2007.
Table 4.
Comparison of functional outcomes according to number of displaced radiographic parameters
| Outcome | Zero (n = 27) | One (n = 13) | Two or more (n = 13) | p Value |
|---|---|---|---|---|
| Range of motion (% recovery) | ||||
| Flexion-extension | 83.9 ± 13.8 | 80.8 ± 12.4 | 81.2 ± 10.0 | 0.70 |
| Radioulnar | 78.8 ± 18.7 | 81.9 ± 15.5 | 89.5 ± 15.8 | 0.20 |
| Supination-pronation | 96.2 ± 10.3 | 97.6 ± 3.8 | 95.7 ± 4.2 | 0.81 |
| Strength (% recovery) | ||||
| Grip strength | 85.1 ± 21.7 | 76.7 ± 20.6 | 71.8 ± 14.5 | 0.13 |
| Pinch strength | 93.5 ± 18.4 | 82.3 ± 20.0 | 88.8 ± 13.3 | 0.18 |
| Subjective function (scaled score) | ||||
| DASH | 14.3 ± 13.1 | 12.9 ± 11.2 | 15.1 ± 12.8 | 0.91 |
| PRWE | 12.8 ± 12.9 | 15.5 ± 13.5 | 16.5 ± 17.2 | 0.70 |
| MASS07 | 5.8 ± 9.0 | 4.9 ± 6.4 | 10.3 ± 12.6 | 0.04 |
| Gartland and Werley | 3.1 ± 3.5 | 3.7 ± 3.0 | 4.2 ± 2.8 | 0.43 |
| Objective hand performance (% recovery) | ||||
| Jebsen-Taylor test | 90.9 ± 15.7 | 92.6 ± 13.7 | 94.7 ± 12.9 | 0.75 |
Values are expressed as average ± standard deviation; DASH = Disabilities of the Arm, Shoulder, and Hand; PRWE = Patient-rated Wrist Evaluation; MASS07 = Modernized Activity Subjective Survey of 2007.
Table 5.
Comparison of operative intervention and functional outcomes according to comminution based on number of parts
| Outcome | Two parts (n = 20) | Three parts (n = 23) | Four + parts (n = 10) | p Value |
|---|---|---|---|---|
| Rate of operative intervention (%) | 25 | 65 | 70 | 0.01 |
| Range of motion (% recovery) | ||||
| Flexion-extension | 85.5 ± 12.7 | 79.6 ± 13.3 | 82.8 ± 9.4 | 0.31 |
| Radioulnar | 81.0 ± 17.7 | 79.8 ± 17.6 | 90.2 ± 16.3 | 0.28 |
| Supination-pronation | 96.8 ± 8.4 | 95.9 ± 8.5 | 97.0 ± 5.2 | 0.91 |
| Strength (% recovery) | ||||
| Grip strength | 82.0 ± 21.7 | 77.7 ± 21.0 | 80.3 ± 17.8 | 0.79 |
| Pinch strength | 90.9 ± 20.4 | 85.9 ± 14.5 | 95.5 ± 20.0 | 0.35 |
| Subjective function (scaled score) | ||||
| DASH | 15.2 ± 14.2 | 15.7 ± 11.0 | 8.5 ± 10.9 | 0.28 |
| PRWE | 14.5 ± 14.8 | 16.9 ± 14.8 | 8.5 ± 8.7 | 0.29 |
| MASS07 | 8.9 ± 11.1 | 6.9 ± 9.5 | 1.9 ± 3.5 | 0.17 |
| Gartland and Werley | 3.1 ± 2.9 | 4.4 ± 3.9 | 2.5 ± 1.1 | 0.22 |
| Objective hand performance (% recovery) | ||||
| Jebsen-Taylor test | 92.0 ± 15.1 | 91.1 ± 15.1 | 95.3 ± 12.2 | 0.75 |
Values are expressed as average ± standard deviation; DASH = Disabilities of the Arm, Shoulder, and Hand; PRWE = Patient-rated Wrist Evaluation; MASS07 = Modernized Activity Subjective Survey of 2007.
We observed a relationship between surgical treatment and various radiographic outcomes but no influence of operative intervention on functional outcomes. Our analysis showed the fractures of patients receiving operative fixation were less deformed (p < 0.001 and p = 0.04, respectively) with respect to dorsal angulation and radial shortening compared with patients receiving nonoperative treatment (Table 6). Despite this, we observed no differences (p = 0.10) in the proportion of fractures that healed with residual displacement (ie, a fracture with any radiographic parameter exceeding the criterion for displacement) between the two groups. Moreover, we observed no differences between the two groups when considering our functional outcome assessments (Table 6). We also found the proportion of patients receiving operative intervention was greater (p = 0.01) in groups of patients with increasing degrees of fracture comminution as measured by parts (Table 5). Multivariate regression analysis showed operative intervention had no independent predictive value on the functional outcome data.
Table 6.
Comparison of outcomes with respect to treatment modality
| Outcome | Nonoperative treatment (n = 26) | Operative treatment (n = 27) | p Value |
|---|---|---|---|
| Radiographic | |||
| Dorsal tilt (degrees) | 21.0 ± 10.9 (n = 16) | 6.5 ± 3.9 (n = 12) | < 0.001 |
| Volar tilt (degrees) | 10.8 ± 5.4 (n = 10) | 7.3 ± 5.0 (n = 15) | 0.11 |
| Radial shortening (mm) | 3.4 ± 3.6 | 1.7 ± 1.9 | 0.04 |
| Articular gap (mm) | 1.3 ± 2.3 | 0.8 ± 1.3 | 0.31 |
| Articular stepoff (mm) | 1.2 ± 1.2 | 1.5 ± 1.1 | 0.45 |
| Displaced (number) | 16 | 10 | 0.10 |
| Range of motion (% recovery) | |||
| Flexion-extension | 84.3 ± 12.7 | 80.7 ± 12.4 | 0.30 |
| Radioulnar | 84.8 ± 17.7 | 79.7 ± 17.3 | 0.30 |
| Supination-pronation | 98.4 ± 3.4 | 94.6 ± 10.2 | 0.08 |
| Strength (% recovery) | |||
| Grip strength | 79.2 ± 22.9 | 80.4 ± 18.2 | 0.83 |
| Pinch strength | 88.7 ± 19.0 | 90.5 ± 17.3 | 0.15 |
| Subjective function (scaled score) | |||
| DASH | 15.7 ± 13.5 | 12.7 ± 11.2 | 0.38 |
| PRWE | 16.0 ± 14.9 | 12.8 ± 13.2 | 0.41 |
| MASS07 | 8.3 ± 10.2 | 5.2 ± 8.7 | 0.23 |
| Gartland and Werley | 3.7 ± 3.0 | 3.4 ± 3.4 | 0.69 |
| Objective hand performance (% recovery) | |||
| Jebsen-Taylor test | 93.2 ± 12.8 | 91.2 ± 16.0 | 0.62 |
Values are expressed as average ± standard deviation; DASH = Disabilities of the Arm, Shoulder, and Hand; PRWE = Patient-rated Wrist Evaluation; MASS07 = Modernized Activity Subjective Survey of 2007.
Gender and duration of followup did not influence the functional outcomes data although we found an equivocal association between patient age and functional data. Using multivariate regression analysis, we observed no associations between gender and ROM, grip strength, subjective outcomes assessments, or objective hand performance testing. We observed no relationship between the length of followup and any of the subjective or objective outcomes. Although increasing patient age had no effect on ROM, grip strength, or Jebsen-Taylor test outcomes, it was associated (p = 0.06, 0.02, and 0.02 for the DASH, PRWE, and MASS07, respectively) with worsened survey outcomes.
Discussion
Despite numerous techniques used to restore anatomic congruity after distal radius fractures, it is unclear if such restoration translates to improved functionality when considering an older patient population. The primary purpose of our study was to evaluate the relationship between anatomic alignment, measured by radiographic displacement and comminution, and our functional outcomes assessments. Our second question investigated the role of operative intervention on radiographic and functional outcomes; our third question assessed the influence of patient demographics (age, gender, length of followup) on the functional outcomes data.
We note some study limitations. All patients came from one tertiary care academic institution, and the results of the patient population and treatment preferences of this institution may not be generalizable to other patients in this age group. However, the demographics of our patient population (ie, age and gender) are similar to those of comparable studies [3, 19, 49]. There were various followups for patients in our study cohort (6–45 months); we recognize 6 months’ minimum followup is perhaps not enough time to unmask major effects of certain potential complications of distal radius fracture, including posttraumatic arthritis, intercarpal instability, and pseudosubluxation, which may occur as a result of long-standing major malalignment. However, similar studies use a comparable followup in terms of minimum or average followup [3, 12, 19, 22, 29, 32]. Moreover, we found no correlations between length of followup and functional outcome. Nevertheless, our results may not be generalizable beyond the ranges of the radiographic data, patient age, and duration of followup included in our study. Because of the retrospective nature of our study, treatments were not randomized; all patients in our study were treated according to surgeon preference before enrollment in the study. However, data revealed no correlation between treatment modality and functional outcome. Increasing fracture comminution as defined by number of parts positively influenced rate of surgery, but we found no link between comminution and any of the assessments of functional outcome in this cohort. The functional outcomes data were collected by one investigator, as noted in the Materials and Methods section. Although this eliminates interobserver variability, the potential for systemic bias, particularly regarding the ROM data, still exists. However, we do not believe this jeopardizes the general results of our study because our conclusions are based largely on the relative, and not absolute, differences between groups. Furthermore, several studies suggest using a standard goniometer to measure ROM in joints, including the wrist, shows excellent intraobserver reliability [4, 17, 43]. In another study specifically examining the intertester and intratester reliability of ROM measurements using a standard goniometer; the intraobserver results showed the minimum detectable change in forearm rotation using a goniometer was 8° [4]. Thus, our study may not be able to resolve small differences in ROM between patient subgroups. Bone mineral density would have been useful [7, 26, 47], but was not available at the time of followup.
Comparing the results of our primary question to published results for this topic, we found several studies that attempted to correlate radiographic and functional outcomes in patients with distal radius fracture. Trumble et al. [48] also attempted to determine this correlation in a series of 52 displaced, intraarticular fractures. These fractures were treated either nonoperatively (cast immobilization) or surgically (external fixation, open reduction and internal fixation, open reduction and internal/external fixation). Functional outcomes measured included ROM, grip strength, and pain evaluation. They reported postoperative gap, stepoff, and radial shortening were all “closely correlated” with the final functional outcomes. Age did not correlate with the functional outcomes. We examined 53 fractures treated with similar methods as those in the study by Trumble et al. [48] (ie, nonoperatively or through closed reduction/percutaneous pinning, open reduction and internal fixation, open reduction and internal/external fixation). However, we focused exclusively on patients older than 55 years with distal radius fractures. We also measured several additional outcomes such as subjective survey responses (DASH, PRWE, MASS07, Gartland and Werley score) and an objective hand performance test (Jebsen-Taylor). We found no associations between residual gap, stepoff, or radial shortening and any of the outcomes measured in the study of Trumble et al. [48] or with the additional outcomes unique to our study. Instead, we found functional outcomes were largely independent of the final radiographic outcomes. A study by McQueen and Caspers [34] evaluated the relationship between functional outcome and radiographic displacement in a series of 30 nonoperatively treated patients with distal radius fractures. The average age of the study cohort was 69 years, and 97% were female. Radiographs were analyzed with respect to dorsal angulation and radial shift, and patients were categorized as having good position or malunion based on these radiographs. The malunited group included all patients with a dorsal angulation greater than 10° or radial shift 2 mm or greater. This study assessed functional outcome using grip strength, ROM measurements, the Jebsen-Taylor test, and subjective surveys. In this study population, the patients with good reduction had improved subjective and objective outcomes compared with their counterparts with malunions. Our study population and functional assessment were similar to those used by McQueen and Caspers [34]; however, we used a more thorough radiographic evaluation. We compared groups of patients with acceptable and unacceptable deformities and compared continuous radiographic data with functional outcomes data in a multivariate analysis. Again, the results of these analyses showed no correlations between radiographic data and functional data. Others have reported results that differ from those of Trumble et al. [48]. Jaremko et al. [19] studied nonoperatively managed distal radius fractures in 74 patients 50 years or older (average age, 69 years; 83% female). Radiographic outcomes included dorsal tilt, radial angle, radial height, ulnar height, and articular gap/stepoff; subjective outcomes included DASH, SF-12, and satisfaction surveys. They reported no differences in DASH, SF-12, or satisfaction scores between patients with and without evidence of radiographic displacement. Our study had a similar cohort of patients with an average age of 69 years and 87% female patients, and we assessed similar radiographic outcomes (except radial tilt). We likewise reported no major outcome differences between patients with and without evidence of radiographic displacement. However, our study assessed considerably more functional outcomes, including ROM, grip/pinch strength, additional surveys (such as PRWE, MASS07, Gartland and Werley score), and measures of observed function (Jebsen-Taylor performance test). Additionally, our study included a more extensive statistical analysis, comparing the outcomes of patients based on varying numbers of displaced parameters (Table 4) and continuous radiographic data. A study by Young and Rayan [49] assessed the functional outcomes in 25 sedentary, low-demand patients older than 60 years (mean, 72 years; 76% female) with displaced distal radius fractures. Radiographic outcomes included radiographic assessment of dorsal angulation, radial shortening, and radial inclination. Functional outcomes were subjective (overall satisfaction, ability to return to previous activity level, concern over appearance, functional survey) and objective (ROM, grip strength). Radiographs were scored according to the Lidstrom system as modified by Sarmiento et al. [42]. They reported no statistical correlation between the radiographic outcomes and functional outcomes (measured by the Gartland and Werley system as modified by Stewart et al. [45, 46]). Our study had similar patient demographics (with a larger patient cohort) and similar outcomes measured. However, the radiographic scoring system used in the study by Young and Rayan [49] was considerably more generous than that in our study. For example, a fracture with as much as 11 mm radial shortening and as much as 10° dorsal angulation would still have been considered a good radiographic outcome in that study. Such a fracture in our study would have been classified as displaced. Furthermore, results in that study were reported as excellent, good, fair, or poor. Our study also provided quantitative outcomes with respect to all ROM and strength, survey, and objective outcomes measured.
A secondary question addressed in our study is the effect of operative management on radiographic and functional outcomes in this patient population. The study of Trumble et al. [48] reported anatomic improvement in the patients treated by surgical means, particularly with respect to articular congruity and radial length. Similarly, our study showed resolution of dorsal angulation and radial shortening with operative treatment. Whereas Trumble et al. reported improvement in functional outcome with anatomic reduction, these benefits were not realized in our study with respect to subjective and objective functional testing. However, we used an objective test of function and more detailed statistical analyses to investigate this relationship. For patients in whom surgery was indicated based on radiographic assessment, functional outcomes were similar to those of counterparts who did not require operative fixation.
Our third purpose in this study was to examine the role of demographic information such as gender, age, and length of followup on our results. The study by Young and Rayan [49] reported a major improvement in the outcomes of the female patients compared with their male counterparts. Although our study had a similar distribution of genders as that of Young and Rayan [49], our analysis revealed no effect of gender on the functional outcomes. With respect to age, Trumble et al. [48] observed no effect of increasing age on their results, concluding patients of all ages benefit from anatomic alignment. We found increasing patient age correlated with poorer subjective functional survey scores, although no differences were found with respect to the objective outcomes. We also observed no major relationships between patient outcomes and their length of followup and were unable to identify other studies that attempted to correlate followup to functional and radiographic outcomes.
As the preceding discussion shows, the current literature on our primary question remains equivocal, with studies that support and oppose the existence of an association between radiographic and functional outcomes in this patient population. Although our findings conflict with those of other well-designed studies, including those of Trumble et al. [48] and McQueen and Caspers [34], we believe our results provide an important piece of evidence against a relationship between anatomic deformity and functional outcome for several reasons; our patient cohort consisted of a larger group of only patients older than 55 years, and we collected a wide variety of functional outcomes data, including subjective, objective, and observed function outcomes. Furthermore, we used a more extensive statistical analysis of our data. These expansions in the methodology of our study strengthen our findings that radiographic displacement and comminution do not contribute considerably to the functional outcomes in older patients with distal radius fractures. However, although we are confident our study has clarified and added to the body of literature arguing against a relationship between functional and radiographic outcomes, this important question remains unsettled. A large, prospective trial is likely necessary to answer the question definitively. The results of our second and third investigative questions also suggest operative intervention and demographic factors (age, gender, and duration of followup) had no statistically significant influence on the radiographic and functional outcomes assessed in this study.
Acknowledgments
We thank David Zurakowski, PhD, for assistance with the statistical analysis, and all the members of the Beth Israel Deaconess Medical Center Orthopaedic Hand Research Group.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abbaszadegan H, Jonsson U. External fixation or plaster cast for severely displaced Colles’ fractures? Prospective 1-year study of 46 patients. Acta Orthop Scand. 1990;61:528–530. [DOI] [PubMed]
- 2.Alexander M, Franko OI, Makhni EC, Zurakowski D, Day CS. Validation of a modern activity hand survey with respect to reliability, construct and criterion validity. J Hand Surg Eur. 2008;33:653–660. [DOI] [PubMed]
- 3.Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29:1121–1127. [DOI] [PubMed]
- 4.Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7:573–580. [DOI] [PubMed]
- 5.Chen NC, Jupiter JB. Management of distal radius fractures. J Bone Joint Surg Am. 2007;89:2051–2062. [DOI] [PubMed]
- 6.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006;88:2687–2694. [DOI] [PubMed]
- 7.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. [DOI] [PubMed]
- 8.Earnshaw SA, Aladin A, Surendran S, Moran CG. Closed reduction of Colles fractures: comparison of manual manipulation and finger-trap traction: a prospective, randomized study. J Bone Joint Surg Am. 2002;84:354–358. [DOI] [PubMed]
- 9.Fitoussi F, Ip WY, Chow SP. Treatment of displaced intra-articular fractures of the distal end of the radius with plates. J Bone Joint Surg Am. 1997;79:1303–1312. [DOI] [PubMed]
- 10.Gartland JJ Jr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895–907. [PubMed]
- 11.Green DP, Hotchkiss RN, Pederson WC, Wolfe SW. Green’s Operative Hand Surgery. 5th ed. Amsterdam, The Netherlands: Elsevier Health Sciences; 2005.
- 12.Hollevoet N, Verdonk R. The functional importance of malunion in distal radius fractures. Acta Orthop Belg. 2003;69:239–245. [PubMed]
- 13.Horne JG, Devane P, Purdie G. A prospective randomized trial of external fixation and plaster cast immobilization in the treatment of distal radial fractures. J Orthop Trauma. 1990;4:30–34. [DOI] [PubMed]
- 14.Howard PW, Stewart HD, Hind RE, Burke FD. External fixation or plaster for severely displaced comminuted Colles’ fractures? A prospective study of anatomical and functional results. J Bone Joint Surg Br. 1989;71:68–73. [DOI] [PubMed]
- 15.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602–608. [DOI] [PubMed]
- 16.Hutchinson DT, Strenz GO, Cautilli RA. Pins and plaster vs external fixation in the treatment of unstable distal radial fractures: a randomized prospective study. J Hand Surg Br. 1995;20:365–372. [DOI] [PubMed]
- 17.Ilahi OA, Kadakia NR, Huo MH. Inter- and intraobserver variability of radiographic measurements of knee alignment. Am J Knee Surg. 2001;14:238–242. [PubMed]
- 18.International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM], 6th ed, 2008. Available at: http://icd9cm.chrisendres.com/. Accessed November 21, 2008.
- 19.Jaremko JL, Lambert RG, Rowe BH, Johnson JA, Majumdar SR. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62:65–72. [DOI] [PubMed]
- 20.Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319. [PubMed]
- 21.Jenkins NH, Jones DG, Mintowt-Czyz WJ. External fixation and recovery of function following fractures of the distal radius in young adults. Injury. 1988;19:235–238. [DOI] [PubMed]
- 22.Jenkins NH, Mintowt-Czyz WJ. Mal-union and dysfunction in Colles’ fracture. J Hand Surg Br. 1988;13:291–293. [DOI] [PubMed]
- 23.Kapoor H, Agarwal A, Dhaon BK. Displaced intra-articular fractures of distal radius: a comparative evaluation of results following closed reduction, external fixation and open reduction with internal fixation. Injury. 2000;31:75–79. [DOI] [PubMed]
- 24.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647–659. [PubMed]
- 25.Knox J, Ambrose H, McCallister W, Trumble T. Percutaneous pins versus volar plates for unstable distal radius fractures: a biomechanic study using a cadaver model. J Hand Surg Am. 2007;32:813–817. [DOI] [PubMed]
- 26.Korpelainen R, Korpelainen J, Heikkinen J, Väänänen K, Keinänen-Kiukaanniemi S. Lifelong risk factors for osteoporosis and fractures in elderly women with low body mass index: a population-based study. Bone. 2006;39:385–391. [DOI] [PubMed]
- 27.Kreder HJ, Agel J, McKee MD, Schemitsch EH, Stephen D, Hanel DP. A randomized, controlled trial of distal radius fractures with metaphyseal displacement but without joint incongruity: closed reduction and casting versus closed reduction, spanning external fixation, and optional percutaneous K-wires. J Orthop Trauma. 2006;20:115–121. [DOI] [PubMed]
- 28.Lagerstrom C, Nordgren B, Rahme H. Recovery of isometric grip strength after Colles’ fracture: a prospective two-year study. Scand J Rehabil Med. 1999;31:55–62. [DOI] [PubMed]
- 29.Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius: factors affecting functional outcome. Hand Surg. 2000;5:145–153. [DOI] [PubMed]
- 30.Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radius fractures. J Bone Joint Surg Am. 2008;90:16–22. [DOI] [PubMed]
- 31.Lilliefors HW. On the Kolmogorov-Smirnov test for normality with mean and variance unknown. J Am Stat Assoc. 1967;62:399–402. [DOI]
- 32.MacDermid JC, Donner A, Richards RS, Roth JH. Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol. 2002;55:849–854. [DOI] [PubMed]
- 33.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12:577–586. [DOI] [PubMed]
- 34.McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70:649–651. [DOI] [PubMed]
- 35.McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996;78:404–409. [PubMed]
- 36.Melone CP Jr. Distal radius fractures: patterns of articular fragmentation. Orthop Clin North Am. 1993;24:239–253. [PubMed]
- 37.Merchan EC, Breton AF, Galindo E, Peinado JF, Beltran J. Plaster cast versus Clyburn external fixation for fractures of the distal radius in patients under 45 years of age. Orthop Rev. 1992;21:1203–1209. [PubMed]
- 38.Missakian ML, Cooney WP, Amadio PC, Glidewell HL. Open reduction and internal fixation for distal radius fractures. J Hand Surg Am. 1992;17:745–755. [DOI] [PubMed]
- 39.Pogue DJ, Viegas SF, Patterson RM, Peterson PD, Jenkins DK, Sweo TD, Hokanson JA. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg Am. 1990;15:721–727. [DOI] [PubMed]
- 40.Pring DJ, Barber L, Williams DJ. Bipolar fixation of fractures of the distal end of the radius: a comparative study. Injury. 1988;19:145–148. [DOI] [PubMed]
- 41.Roumen RM, Hesp WL, Bruggink ED. Unstable Colles’ fractures in elderly patients: a randomised trial of external fixation for redisplacement. J Bone Joint Surg Br. 1991;73:307–311. [DOI] [PubMed]
- 42.Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles’ fractures: functional bracing in supination. J Bone Joint Surg Am. 1975;57:311–317. [PubMed]
- 43.Solgaard S, Carlsen A, Kramhøft M, Petersen VS. Reproducibility of goniometry of the wrist. Scand J Rehabil Med. 1986;18:5–7. [PubMed]
- 44.Stein H, Volpin G, Horesh Z, Hoerer D. Cast or external fixation for fracture of the distal radius: a prospective study of 126 cases. Acta Orthop Scand. 1990;61:453–456. [DOI] [PubMed]
- 45.Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures: a comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66:749–753. [DOI] [PubMed]
- 46.Stewart HD, Innes AR, Burke FD. Factors affecting the outcome of Colles’ fracture: an anatomical and functional study. Injury. 1985;16:289–295. [DOI] [PubMed]
- 47.Szulc P, Munoz F, Duboef F, Marchand F, Delmas PD. Bone mineral density predicts osteoporotic fractures in elderly men: the MINOS study. Osteoporos Int. 2005;16:1184–1192. [DOI] [PubMed]
- 48.Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19:325–340. [DOI] [PubMed]
- 49.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25:19–28. [DOI] [PubMed]