Abstract
There is an increasingly growing interest world-wide for the genomics, transcriptomics and proteomics of saliva and the oral cavity, since they provide a non-invasive source of unprecedently rich genetic information. The complexity of oral systems biology goes much beyond the human genome, transcriptome and proteome revealed by oral mucosal cells, gingival crevicular fluid, and saliva, and includes the complexity of the oral microbiota, the symbiotic assembly of bacterial, fungal and other microbial flora in the oral cavity. In our review we summarize the recent information on oral genomics, transcriptomics and proteomics, of both human and microbial origin. We also give an introduction and practical advice on sample collection, handling and storage for analysis. Finally, we show the usefulness of salivary and oral genomics in early diagnosis of cancer, as well as in uncovering other systemic diseases, infections and oral disorders. We close the review by highlighting a number of possible exploratory pathways in this emerging, hot research field.
Key Words: Saliva, genome, transcriptome, proteome, systemic diseases, oral diseases, screening, early diagnosis.
INTRODUCTION
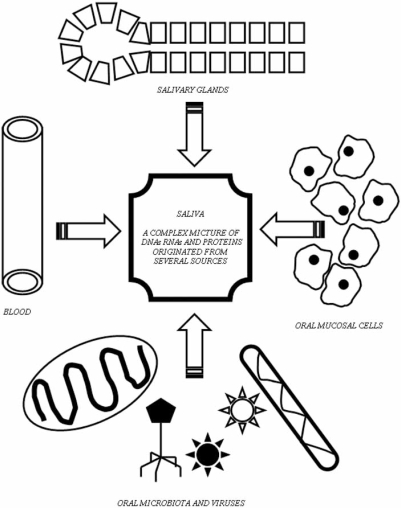
The genomics, transcriptomics and proteomics of saliva and the oral cavity became increasingly popular subjects of research in recent years, since they represent a non-invasive, safe, and cheap source of complex genetic information. The source of this information-complexity is the large variety of DNAs, RNAs and proteins present in the saliva (Fig. 1). Salivary DNAs represent (a) the genetic information (genome) of the hosting human body, (b) the oral microbes present in the mouth (oral microbiota), and (c) the infecting DNA-viruses. Salivary mRNAs provide information on the transcription rates of host genes (the human oral transcriptome) and those of the oral microbiota. Other salivary RNAs may indicate RNA-virus infections. Salivary proteins (proteome) represent both genetic information (i.e. the mass-spectrometry reveals amino acid sequences, which help to elucidate the encoding genes) and help to understand the translational regulation of the host body and the oral microbiota. This explains the increasing interest on this subject in several fields including dentistry, medicine and microbiology.
Fig. (1).
Complexity of salivary genome, transcriptome and proteome.
Many aspects of salivary genomics and proteomics were reviewed in recent years. The diagnostic applications of saliva were covered rather extensively [1-4]. Other reviews highlighted the possible use of saliva in cancer diagnosis [5- 8], in the diagnosis of systemic diseases [9], in microbiota analysis [10] in proteome analysis [11] in psychobiological medicine [12] and in forensic dentistry [13]. However, most of the above reviews discussed a certain specific aspect of the field [5-13]. Other summaries either gave a short general overview [1, 3, 4, 9], or included many other aspects, which are not related to salivary genomics and proteomics (e.g. secretory rates, nonpeptide hormones, ionic changes etc.) [2]. The aim of the present review is to give an integrative overview of salivary genomics, transcriptomics and proteomics including the description of saliva collection, handling and storage; diagnostic possibilities as well as future perspectives.
SALIVARY GENOMICS, TRANSCRIPTOMICS AND PROTEOMICS: COMPARISON WITH OTHER SAMPLE SOURCES
Cytologic and Biopsic Collection of Samples
Colpocytology, buccal cell cytology, and several incisial-, needle-, and excisial biopsic sample collection methods (etc.) are usually used for the analysis of local tissues and organs [14-16]. Advantage of such samples is that clear evidence may be reached related to the target tissue [16]. The disadvantage of such sampling is that such methods (especially biopsy methods) are invasive and mostly rather unpleasant for the patients. Another disadvantage is exemplified by their above-mentioned advantage: they provide a local information and are rather unsuitable for the general screening of the organism, although it is true that, they also contain the whole human genome (DNA) [17]. Cytological and biopsy samples are usually sources for detection of local changes related to transcriptome (mRNA) and proteome. Such samples are also used for verifying infections of the target organ by identifying microbial or viral RNA and DNA [16, 18].
Blood and Body Fluid Sampling
Blood and body fluid sampling such as collection of blood and saliva is different. Such samples represent more information related to general conditions of the whole body, which is advantageous for screening purposes [19]. Disadvantage of such sampling is that there is usually no clear evidence related to the origin (localization) of the alterations detected. Blood sampling also has the disadvantage that it is invasive and unpleasant [17]. On the contrary, collection of saliva is noninvasive and not unpleasant at all [17]. Blood samples contain many mRNAs and proteins from several body sources, and blood is a source of human genome (human DNA), too. Blood may also contain RNAs and DNAs of infecting viruses and microbes [20]. Whole saliva is a source of both the human and oral microbiotal genome. Saliva is also a good tool to detect systemic changes of mRNA and proteome because it is blended with contaminating blood, gingival crevicular fluid, mucosal transudate and also ultrafiltrate of the salivary glands' acini [2] (Fig. 2). Further, alterations of oral mucosal cells, salivary glands and oral microbiota are also detectable via analysis of salivary mRNA and proteome. Finally, saliva contains RNAs and DNAs of infecting microbes and viruses of both local tissues (i.e. oral mucosal cells, salivary glands) and also tissues located in other part of the body [14, 20].
Fig. (2).
Routes of DNAs, RNAs and proteins of blood origine into the saliva.
Comparison of Blood, Oral Mucosal Cell and Saliva Samples
Regarding to DNA quality blood samples seem to be superior to all other DNA sources, usually all of the samples could be genotyped, amplified or sequenced [17]. DNA yield from saliva is also rather good in quality, the majority of the samples could be genotyped, amplified or sequenced [17, 21]. Quality of buccal cell DNA seems to be poor [17, 21]. Samples of buccal cells collected with swabs were found not suitable for genotyping, and could be weakly amplified in a comparative study [17]. Buccal cell samples collected with foam-tipped applicators (FTA) could be genotyped in the majority of the cases, however this kind of sample was not suitable for amplification (probably because of the rather small DNA-yield) [17]. The above findings are interesting all the more, because desquamating mucosal cells are the likely source of salivary DNA as well [1]. It might be that DNA of spontaneously desquamated cells - present in saliva - is more intact than that of artificially removed cells. For mRNA analysis all sources including blood [22, 23], mucosal cells [24] and saliva [25, 26] can be used effectively. However, there are some differences related to the origin of mRNA present in a certain kind of samples as pointed out above. Regarding to protein analysis all the three sources may be used, and the protein-yield is good in all cases. However, it should be considered that there are proteins of different origin present in most of these samples as mentioned above.
GENOMIC, TRANSCRIPTOMIC AND PROTEOMIC CONSTITUENTS OF SALIVA
Genome (Human DNA)
The value of total DNA content in human whole saliva was found in a range between 1.8 – 128.4 μg/mL with a mean value of 21.6 μg/mL [17]. In other studies higher values like 40.3 ± 36.5 μg/mL [27] and 77.5 ± 51.5 μg/mL [21] were also reported. A proportion of roughly 70% is of human origin [27] the other 30% is originated from the oral microbiota (and viruses if any). Although it was not jet investigated in detail, it is likely that desquamated oral mucosal cells represent the main human DNA source of saliva. The quality of salivary DNA yield is good, 72% to 96% of samples could be genotyped [17, 27], 84% could be amplified [17] and 67% could be sequenced [17].
Transcriptome (Human mRNA)
Although rRNSs and tRNAs are rather stable in the cell, mRNAs are usually rapidly degraded (which may happen in a few minutes). Partly because of these reasons mRNA constitutes a small proportion of total cellular RNA comparing to the much more abundant rRNA and tRNA fractions. Consequently, extracellular RNAs belong mostly to rRNA and tRNA fractions, whereas the proportion of mRNA believed to be the smallest. It would also be likely that, a high proportion of the salivary RNA is of microbial origin because of the rather rich oral microbiota. Based on the above considerations some authors suppose the absence of detectable amount of human mRNAs in a cell free saliva [28]. Although this opinion seems to be a bit exaggerated [29] (see below), but we would like to point out that caution should be used in interpreting saliva-based mRNA expression studies without the technical exclusion of possible DNA contamination artifacts [28, 29].
The total RNA level in cell free (centrifuged) whole saliva is ranging from 0.108 ± 0.023 μg/mL [25] to 6.6 ± 3.6 μg/mL [26]. Interestingly, the majority of RNAs present in cell free whole saliva is genuine human mRNA [29]. The detectable amount of distinct human mRNA specii is between 3,000 [25] and 6,400 [26]. These represent roughly 16% [25] and 13% [26] of the included sequences of applied human arrays, respectively, and 28% of the protein-coding human genes (calculating with middle value of estimations between 20,000 - 25,000 [30, 31]). The proportion of function-unknown salivary mRNSs is about of 27.5% [32]. There are roughly 200 salivary mRNAs found in all the individuals termed "normal salivary transcriptome core" (NSCT) [25, 26, 32, 33]. However, the overlap of individual mRNA stocks are usually higher, 419 and 570 identical transcripts were found in 90% and 80% of the subjects respectively [32].
There is also a comparable amount of RNA in isolated parotid saliva (3.6 ± 1.5 μg/mL [26]). However, it contains lower number (4,778 transcripts) of informative mRNAs than whole saliva does [34]. There are also high number of mRNA in sublingual saliva (1,831 transcripts), submandibular saliva (1,543 transcripts), gingival crevicular fluid (2,689 transcripts), and desquamated oral epithelial cells (3,142 transcripts) [34] indicating that, mRNA enters whole saliva from various sources [34].
Microbial DNA and RNA
There proportion of oral microbiotal DNA is roughly 32% indicating a significant amount of non-human genome in whole not-centrifuged saliva [17]. Although there is no concrete data available in the literature about the whole amount of non human RNAs in whole not-centrifuged saliva, a comparable proportion as in case of DNA is likely. (As mentioned above, the majority of RNAs in centrifuged whole saliva is of human origin [29] but in this case microbiota is removed).
Salivary Proteome
The total amount of proteins in whole saliva is ranging between 0.5 to 3 mg/mL. This proteome consists of roughly 1,000 distinct protein sequences [26], from which around 300 sequences are of human origin [32]. A proportion ranging between 22.8% to 28.7% of detected human sequences have an unknown function [32], which is rather similar to the proportion of mRNAs with no functional identification [32]. The co-existence of a certain protein sequence and its own mRNA is detectable in a rather high proportion of proteins with exact values ranging between 70% to 93%, which is depending on the actual methods used [32]. However, only a little correlation of the change of the amount of a certain protein and the alterations of its mRNA level were found under a particular pathological condition, like the Sjögren's syndrome [26]. Latter finding gives an experimental proof of our general assumption that both protein and mRNA markers are important and provide a non-redundant information [26].
COLLECTION, HANDLING AND STORAGE OF SALIVA FOR DNA, RNA AND PROTEOME ANALYSIS
Collection of Saliva
Whole saliva can be collected by drooling into a vial with forward tilted heads, or by allowing the saliva to accumulate in the mouth and than expectorate it into a vial [35, 36]. Isolated parotid saliva may be collected with direct cannulation of the parotid duct, or with the use of parotid cup (a plastic container stabilized on the mucosal surface via a pocket enabling negative pressure). Mixed submandibular/sublingual saliva may be collected with direct cannulation of submandibular duct [26].
Handling of Saliva
Since the main source of salivary DNA is given by desquamated oral mucosal cells [1], preclearing (i.e. centrifuging, microfiltering) of saliva before DNA analysis is not suggested. In contrast, for RNA analysis saliva sample is usually centrifuged (i.e. 2,600 x g, 15 min. 4°C [25, 26]), because the majority of RNAs present in cell free (centrifuged) whole saliva are genuine human mRNAs [29]. However, the microfiltration of saliva (i.e. instead of centrifuging) is not suggested for RNA analysis, because majority of salivary RNA is macromolecule-associated (see also below) and will not pass through 0.22 μm or 0.45 μm pore size microfilters [34]. For RNA studies focusing on oral microbiota, any kind of preclearing of saliva should be avoided. For analyzing salivary proteome of human origin, saliva may be precleared by centrifugation (i.e. 10,000 x g; 10 min. 4°C) and/or microfiltered by 0.22 μm or 0.45 μm pore size microfilters [35, 36]. However, it should be considered that, high molecular weight macromolecule complexes may be sedimented by centrifugation or blocked in pores of microfilters leading to certain loss of such complexes (and quick obstruction of filters). To avoid such loss of macromolecule complexes a lower g-value centrifugation (i.e. 2,600 x g 15 min. 4°C [25, 26]) may be used, however, in this case microbial contamination of the sample is somewhat higher. In case that, the proteome of oral microbiota is targeted, all kind of preclearing of saliva samples should be avoided.
DNA Stability
In appropriate buffers of DNA extraction kits saliva can be stored at room temperature for up to at least 1 year [17]. However before adding such buffers saliva should be stored on ice (+4°C) to prevent bacterial (or other microbial growth) and to decrease salivary DNase activity. Saliva can also be frozen and stored on -20°C or -80°C before DNA extraction [37]. Extracted DNA can be also frozen and stored on -20°C or -80°C until use [17].
RNA Stability
There are several microbial and/or human RNases present in saliva which may destroy RNA molecules, in some cases even with a half-lives of a few minutes (range between 0.4 to 12.2 min.) [34]. Interestingly human salivary mRNAs are more stable in saliva than exogenous ones (i.e. mouse mRNA added to saliva [34]) indicating that human mRNA is protected by certain human-specific mechanisms against salivary nucleases [34]. This protective phenomenon likely occurs because of RNA-macromolecule interactions [34] and can be abolished with detergents [34]. (The phenomenon that RNAs associate with other macromolecules is known also in serum and plasma. Such complexes are called particle-associated RNAs [23]). Possible associated proteins of salivary mRNA may be apoptotic bodies of desquamated mucosal cells [22, 34] and several saliva proteins like mucines [34]. It may also be hypothesized that, salivary chaperone Hsp70 [35, 38] may take part in the protection of human mRNA, too. Because of premised possible role of proteins in salivary mRNA stability, addition of protease inhibitors to salivary samples can be useful even in case of mRNA analysis [25, 26]. Cooling of saliva samples on ice (+4°C) is also suggested [25, 26].
Because of above mechanisms, most of salivary RNAs are partially degraded only [29, 34]. On the average salivary mRNA represents 42% of its respective (original) full length [29]. In contrast to blood the degradation pattern is rather random with only a slightly more degradation at the 5' end (if any) [29, 34]. Further, those of long transcripts have an increased chance of being degraded than shorter [29, 34]. These findings indicate a predominant endonuclease activity in saliva [29, 34] in contrast to blood, in which the activity of exonucleases is typical [19]. Because of above, use of RNase inhibitors (especially against endonucleases) is recommended to avoid destruction of salivary RNAs. Although with the use of certain RNase inhibitors mRNA can be stabilized for longer run even in room temperature [39], however cooling of saliva samples on ice (+4°C) is still useful [26]. RNA can be preserved in saliva also by freezing at -80°C [25], in this case supplementation with stabilizing "RNAlater" reagents may be suggested [26].
Protein Stability
Precleared saliva can be stored on ice (+4°C) without significant protein degradation only for few hours, and without preclearing the degradation is even quicker. Consequently addition of protease inhibitors is advantageous especially for time consuming analysis procedures. Freezing frequently resulted in significant protein precipitation, even if quick freezing is used, and the frozen sample can be stored for a few days only without any further damage at -20°C. Somewhat longer storage is possible in liquid nitrogen or at -80°C, however proteins are not stable for a longer run even in such conditions.
SYSTEMS BIOLOGY OF SALIVARY MICROBIOTA
Complexity of the Oral Microbiota
The microbiota of the oral cavity consists of more than 600 microbial specii (or not yet cultivated phylotypes) including predominantly bacteria, but also fungi and protozoa [40-43], from which 347 clones are predominant in subgingival pocket [43], others are more frequent in the supragingival bacterial biofilm (i.e. dental plaque). However in individual hosts just a subset of all specii can be found [44], indicating a high degree of interpersonal variability. The subgingival bacterial community in a single individual was found to consist of 25 to 34 [45], 59 [46] or 72 to 99 [43] specii and phylotypes in different studies. Similarly, supragingival tooth-surface attached biofilm (dental plaque) consisted of 11 to 29 [47], or 32 [48], or 52 [49], or up to 94 to 114 (pooled sample) [50] specii and phylotypes in several studies.
Microbiota of the Saliva
Despite the important antimicrobial activity of saliva [38, 51, 52] the complexity of salivary microbiota was similar to the oral microbiota above including 37 [40] or 33 to 53 [44] different bacterial specii and phylotypes and 1 to 3 yeast (Candida) [53] specii, (altogether up to 56 specii and phylotypes). It is likely that, the total number of salivary specii is even higher [44]. To understand the high number of specii despite the antimicrobial saliva activity it should be considered that, the bacterial metabolism alters when certain bacteria get in contact with saliva [54], and several bacteria can even ferment and grow on saliva [55]. Further, microorganisms attached to the surfaces of the mouth and teeth are continuously shed into the salivary fluid, and bacteria residing in the periodontal pockets are constantly washed into saliva by the gingival crevicular fluid [44]. Because of the above mentioned constant microbial replacement, salivary microbiota reflect to many changes occurring in any part of the mouth as a "fingerprint" of the whole oral microbiota [44, 56].
Effect of Salivary Microbiota on other Parts of Gastrointestinal Tract
Increased expression of molecular chaperones (especially DnaK) strongly increases the acid tolerance of salivary bacteria (i.e. Streptococcus mutans) on pH 5 (or even lower) [57]. Such a low pH occur regularly in the deeper area of tooth surfaces attached bacterial biofilm (i.e. dental plaque) [57] indicating that, many of bacteria present in such biofilm may survive in rather low pH. Thus, such bacteria also may survive passing through the stomach. This route opens the possibility that, oral microbiota may have an influence on and alter the microbiota of other parts of gastrointestinal tract. For example, Helicobacter pylori bacteria, (a known cause of peptic ulcer disease and chronic gastritis) was found in higher prevalence in saliva than in feces, indicating that oral rout (including oral-oral route like kissing) may be an important means of transmission of this infection [58]. Some Lactobacillus specii present in the faeces were also found to be transient (allochthonous) to the intestine and originate from the oral cavity [59]. It is likely that, recently developed oral microbiota diagnostic systems based on 16S rRNA microarrays [10, 60] may lead to recognition of numerous similar interference of oral and gastrointestinal microbiota. Although the microbiota normally configure to match the usual normal community structure, in some cases as-yet uncharacterized properties may alter the microbial balance [61, 62]. It may not be excluded that, certain transient species of oral origin can be responsible for such alterations, leading to several pathologic conditions of the gastrointestinal tract.
SALIVARY DNA, RNA AND PROTEOME IN THE DIAGNOSIS OF DISEASES
Early Cancer Diagnosis
In case of saliva two major facets of cancer diagnosis should be distinguished, such as diagnosis of oral cancers (getting direct contact with saliva) and of those in other locations. Advanced stage oral cancers are usually detectable by inspection of the oral cavity. In contrast, early stage oral carcinomas are not viewable, frequently not diagnosed or treated in time, because even microscopic level for a progressive cancer can be too late for successful intervention [6, 63]. Similarly, tumors of other locations are also usually not diagnosed early enough, because they are out of sight in early stages and also because they are frequently not viewable even in advanced stages (depending on location). Since the prognosis of advanced stage cancers are much worse than of early stage ones, highly sensitive methods for both oral and other located early cancer detection are needed to reduce lethal outcome of these dangerous diseases [63].
There are some tumor specific DNA markers in serum and other body fluids may be used for the diagnosis of both oral and other tumors, based on the assumption that the initiation and progression of malignant tumors is driven by the accumulation of specific genetic alterations [1, 6]. In saliva, mutated salivary DNA at p53 gene was found in 62.5% of oral cancer patients [64]. Similarly, an increased content of mitochondrial DNA was found in the saliva (also in tumor tissue [65]) of head and neck cancer patients [66], which decreased after the surgical removal of such tumors [67]. Detection of HPV (human papilloma virus) DNA in saliva also enables the detection of HPV-related head and neck cancers [68]. Similarly, detection of DNA (or proviral DNA) of other tumor-inducing viruses like HIV (human immunodeficiency virus) [69] and HHV-8 (human herpesvirus 8) [70] in saliva may also be useful for oral and/or other located cancer risk assessment.
Analysis of serum mRNAs can also be a good and sensitive tool for detection of certain oral and other tumors [71-73]. Especially global mRNA-profiling of serum seems to be promising [71]. However collection of blood is unpleasant for many of subjects [17], it is invasive and expensive to some extent. Consequently, the collection of saliva seems to be more suitable for the screening of larger populations. Profiling of salivary mRNA indicated four major biomarkers of oral cancer including interleukin-1-β (IL1β), interleukin-8 (IL8), ornithine decarboxylase antizyme-1 (OAZ1) and spermidine/spermine N1-acetyltransferase (SAT). Regression tree (CART) analysis of these four, elevated biomarkers was able to distinguish patients with T1 and T2 oral cancer from control subjects with very high sensitivity (91%) and specificity (91%) [63]. Beside the above markers, detection of tumorigenic virus RNAs, like HIV-1 may also be useful in evaluating risk of malignancies [20].
Salivary proteome can also be used for tumor detection. Increased salivary level of defensin-1 [74], cancer antigen CA15-3 [5, 75], tumor marker proteins, like c-erbB-2 [5, 75] or CA-125 [76] and antibodies against the tumor suppressor protein, p53 [77] seem to be promising markers for both oral and other malignancies [2]. A future global proteome profiling of saliva with newly developed methods of proteome analysis [78-82] would likely resulted in further candidate peptide sequences of sensitive tumor detection [3].
Other Systemic Conditions
There are significant changes of salivary proteome and transcriptome also in the case of Sjögren's syndrome [26]. A recent study indicated 16 down-regulated and 25 upregulated distinct amino-acid sequences in whole saliva proteome, from which 10 up-regulated and 6 down-regulated proteins seemed to be statistically significant biomarkers of Sjögren's syndrome [26]. This study also indicated a higher level of total RNA of both whole and parotid cell free saliva [26]. In whole saliva 162 mRNAs were up-regulated (at least 2-fold), whereas only few were down-regulated. 27 mRNAs were up-regulated at least 3-fold, and 13 mRNAs were upregulated more than 10-fold [26]. From the 27 (at least 3-fold upregulated) genes 19 were interferon-inducible, or were related to lymphocyte infiltration, and antigen presentation known to be involved in the pathogenesis of Sjögren's syndrome. The mRNA of an interferon-α inducible protein (G1P2) was 500-fold upregulated [26]. Taking together these data, it is obvious that the analysis of salivary proteome and transcriptome (especially, when used together) provides a great possibility for both the better understanding and the improved diagnostics of Sjögren's syndrome [26] and other diseases.
Psychological stress conditions also induce significant changes in both salivary proteome and transcriptome. The increase of salivary amylase is a known proteomic indicator of psychological stress [36, 83] and sympathetic activation [84, 85]. A recent paper indicated that amylase specific salivary mRNA level also increases significantly after stress with some delay [86]. Besides the above stress-markers, decrease of secretory IgA [87], and increase [36] of immune-modulator defense protein salivary chaperone Hsp70 [35, 38] was also reported. Global profiling of genome, transcriptome and proteome present in saliva likely lead to the recognition of numerous other stress-markers and stress sensitivity markers in the next future.
A number of other disorders exist, where salivary changes with significant diagnostic value were also characterized. In Cystic fibrosis the excretion of an unusual, less effective form [88] of salivary epidermal growth factor (EGF [89]) was reported. There are also characteristic salivary changes in case of graft-versus-host disease including the elevated concentration of total protein, albumin, EGF, IgG, and a decreased amount of IgA and IgM in the saliva [90]. In coeliac disease the elevated salivary level of IgA antigliadin antibodies (AGA) may be used for screening purposes with moderate sensitivity (60%) and high specificity (93%) [91]. In case of peptic ulcers and chronic gastritis, Helicobacter pylori infection (a frequent cause) can be detected with 84% sensitivity and 82% specificity via detection of bacterial DNA in saliva [58]. H. Pylori may also be detected with salivary antibodies against this bacterium (sensitivity 85%, specificity 55%) [92]. Neurocistercosis can also be identified with the detection of antibodies against Taenia solium larvae with a sensitivity of roughly 70% [93]. The above mentioned disorders and molecular markers may also be taken as examples of the next future possibilities opening to recognize sensitive diagnostic markers of further disorders [1, 3, 4, 79].
Virus Infections
Saliva analysis is a good tool for detection of virus infections, based on identification of viral DNAs and RNAs, antibodies against viruses, and viral antigens [2, 94]. DNA and RNA analysis shows moderate to high sensitivity, however a progress related to the accuracy of such methods is very likely in the next future. Proteomic methods like detection of antibodies against viruses and detection of virus antigens are highly sensitive and specific methods available already today (see below). Detection of salivary viral DNA is a possible diagnostic tool for screening with a moderate to high sensitivity in case of several viruses like cytomegalovirus (sensitivity 36% [14]), human herpes virus (HHV) type 6 (sensitivity 80% [95]), HHV type 7 (sensitivity 100% [95]), HHV type 8 (sensitivity 30% to 66% [18, 70]) and transfusion transmitted (TTV [96]) virus (sensitivity 39% [97]). Detection of salivary proviral DNA (host cell integrated viral sequences) may also be used for such purposes with moderate sensitivity (40% [98]) in case of human immunodeficiency virus type 1 [16, 69, 98]. Detection of viral RNA in saliva may also be used with moderate to high sensitivity in detection of viruses like hepatitis G virus (sensitivity 35% to 100% [97, 99]) and HIV-1 (sensitivity 37% to 100% [14, 20, 98, 100, 101]). In the proteomic level numerous viruses can be detected with high sensitivity and specificity via detection of salivary antibodies against viruses. There are highly sensitive methods available for dengue virus (sensitivity 92%, specificity 100% [102]), hepatitis A (sensitivity 99%, specificity 99% [103]), hepatitis B (sensitivity 100%, specificity 100% [104]), hepatitis C (sensitivity 100%, specificity 100%) [104, 105], HIV-1 (sensitivity 95% to 100%, specificity 95% to100% [106-109]), measles (sensitivity 97%, specificity 100% [110]), mumps (sensitivity 94%, specificity 94% [110]), parvovirus type B19 (sensitivity 100%, specificity 95% [111]), and rubella (sensitivity 98%, specificity 98% [110]). Detection of virus antigens in saliva is also a possible highly sensitive and specific method in detection of hepatitis B virus (sensitivity 92%, specificity 87% [112]).
Dental Caries
There are some more or less specific changes of salivary proteome, which may be used for recognizing caries-risk patients. These include decreased level of proline-rich proteins (PRP1 and PRP3), histatin 1 and statherin [113]. Increased numbers of Streptococcus mutans and Lactobacilli in saliva were also associated with increased caries prevalence [114, 115], and with the presence of root caries [116]. Decreased complexity (fewer number of specii and phylotypes) of the oral microbiota was also found to be a risk for early childhood caries [50]. Although caries related microbiotal data were recognized mainly by analysis of tooth-surface biofilm (dental plaque) but the complex microbiota present in saliva [40] likely reflect to this differences as well [44, 56]. Investigation of salivary microbiota with high capacity automatized nucleic acid extraction and analysis [117] and also global genome, transcriptome and proteome profiling of saliva will likely lead to further new caries related predictive markers in the future.
Periodontal Inflammation
The presence of certain periodontopathogen bacterial species in saliva reflect their presence in dental plaque and periodontal pockets [45, 56, 118, 119] indicating that saliva may be a good tool to detect bacterial risk factors by salivary DNA analysis of oral microbiota [45]. Such DNA-based methods open new perspectives in both the understanding and the diagnosis of periodontal disorders, since they allow the analysis of non cultivable (yet-to-be cultured) microorganisms as well [45]. Besides genomic methods, proteomic analysis may also become important in the next future. It is known for example that the level of alpha-2-macroglobulin, alpha-1-antitripsin, elastase and also albumin in saliva may be good indicators of gingivitis and/or periodontitis. The level of salivary defense proteins like immunoglobulin, molecular chaperone Hsp70, cystatin S, salivary amylase, calprotectin, hystatins, lysozyme, lactoferrine, defensins, peroxidases, prolin-rich proteins and mucins [38, 51, 52] may also have prognostic value related to the possible passing of gingivitis to periodontitis (where the latter is a more severe inflammation with irreversible destruction) [38, 120, 121]. It is also likely that the global profiling of salivary genome, transcriptome and proteome will lead to recognition of further highly sensitive diagnostic markers of periodontal conditions.
Oral Candidiasis
Saliva may also be used for detection of oral fungi [53, 122]. In case of oral candidiasis, salivary fungal counts may also reflect mucosal colonization [123]. Alteration of salivary proteome related to proteins showing antifungal properties like immunoglobulin, calprotectine, histatin-5, mucins peroxidases, basic prolin-rich proteins, molecular chaperone Hsp70 etc. [38, 51, 52] may also have important diagnostic/prognostic value especially in recurrent cases.
CONCLUSIONS AND PERSPECTIVES
With advances in genomics, transcriptomics and proteomics of saliva, salivary testing in clinical and research settings is rapidly proving to be a practical and reliable means of recognizing several systemic and oral conditions [2, 9]. However, further detailed studies establishing the diagnostic value of saliva in comparison with that of other biomedia, (especially with blood) will be necessary to assess the detailed prognostic and diagnostic value of saliva [4]. At this stage of knowledge saliva seems to be a highly important possible tool for regular screening of larger populations. However, it may also turn out in many cases that saliva is as accurate (or even better) as blood in establishing a definitive diagnosis of certain disorders and monitoring disease progression [1, 4]. However, the road to practical and effective regular use of salivary diagnostics is expected to be promising, but long [6, 7]. For the regular clinical use the analysis should be highly automatized, and coupled with microfluidic technology, enabling a small sample size to be used, avoiding reagents' and waste's cost and allowing that types of assays that are impossible at the macroscopic level [10]. The identification of biomarkers with a proper and definite sensitivity and specificity to as many disorders and conditions as possible is also a prerequisite [7]. Thus, further technological advancement and identification of robust and discriminatory sets of salivary biomarkers is necessary [7] to fulfill all requirements for being regular diagnostic tool for the everyday clinical practice. Despite limitations we experience today, the use of saliva for diagnostic purposes becomes increasingly popular, and as a result, more and more diagnostic tests become commercially available, and are currently used by clinicians and researchers [2]. Taking together all these aspects, it can be concluded that there are rich possibilities in saliva-diagnostics already at present, and the immediate future of this area is even more promising.
ACKNOWLEDGEMENTS
Work in the authors’ laboratory was supported by research grants from the Hungarian National Science Foundation (OTKA-K69105) and from the EU (FP6-016003).
REFERENCES
- 1.Tabak LA. A revolution in biomedical assessment: the development of salivary diagnostics. J. Dent. Education. 2001;65:1335–1339. [PubMed] [Google Scholar]
- 2.Kaufman E, Lamster IB. The diagnostic application of saliva - a review. Crit. Rev. Oral Biol. Med. 2002;13:97–202. doi: 10.1177/154411130201300209. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Denny P, Ho C-M, Montemagno C, Shi W, Qi F, Wu B, Wolinsky L, Wong DT. The oral fluid MEMS/NEMS chip (OFMNC): Diagnostic & translational applications. Adv. Dent. Res. 2005;18:3–5. doi: 10.1177/154407370501800102. [DOI] [PubMed] [Google Scholar]
- 4.Wong DT. Salivary diagnostics powered by nanotechnologies, proteomics and genomics. JADA. 2006;137:313–321. doi: 10.14219/jada.archive.2006.0180. [DOI] [PubMed] [Google Scholar]
- 5.Streckfus C, Bigler L. The use of soluble, salivary c-erbB-2 for the detection and post-operative follow-up of breast cancer in women: The results of a five-year translational research study. Adv. Dent. Res. 2005;18:17–24. doi: 10.1177/154407370501800105. [DOI] [PubMed] [Google Scholar]
- 6.Westra WH, Califano J. Toward early oral cancer detection using gene expression profiling of saliva: A thoroughfare or dead end? Clin. Cancer. Res. 2004;10:8130–8131. doi: 10.1158/1078-0432.CCR-04-1906. [DOI] [PubMed] [Google Scholar]
- 7.Wong DT. Toward a simple, saliva-based test for the detection of oral cancer. Expert Rev. Mol. Diagn. 2006;6:267–272. doi: 10.1586/14737159.6.3.267. [DOI] [PubMed] [Google Scholar]
- 8.Streckfus C, Dubinsky WP. Proteomic analysis of saliva for cancer diagnosis. Expert. Rev. Proteomics. 2007;4:329–332. doi: 10.1586/14789450.4.3.329. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J. Can. Dent. Assoc. 2002;68:170–174. [PubMed] [Google Scholar]
- 10.Smooth LM, Smooth JC, Smidt H, Noble PA, Könneke M, McMurry ZA, Stahl DA. DNA microarrays as salivary diagnostic tools for characterizing the oral cavity's microbial community. Adv. Dent. Res. 2005;18:6–11. doi: 10.1177/154407370501800103. [DOI] [PubMed] [Google Scholar]
- 11.Helmerhorst EJ, Oppenheim FG. Saliva: a dynamic proteome. J. Dent. Res. 2007;86:680–693. doi: 10.1177/154405910708600802. [DOI] [PubMed] [Google Scholar]
- 12.Chiapelli F, Iribarren FJ, Prolo P. Salivary biomarkers in psychobiological medicine. Bioinformation. 2006;1:331–334. doi: 10.6026/97320630001331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lijnen I, Willems G. DNA research in forensic dentistry. Methods Find. Exp. Clin. Pharmacol. 2001;23:511–517. doi: 10.1358/mf.2001.23.9.662139. [DOI] [PubMed] [Google Scholar]
- 14.Lurain NS, Robert ES, Xu J, Camarca M, Landay A, Kovacs AA, Reichelderfer PS. HIV type 1 and cytomegalovirus infection in the female genital tract. JID. 2004;190:619–623. doi: 10.1086/422533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gulley ML, Sargeant KP, Grider DJ, Eagan PA, Davey DD, Damm DD, Robinson RA, Vandersteen DP, McGuff HS, Banks PM. Lymphomas of the oral soft tissues are not preferentially associated with latent or replicative Epstein-Barr virus. Oral Surg. Oral Med. Oral Pathol. Radiol. Endod. 1995;80:425–431. doi: 10.1016/s1079-2104(05)80336-1. [DOI] [PubMed] [Google Scholar]
- 16.Yeh CK, Fox PC, Goto Y, Austin HA, Brahim JS, Fox CH. Human immunodeficiency virus (HIV) and HIV infected cells in saliva and salivary glands of a patient with systemic lupus erythematosus. J. Rheumatol. 1992;19:1810–1812. [PubMed] [Google Scholar]
- 17*.Hansen TO, Simonsen MK, Nielsen FC, Hundrup YA. Collection of blood, saliva, and buccal cell samples in a pilot study on the Danish nurse cohort: Comparison of the response rate and quality of genomic sample. Cancer Epidemiol. Biomarkers Prev. 2007;16:2072–2076. doi: 10.1158/1055-9965.EPI-07-0611. * This important paper is a detailed comparison of several sample sources like blood, saliva and buccal cell samples related to quantity and quality of enriched DNA. [DOI] [PubMed] [Google Scholar]
- 18.Pauk J, Huang M-L, Brodie SJ, Wald A, Koelle DM, Schacker T, Celum C, Selke S. Mucosal shedding of human herpesvirus 8 in men. N. Engl. J. Med. 2000;343:1369–1377. doi: 10.1056/NEJM200011093431904. [DOI] [PubMed] [Google Scholar]
- 19.Wong BC, Chiu RW, Tsui NB, Chan KC, Chan LW, Lau TK, Leung TN, Lo YMD. Circulating placental RNA in maternal plasma is associated with a preponderance of 5' mRNA fragments: implications for noninvasive prenatal diagnosis and monitoring. Clin. Chem. 2005;51:1786–1795. doi: 10.1373/clinchem.2005.052340. [DOI] [PubMed] [Google Scholar]
- 20.Freel SA, Williams JM, Nelson JAE, Patton LL, Fiscus SA, Swanstrom R, Shugars DC. Characterization of human immunodeficiency virus type 1 in saliva and blood plasma by V3-Specific heteroduplex tracking assay and genotype analyses. J. Virol. 2001;75:4936–4940. doi: 10.1128/JVI.75.10.4936-4940.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rogers NL, Cole SA, Lan HC, Crossa A, Demerath EW. New saliva DNA collection method compared to buccal cell collection techniques for epidemiological studies. Am. J. Human. Biol. 2007;19:319–326. doi: 10.1002/ajhb.20586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasselmann DO, Rappl G, Tilgen W, Reinhold U. Extrcaellular tyrosinase mRNA within apoptotic bodies is protected from degradation in human serum. Clin. Chem. 2001;47:1488–1489. [PubMed] [Google Scholar]
- 23.Tsui NBY, Ng EKO, Lo YMD. Stability of endogenous and added RNA in blood specimens, serum, and plasma. Clin. Chem. 2002;48:1647–1653. [PubMed] [Google Scholar]
- 24.Spivack SD, Hurteau GJ, Jain R, Kumar SV, Aldous KM, Gierthy JF, Kaminsky LS. Gene-environment interaction singatures by quantitative mRNA profiling in exfoliated buccal mucosal cells. Cancer Res. 2004;64:6805–6813. doi: 10.1158/0008-5472.CAN-04-1771. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Zhou X, St John MAR, Wong DTW. RNA profiling of cell-free saliva using microarray technology. J. Dent. Res. 2004;83:199–203. doi: 10.1177/154405910408300303. [DOI] [PubMed] [Google Scholar]
- 26**.Hu S, Wang J, Meijer J, Leong S, Xie Y, Yu T, Zhou H, Henry S, Vissink A, Pijpe J, Kallenberg C. Salivary proteomic and genomic biomarkers for primary Sjögren's syndrome . Arthritis & Rheumatism. 2007;56:3588–3600. doi: 10.1002/art.22954. ** In this important paper there are highly interesting data related to parallel changes of transcriptome and proteome under systemic disease, which allows the reader to have a look in to the deepness and complexity of saliva diagnostics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rylander-Rudquist T, Hakansson N, Tybring G, Wolk A. Quality and quantity of saliva DNA obtained from the self-administered oragene method - a pilot study on the cohort of Swedish men. Cancer Epidemiol. Biomarkers Prev. 2006;15:1742–1745. doi: 10.1158/1055-9965.EPI-05-0706. [DOI] [PubMed] [Google Scholar]
- 28.Kumar SV, Hurteau GJ, Spivack SD. Validity of messenger RNA expression analysis of human saliva. Clin. Cancer. Res. 2006;12:5033– 5039. doi: 10.1158/1078-0432.CCR-06-0501. [DOI] [PubMed] [Google Scholar]
- 29**.Park NJ, Zhou X, Yu T, Brinkman BMN, Zimmermann BG, Palanisamy V, Wong DT. Characterization of salivary RNA by cDNA library analysis. Arch. Oral. Biol. 2007;52:30–35. doi: 10.1016/j.archoralbio.2006.08.014. ** This important paper gives clear evidences that, salivary mRNA data are not because of artifacts caused by salivary DNA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG, Smith HO, Yandell M, Evans CA, Holt RA, Gocayne JD, Amanatides P, Ballew RM, Huson DH, Wortman JR, Zhang Q, Kodira CD, Zheng XH, Chen L, Skupski M, Subramanian G, Thomas PD, Zhang J, Gabor Miklos GL, Nelson C, Broder S, Clark AG, Nadeau J, McKusick VA, Zinder N, Levine AJ, Roberts RJ, Simon M, Slayman C, Hunkapiller M, Bolanos R, Delcher A, Dew I, Fasulo D, Flanigan M, Florea L, Halpern A, Hannenhalli S, Kravitz S, Levy S, Mobarry C, Reinert K, Remington K, Abu-Threideh J, Beasley E, Biddick K, Bonazzi V, Brandon R, Cargill M, Chandramouliswaran I, Charlab R, Chaturvedi K, Deng Z, Di Francesco V, Dunn P, Eilbeck K, Evangelista C, Gabrielian AE, Gan W, Ge W, Gong F, Gu Z, Guan P, Heinman TJ, Higgins ME, Ji RR, Ke Z, Ketchum KA, Lai Z, Lei Y, Li Z, Li J, Liang Y, Lin X, Lu F, Merkulov GV, Milshina N, Moore HM, Naik AK, Narayan VA, Neelam B, Nusskern D, Rusch DB, Salzberg S, Shao W, Shue B, Sun J, Wang Z, Wang A, Wang X, Wang J, Wei M, Wides R, Xiao C, Yan C, Yao A, Ye J, Zhan M, Zhang W, Zhang H, Zhao Q, Zheng L, Zhong F, Zhong W, Zhu S, Zhao S, Gilbert D, Baumhueter S, Spier G, Carter C, Cravchik A, Woodage T, Ali F, An H, Awe A, Baldwin D, Baden H, Barnstedt M, Barrow I, Beeson K, Busam D, Carver A, Center A, Cheng ML, Curry L, Danaher S, Davenport L, Desilets R, Dietz S, Dodson K, Doup L, Ferriera S, Garg N, Gluecksmann A, Hart B, Haynes J, Heiner C, Hladun S, Hostin D, Houck J, Howland T, Ibegwam C, Johnson J, Kaulsh F, Kline L, Koduru S, Love A, Mann F, May D, McCawley S, McIntosh T, McMullen I, Moy M, Moy L, Murphy B, Nelson K, Pfannkoch C, Pratts E, Puri V, Querishi H, Readon M, Rodriguez R, Rogers YH, Romblad D, Ruhfel B, Scott R, Sitter C, Smallwood M, Stewart E, Strong R, Suh E, Thomas R, Tint NN, Tse S, Vech C, Wang G, Wetter J, Williams M, Windsor S, Winn-Deen E, Wolfe K, Zavery J, Abril JF, Guigó R, Campbell MJ, Sjolander KV, Karlak B, Kejarival A, Mi H, Lazareva B, Hatton T, Narechania A, Diemer K, Muruganujan A, Guo N, Sato S, Bafna V, Istrail S, Lippert R, Schwartz R, Walenz B, Yooseph S, Allen D, Basu A, Baxendale J, Blick L, Caminha M, Carnes-Stine J, Caulk P, Chiang YH, Coyne M, Dahlke C, Mays A, Dobroski M, Donelly M, Ely D, Esparham S, Fosler C, Gire H, Glanowski S, Glasser K, Glodek A, Gorokhov M, Graham K, Gropman B, Harris M, Heil J, Henderson S, Hoover J, Jennings D, Jordan J, Kasha J, Kagan L, Kraft C, Levitsky A, Lewis M, Liu X, Lopez J, Ma D, Majoros W, McDaniel J, Murphy S, Newman M, Nguyen T, Nguyen N, Nodell M, Pan S, Peck J, Peterson M, Rowe W, Sanders R, Scott J, Simpson M, Smith T, Sprague A, Stockwell T, Turner R, Venter E, Wang M, Wen M, Wu D, Wu M, Xia A, Zahndieh A, Zhu X. The sequence of the human genome. Science. 2001;291:1304–1351. doi: 10.1126/science.1058040. [DOI] [PubMed] [Google Scholar]
- 31.Levy S, Sutton G, Ng PC, Feuk L, Halpern AL, Walenz BP, Axelrod N, Huang J, Kirkness EF, Denisov G, Lin Y, MacDonald JR, Pang AWC, Shago M, Stockwell TB, Tsiamuri A, Bafna V, Bansal V, Kravitz SA, Busam DA, Beeson KY, McIntosh TC, Remington KA, Abril JF, Gill J, Borman J, Rogers YH, Frazier ME, Scherer SW, Strausberg RL, Venter JC. The diploid genome sequence of an individual human. PLoS. Biol. 2007;5:e254, 2113–2144. doi: 10.1371/journal.pbio.0050254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu S, Li Y, Wang J, Xie Y, Tjon K, Wolinsky L, Loo RRO, Loo JA, Wong DT. Human saliva proteome and transcriptome. J. Dent. Res. 2007;85:1129–1133. doi: 10.1177/154405910608501212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zimmermann BG, Park NJ, Wong DT. Genomic targets of saliva. Ann. N.Y. Acad. Sci. 2007;1098:184–191. doi: 10.1196/annals.1384.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34*.Park NJ, Li Y, Yu T, Brinkman BMN, Wong DT. Characterization of RNA in saliva. Clin. Chemistry. 2006;52:988–994. doi: 10.1373/clinchem.2005.063206. * This important paper gives evidences of association of salivary mRNA with other salivary macromolecules, and a detailed overview about the degradation pattern of salivary mRNA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fábián TK, Gáspár J, Fejérdy L, Kaán B, Bálint M, Csermely P, Fejérdy P. Hsp70 is present in human saliva. Med. Sci. Monitor. 2003;9:BR62–65. [PubMed] [Google Scholar]
- 36.Fábián TK, Tóth Zs, Fejérdy L, Kaán B, Csermely P, Fejérdy P. Photo-acoustic stimulation increases the amount of 70 kDa heat shock protein (Hsp70) in human whole saliva. A pilot study. Int. J. Psychophysiol. 2004;52:211–216. doi: 10.1016/j.ijpsycho.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 37*.Bello FD, Hertel C. Oral cavity as natural reservoir for intestinal lactobacilli Systemat . Appl. Microbiol. 2006; 29:69–76. doi: 10.1016/j.syapm.2005.07.002. * This important paper gives evidences that, oral microbiota may influence the microbiota of other parts of the gastrointestinal system. [DOI] [PubMed] [Google Scholar]
- 38.Fábián TK, Fejérdy P, Nguyen MT, Sőti Cs, Csermely P. Potential immunological functions of the salivary chaperone, Hsp70 in the mucosal and periodontal defense mechanisms (Review) Arch. Immunol. Ther. Exp. 2007;55:1–8. doi: 10.1007/s00005-007-0012-z. [DOI] [PubMed] [Google Scholar]
- 39*.Park NJ, Yu T, Nabili V, Brinkman BMN, Henry S, Wang J, Wong DT. RNAprotect Saliva: An optimal room-temperature stabilization reagent for the salivary transcriptome. Clin. Chemistry. 2006;52:2303–2304. doi: 10.1373/clinchem.2006.075598. * This is a short but important technical paper related to the stabilization and long run storage of salivary mRNA samples. [DOI] [PubMed] [Google Scholar]
- 40*.Kang J-G, Kim H, Ahn T-Y. Bacterial diversity in the human saliva from different ages. J. Microbiol. 2006;44:572–576. * This important paper is dedicated to uncover the bacterial constituents of normal oral microbiota in healthy subjects, and as such it is unique. [PubMed] [Google Scholar]
- 41.Moore WE, Moore LV. The bacteria of periodontal diseases. Periodontol 2000. 1994;5:66–77. doi: 10.1111/j.1600-0757.1994.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 42.Kolenbrander PE. Oral microbial communities: biofilms, interactions, and genetic systems. Annu. Rev. Microbiol. 2000;54:413–437. doi: 10.1146/annurev.micro.54.1.413. [DOI] [PubMed] [Google Scholar]
- 43.Paster BJ, Boches SK, Galvin JL, Ericson RE, Lau CN, Levanos VA, Sahasrabudhe A, Dewhirst FE. Bacterial diversity in human subgingival plaque. J. Bacteriol. 2001;183:3770–3783. doi: 10.1128/JB.183.12.3770-3783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li Y, Ku CYS, Xu J, Saxena D, Caufield PW. Survey of oral microbial diversity using PCR-based denaturing gradient gel electrophoresis. J. Dent. Res. 2005;84:559–564. doi: 10.1177/154405910508400614. [DOI] [PubMed] [Google Scholar]
- 45.Sakamoto M, Huang Y, Ohnishi M, Umeda M, Ishikawa I, Benno Y. Changes in oral microbial profiles after periodontal treatment as determined by molecular analysis of 16s rRNA genes. J. Med. Microbiol. 2004;53:563–571. doi: 10.1099/jmm.0.45576-0. [DOI] [PubMed] [Google Scholar]
- 46.Kroes I, Lepp PW, Relman DA. Bacterial diversity within the human subgingival crevice. Proc. Natl. Acad. Sci. USA. 1999;96:14547–14552. doi: 10.1073/pnas.96.25.14547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Becker MR, Paster BJ, Leys EJ, Moeschberger ML, Kenyon SG, Galvin JL, Boches SK, Dewhirst FE, Griffen AL. Molecular analysis of bacterial species associated with childhood caries. J. Clin. Microbiol. 2002;40:1001–1009. doi: 10.1128/JCM.40.3.1001-1009.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Munson MA, Banerjee A, Watson TF, Wade WG. Molecular analysis of the microflora associated with dental caries. J. Clin. Microbiol. 2004;42:3023–3029. doi: 10.1128/JCM.42.7.3023-3029.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 2005;43:5721–5732. doi: 10.1128/JCM.43.11.5721-5732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50**.Li Y, Ge Y, Saxena D, Caufield PW. Genetic profiling of the oral microbiota associated with severe early-childhood caries. J. Clin. Microbiol. 2007;45:81–87. doi: 10.1128/JCM.01622-06. ** This important paper presents interesting data related to the oral microbiota, and gives example about that, how saliva analysis may improve understanding, and prevention of oral disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tenovuo J. Antimicrobial agents in saliva - Protection of the whole body. J. Dent. Res. 2002;81:807–809. doi: 10.1177/154405910208101202. [DOI] [PubMed] [Google Scholar]
- 52.Li XS, Reddy MS, Baev D, Edgerton M. Candida albicans Ssa1/2p is the cell envelope binding protein for human salivary histatin 5. J. Biol. Chem. 2003;278:28553–28561. doi: 10.1074/jbc.M300680200. [DOI] [PubMed] [Google Scholar]
- 53**.Liguori G, Lucariello A, Colella G, De Luca A, Marinelli P. Rapid identification of Candida species in oral rinse solution by PCR. J. Clin. Pathol. 2007;60:1035–1039. doi: 10.1136/jcp.2006.040782. ** This important paper is a clear indication of the importance and promising perspectives of salivary diagnostics in the clinical practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dû LD, Kolenbrander PE. Identification of saliva-regulated genes of Streptococcus gordonii DL1 by differential display using random arbitrarily primer PCR. Infect. Immun. 2000;68:4834–4837. doi: 10.1128/iai.68.8.4834-4837.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.de Jong MH, van der Hoeven JS. The growth of oral bacteria on saliva. J. Dent. Res. 1987;66:498–505. doi: 10.1177/00220345870660021901. [DOI] [PubMed] [Google Scholar]
- 56**.Boutaga K, Savelkoul PH, Winkel EG, van Winkelhoff AJ. Comparison of subgingival bacterial sampling with oral lavage for detection and quantification of periodontal pathogens by real-time polymerase chain reaction. J. Periodontol. 2007;78:79–86. doi: 10.1902/jop.2007.060078. ** This important paper gives evidences that salivary microbiota refers to periodontal microbiota, and can be used for diagnosis and monitoring of periodontal patients in a regular basis. [DOI] [PubMed] [Google Scholar]
- 57.Lemos JAC, Chen Y-YM, Burne RA. Genetic and physiologic analysis of the groE operon and role of the HrcA repressor in stress gene regulation and acid tolerance in Streptococcus mutans. J. Bacteriol. 2001;183:6074–7084. doi: 10.1128/JB.183.20.6074-6084.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li C, Ha T, Ferguson Jr DA, Chi DS, Zhao R, Patel NR, Krishnaswamy G, Thomas E. A newly developed PCR assay of H. pylori in gastricbiopsy, saliva, and feces. Evidence of high prevalence of H. pylori in saliva supports oral transmission. Dig. Dis. Sci. 1996;41:2142–2149. doi: 10.1007/BF02071393. [DOI] [PubMed] [Google Scholar]
- 59.Dal Bello F, Hertel C. Oral cavity as natural reservoir for intestinal lactobacilli. Systematic and Applied Microbiology. 2006;29:69–76. doi: 10.1016/j.syapm.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 60.Starke EM, Smooth JC, Wu JH, Liu WT, Chandler D, Stahl DA. Saliva-based diagnostics using 16S rRNA microarrays and microfluidics. Ann. N.Y. Acad. Sci. 2007;1098:345–361. doi: 10.1196/annals.1384.007. [DOI] [PubMed] [Google Scholar]
- 61.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 62.Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Human gut microbes associated with obesity. Nature. 2006;444:1022–1023. doi: 10.1038/4441022a. [DOI] [PubMed] [Google Scholar]
- 63.Li Y, St John MAR, Zhou X, Kim Y, Sinha U, Jordan RCK, Eisele D, Abemayor E, Elashoff D, Park N-H, Wong DT. Salivary transcriptome diagnostics for oral cancer detection. Clin. Cancer. Res. 2004;10:8442–8450. doi: 10.1158/1078-0432.CCR-04-1167. [DOI] [PubMed] [Google Scholar]
- 64.Liao PH, Chang YC, Huang MF, Tai KW, Chou MY. Mutation of p53 gene codon 63 in saliva as a molecular marker for oral squamous cell carcinomas. Oral. Oncol. 2000;36:272–276. doi: 10.1016/s1368-8375(00)00005-1. [DOI] [PubMed] [Google Scholar]
- 65.Kim MM, Clinger JD, Masayesva BG, Ha PK, Zahurak ML, Westra WH, Califano JA. Mitochondrial DNA quantity increases with hystopathologic grade in premalignant and malignant head and neck lesions. Clin. Cancer Res. 2004;10:8512–8515. doi: 10.1158/1078-0432.CCR-04-0734. [DOI] [PubMed] [Google Scholar]
- 66.Jiang WW, Masayesva B, Zahurak M, Carvalho AL, Rosenbaum E, Mambo E, Zhou S, Minhas K, Benoit N, Westra HW. Increased mitochondrial DNA content in saliva associated with head and neck cancer. Clin. Cancer Res. 2005;11:2486–2491. doi: 10.1158/1078-0432.CCR-04-2147. [DOI] [PubMed] [Google Scholar]
- 67.Jiang WW, Rosenbaum E, Mambo E, Zahurak M, Masayesva B, Carvalho AL, Zhou S, Westra WH, Alberg AJ. Decreased mitochondrial DNA content in posttreatment salivary rinses from head and neck cancer patients. Clin. Cancer Res. 2006;12:1564–1569. doi: 10.1158/1078-0432.CCR-05-1471. [DOI] [PubMed] [Google Scholar]
- 68.Zhao M, Rosenbaum E, Carvalho AL, Koch W, Jiang WW, Sidransky D, Califano J. Feasibility of quantitative PCR-based saliva rinse screening of HPV for head and neck cancer. Int. J. Cancer. 2005;117:605–610. doi: 10.1002/ijc.21216. [DOI] [PubMed] [Google Scholar]
- 69.Matičič M, Poljak M, Kramar B, Tomažič J, Vidmar L, Zakotnik B, Skalerič U. Proviral HIV-1 DNA in gingival crevicular fluid of HIV-1-infected patients in various stages of HIV disease. J. Dent. Res. 2000;79:1496–1501. doi: 10.1177/00220345000790071101. [DOI] [PubMed] [Google Scholar]
- 70.Vieira J, Huang M-L, Koelle DM, Corey L. Transmissible Kaposi's sarcoma-associated Herpesvirus (Human herpesvirus 8) in saliva of men with a history of Kaposi's sarcoma. J. Virol. 1997;71:7083–7087. doi: 10.1128/jvi.71.9.7083-7087.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li Y, Elashoff D, Oh M, Sinha U, St John MAR, Zhou X, Abemayor E, Wong DT. Serum circulating human mRNA profiling and its utility for oral cancer detection. J. Clin. Oncol. 2006;24:1754–1760. doi: 10.1200/JCO.2005.03.7598. [DOI] [PubMed] [Google Scholar]
- 72.Koperski MS, Benko FA, Gocke CD. Circulating RNA as a tumor marker: Detection of 5T4 mRNA in breast and lung cancer patient serum. Ann. N.Y. Acad. Sci. 2001;945:172–178. [PubMed] [Google Scholar]
- 73.Bunn Jr PJ. Early detection of lung cancer using serum RNA or DNA markers: Ready for "prime time" or for validation? J. Clin. Oncol. 2003;21:3891–3893. doi: 10.1200/JCO.2003.07.976. [DOI] [PubMed] [Google Scholar]
- 74.Mizukawa N, Sugiyama K, Fukunaga J, Ueno T, Mishima K, Takagi S, Sugahara T. Defensin-1, a peptide detected in the saliva of oral squamous cell carcinoma patients. Anticancer Res. 1998;18:4645–4649. [PubMed] [Google Scholar]
- 75.Streckfus C, Bigler L, Tucci M, Thigpen JT. A preliminary study of CA15-3, c-erbB-2, epidermal growth factor receptor, cathepsin-D, and p53 in saliva among women with breast carcinoma. Cancer Invest. 2000;18:101–109. doi: 10.3109/07357900009038240. [DOI] [PubMed] [Google Scholar]
- 76.Chien DX, Schwartz PE. Saliva and serum CA 125 assays for detecting malignant ovarian tumors. Obstet. Gynecol. 1990;75:701–704. [PubMed] [Google Scholar]
- 77.Tavassoli M, Brunel N, Maher R, Johnson NW, Soussi T. P53 antibodies in the saliva of patients with sguamous cell carcinoma of the oral cavity. Int. J. Cancer. 1998;78:390–391. doi: 10.1002/(SICI)1097-0215(19981029)78:3<390::AID-IJC23>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 78.Vitorino R, Lobo MJC, Ferrer-Correira AJ, Dubin JR, Tomer KB, Domingues PM, Amado FML. Identification of human whole saliva protein components using proteomics. Proteomics. 2004;4:1109–1115. doi: 10.1002/pmic.200300638. [DOI] [PubMed] [Google Scholar]
- 79.Huang C-M. Comparative proteomic analysis of human whole saliva. Arch. Oral. Biol. 2004;49:951–962. doi: 10.1016/j.archoralbio.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 80.Amado FM, Vitorino RM, Domingues PM, Lobo MJ, Duarte JA. Analysis of the human saliva proteome. Expert Rev. Proteomics. 2005;2:521–539. doi: 10.1586/14789450.2.4.521. [DOI] [PubMed] [Google Scholar]
- 81.Washburn MP. Utilisation of proteomics datasets generated via multidimensional protein identification technology (MudPIT). (Technical review) Brief Funct. Genomic Proteomic. 2004;3:280–286. doi: 10.1093/bfgp/3.3.280. [DOI] [PubMed] [Google Scholar]
- 82.Florens L, Washburn MP. Proteomic analysis by multidimensional protein identification technology. Methods Mol. Biol. 2006;328:159–175. doi: 10.1385/1-59745-026-X:159. [DOI] [PubMed] [Google Scholar]
- 83.Nater UM, Rohleder N, Gaab J, Simona B, Andreas J, Kirschbaum C, Ehlert U. Human salivary alpha-amylase reactivity in a psychosocial stress paradigm. Int. J. Psychophysiol. 2005;55:333–342. doi: 10.1016/j.ijpsycho.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 84.Anderson LC, Garrett JR, Johnson DA, Kauffman DL, Keller PJ, Thulin A. Influence of circulating catecholamines on protein secretion into rat parotid saliva during parasympathetic stimulation. J. Physiol. 1984;352:163–171. doi: 10.1113/jphysiol.1984.sp015284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Proctor GB, Carpenter GH, Anderson LC, Garrett JR. Nerve-evoked secretion of immunoglobulin A in relation to other proteins by parotid glands in anaesthetized rat. Exp. Physiol. 2000;85:511–518. [PubMed] [Google Scholar]
- 86.Seugnet L, Boero J, Gottschalk L, Duntley SP, Shaw PJ. Identification of a biomarker for sleep drive in flies and humans. PNAS. 2006;103:19913–19918. doi: 10.1073/pnas.0609463104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Deinzer R, Schuller N. Dynamics of stress related decrease of salivary immunoglobulin A (sIgA): relationship to symptoms of the common cold and studying behavior. Behav. Med. 1998;23:161–169. doi: 10.1080/08964289809596372. [DOI] [PubMed] [Google Scholar]
- 88.Aubert B, Cochet C, Souvignet C, Chambaz EM. Saliva from cystic fibrosis patients contains an unusual form of epidermal growth factor. Biochem. Biophys. Res. Commun. 1990;16:1144–1150. doi: 10.1016/0006-291x(90)90512-l. [DOI] [PubMed] [Google Scholar]
- 89.Zelles T, Purushotham KR, Macauley SP, Oxford GE, Humphreys-Becher MG. Saliva and growth factors. J. Dent. Res. 1995;74:1826–1832. doi: 10.1177/00220345950740120301. [DOI] [PubMed] [Google Scholar]
- 90.Nagler RM, Nagler A. The molecular basis of salivary gland involvement in graft-versus-host disease. J. Dent. Res. 2004;83:98–103. doi: 10.1177/154405910408300203. [DOI] [PubMed] [Google Scholar]
- 91.Ruyner J, Socha J, Barra E, Gregorek H, Madaliński K, Woźniewicz B, Giera B. Serum and salivary antigliadin antibodies and serum IgA anti-andomysium antibodies as a screening test for coeliac disease. Acta Paediatr. 1996;85:814–817. doi: 10.1111/j.1651-2227.1996.tb14157.x. [DOI] [PubMed] [Google Scholar]
- 92.Loeb MB, Riddel RH, James C, Hunt R, Smaill FM. Evaluation of salivary antibodies to detect infection with Helicobacter pylori. Can. J. Gastroenterol. 1997;11:437–440. doi: 10.1155/1997/294081. [DOI] [PubMed] [Google Scholar]
- 93.Feldman M, Plancarte A, Sandoval M, Wilson M, Flisser A. Comparison of two assays (EIA and EITB) and two samples (saliva and serum) for the diagnosis of neurocystercosis. Trans R. Soc. Trop. Med. Hyg. 1990;84:559–562. doi: 10.1016/0035-9203(90)90040-l. [DOI] [PubMed] [Google Scholar]
- 94.Abrams WR, Barber CA, McCann K, Tong G, Chen Z, Mauk MG, Wang J, Volkov A, Bourdelle P, Corstjens PL, Zuiderwijk M, Kardos K, Li S, Tanke HJ, Niedbala SR, Malamud D, Bau H. Development of a microfluidic device for detection of pathogens in oral samples using upconverting phosphor technology (UPT) Ann. N.Y. Acad. Sci. 2007;1098:375–388. doi: 10.1196/annals.1384.020. [DOI] [PubMed] [Google Scholar]
- 95.Watanabe T, Kawamura T, Jacob SE, Aquilino EA, Orenstein JM, Black JB, Blauvelt A. Pityriasis rosea is associated with systemic active infection with both human herpesvirus-7 and human herpesvirus-6. J. Invest. Dermatol. 2002;119:793–797. doi: 10.1046/j.1523-1747.2002.00200.x. [DOI] [PubMed] [Google Scholar]
- 96.Nishizawa T, Okamoto H, Keinishi K, Yoshizawa H, Miyakawa Y, Mayumi M. A novel DNA virus (TTV) associated with elevated transaminase levels in posttransfusion hepatitis of unknown etiology. Biochem. Biophys. Res. 1997;Commun. 241:92–97. doi: 10.1006/bbrc.1997.7765. [DOI] [PubMed] [Google Scholar]
- 97.Yan J, Chen L-l, Lou Y-L, Zhong X-Z. Investigation of HGV and TTV infections in sera and saliva from non-hepatitis patients with oral diseases. World J. Gastroenterol. 2002;8:857–862. doi: 10.3748/wjg.v8.i5.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Qureshi MN, Barr CE, Hewlitt I, Boorstein R, Kong F, Bagasra O, Bobroski LE, Joshi B. Detection of HIV in oral mucosal cells. Oral Dis. 1997;3(Suppl-1):S73–78. doi: 10.1111/j.1601-0825.1997.tb00380.x. [DOI] [PubMed] [Google Scholar]
- 99.Seemayer CA, Viazov S, Philipp T, Roggendorf M. Detection of GBV-C/HGV RNA in saliva and serum, but not in urine of infected patients. Infection. 1998;26:39–41. doi: 10.1007/BF02768751. [DOI] [PubMed] [Google Scholar]
- 100.Rey D, Fritsch S, Schmitt C, Meyer P, Lang JM, Stoll-Keller F. Quantitation of hepatitis C virus RNA in saliva and serum of patients coinfected with HCV and human immunodeficiency virus. J. Med. Virol. 2001;63:117–119. [PubMed] [Google Scholar]
- 101.Shugars DC, Patton LL, Freel SA, Gray LR, Vollmer RT, Eron Jr JJ, Fiscus SA. Hyper-excretion of human immunodeficiency virus type 1 RNA in saliva. J. Dent. Res. 2001;80:414–420. doi: 10.1177/00220345010800020301. [DOI] [PubMed] [Google Scholar]
- 102.Cuzzubbo AJ, Vaughn DW, Nisalak A, Suntayakorn S, Aaskov J, Devine PL. Detection of specific antibodies in saliva during dengue infection. J. Clin. Microbiol. 1998;36:3737–3739. doi: 10.1128/jcm.36.12.3737-3739.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ochnio JJ, Scheifele DW, Ho M, Mitchell LA. New, ultra-sensitive enzyme immunoassay for detecting vaccine- and disease-induced hepatitis A virus-specific immunoglobulin G in saliva. J. Clin. Microbiol. 1997;35:98–101. doi: 10.1128/jcm.35.1.98-101.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Thieme T, Yoshihara P, Piacentini S, Beller M. Clinical evaluation of oral fluid samples for diagnosis of viral hepatitis. J. Clin. Microbiol. 1992;30:1076–1079. doi: 10.1128/jcm.30.5.1076-1079.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.El-Medany OM, El-Din Abdel Wahab KS, Abu Shady EA, Gad Elhak N. Chronic liver disease and hepatitis C virus in Egyptian patients. Hepatogastroenterology. 1999;46:1895–1903. [PubMed] [Google Scholar]
- 106.Tamashiro H, Constantine NT. Serological diagnosis of HIV infection using oral fluid samples. Bull. World Health Org. 1994;72:135–143. [PMC free article] [PubMed] [Google Scholar]
- 107.Tess BH, Granato C, Parry JV, Santos VA, Lago TG, Newell ML. Salivary testing for human immunodeficiency virus type 1 infection in children born to infected mothers in São Paolo, Brazil. The São Paolo collaborative study for vertical transmission of HIV-1. Pediatr. Infect. Dis. J. 1996;15:787–790. doi: 10.1097/00006454-199609000-00010. [DOI] [PubMed] [Google Scholar]
- 108.Emmons W. Accuracy of oral specimen testing for human immunodeficiency virus. Am. J. Med. 1997;102:15–20. doi: 10.1016/s0002-9343(97)00033-8. [DOI] [PubMed] [Google Scholar]
- 109.Malamud D. Oral diagnostic testing for detecting human immunodeficiency virus-1 antibodies: a technology whose time has come. Am. J. Med. 1997;102:9–14. doi: 10.1016/s0002-9343(97)00032-6. [DOI] [PubMed] [Google Scholar]
- 110.Thieme T, Piacentini S, Davidson S, Steingart K. Determination of measles, mumps, and rubella immunization status using oral fluid samples. J. Am. Med. Assoc. 1994;272:219–221. [PubMed] [Google Scholar]
- 111.Rice PS, Cohen BJ. A school outbreak of parvovirus B19 infection investigated using salivary antibody assays. Epidemiol. Infect. 1996;116:331–338. doi: 10.1017/s0950268800052651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chaita TM, Graham SM, Maxell SM, Sirivasin W, Sabchareon A, Beeching NJ. Salivary sampling for hepatitis B surface antigen carriage: a sensitive technique suitable for epidemiological studies. Ann. Trop. Paediatr. 1995;15:135–139. doi: 10.1080/02724936.1995.11747761. [DOI] [PubMed] [Google Scholar]
- 113.Vitorino R, Lobo MJC, Duarte JR, Ferrer-Correia AJ, Domingues PM, Amado FML. The role of salivary peptides in dental caries. Biomed. Chromatog. 2005;19:214–222. doi: 10.1002/bmc.438. [DOI] [PubMed] [Google Scholar]
- 114.Klock B, Svanberg M, Petersson LG. Dental caries, mutans streptococci, lactobacilli, and saliva secretion rate in adults. Community Dent. Oral Epidemiol. 1990;18:249–252. doi: 10.1111/j.1600-0528.1990.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 115.Kohler B, Bjarnason S. Mutans streptococci, lactobacilli and caries prevalence in 15 to 16-year olds in Göteborg Part II. Swed. Dent. J. 1992;16:253–259. [PubMed] [Google Scholar]
- 116.Van Houte J, Jordan HV, Laraway R, Kent R, Soparkar PM, DePaola PF. Association of the microbial flora of dental plaque and saliva with human root-surface caries. J. Dent. Res. 1990;69:1463–1468. doi: 10.1177/00220345900690080301. [DOI] [PubMed] [Google Scholar]
- 117.Chen Z, Mauk MG, Wang J, Abrams WR, Corstjens PL, Niedbala RS, Malamud D, Bau HH. A microfluidic system for saliva-based detection of infectious diseases. Ann. N.Y. Acad. Sci. 2007;1098:429–436. doi: 10.1196/annals.1384.024. [DOI] [PubMed] [Google Scholar]
- 118.Asikainen S, Alauusua S, Saxen L. Recovery of Actinomycetemcomitans from teeth, tongue, and saliva. J. Periodontol. 1991;62:203–206. doi: 10.1902/jop.1991.62.3.203. [DOI] [PubMed] [Google Scholar]
- 119.Umeda M, Contreras A, Chen C, Bakker I, Slots J. The utility of whole saliva to detect the oral presence of periodontopathic bacteria. J. Periodontol. 1998;69:828–833. doi: 10.1902/jop.1998.69.7.828. [DOI] [PubMed] [Google Scholar]
- 120.Petit MDA, Wassenaar A, van der Velden U, van Eden W, Loos BG. Depressed responsiveness of peripheral blood mononuclear cells to heat-shock proteins in periodontitis patients. J. Dent. Res. 1999;78:1393–1400. doi: 10.1177/00220345990780080401. [DOI] [PubMed] [Google Scholar]
- 121.Lopatin DE, Shelburne CE, Van Poperin N, Kowalski CJ, Bagramian RA. Humoral immunity to stress proteins and periodontal disease. J. Periodontol. 1999;70:1185–1193. doi: 10.1902/jop.1999.70.10.1185. [DOI] [PubMed] [Google Scholar]
- 122.Hicks MJ, Carter AB, Rossmann SN, Demmler GJ, Simon CL, Cron SG, Flaitz CM, Shearer WT, Kline MW. Detection of fungal organisms in saliva from HIV-infected children: a preliminary cytologic analysis. Pediatr. Dent. 1998;20:162–168. [PubMed] [Google Scholar]
- 123.Bergmann OJ. The demonstration of candidal pseudohyphae in salivary smears as a method of early diagnosis of oral candidiasis in patients with acute myeloid leukemia. Oral. Microbiol. Immunol. 1996;11:362–364. doi: 10.1111/j.1399-302x.1996.tb00195.x. [DOI] [PubMed] [Google Scholar]