Abstract
Recently, a strong emphasis has been placed on establishing rehabilitation protocols after primary total hip and knee arthroplasty in an attempt to shorten, improve, and standardize the postoperative period of recovery. Less invasive surgical techniques, patient demands, and the pressure of insurance regulations have forced postoperative rehabilitation to be placed on an expedited scale. With these concerns in mind, we introduce a pre- and postarthroplasty program involving the Pilates method. Modified exercises have been developed to account for the postoperative precautions and needs of total hip and knee arthroplasty patients. A patient-driven interest in the use of Pilates for postoperative rehabilitation has led to the development of our programs following total hip or knee arthroplasty. In reviewing our early observations of a small series of patients, it appears this technique can be utilized without early complications; however, further studies are necessary to confirm its utility and safety.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The number and rate of total hip and knee arthroplasties being performed in the United States each year is steadily increasing, while the average age of surgical candidates continues to decline. In a report by Kurtz et al., the number of primary total hip arthroplasties (THAs) increased 50% per 100,000 persons (193,000 THAs performed) and total knee arthroplasties (TKAs) tripled (381,000 TKAs performed) from 1990 to 2002 in the United States [16]. Similarly, the healthcare environment, patient expectations, and various insurance regulations have been altered, driving initiatives calling for shorter inpatient hospital length of stay for total joint arthroplasty patients. During this time, the benefits and efficacy of early, aggressive physical rehabilitation and patient mobilization were being studied [23, 30]. Ganz et al. reported a decrease in the average length of hospital stay from 9.7 days to 5.3 days in 11,000 total hip arthroplasties from 1990 to 2000 [13]. Currently, in our institutions there has been an emphasis to shorten inpatient stays to 72 hours and pursue methods for earlier postoperative discharge. In other centers, surgeons are now performing total hip and knee replacements as an outpatient (or 23-hour stay) procedure [5–7].
One of the important benefits less invasive surgical techniques have provided is the evolution of rapid rehabilitation protocols/pathways and early (within the first 4 to 5 days after surgery) enrollment in outpatient physical therapy. One contemporary report has documented the early benefits of rapid rehabilitation in which the goals of early discharge and rapid mobilization were met by the majority of patients after minimally invasive THA [6]. Recent studies comparing less invasive THA and TKA demonstrate expedited rehabilitation protocols can be safely applied to all total joint replacements including those with traditional incisions [4, 19, 29]. Being able to incorporate these rapid rehabilitation guidelines universally has led to the current debate as to whether less invasive technique or more aggressive perioperative protocols (rehabilitation, regional anesthesia, and aggressive pain management protocols) are actually responsible for the more rapid recovery patients experience today [4, 19, 22]. Rapid rehabilitation pathways are safe and combining these protocols with preoperative physical therapy may improve a patient’s balance and neuromuscular coordination while decreasing adverse outcomes [9, 24]. Similarly, using pre- and postoperative targeted exercise programs may improve upon gait adaptations associated with hip and knee osteoarthritis/arthroplasty [12, 15, 26, 31].
Younger, more active patients currently account for an increasing population seeking total joint replacement. In turn, they also seek a more rapid and complete return to function as compared to traditional candidates for total joint arthroplasty. With this in mind, we introduced the concept of using the Pilates method for preoperative and postoperative rehabilitation for total joint arthroplasty patients in a previous report [20]. The proposed advantages of utilizing Pilates include maximizing preoperative function, developing a pathway for return to outpatient exercise, and promotion of a whole body approach to postoperative rehabilitation. The aforementioned manuscript described the philosophy, background, and means for implementing Pilates into a pre- and/or postoperative exercise regimen. A preliminary program with appropriate modifications for total hip and knee arthroplasty precautions was introduced. The timing of the postoperative interval and return to exercise was reviewed as well.
The goals of this paper are to: (1) further introduce Pilates to the orthopaedic community as a safe and efficacious modality that can be used to restore function, strength, and balance to the motivated patient; (2) describe an improved program suited to all levels of skill that can be continued as a long-term fitness and health maintenance regimen. Specific protocols with appropriate modifications for TKA and THA patients are suggested; and (3) review a series of patients having completed the described hip and knee rehabilitation programs at 1-year followup.
Introduction to Pilates
German-born Joseph Hubertus Pilates developed the Pilates method in New York from the late 1920s to the 1960s [20, 27]. Pilates, himself, suffered from several ailments during his childhood including rickets, asthma, and rheumatic fever. To overcome these medical conditions Pilates turned to exercise and fitness to improve his health, focusing on improving his strength without developing bulk. The majority of his teachings have been passed down via apprenticeship and little has been published on the Pilates method until recently [3, 8, 10, 16]. The Pilates method combines the faculties of strength and fitness training, gymnastics, boxing, self-defense instruction, and dance. The number of people participating in Pilates has increased from 1.7 million in 2000 to 10.5 million in 2004 [2].
Today several randomized, controlled trials have evaluated the efficacy of Pilates in treating low back pain with promising early results [10, 25]. The concept of strengthening the core (superficial and deep muscles that stabilize, align, and move the trunk) refers mainly to the abdominal and paraspinal musculature and building off of this foundation is becoming more acceptable in current medical practices. Recently, Rydeard et al., in a randomized controlled trial, reported a decrease in pain and disability that was sustained for a 12-month period in treating chronic low back pain using Pilates compared to traditional physical therapy [25].
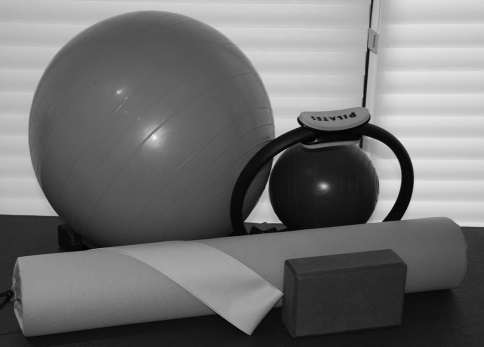
The Pilates method is a concept similar to modern principles of fitness, while connecting physical training and mental happiness. Quality movements are emphasized while maintaining a neutral spine during these ascribed exercises. Floor and apparatus work are balanced to focus on improving strength and stamina. The floor exercises use gravity to increase the difficulty while several small aids have been developed to supplement these activities. The apparatus work utilizes several devices including the fitness circle, resistance bands, physioballs, foams, and weighted balls (Fig. 1).
Fig. 1.
Supplemental devices are used with the Pilates method, including the fitness circle, resistance bands, physioballs and foam and weighted balls.
This concept of strengthening the core was recently reviewed by Willson et al. [33]. They reported that decreased core stability may predispose one to lower extremity injuries, while suggesting that achieving core stability is crucial to establishing a stable base for movement of the extremities [33]. More recent use of the Pilates method includes fine tuning of performance for elite athletes and dancers [20, 27]. Several reports have documented the use of the Pilates method in rehabilitating postsurgical patients and for recuperation of musculoskeletal conditions (adhesive capsulitis and low back pain) [8, 11, 14, 21].
Methods and Materials
We instruct patients requesting to use Pilates in their postoperative rehabilitation after a hip or knee arthroplasty to use specific regimens (Tables 1, 2). All patients are encouraged to follow the guidance of a certified Pilates instructor and to start training preoperatively. In reviewing the office notes of the senior author (WLJ) for the last 36 months, we identified 38 patients that followed these protocols. Followup and results were extracted from office notes and telephone conversations with patients at 1 year after their respective surgery.
Table 1.
Recommended postoperative THA protocols
| 2 weeks to 6 weeks*,† | 6 weeks to 6 months†,‡ | 6 months and beyond†,‡ |
|---|---|---|
| Hundred | All previous exercises | All previous exercises |
| 1/2 roll down | Full roll up | Open leg rocker |
| Single leg circles | Rolling like a ball | Swan |
| Single leg stretch | Corkscrew | Neck pull |
| Double leg stretch | Double leg kick | Side kick, variations |
| Single straight leg stretch | Neck pull, modified | Teaser 2 |
| Double straight leg stretch | Shoulder bridge | Can can |
| Criss cross | Spine twist | Hip circles |
| Spine stretch forward | Side kick, variations | Mermaid, modified |
| Saw | Teaser 1 | Leg pull front, modified |
| Swan prep | Can can, modified | Serratus push-up, modified or full |
| Single leg kick | Hip circles, modified | Push-up, modified or full |
| Shoulder bridge, modified | Swimming | |
| Side kick, variations | ||
| Teaser prep 1&2 |
* Two weeks to 6 weeks. The patient starts the mat series with a very limited pre-Pilates warmup.
†All of the above exercises (or modifications thereof) are performed under the guidelines recommended by the surgeon.
‡Any individual performing these exercises only advances to the next level after demonstrating a strong sense of core stability and strength.
(Adapted with permission from: Levine B, Kaplanek B, Scafura D, Jaffe WL. Rehabilitation after total hip and knee arthroplasty: a new regimen using Pilates training. Bull NYU Hosp Jt Dis. 2007;65(2):120–125.)
Table 2.
Recommended postoperative TKA protocols
| 2 weeks to 6 weeks*,† | 6 weeks to 6 months†,‡ | 6 months and beyond†,‡ |
|---|---|---|
| Hundred | All previous exercises | All previous exercises |
| 1/2 roll down | Full roll up | Rolling like a ball |
| Single leg circles | Double leg kick | Open leg rocker |
| Single leg stretch | Corkscrew | Swan |
| Double leg stretch | Neck pull, modified | Neck pull |
| Single straight leg stretch | Shoulder bridge | Side kick, variations |
| Double straight leg stretch | Spine twist | Teaser 2 |
| Criss cross | Side kick, variations | Can can, modified |
| Spine stretch forward | Teaser 1 | Hip circles, modified |
| Saw | Swimming | Serratus push-up |
| Swan prep | Serratus push-up, modified | Mermaid, modified |
| Single leg kick | Push-up, modified | Leg pull up, modified |
| Shoulder bridge, modified | Push-up | |
| Side kick, variations | ||
| Teaser prep 1&2 |
* Two weeks to 6 weeks. The patient starts the mat series with a very limited pre-Pilates warm-up, staying within the postoperative restrictions.
†All of the above exercises (or modifications thereof) are performed under the guidelines of the hip precautions recommended by the surgeon.
‡Any individual performing these exercises only advances to the next level after demonstrating a strong sense of core stability and strength.
(Adapted with permission from: Levine B, Kaplanek B, Scafura D, Jaffe WL. Rehabilitation after total hip and knee arthroplasty: a new regimen using Pilates training. Bull NYU Hosp Jt Dis. 2007;65(2):120–125.)
The preoperative regimen depends on the patient’s initial range of motion, pain level, and disease progression. Classic beginner mat work with individualized modifications, related to the extent of degenerative joint disease, can be initiated prior to surgery to familiarize patients with the Pilates method. The benefit of Pilates presurgically is to establish muscle memory and improve strength, mobility, and range of motion of the involved and adjacent joints. It is also helpful in establishing a working relationship with a certified Pilates instructor for later continuity [20]. The goal is for the patient to adopt a way to cope with their symptoms and to stimulate function and participation in activities despite their preoperative pain and stiffness. Patients should participate in Pilates at regular intervals, typically three to four times for 1 to 2 hours per session each week as they can tolerate. Recommended exercises include the 2 to 6 week regimen (Tables 1, 2) for the hip and knee, respectively. Incorporation of a regular exercise routine into the patient’s weekly schedule is an important part of meeting long-term physical goals.
Pilates mat exercises are designed to incorporate a whole-body workout while following six basic principles: (1) Centering is the foundation of all movements, requiring core muscle stabilization prior to initiating arm or leg movements. (2) Control refers to the ability to monitor movements while performing them with the correct mindful intent from the appropriate muscle groups. (3) Precision relates to the focus on completing an exercise utilizing the proper form and execution. (4) Concentration places form and the mental fortitude to perform an exercise as the focal point. (5) Breath refers to maintaining proper breathing techniques crucial to performing these exercises (inhalation is used to prepare for the movement and exhalation is used to execute the movement, activate core muscle support, and intensify the movement). (6) Flow is the connection of one movement to the next and is developed over time as the patient becomes familiar with the exercises [20, 32].
While the Pilates method is an integrative approach for a complete body workout, this form of exercise is fundamentally flexible and can be individualized to meet specific postoperative rehabilitative needs, such as that for total hip and knee arthroplasty (Tables 1, 2) [1, 20, 28, 32]. Particularly in the early postoperative phase, the Pilates exercises may be readily modified depending upon individual limitations and surgeon-based restrictions (ie, posterior approach hip precautions would limit hip flexion to 90°, avoid hip adduction across the midline, as well as limit degrees of internal rotation). Such alterations can be easily incorporated into a daily regimen using pillows, padding, or physioballs in the appropriate locations to restrict joint motion and abide by postoperative guidelines (Figs. 2, 3, 4).
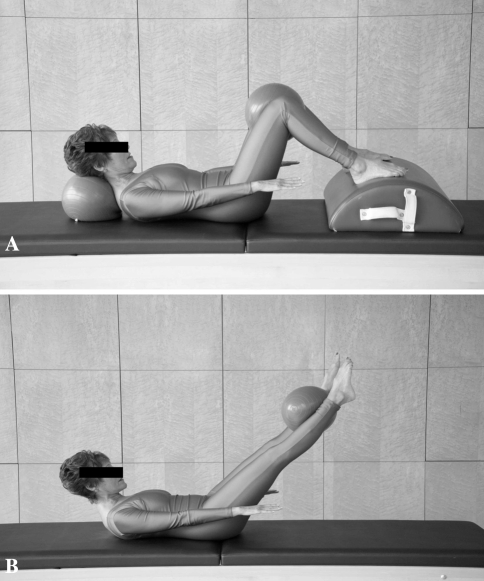
Fig. 2A–B.
Versions of the Hundred are shown with (A) modifications used at 2–6 weeks postoperatively and (B) 6 months and beyond (unrestricted activity). This is a stretching exercise utilized to increase core temperature and stimulate circulation during the warm-up period. The core muscles are engaged while actively moving the arms and legs. These motions are coordinated with an appropriate breathing pattern.
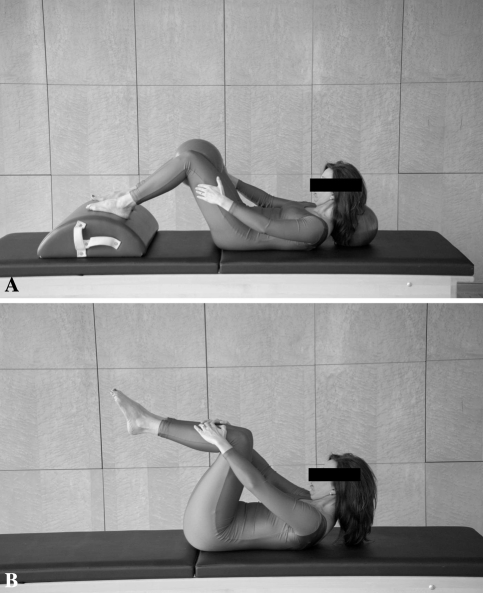
Fig. 3A–B.
Double leg stretch is shown using (A) a modified approach at 2-6 weeks postoperatively and (B) during the 6 months and beyond time frame when activity is no longer restricted. This exercise focuses on strengthening the core to provide a stable base for gait and daily function. Restrictions on flexion and extension can be controlled using the modified version of the exercise seen here.
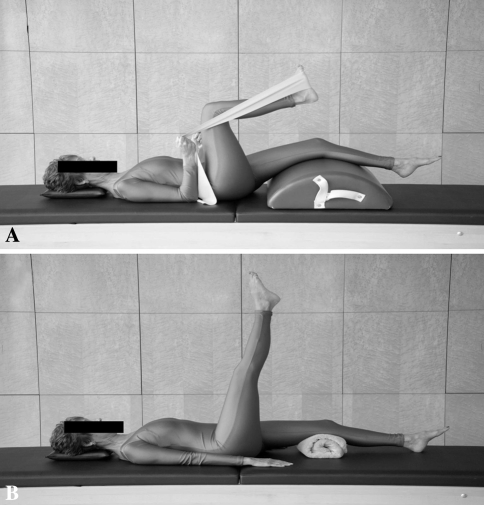
Fig. 4A–B.
Single leg circles are (A) modified for postoperative precautions during the early phase (2–6 weeks) of rehabilitation. (B) This exercise can be expanded to allow further motion and stretching as the patient’s rehabilitation progresses to 6 months and beyond.
Targeted exercise regimens can be specifically developed to meet the needs of total hip and knee arthroplasty patients (Tables 1, 2). Each patient may progress to more advanced stages as directed by a certified Pilates instructor, again keeping in mind postoperative precautions. As surgeons become more comfortable with the rapid rehabilitation process, options to supplement postoperative protocols using the Pilates method become an attractive means to potentially improve patient compliance. The multidisciplinary experience of Pilates often provides an enjoyable approach to postoperative rehabilitation that is durable and can be molded into a long-term health maintenance program.
The goals will evolve postoperatively. Guided by the Pilates principles of initiating movements from a stable source, the goals from 2–6 weeks include: performance of active and active-assisted exercises to increase hip or knee range of motion (within postoperative guidelines), early strengthening, and development of muscle memory for the hip (flexors, extensors, adductors, abductors, and internal/external rotators) and knee (flexors and extensors). Slow and controlled performance of these exercises will help strengthen the core muscles, improve hip or knee range of motion, enhance the stamina of adjacent muscles and joints, and improve ambulatory capacity.
Patients are encouraged to begin the modified Pilates program for THA (Table 1) and TKA (Table 2) within the first 2 weeks of discharge from the hospital. Progression of the program should occur as pain levels permit and patients feel safe in performing quality movements. Patients are asked to follow the exercise regimen a minimum of three to four times a week for a minimum of 1 hour a day. Appropriate use of the Pilates method facilitates the assimilation of a routine into one’s weekly schedule.
After soft tissue healing and from 6 weeks to 6 months the posterior hip precautions are eased and patients can advance to a higher level of exercise requiring a longer lever and increased core muscle stability to perform. Additional versions of the side-kick series affords an opportunity to increase the range of motion, flexibility, and strength and stamina of adjacent joints and muscles for patients after hip or knee arthroplasty. Benefits of these exercises may be seen with improved balance, ambulatory capacity, and return to other athletic activities.
Patients are encouraged to progress to the next level of the modified Pilates program for THA (Table 1) and for TKA (Table 2) at 6 weeks after surgery. An emphasis on quality/controlled movements is placed and plans for return to work and full functional capacity are outlined. At this time patients who will incorporate the Pilates method into their daily routine will continue their own exercise schedule, while those utilizing the technique for postoperative rehabilitation often discontinue their exercise regimen. If full recovery is not complete then a more targeted protocol or formal physical therapy can be initiated during this time period.
Beyond 6 months patients are near full strength and have maximized their range of motion for their respective joint arthroplasty. Postoperative precautions are released and patients may perform more intensive movements. As the core musculature strengthens patients can perform their exercises more efficiently and with enhanced stamina. Return to approved sporting activities and full participation in the Pilates method can be anticipated during this time period [18]. For rehabilitation purposes continued participation in Pilates is not required and patients may resume their normal exercise regimen and sporting activities. We have utilized the Pilates protocols outlined for interested patients over the last 5 years.
Materials and Methods
As a preliminary report, we retrospectively reviewed the office notes over the last 36 months from the senior surgeon (WLJ) in which 38 patients were noted to use Pilates for their rehabilitation after total joint arthroplasty. There were 30 women and eight men. Twenty-two THAs (21 patients) were performed, all using cementless femoral and acetabular components (Omnifit, Stryker, Mahwah, NJ), while 17 TKAs (17 patients) were performed using cemented Scorpio NRG implants (Stryker, Mahwah, NJ). The average age at the time of surgery for THA was 46.2 years and for TKA 55.4 years.
The preoperative diagnosis for TKAs included 14 cases involving osteoarthritis and three cases of inflammatory arthritis (two rheumatoid arthritis and one systemic lupus erythematosus). For patients undergoing THA, preoperative diagnoses included 16 cases with osteoarthritis, four cases of osteonecrosis of the femoral head, one case of hip dysplasia, and one case of systemic lupus erythematosus. Five women and no men had prior experience with Pilates and 26 women and two men had heard of Pilates before.
Results
At 1 year followup, review of patient charts and followup telephone calls revealed; 25 patients were extremely satisfied and 13 were satisfied with their outcome and use of Pilates in their rehabilitation. There were no patients who ranked their experience or outcome as somewhat satisfied or not satisfied. Twenty-two of 30 women (73%) reported continuing on with the Pilates method on a routine basis at 1 year after their respective joint replacement. We qualitatively observed less enthusiasm for this technique both in the short and long- term in the male patients. We have observed no adverse event.
Discussion
We present here a novel alternative for rehabilitation after total hip or knee arthroplasty. While there have been no prospective randomized studies using the Pilates method for postarthroplasty rehabilitation, our observations of patients using this protocol has been promising. Several advantages of this approach include: the use of preoperative exercises to maximize function and flexibility, the formation of a relationship with a certified instructor that can be maintained postoperatively, the relative ease in implementing these exercises into a home program, and the adaptability of the Pilates method to accommodate various joint precautions and range-of-motion restrictions. Patient compliance appears improved, particularly among our female joint replacement patients, with 73% maintaining an active role in Pilates at 1 year after surgery. However, we did observe less enthusiasm for this technique both in the short and long- term for the male patients in our practices.
The current report has several inherent limitations associated with the retrospective nature of data collection. Additionally we do not have a control study to compare our results to, nor was the selection of patients randomized. Essentially patients were self-selected by expressing the desire to use this technique for their postoperative rehabilitation. This introduces a selection bias for motivated patients into our results. However, the goal of this paper and technique is not to show that Pilates as a form of rehabilitation is better than traditional therapy, but to offer it as a viable option for postoperative hip and knee therapy. Despite these study limitations, this preliminary report supports using the Pilates method as an alternative form of rehabilitation after total hip and knee arthroplasty.
In recent years there has been a resurgence in the teachings of the Pilates method, with more than 10 million active participants [2]. The number of Pilates studios and fitness centers offering Pilates training has been increasing across the United States. In a survey of the members of the Hip Society and the American Association of Hip and Knee Surgeons (AAHKS), Pilates was rated as a sports activity that patients are allowed (58% allowed without experience and an additional 24% recommended to allow participation with experience) to participate in after a THA [18]. There are multiple levels of difficulty and individual exercises are easily modified to allow compliance with postoperative total joint precautions. Patients can safely progress in their rehabilitation course as directed by their surgeon and certified Pilates instructor. The goal after surgery is to resume training with the patient’s preoperative instructor, starting within 2 weeks from the surgery (similar to when patients start standard outpatient physical therapy protocols). The concept of mind-body rehabilitation is becoming more popular in the United States today and has been applied to the treatment of low back pain, common shoulder disorders, and general myalgias [10, 17, 25]. This approach represents an expansion of this form of exercise for postoperative rehabilitation in total hip and knee arthroplasty patients.
Our protocols were developed in conjunction with certified Pilates instructors. Pilates as a form of rehabilitation has been utilized by the senior author (WLJ) for willing and motivated THA and TKA patients for the past 5 years without a single negative event and a high degree of patient satisfaction both physically and emotionally. For now, the implementation of such a program should be individualized and limited to include close supervision by certified Pilates instructors only. The authors offer these guidelines not to replace formal postarthroplasty physical therapy, but as a safe alternative for those willing and self-motivated patients.
Acknowledgments
We thank Beth Kaplanek and Dina Scafura for developing the following protocol: Specified Pilates Techniques for Hip and /or Knee Syndromes®.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at New York University Hospital for Joint Diseases.
References
- 1.Adamand K, Loigerot D. The Pilates Edge: An Athlete’s Guide to Strength and Performance. New York, NY: Penguin Books; 2004.
- 2.American Sports Data Inc. Available at http://www.americansportsdata.com. Accessed March 4, 2008.
- 3.Beck R. Getting to the core. Using pilates to promote overall wellness during rehabilitation. Rehab Manag. 2008;21:34–36. [PubMed]
- 4.Bennett D, Ogonda L, Elliott D, Humphreys L, Lawlor M, Beverland D. Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: a prospective blinded study. J Arthroplasty. 2007;22:490–495. [DOI] [PubMed]
- 5.Berger RA. A comprehensive approach to outpatient total hip arthroplasty. Am J Orthop. 2007;36(9 Suppl):4–5. [PubMed]
- 6.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. [DOI] [PubMed]
- 7.Berry DJ, Berger RA, Callaghan JJ, Dorr LD, Duwelius PJ, Hartzband MA, Lieberman JR, Mears DC. Minimally invasive total hip arthroplasty. Development, early results, and a critical analysis. Presented at the Annual Meeting of the American Orthopaedic Association, Charleston, South Carolina, USA, June 14, 2003. J Bone Joint Surg Am. 2003;85:2235–2246. [PubMed]
- 8.Blum CL. Chiropractic and Pilates therapy for the treatment of adult scoliosis. J Manipulative Physiol Ther. 2002;25:E3. [DOI] [PubMed]
- 9.Brosseau L, MacLeay L, Robinson V, Wells G, Tugwell P. Intensity of exercise for the treatment of osteoarthritis. Cochrane Database Syst Rev. 2003;2:CD004259. [DOI] [PubMed]
- 10.Donzelli S, Di Domenica E, Cova AM, Galletti R, Giunta N. Two different techniques in the rehabilitation treatment of low back pain: a randomized controlled trial. Eura Medicophys. 2006;42:205–210. [PubMed]
- 11.Duschatko DM. Certified pilates and gyrotonics trainer. J Bodyw Mov Ther. 2000;4:13–19. [DOI]
- 12.Foucher KC, Hurwitz DE, Wimmer MA. Preoperative gait adaptations persist one year after surgery in clinically well-functioning total hip replacement patients. J Biomech. 2007;40:3432–3437. [DOI] [PubMed]
- 13.Ganz SB, Wilson PD, Jr, Cioppa-Mosca J, Peterson MG. The day of discharge after total hip arthroplasty and the achievement of rehabilitation functional milestones: 11-year trends. J Arthroplasty. 2003;18:453–457. [DOI] [PubMed]
- 14.Herrington L, Davies R. The influence of Pilates training on the ability to contract the transversus abdominis muscle in asymptomatic individuals. J Bodyw Mov Ther. 2005;9:52–57. [DOI]
- 15.Hurwitz DE, Ryals AR, Block JA, Sharma L, Schnitzer TJ, Andriacchi TP. Knee pain and joint loading in subjects with osteoarthritis of the knee. J Orthop Res. 2000;18:572–579. [DOI] [PubMed]
- 16.Jago R, Jonker ML, Missaghian M, Baranowski T. Effect of 4 weeks of Pilates on the body composition of young girls. Prev Med. 2006;42:177–180. [DOI] [PubMed]
- 17.Keays KS, Harris SR, Lucyshyn JM, MacIntyre DL. Effects of Pilates exercises on shoulder range of motion, pain, mood, and upper-extremity function in women living with breast cancer: a pilot study. Phys Ther. 2008;88:494–510. [DOI] [PubMed]
- 18.Klein GR, Levine BR, Hozack WJ, Strauss EJ, D’Antonio JA, Macaulay W, Di Cesare PE. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J Arthroplasty. 2007;22:171–175. [DOI] [PubMed]
- 19.Lawlor M, Humphreys P, Morrow E, Ogonda L, Bennett D, Elliott D, Beverland D. Comparison of early postoperative functional levels following total hip replacement using minimally invasive versus standard incisions. A prospective randomized blinded trial. Clin Rehabil. 2005;19:465–474. [DOI] [PubMed]
- 20.Levine B, Kaplanek B, Scafura D, Jaffe WL. Rehabilitation after total hip and knee arthroplasty: a new regimen using Pilates training. Bull NYU Hosp Jt Dis. 2007;65:120–125. [PubMed]
- 21.Maher CG. Effective physical treatment for chronic low back pain. Orthop Clin North Am. 2004;35:57–64. [DOI] [PubMed]
- 22.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. [DOI] [PubMed]
- 23.Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br. 2007;89:316–322. [DOI] [PubMed]
- 24.Pilot P, Bogie R, Draijer WF, Verburg AD, van Os JJ, Kuipers H. Experience in the first four years of rapid recovery; is it safe? Injury. 2006;37(Suppl 5):S37–40. [DOI] [PubMed]
- 25.Rydeard R, Leger A, Smith D. Pilates-based therapeutic exercise: effect on subjects with nonspecific chronic low back pain and functional disability: a randomized controlled trial. J Orthop Sports Phys Ther. 2006;36:472–484. [DOI] [PubMed]
- 26.Shakoor N, Hurwitz DE, Block JA, Shott S, Case JP. Asymmetric knee loading in advanced unilateral hip osteoarthritis. Arthritis Rheum. 2003;48:1556–1561. [DOI] [PubMed]
- 27.Shand D. Pilates to pit. Lancet. 2004;363:1340. [DOI] [PubMed]
- 28.Siler B. The Pilates Body. New York, NY: Broadway Books; 2000.
- 29.Tanavalee A, Thiengwittayaporn S, Itiravivong P. Progressive quadriceps incision during minimally invasive surgery for total knee arthroplasty: the effect on early postoperative ambulation. J Arthroplasty. 2007;22:1013–1018. [DOI] [PubMed]
- 30.Thien TM, Ahnfelt L, Eriksson M, Stromberg C, Karrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop. 2007;78:730–738. [DOI] [PubMed]
- 31.Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheum. 2006;54:3842–3849. [DOI] [PubMed]
- 32.Ungaro A. Pilates Body in Motion. New York, NY: DK Publishing; 2002.
- 33.Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005;13:316–325. [DOI] [PubMed]