Abstract
Patients undergoing total knee arthroplasty often experience substantial postoperative pain, which may delay functional recovery and hospital discharge. We recently reported the short-term analgesic efficacy of a single-injection femoral nerve block after spinal anesthesia in total knee arthroplasty. We have now followed 30 patients a minimum of 1 year to determine the functional outcome and pain relief after femoral and obturator nerve block after total knee arthroplasty. Patients undergoing primary unilateral total knee arthroplasty were randomized to one of three treatment groups: (1) femoral nerve block; (2) obturator nerve block; or (3) placebo (sham block). At 6 weeks and 1 year, all three groups had similar total Hospital for Special Surgery knee scores and similar subscores such as range of motion, daily function, and resting and dynamic pain. The data support the usefulness of a peripheral nerve blockade in the context of a multimodal analgesic regimen and a tailored rehabilitation program to individual patients and institutions.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA is one of the most successful orthopaedic procedures at improving health-related quality of life. However, patients undergoing knee arthroplasty often experience substantial postoperative pain [1, 6, 13, 17, 18], which may delay functional recovery and discharge from either the hospital or rehabilitation center [4, 6, 17, 18]. Inadequate analgesia has also been associated with a decrease in patient satisfaction after surgery; in a large prospective survey of surgical inpatients, moderate or severe pain on the first postoperative day as well as nausea and vomiting was strongly correlated with patient dissatisfaction [14]. Current concepts in perioperative pain management after TKA have sought to improve analgesia while minimizing the risk of side effects. Multimodal analgesia involves the combination of different analgesic agents to provide superior pain control after surgery. One of the main objectives of multimodal analgesia is to limit the perioperative use of opioids to reduce the rate of dose-dependent side effects. Such regimens include peripheral regional nerve blocks, local anesthetic infiltrations, systemic glucocorticoids, nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and cryotherapy. This multimodal approach has an opioid-sparing effect through the synergistic action of each agent, allowing for smaller doses and fewer complications. It is now evident adequate pain control after TKA can be achieved using such a regimen without routine parenteral narcotics [8].
Patient-controlled intravenous analgesia (PCA) has traditionally been used for postoperative pain relief after TKA. Parenteral opioids can achieve some analgesia, although the effect is inconsistent and often results in persistent pain and important side effects [4, 6, 9, 13, 17–19]. Central neuraxial anesthesia, such as spinal and epidural blocks, has been successful in providing adequate pain relief and improving functional recovery after TKA [4, 13, 17, 20]. However, the risk of spinal hematoma and other serious side effects in patients treated with thromboprophylaxis after joint arthroplasty has led to the pursuit of alternative peripheral nerve blocks. The selective blockade of the lumbosacral plexus has resulted in quality analgesia and fewer complications than systemic opioids and neuraxial anesthesia [2, 4, 6, 17]. Several of us recently reported short-term analgesic efficacy of a single-injection femoral nerve block, as compared with obturator nerve block and placebo, after spinal anesthesia in TKA [11]. However, the longer-term effects of various peripheral nerve blocks remain unknown. We believed higher satisfaction rates in the immediate postoperative period due to better analgesia would result in improved function at 6 weeks, and possibly 1 year.
Therefore, we followed these same patients in a randomized, placebo-controlled, prospective double-blind study for a minimum of 1 year to determine the functional outcome and pain relief after femoral and obturator nerve block in TKA.
Materials and Methods
We previously randomized 60 patients undergoing primary unilateral TKA using spinal anesthesia to one of three treatment groups between June 2005 and July 2006 [11]. The three groups were (1) femoral nerve block (n = 20); (2) obturator nerve block (n = 20); or (3) placebo (sham block) (n = 20). Patients were enrolled on the day of surgery and randomly assigned to a study intervention using blocks of different sizes (4, 6, and 8) [11]. Inclusion criteria included age 18 years or older, primary knee arthroplasty, and fluency in English or French. We excluded 27 patients because they had contraindications to regional or spinal anesthesia, morbid obesity (body mass index greater than 35 kg/m2), renal failure, or hypersensitivity to opioids, local anesthetics, or NSAIDs. One patient who received a femoral nerve block was excluded from the original short-term study because of postoperative confusion in the recovery room precluding adequate assessment. Twenty-nine patients had 6-week and 1-year followups in an external clinic and data were not available for analysis; while we originally had the intent of following these patients for 1 year, we were unable to do so owing to limited resources at that clinic. The remaining 30 patients were available for the 6-week followup and 27 (90%) at 1 year with equal distribution in each group. These reduced groups were similar in regard to the preoperative total Hospital for Special Surgery (HSS) knee score and specific subcategories such as range of motion (ROM), daily function, and resting and dynamic pain (Table 1). We had prior ethical committee approval and informed written consent.
Table 1.
Preoperative HSS scores (mean ± standard deviation) in patients undergoing TKA*
| Study group | HSS | Function | ROM | Pain (during activity) | Pain (at rest) |
|---|---|---|---|---|---|
| Placebo | 55 ± 10 | 11.7 ± 3.2 | 12.9 ± 1.1 | 1.5 ± 2.4 | 12.9 ± 1.1 |
| Femoral | 42 ± 16 | 11.6 ± 2.0 | 12.4 ± 1.7 | 2.5 ± 5.3 | 12.4 ± 1.7 |
| Obturator | 48 ± 11 | 12.1 ± 3.3 | 12.6 ± 3.6 | 5.0 ± 7.1 | 12.6 ± 3.6 |
* Results show there are no differences in preoperative scores among the three groups; HSS = Hospital for Special Surgery; ROM = range of motion.
Standard lumbar spinal anesthesia was performed using 12 mg of 0.5% bupivicaine. The anesthesiologist administered the nerve block or sham injection after the completion of surgery while the patient’s view was still obstructed by the surgical drapes. Peripheral nerve blocks were only performed if spinal anesthesia provided persistent lack of needle prick sensation at the site without any additional sedation or analgesia. The patients and nurse coordinators (MA, LDR) collecting the data were both blinded to the study groups.
A classic paravascular femoral nerve block or obturator block was performed with a nerve stimulator for localization producing visible contractions of either the quadriceps or adductors, respectively. Nerve blocks consisted of 20 mL bupivicaine 0.5% solution with 1:200,000 epinephrine. The placebo group did not receive any injections, although the inguinal area was prepped before a sham block behind the surgical drapes. A dressing was applied for every patient to maintain double-blinding throughout the study. Adequate peripheral nerve blockade was assessed by the same anesthesiologist (KJK) in the recovery room after spinal anesthesia had completely worn off in the contralateral limb. Sensation to light touch along the cutaneous distribution of the femoral and obturator nerves was tested while motor blockade was measured with active quadriceps contraction and adduction of the operative leg. In the postoperative period, celecoxib (100 mg twice daily) and acetaminophen (650 mg four times daily) were given orally on arrival in the recovery room and regularly thereafter. Each patient also received a PCA system set to deliver 25 μg of fentanyl every 5 minutes as needed.
The 6-week and 1-year functional outcomes were measured using the HSS knee score [10]. This functional outcome measure was chosen because it evaluates both resting and dynamic pain as well as daily function and ROM. The total score, along with each of the subgroups mentioned, was analyzed separately to determine whether different peripheral nerve blocks had any effect on individual scoring items. The questionnaires were administered preoperatively and at 6 weeks (or earliest outpatient followup) and 1 year postoperatively. The orthopaedic surgeons (OLH, DJZ, JA) and nurse coordinators (MA, LDR) responsible for the questionnaires and recording the clinical data (ROM, alignment, instability, and muscle strength) remained blinded throughout the study period.
Baseline continuous data were compared between treatment groups using one-way analysis of variance. Categorical data were analyzed using chi square or Fisher’s exact test when appropriate. Results are expressed as mean ± standard error. A Bonferroni correction was applied and the groups compared two at a time when we identified a probability value less than 0.05.
Results
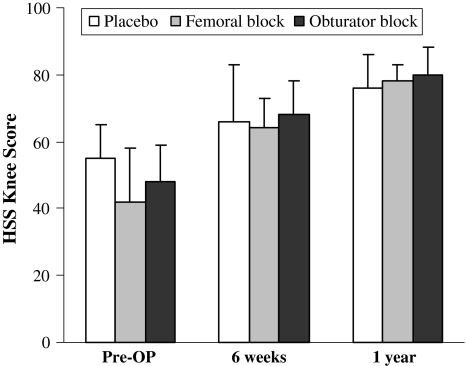
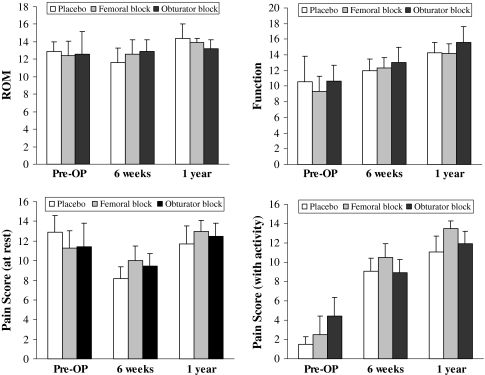
At the 6-week and 1-year followup, the three groups exhibited similar total HSS scores (Fig. 1). There was no difference in the HSS subscores such as ROM and daily function as well as resting and dynamic pain (Fig. 2). We observed no long-term complications at each followup interval from the multimodal analgesic regimen.
Fig. 1.
Total Hospital for Special Surgery (HSS) knee scores are shown. Patients were evaluated preoperatively and at 6 weeks and 1 year postoperatively. The data demonstrate no difference in HSS scores at 6 weeks and 1 year among the three study groups.
Fig. 2.
Hospital for Special Surgery (HSS) knee subscores are shown. Patients were evaluated preoperatively and at 6 weeks and 1 year postoperatively. The data demonstrate no difference in HSS subscores at 6 weeks and 1 year among the three study groups. ROM = range of motion.
Discussion
We have recently reported the short-term benefit of a single-injection femoral nerve block in TKA [11]. In the present study, we sought to determine the effect of a femoral and obturator nerve block on the functional outcome at 6 weeks and 1 year after TKA. We were unable to demonstrate any difference in the HSS knee scores after femoral or obturator nerve blocks compared with placebo at either followup period.
The relatively low number of patients (10 in each group) raises caution in the interpretation of these results. Despite this limitation, we do not believe increasing the number of patients would have resulted in an improvement between the study groups. The effects of various analgesic regimens after TKA appear limited to the immediate perioperative period without any additional longer-term benefit.
We observed no cases of persistent quadriceps weakness. The motor blockade following a single-injection femoral nerve block is usually short duration lasting less than 24 hours [1, 16]. Prolonged neurological deficit beyond one week as a result of regional anesthesia occurs infrequently and the rate of peripheral neuropathy has been estimated to below 1% [2, 3]. We discourage the use of knee immobilizers unless necessary following a neurologic complication. None of our patients required knee immobilizers. Several studies document a greater number of patients can mobilize and walk earlier following either a single or continuous femoral nerve block compared to systemic analgesia in TKR [4, 17, 18].
Postoperative pain is often substantial after TKA. Failure to provide adequate analgesia can decrease patient satisfaction, delay rehabilitation and functional recovery as well as prolong length of hospital stay. Patient-controlled analgesia is commonly used to provide pain control after TKA. However, moderate to severe pain, especially with activity, can persist in the early postoperative period despite the use of a PCA [4, 6, 9, 13, 17, 18]. The larger doses required to achieve substantial pain relief with parenteral opioids inevitably increase the risk of side effects. A systematic review reported approximately 37% of patients using PCA will experience adverse gastrointestinal effects (nausea, vomiting, ileus) as well as central nervous system effects (sedation and somnolence) in 34%, urinary retention in 16%, pruritus in 15%, and respiratory depression in 2% of patients [19].
Intraoperative neuraxial blockade is usually preferred over general anesthesia alone because it reduces the overall mortality rate by almost one-third [15]. Neuraxial anesthesia also minimizes the risk of other serious adverse events such as respiratory depression (59%), deep vein thrombosis (44%), pulmonary embolism (55%), transfusion requirements (50%), and pneumonia (39%). Central blocks, however, are not without complications and the type of side effect is relative to the concentration of opioids and local anesthetic agent within the solution. Epidural anesthesia has been associated with higher rates of urinary retention, pruritus, and hypotension when compared with systemic analgesia [7].
Central neuraxial anesthesia successfully reduces postoperative pain and may improve functional recovery after TKA [4, 13, 17, 20]. Although several studies have reported faster rehabilitation after neuraxial blocks such as knee flexion and ability to ambulate and climb stairs, these results remain debatable [4, 13, 17, 20]. A meta-analysis comparing lumbar epidural analgesia with systemic analgesia in patients undergoing joint arthroplasty found epidural anesthesia only provided better pain relief at rest in the first 4 to 6 hours after surgery [7]. In regard to dynamic pain during ROM or ambulation, epidural analgesia does appear superior to systemic analgesia in the initial 24 hours after surgery. The effect of epidural anesthesia on functional outcomes and length of hospital stay remains unknown because the data from previous randomized, controlled trials were inconclusive.
A number of studies comparing PCA, epidural analgesia, and continuous femoral block in TKA have reported similar results. Continuous femoral blocks and epidural anesthesia provided equivalent resting and dynamic analgesic effect in the first 24 to 48 hours while providing substantially better pain relief than PCA [4, 6, 17]. Functional recovery and ROM also appear improved after epidural and continuous femoral infusions compared with PCA [4, 6, 17], although no difference exists between the former two techniques. The main difference between epidural and continuous femoral blockade is the increased risk of side effects (urinary retention and hypotension) associated with central neuraxial anesthesia.
There have been conflicting reports in the literature regarding the benefits of continuous femoral infusion over a single injection. Salinas et al. reported an advantage of continuous femoral nerve blocks in resting and dynamic pain scores during the first 2 days postoperatively, whereas no difference was seen in length of hospital stay or ROM at 6 weeks and 3 months [16]. However, another study revealed no differences between PCA, single or continuous femoral blocks on patient satisfaction as well as opioid consumption, pain at rest, and with motion beyond the recovery room [9]. The combination of various peripheral nerve blocks such as the addition of an obturator block has also been studied. A single-injection femoral and obturator nerve block reduced opioid use and resting pain scores until 6 hours postoperatively, whereas scores for femoral block alone and PCA were similar [12].
In a previous study, we found femoral nerve blockade decreased both dynamic and resting pain at recovery room discharge when compared with an obturator block or placebo after TKA. There was no clinical benefit to performing an obturator nerve block alone compared with the control group. We found no difference in functional outcome scores (HSS knee score) at 6 weeks and 1 year with either block. Most of the analgesic benefit of neuraxial and peripheral blockade seems to occur in the first few days after TKA with very little effect extending beyond 48 hours. The longest followup that we could find in the literature was at 12 weeks and assessed function by measuring ROM [16, 17]. No other studies have used a validated outcome tool to objectively evaluate functional recovery after different anesthetic techniques for TKA. Preoperative and postoperative outcome measures should become an essential component in such studies given function and length of hospital stay are multifactorial outcomes not solely determined by the type of perioperative anesthesia. Length of hospital admission is intuitively a poor indicator of recovery reflecting an administrative end point rather than the isolated effect of a specific intervention [5]. Such outcomes are often influenced by patient factors (age, preoperative condition, and social support), type of surgical technique (standard versus minimally invasive), postoperative analgesia, intensity of physical therapy program, anticipated rehabilitation (inpatient versus outpatient), financial motivation, and healthcare system. In light of the current evidence, we support the use of peripheral nerve blockade in the context of a multimodal analgesic regimen and a tailored rehabilitation program to individual patients and institutions.
Acknowledgments
We thank Alain Petit for help in the preparation of the manuscript and Maricar Alminia and Laura Des Rosiers for administration of the questionnaires and recording the clinical data.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998;87:93–97. [DOI] [PubMed]
- 2.Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ, Bouaziz H, Samii K. Major complications of regional anesthesia in France: the SOS Regional Anesthesia Hotline Service. Anesthesiology. 2002;97:1274–1280. [DOI] [PubMed]
- 3.Brull R, McCartney CJL, Chan VWS, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104:965–974. [DOI] [PubMed]
- 4.Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15. [DOI] [PubMed]
- 5.Carli F, Mayo N. Measuring the outcome of surgical procedures: what are the challenges? Br J Anaesth. 2001;87:531–533. [DOI] [PubMed]
- 6.Chelly JE, Greger J, Gebhard R, Coupe K, Clyburn TA, Buckle R, Criswell A. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16:436–445. [DOI] [PubMed]
- 7.Choi PT, Bhandari M, Scott J, Douketis J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev. 2003;3:CD003071. [DOI] [PMC free article] [PubMed]
- 8.Door LD, Raya J, Long WT, Boutary M, Sirianni LE. Multimodal analgesia without parenteral narcotics for total knee arthroplasty. J Arthroplasty. 2008;23:502–508. [DOI] [PubMed]
- 9.Hirst GC, Lang SA, Dust WN, Cassidy JD, Yip RW. Femoral nerve block. Single injection versus continuous infusion for total knee arthroplasty. Reg Anesth. 1996;21:292–297. [PubMed]
- 10.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed]
- 11.Kardash K, Hickey D, Tessler MJ, Payne S, Zukor D, Velly AM. Obturator versus femoral nerve block for analgesia after total knee arthroplasty. Anesth Analg. 2007;105:853–858. [DOI] [PubMed]
- 12.Macalou D, Trueck S, Meuret P, Heck M, Vial F, Ouologuem S, Capdevila X, Virion JM, Bouaziz H. Postoperative analgesia after total knee replacement: the effect of an obturator nerve block added to the femoral 3-in–1 nerve block. Anesth Analg. 2004;99:251–254. [DOI] [PubMed]
- 13.Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990;260:30–37. [PubMed]
- 14.Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84:6–10. [DOI] [PubMed]
- 15.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321:1493. [DOI] [PMC free article] [PubMed]
- 16.Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg. 2006;102:1234–1239. [DOI] [PubMed]
- 17.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92. [DOI] [PubMed]
- 18.Wang H, Boctor B, Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002;27:139–144. [DOI] [PubMed]
- 19.Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: a systematic review. J Pain. 2002;3:159–180. [DOI] [PubMed]
- 20.Williams-Russo P, Sharrock NE, Haas SB, Insall J, Windsor RE, Laskin RS, Ranawat CS, Go G, Ganz SB. Randomized trial of epidural versus general anesthesia: outcomes after primary total knee replacement. Clin Orthop Relat Res. 1996;331:199–208. [DOI] [PubMed]