Abstract
A family history of atherosclerosis is independently associated with an increased incidence of cardiovascular events. The genetic factors underlying the importance of inheritance in atherosclerosis are starting to be understood. Genetic variation, such as mutations or common polymorphisms has been shown to be involved in modulation of a range of risk factors, such as plasma lipoprotein levels, inflammation and vascular calcification. This review presents examples of present studies of the role of genetic polymorphism in atherosclerosis.
Key Words: Atherosclerosis, genetic polymorphism, risk factors.
INTRODUCTION
Atherosclerosis and the complications of this disease are the leading cause of disability and death in Western societies. The development of advanced atherosclerosis is a slow progressive process that starts in childhood and remains asymptomatic for many decades, with complications such as myocardial infarction, stroke or peripheral ischaemia usually occurring in later life [1]. Recognised risk factors for the development of atherosclerosis include hypertension, diabetes, dyslipidaemia, obesity, smoking, ageing and sedentary life style [2, 3]. Twin studies have suggested that the heritability of coronary atherosclerosis based on fatal cardiac events is between 38 and 57% [4, 5]. Epidemiology studies suggest that a positive family history is independently associated with the incidence of cardiovascular events [6]. Besides major genetic determinants of traditional cardiovascular risk factors, such as those influencing the lipid profile, it is likely that a large number of additional genetic factors interact with environmental factors to determine overall cardiovascular risk. Development of molecular biology techniques has promoted identification of these candidate genes by using high-throughput technologies, such as genome-wide scans. This review provides examples of advances in our understanding of the role of the genomic variations in atherosclerosis and candidate genes which have been related to atherosclerosis.
CONSIDERATIONS IN GENOME STUDIES
The methods used to examine genetic factors involved in chronic diseases such as atherosclerosis are evolving rapidly. Traditionally studies have centred on examining sub-population where the early onset of presentation, presence of multiple affected family members and mode of inheritance suggest a very important role for genetics in the development of the disease. Using techniques such as affected-relative pair linkage analysis it is possible to identify genomic regions in which a single gene involved in the disease may be located. In most chronic diseases however it is likely that multiple genes acting in concert under the influence of a range of environmental factors determine development of diseases, such as atherosclerosis. The identification of these genes has mainly followed a candidate gene approach. Based on understanding of the pathogenesis of atherosclerosis genes involved in control lipid mobilisation, inflammation and endothelial function for example have been examined for association with atheroma presence or cardiovascular events. The selection of which sites of genetic variation within the genes to examine is complex depending on frequency of the variation, sample size or power, estimated functional effect and ability to predict other related genetic polymorphisms [7]. Over the last few years with the rapid advances in genotyping there has been the introduction of genome wide association studies. This approach uses a screening rationale to examine up to 1 million allelic variations in large numbers of samples from cases and controls. The approach generates enormous data set which will ultimately enable analysis of epigenetic interaction and environmental responsive loci. At present our ability to analyse such data sets is relatively rudimentary.
In this review we will mainly discuss examples of the candidate gene approach since this has been the main technique applied. The selection of genes has been primarily based on our present understanding of the biology of atherosclerosis from in vitro, animal and pathological studies. An important issue in association studies is whether the correct allelic variation site in the gene of interest has been examined. Given the enormous number of variation even within a single gene it is usually not possible to examine every one. The size of cohort required for sufficient power to detect likely influence of a single genetic variation is very dependant on the frequency of the minor allele within the population being studied. For polymorphisms imparting a relative risk of 1.5 or less minor allele frequencies >5% are required for most achievable samples sizes [8]. Thus it is usual to target variations which are more common. Since a number of allelic variations are inherited together another important way of minimising the number of variations genotyped is by selected those which are maximally linked to other common sequence changes. It has been demonstrated that the human genome can be organized into haplotype blocks i.e. regions of strong linkage disequilibrium (LD) separated by regions of low level LD [9-13]. The availability of detailed linkage information on different populations, such as that presented in HapMap (The International HapMap Consortium 2007 [14]), allows researchers to select tagging single nucleotide polymorphisms and assesses different combinations of polymorphisms or haplotypes. Another consideration in the selection of the allelic variations to be examined is its functional effect. Databases, such as PANTHER (Protein ANalysis THrough Evolutionary Relationships) gene ontology database [15] can be utilised to provide estimates of the functional effects of allelic variations. PANTHER uses subSPEC (substitution position-specific evolutionary conservation) score to predict the probability (Pdeleterious) that a given coding variant will cause a deleterious functional change, such that a subPSEC score of -3 corresponds to a Pdeleterious of 0.5 [16, 17].
A number of issues are raised in the selection of cases and controls for association studies, such as what criteria are used to define cases (e.g. history, documented events, imaging), are controls from the same populations and has atherosclerosis been excluded thoroughly (history or imaging) [18].
GENETIC VARIANTS IN LIPOPROTEIN METABOLISM
Aberrations in lipid handling are one of the fundamental mechanisms that have been linked to atherosclerosis, particularly in patients presenting with positive family history and at younger age [19]. About three quarters of low density lipoprotein (LDL) in the blood stream is taken up by hepatic or peripheral cells via LDL receptors (LDLR) on the cell surface. These receptors recognize apolipoprotein B and apolipoprotein E with high affinity. In hepatocytes, the absorbed LDL is reused for lipoprotein synthesis and excess cholesterol is secreted into bile. In non-hepatic cells, the absorbed LDL supplies the cholesterol content essential for cell function.
There is also reverse transport of excess cholesterol from the periphery back to the liver by high density lipoprotein (HDL) secreted by liver as nascent pre β-HDL. Cholesterol efflux into mature HDL (HDL-C) is mediated by the ATP-binding cassette (ABC) transporter family of membrane proteins, especially ABCA1. HDL-C can then return to the liver via a hepatocyte scavenger receptor (SCARB1). In the liver, cholesterol can be stored within hepatocytes, converted into bile acids by the cytochrome P450 member CYP7A1 (7-α-hydroxylase), or transported directly by ABCG5 and ABCG8 transporters. There is accumulated evidence that impaired homeostasis in these processes has a strong genetic background [20, 21].
Low-Density Lipoprotein Receptor Gene (LDLR)
Familial hypercholesterolemia (FH) is a monogenic autosomal codominant trait affecting 1 in 500 individuals in Caucasian populations [19] with an estimated world prevalence of about 0.2% [22]. FH is characterized by elevated plasma cholesterol bound to LDL (LDL-C) due to a deficiency in LDLR activity on the cell surfaces [23].
LDLR is located on chromosome 19 [24] at 19p13.1-p13.3 [23] and encodes a protein of 860 amino acids [25]. There are more than 800 different allelic variations in this gene described [26-30], which have been divided into 5 classes according to the effect they have on LDLR function [26]. Class 1 mutations lead to an inability to produce immunoprecipitable protein (receptor-negative mutations), whereas classes 2-5 affect function of the receptor (receptor-defective mutations). FH heterozygotes express half the normal number of functional LDLR on their cell surfaces leading to a twofold elevation in circulating LDL-C concentration (300-500 mg/dL) associated with premature atherosclerosis development [19]. The rare FH homozygotes (1 in 1,000,000) express only few or no functional receptors on their cell surfaces. These individuals have plasma LDL-C of 600-1,200 mg/dL and may suffer fatal heart attacks before the age of 20 (reviewed in [19]).
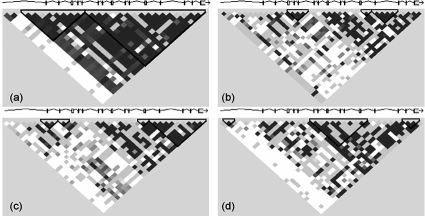
There is promising evidence that DNA polymorphisms within LDLR could be useful to monitor the inheritance of FH. Most association studies confirm the link between the restriction fragment length polymorphisms (RFLPs) in LDLR exon 12 or 13 and FH [31-34]. Two research groups reported strong linkage disequilibrium of two microsatellite markers (D19S394 and D19S221) to the most common LDLR mutations (p.C152R, p.S265R, p.V408M and p.G528D), accounting for 20% and 60% of FH heterozygotes, respectively [35]; [36]. On the other hand, there is some consideration to generalize these polymorphisms as molecular markers for FH. At least, the data are based on individuals of different ethnic origin. The comparisons of haplotypes found in subjects of diverse ethnicity suggest heterogeneity among populations. For example, by using the LDLR HapMap genotype data [14], there were found distinct haplotype block patterns in four different populations (Fig. 1). To monitor the inheritance of FH by using the common LDLR genetic variations, it is necessary to establish the panel of informative polymorphisms for any population of interest.
Fig. (1).
Complex correlation structure to the HapMap genotype data at LDLR gene locus (19p13.2) in four populations.
(a) Utah residents with ancestry from northern and western Europe, (b) Han Chinese in Beijing (China), (c) Japanese in Tokyo (Japan), (d) Yoruba in Ibadan (Nigeria).
Apolipoprotein B Gene (APOB)
Human APOB is located on the short arm of chromosome 2 [37] at 2p24-p23 [38] and codes for the main apolipoprotein of chylomicrons and LDL. The protein occurs in plasma in two main isoforms via a unique mRNA editing process: intestinal apoB-48 and hepatic apoB-100. ApoB-48 is identical to the N-terminal 48% of full-length apoB-100 [39, 40]. Two genetic disorders, familial hypobetalipoproteinemia (FHBL) and familial ligand-defective apoB-100 (FDB) are attributable to mutations in the APOB gene. FHBL is an autosomal dominant trait characterized by low plasma levels of total cholesterol (TC), LDL-C, and apoB. FDB is an autosomal dominant disorder accompanied by hypercholesterolemia and premature atherosclerosis [41]. Mutations within APOB cause the production of truncated proteins (between apoB-4.6 to apoB-89) and can be responsible for FHBL (reviewed in [42]). Defects in the C-terminus of the apoB LDLR-binding domain are accountable for FDB, which is clinically indistinguishable from FH [43].
The amino acid substitution p.R3500Q has been found to be strongly associated with hypercholesterolemia and FDB [41-46]. The frequency of p.R3500Q in Europe is about 0.09% [47, 48]. The sequence variation p.R3531C impairs LDLR binding capacity up to 49% of normal and increases LDL-C concentration in plasma [49]. The p.R3480W substitution leads to impaired binding to LDLR [50].
APOB is highly polymorphic gene with more than 80 allelic variations within its entire sequence and other common genetic variants. For example, the APOB signal peptide exhibits variability in length (24 or 27 amino acids) due to the insertion (ins allele) or deletion (del allele) of three codons [51-53]. The frequency of del allele is about 30% in Caucasians [54] and has been associated with altered plasma total cholesterol and LDL-C levels in different ethnic groups [55-60] but interestingly not with the risk of vascular diseases [54]. Thus variation at the apoB gene may act in pathogenesis of vascular diseases through mechanisms not directly related to effects on measured lipid traits. Linkage analysis of quantitative trait loci (QTL) associated with increased plasma levels of apoB protein provided evidence for chromosomal segments at 1p21-31 and 17p11-q21 with LOD scores 2.2 and 3.7, respectively [61] in familial combined hyperlipidemia (FCHL) patients. While linkage peak on chromosome 1 fits to the dietary energy and nutrient intake linkage peak [62]; the peak at chromosome 17 corelates to QTL for type 2 diabetes [63] and blood pressure variation and hypertension [64, 65]; all risk factors for cardiovascular diseases.
Several restriction fragment length polymorphisms (RFLP) and variable number of tandem repeats (VNTR) polymorphisms have also been described within APOB coding as well as 3’-untranslated region (3’-UTR), [66, 67]. Studies examining the association of these common genetic variations in APOB with atherosclerosis have led to inconsistent findings [68-72].
Apolipoprotein E Gene (APOE)
APOE is a key protein of the lipid-transporting system [73, 74], regulating serum cholesterol [75], and participating in formation of high density lipoprotein (HDL) particles [76]. Hepatic parenchymal cells mediate production of all peripheral APOE [73]. APOE-containing particles are rapidly removed from the circulation by binding to LDLR or LDLR-like protein receptor (LRP)-mediated endocytosis in the liver [77-79].
APOE is mapped to chromosome 19 at 19q13.2 [80]; [81] where it is linked to apolipoprotein C1 and C2 [82]. APOE has four exons and three introns [83]. The gene is polymorphic with three major alleles (APOE2, APOE3, and APOE4) translating into three protein isoforms ε2, ε3, and ε4 [84-86]. They differ from each other only by single amino acid substitutions at residues 112 and 158 [87, 88]. The most common variant is ε3 (~78% in Caucasians; [89]) and carries cysteine and arginine at position 112 and 158, respectively. Minor molecular change has profound pathological consequences. While E3 allele codes for wild-type protein (Cys112/Arg158), E2 (Cys112/Cys158) is associated with type III hyperlipoproteinemia (HPL III), and allele E4 (Arg112/Arg158) has been implicated in atherosclerosis [90, 91].
Other polymorphisms like g.491A>T, g.427C>T, g.219G>T found within the APOE promoter [92, 93] and coding g.113G>C [94] regions have been linked with atherosclerosis. Regarding the APOE promoter g.491A>T SNP, circulating APOE concentrations are elevated in TT homozygotes compared to individuals bearing AA genotype [95]. The APOE promoter g.219G>T and coding g.113G>C allelic variations have been associated with changes in LDL-C and total cholesterol (TC) concentrations [96]. Present evidence suggests that the influence of other APOE genetic variants is small by comparison to its major alleles (E2, E3, and E4).
ATP Binding Cassette Transporter 1 Gene (ABCA1)
ABCA1 functions as a cholesterol efflux pump in the apolipoprotein mediated cellular lipid removal pathway [97]. Specifically, ABCA1 mediates the transport of cholesterol from cells to lipid-poor apolipoprotein (apo) A-I, the major HDL protein (reviewed in [98]); [99]. Mutations within the ABCA1 gene explained the molecular basis of Tangier disease, the autosomal codominant trait characterized by reduced serum HDL (<5mg/dL) and subsequent premature coronary atherosclerosis [100-102]. Disease causative mutations (e.g. g.3283_3284delTC in exon 22; [103]) have led to the hypothesis that common polymorphisms in ABCA1 control serum lipoprotein levels as a risk factor of atherosclerosis in the general population. ABCA1 is mapped to chromosome 9 at 9q31.1 [104] and displays multiple common variations within its sequence. Some of these polymorphisms correlate to circulating lipid or lipoprotein levels [105-110].
Among major lipid-relevant genes, ABCA1 haplotypes influence HDL and LDL/HDL ratio by only 10% and 4%, respectively [111]. Thus, it is not surprising that other studies by Zwarts et al. [108] and Tregouet et al. [112] (ECTIM - Etude Cas-T´emoins de l’Infarctus du Myocarde study) reported that ABCA1 polymorphisms are associated with the frequency and severity of coronary events independent of changes in the circulating lipoprotein levels. Promoter as well as 5’-UTR variants have been associated with multiple increases in coronary events and severity of coronary artery disease.
CYP7A1 Gene
This gene codes for a member of the cytochrome P450 superfamily of enzymes and is located on chromosome 8 at 8q11-q12 [113]. CYP7A1 is one of the critical genes playing a role in the classical pathway of cholesterol conversion into bile acids (reviewed in [114]). Genetic variations in CYP7A1 have been extensively studied and associated with hypercholesterolaemia in some [115-118] but not all studies [119, 120]. When association was reported, it consistently related to the promoter region of the gene. There is not any common non-synonymous polymorphism within its coding sequences, except the exon 3 c.762A>G with the estimated frequency of heterozygosity at about 0.006. While it is not known any functional variants of this polymorphism, it can not be excluded that there is another close-linked gene with common polymorphisms that is involved in the control of plasma lipids. Gene layout around the CYP7A1 locus indicates for syntenin (SDCBP), the gene coding for protein with pleiotropic functions, including the cell signalling and lipid metabolism.
ABCG5/ABCG8 Locus
ATP-binding cassette sub-family G members 5 and 8 (ABCG5 and ABCG8) are tandemly arranged in a head-to-head orientation on chromosome 2p21 [121, 122]. The ABC transporters, ABCG5 (sterolin-1) and ABCG8 (sterolin-2) function in trafficking of all sterols, including cholesterol [123]. Multiple mutations in either ABCG5 or ABCG8 may result in sitosterolaemia [124-127]; a rare autosomal recessive trait characterized by increased intestinal absorption and decreased biliary excretion of sterols. Subjects with this disorder develop premature coronary atherosclerosis [128]. Genetic polymorphisms within the sitosterolaemia locus explain inter-individual differences in sterol metabolism and plasma sitosterol [129]. Polymorphic variants p.Q604E (ABCG5), p.D19H and p.T400K (ABCG8) have been associated with plasma plant sterols and lipid levels in normocholesterolaemic individuals or mildly hypercholesterolaemic patients [130-133]. Variant p.M429V (ABCG8) was linked to higher cholesterol absorption efficiency in hypercholesterolaemic patients [134]. Pandit et al. [135] published a detailed haplotype map of the sitosterolaemia locus. They found ABCG8 gene to be more polymorphic than ABCG5. Some of allelic variations were in strong LD and very unique to different ethnic groups. A polymorphism in ABCG8 has been linked to the response of serum LDL cholesterol to atorvastatin therapy [136]. This is an example of how genetic variability can influence the outcome of treatment of atherosclerosis not just its development.
SCARB1 Gene
Scavenger receptors (SRs) are receptors for modified forms of lipoproteins including oxidized and acetylated LDL (ox-LDL and ac-LDL), lipopolysaccharides (LPS) of Gram-negative bacteria, and other poly-anionic ligands [137, 138]. They are divided into eight classes (A-H) and the majority of them are expressed on the surface of antigen presenting cells – APC [139]. Several informative sequence variations have been found within the member of the scavenger receptors gene family B, scavenger receptor class B type 1 gene (SCARB1). This gene spans approximately 75kb on chromosome 12 at 12q24.31 [140, 141]. Allelic variations within the coding sequence of the SCARB1 gene have been found in exons 1 and 8 [142, 143]. Both polymorphisms exhibit anti-atherogenic properties and the phenotype seems to vary with gender. While exon 1 variant was associated with increased HDL-C and lower LDL-C in men, exon 8 variation was linked to lower LDL-C concentrations in women [142, 144]. Exon 8 allelic variation has no impact on amino acid sequence and is believed to be in linkage disequilibrium with other functional mutations within SCARB1 or adjacent loci at 12q24 chromosomal region. Other putative susceptibility genes in this region include TP53 regulated inhibitor of apoptosis 1 (TRIAP1) and ATP-binding cassette sub-family B member 9 (ABCB9).
Other Loci Controlling Lipid Metabolism
Several genome-wide linkage scans have been performed to detect quantitative trait loci (QTLs) regulating lipid or lipoprotein metabolism. As the most significant results, these studies identified linkage between 19p13 (LOD score 3.00) and plasma cholesterol concentration [145]. Chromosomes 16q23.1-24.2 (LOD score 3.73), [146], 12q14.1 (LOD score 4.06), [147] and 15q21 (LOD score 4.77), [148] were linked to HDL-C. While sequences at 1q43, 11q23.2, 15q25.1 and 19q13.32 (LOD scores 2.50, 3.22, 3.11 and 3.59), [147] and 1p33-35 (LOD score 3.60), [149] were linked with LDL-C. Chromosomal segments at 15q12-q13.1 (LOD score 3.88), [150] and 7q36 (LOD score 2.98), [151] linked to TG.
Several prominent candidate genes residing within these linkage regions are shown in Table 1. Among them, mutations in proprotein convertase subtilisin/kexin type 9 (PCSK9) gene and low density lipoprotein receptor adaptor protein (LDLRAP1) gene (encoding a protein required for clathrin-mediated internalization of the LDL receptor by liver cells) have already been reported to affect LDLR pathway. Recent data indicates that about ten PCSK9 mutations are associated with hypercholesterolemic or hypocholesterolemic phenotype [152-156]. Recessive null mutations within LDLRAP1 were observed to co-segregate with hypercholesterolemia [157] that is particularly common in Sardinia [158], presumably because of the founder effect.
Table 1.
Candidate Genes within Chromosomal Linkage Regions Involved in Lipoprotein Metabolism
| Ref. | Subjects | Ethnicity | Linkage Site | LOD | Related Phenotype | Candidate Gene(s) |
|---|---|---|---|---|---|---|
| [147] | Obese families | Caucasian | 12q14.1 | 4.06 | HDL-C | SOAT2, APOF, CYP27B1 |
| [224] | Population based study | Caucasian | 5p13.1 | 3.64 | HDL-C | |
| [146] | Population based study | Mexican Americans | 16q23.1-24.2 | 3.73 | HDL-C | LCAT |
| [225] | Familial combined hyperlipidemia | Caucasian | 3p14 | 3.00 | HDL-C | ACOX2 |
| [148] | Population based study | Caucasian | 15q21 | 4.77 | HDL-C | LIPC |
| [226] | Low HDL-C families | Caucasian | 8q23 | 4.70 | HDL-C | |
| [147] | Obese families | Caucasian | 1q43 11q23.2 15q25.1 19q13.32 |
2.50 3.22 3.11 3.59 |
LDL-C |
ABCB10, GGPS1 ACAT1, APOA1, APOC3 CYP11A LRP3, APOE,LIPE,APOC1 |
| [227] | Type 2 diabetes families | Caucasian | 3p25 2p23 19p13 |
2.47 2.17 2.23 |
LDL-C |
PPARG APOB, LPIN1, ABCG5, ABCG8 LDLR |
| [149] | Healthy children | African Americans | 1p33-35 | 3.60 | LDL-C | PCSK9, LDLRAP1, CYP4A11 |
| [147] | Obese families | Caucasian | 2p14 11p13 11q24.1 |
1.75 | TG |
FABP1 ABCC8, LRP4 ACAT1, APOA1, APOC3, ACAD8 |
| [228] | Hypertriglyceridemic families | Caucasian | 15q21-q24 | 2.56 | TG | LIPC |
| [151] | Obese families | Caucasian | 7q36 | 2.98 | TG | INSIG1, ABCF2, FABP5L3 |
| [150] | Type 2 diabetes families | Caucasian | 15q12-q13.1 | 3.88 | TG | LIPC |
| [229] | Population based study | Caucasian | 7q32.3-qter | 2.50 | TG/HDL-C ratio | ABCF2 |
| [145] | Type 2 diabetes families | Pima Indians | 19p13 | 3.00 | TC | INSR, C3 |
SOAT2 sterol O-acyltransferase 2; APOF apolipoprotein F; CYP27B1 cytochrome P450, subfamily XXVIIB, polypeptide 1; LCAT lecithin: cholesterol acyltransferase; PLAGL1 pleomorphic adenoma gene-like 1; ACOX2 acyl-CoA oxidase 2, LIPC lipase, hepatic; ABCB10 ATP-binding cassette, subfamily B, member 10; GGPS1 geranylgeranyl diphosphate synthase 1; ACAT1 acetyl-CoA acetyltransferase 1; APOA1 apolipoprotein A-I; APOC3 apolipoprotein C-III; CYP11A cytochrome P450, subfamily XIA, polypeptide 1; LRP3 low density lipoprotein receptor-related protein 3; APOE apolipoprotein E; LIPE lipase, hormone-sensitive; APOC1 apolipoprotein C-I; PPARG peroxisome proliferator-activated receptor-gamma; APOB apolipoprotein B; ABCG5 ATP-binding cassette, subfamily G, member 5; ABCG8 ATP-binding cassette, subfamily G, member 8; LDLR low density lipoprotein receptor; PCSK9 proprotein convertase, subtilisin/kexin-type, 9; LDLRAP1 low density lipoprotein receptor adaptor protein 1; CYP4A11 cytochrome P450, subfamily IVA, polypeptide 11; FABP1 fatty acid-binding protein 1; ABCC8 ATP-binding cassette, subfamily C, member 8; LRP4 low density lipoprotein receptor-related protein 4; ACAD8 acyl-CoA dehydrogenase family, member 8; INSIG1 insulin-induced GENE 1; ABCF2 ATP-binding cassette sub-family F member 2; FABP5L3 fatty acid binding protein 5-LIKE 3; INSR insulin receptor; C3 complement component 3.
BEYOND LIPOPROTEINS
An abundance of data has shown the relationship between circulating lipoprotein variables and risk of cardiovascular events. On the other hand, half of all coronary events occur in subjects with below-average cholesterol levels [3]. In this section we discuss some other genes that have been associated with atherosclerosis. Inflammation plays an important role in the development and complications of atherosclerosis (reviewed in [2]); [159]. Monocyte-macrophage recruitment appears to be particularly important. This process engages multiple genes. As an example we highlight transforming growth factor beta 1 (TGFB1) and scavenger receptors or toll like receptor family (TLR). Calcification is another important feature of advanced atherosclerosis. We also highlight two genes linked to calcification i.e. secreted phosphoprotein 1 (SPP1), also known as osteopontin (OPN) and tumor necrosis factor receptor superfamily member 11B (TNFRSF11B), also known as osteoprotegerin (OPG). Matrix metalloproteinases have been identified in many important stages in atheroma formation including inflammation and plaque rupture [160].
Transforming Growth Factor Beta 1 Gene (TGFB1)
This gene is located on chromosome 19 at 19q13.1-q13.3 [161, 162] and codes for a pleiotropic cytokine, which regulates proliferation and differentiation of a wide variety of cell types [163]. The quantitative production of TGFB1 differs amongst individuals due to genetic polymorphism with estimated heritability of approximately 0.54 [164]. Increased plasma levels of the cytokine are associated with the T-allele of the promoter g.509C>T sequence variation due to loss of negative regulation by the complex of transcription factors AP1, JUND, and c-FOS [165]. This complex can bind TGFβ1 only when wild-type C-allele is present. The deregulation of this pathway has been suggested to play a role in mediating predisposition to various diseases, including atherosclerosis [166-169]. For example a polymorphism in TGFβ1 has been associated with stroke [170].
Toll Like Receptors (TLR) and Scavenger Receptors (SR)
Toll like receptor family contains the pattern recognition receptors (PRRs) of various pathogen-associated molecular patterns (PAMPS), [171]. There are more than ten human members of the family specialized in recognition of both endogenous and exogenous ligands [172-174]; (reviewed in [175]). Ligation of TLR4 that signals through myeloid differentiation primary response protein MyD88-dependent pathway towards the pro-inflammatory nuclear factor κB (NF-κB) signalling cascade (reviewed in [176]) has been proposed to play an important role in the initiation and progression of atherosclerosis (reviewed in [177]). TLR4 has been demonstrated in macrophages within atherosclerotic plaques and shown to be up-regulated by ox-LDL [178]. Hoebe et al. [179] demonstrated that TLRs and macrophage type A scavenger receptor (SR-A) can functionally cooperate in macrophage-bacteria interactions and signalling. Recent work by Seimon et al. [180] has revealed that macrophages in the atherosclerotic plaques apoptose when TLR4 and SR-A are activated at the same time. SR-A ligands trigger macrophage apoptosis via endoplasmic reticulum (ER)-stressed pathway by redirection of TLR4 signalling from pro-survival to pro-apoptotic. This combination of signalling can lead to plaque rupture and arterial thrombosis.
Given the role of TLRs and SRs in cell signalling, identification and functional characterization of polymorphisms in genes coding for these receptors may influences important stages of the development and complications of atherosclerosis. Common, co-segregating missense coding allelic variations in the TLR4 gene on chromosome 9q32-q33 [181] encode the p.D299G, and p.T399I substitutions that blunt receptor signalling [182]. A link between hypo-responsive TLR4 and susceptibility to cardiovascular events has been assessed in multiple association studies with variable observations. Ameziane et al. [183], Edfeldt et al. [184] and Holloway et al. [185] reported the association of TLR4 allelic variation with myocardial infarction; however other studies could not confirm these findings [186, 187]. These inconsistencies may be clarified by simultaneous examination of sequence variations with other polymorphic associates of the TLR4 physiological pathway.
The class A scavenger receptors are responsible for approximately 75% of the degradation of ox-LDL and ac-LDL [188]. Matsumoto et al. and [189] Emi et al. [190] mapped the SR-A gene on chromosome 8 to 8p22. Besides several germ-line mutations identified within this gene [191], there are more than 200 polymorphisms mapped to the entire genomic region of the SR-A including three putative non-synonymous sequence variations in exon 4 at amino acid position 105 (rs13306549), exon 5 at amino acid position 269 (rs13306543) and exon 6 at amino acid position 275 (rs3747531).
Secreted Phosphoprotein Gene (SPP1)
SPP1 is an acidic glycophosphoprotein normally found in mineralized tissues acting as an inhibitor of apatite crystal growth [192]. SPP1 has been demonstrated at sites of calcification in atherosclerotic plaques and in calcified aortic valves [193-195]. SPP1 has been implicated in a variety of mechanisms important in atherosclerosis including proliferation and migration of endothelial cells, macrophages, and vascular smooth muscle cells [196, 197].
The gene coding for SPP1 was assigned to chromosome 4q21-q25 [198]. There are more than sixty allelic variations at the SPP1 locus, including six non-synonymous variants coding for an amino acid change. Recently, Taylor et al. [199] in the CARDIA study and Brenner et al. [200] reported an SPP1 allele specific association with coronary artery calcification and stroke, respectively.
Tumor Necrosis Factor Receptor Superfamily Member 11b Gene (TNFRSF11B)
TNFRSF11B gene was mapped to chromosome 8q24 [201]. TNFRSF11B belongs to the tumour necrosis factor (TNF) receptor super-family and acts as a decoy receptor of the receptor activator of the NF-κB ligand (RANKL) that is a strong inducer of osteoclast differentiation acting through its receptor activator of NF-κB (RANK) receptor [202].
Recent studies on TNFRSF11B tissue expression, serum levels, or gene polymorphisms also suggest an important role of the RANKL/RANK/TNFRSF11B cytokine system in atherosclerosis and vascular calcification. While TNFRSF11B is detected in both normal and atherosclerotic tissue, RANKL/RANK is expressed only in calcified arteries [203]. Moreover, TNFRSF11B is more abundant in symptomatic than in asymptomatic carotid plaques, suggesting a role in the plaque instability [204].
Recent study of four promoter polymorphisms (g.163A>G, g.209G>A, g.245T>G and g.950T>C) in the promoter region of the TNFRSF11B gene in a Korean cohort failed to identify any association with coronary artery disease (CAD) or aortic calcification [205]. On the other hand, previous haplotype analysis of the g.950T>C and g.G1181G>C (exon 1) showed significant association with CAD in Caucasian men [206] suggesting ethnic differences. An increased risk of CAD was reported in carriers of at least one C allele of both polymorphisms. The C allele at position 950 also correlated with serum TNFRSF11B levels.
Matrix Metalloproteinases (MMPs)
MMPs, a family of diverse enzymes consisting of 24 zinc-dependent endopeptidases, process various components of the extra-cellular matrix and cell surface proteins (reviewed in [207]). Altered MMP activities have been implicated in a variety of pathological processes, including atherosclerosis [208]. Several members of the MMP family have functional polymorphisms that have been assessed for association to atherosclerosis, e.g. MMP1, MMP3, and MMP9. For these genes, promoter polymorphisms have been linked to increased risk of carotid artery stenosis [209, 210].
Other Candidate Genes
A genome-wide scan by Lange et al. [211] revealed two distinct linkage peaks at chromosomal regions 6p21.3 (LOD score 2.22) and 10q21.3 (LOD score 3.24), which may harbour genes associated with coronary atherosclerosis. Suggested candidate genes within these regions include collagen type XI α2 (COL11A2) and allograft inflammatory factor 1 (AIF1) on chromosome 6, plus collagen type XIII α1 (COL13A1) and bone morphogenetic protein receptor type 1A (BMPR1A) on chromosome 10. BMPR1A was found overexpressed in asymmetric dimethylarginine (ADMA) conditioned coronary artery endothelial cells under pathophysiological concentrations [212]. ADMA is a naturally occurring component of plasma that inhibits nitric oxide synthesis and was linked to major adverse cardiovascular events or death [213].
Association of coronary artery disease with polymorphism on chromosome 6 has been confirmed by another study reporting a linkage peak between 6p12–p22 [214]. The investigators suggested vascular endothelial growth factor (VEGF) localized at 6p12 (LOD score 2.21) as a promising candidate gene. A number of other studies have suggested genomic sites linked with coronary atherosclerosis and/or myocardial infarction [215-223]. Helgadottir et al. [220] in their linkage study of 713 cardiac patients reported linkage peak at 12q22 coding for leukotriene A4 hydrolase (LTA4H) as a candidate gene. The authors proposed the role of leukotrienes in mediating individual susceptibility to myocardial infarction. Table 2 provides examples of putative genes residing within these loci and their amino acid substitution causing by non-synonymous SNPs. We scored these polymorphisms to predict their functional significance (subPSEC value) by using the PANTHER’s coding SNP analysis tool [17]. The substitutions T600S (LTA4H) and R443C (BMPR1A) showed the highest subPSEC values of -2.62 and -8.29 with probability of deleterious effect (Pdeleterious) of 0.41 and 0.99, respectively; suggesting these variants for further studies in relation to cardiovascular diseases.
Table 2.
Candidate Genes in Relation to Coronary Atherosclerosis and Myocardial Infarction
| Gene | OMIM gene ID | Chromosome | Substitution (SNP rs#) | subPSEC | Pdeleterious | Reference |
|---|---|---|---|---|---|---|
| ALOX5AP | 603700 | 13q12 | Y133H (rs41323349) | -0.31 | 0.06 | [220] |
| LTA4H | 151570 | 12q22 | T600S (rs1803916) | -2.62 | 0.41 | [220] |
| BMPR1A | 601299 | 10q22.3 | R443C (rs35619497) | -8.29 | 0.99 | [211] |
| LGALS2 | 150571 | 22q13.1 | A25P (rs9607476) | -1.86 | 0.24 | [230] |
| V119I (rs2235339) | -0.99 | 0.12 |
ALOX5AP arachidonate 5-lipoxygenase-activating protein, LTA4H leukotriene A4 hydrolase, BMPR1A bone morphogenetic protein receptor type, LGALS2 lectin galactoside-binding soluble 2, OMIM online mendelian inheritance in man, q long arm of a chromosome, SNP single nucleotide polymorphism, * http://www.ncbi.nlm.nih.gov/ (Genome build 36.1).
CONCLUSION
Atherosclerosis is a complex disorder depending on an interaction between genotype and environment. The relative contribution of genes and environment varies from one patient to another. There is no unifying genetic pattern that is associated with atherosclerosis. Mendelian disorders, such as FH or sitosterolaemia explain only a small part of disease risk indicating the involvement of complex non-Mendelian traits and their combined effects. While some individuals suffer from hereditary impaired lipoprotein homeostasis, for others, chronic inflammation or vascular calcification may be the prevalent cause of their increased susceptibility. Large studies examining different populations are on going and will shed further light on the importance of different genes for different presentations of atherosclerosis.
ACKNOWLEDGEMENTS
Funding from the National Institute of Health, USA (RO1 HL080010-01) and NHMRC (project grant 379600) supported this work.
REFERENCES
- 1.Stary HC. Composition and classification of human atherosclerotic lesions. Virchows Arch A Pathol. Anat. Histopathol. 1992;421:277–290. doi: 10.1007/BF01660974. [DOI] [PubMed] [Google Scholar]
- 2.Ross R. Atherosclerosis--an inflammatory disease. N. Engl. J. Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 3.Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–874. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]
- 4.Marenberg ME, Risch N, Berkman LF, Floderus B, de Faire U. Genetic susceptibility to death from coronary heart disease in a study of twins. N. Engl. J. Med. 1994;330:1041–1046. doi: 10.1056/NEJM199404143301503. [DOI] [PubMed] [Google Scholar]
- 5.Zdravkovic S, Wienke A, Pedersen NL, Marenberg ME, Yashin AI, De Faire U. Heritability of death from coronary heart disease: a 36-year follow-up of 20 966 Swedish twins. J. Intern. Med. 2002;252:247–254. doi: 10.1046/j.1365-2796.2002.01029.x. [DOI] [PubMed] [Google Scholar]
- 6.Yarnell J, Yu S, Patterson C, Cambien F, Arveiler D, Amouyel P, Ferrieres J, Luc G, Evans A, Ducimetiere P. Family history, longevity, and risk of coronary heart disease: the PRIME Study. Int. J. Epidemiol. 2003;32:71–77. doi: 10.1093/ije/dyg038. [DOI] [PubMed] [Google Scholar]
- 7.Hattersley AT, McCarthy MI. What makes a good genetic association study? Lancet. 2005;366:1315–1323. doi: 10.1016/S0140-6736(05)67531-9. [DOI] [PubMed] [Google Scholar]
- 8.Dichgans M, Markus HS. Genetic association studies in stroke: methodological issues and proposed standard criteria. Stroke. 2005;36:2027–2031. doi: 10.1161/01.STR.0000177498.21594.9e. [DOI] [PubMed] [Google Scholar]
- 9.Daly MJ, Rioux JD, Schaffner SF, Hudson TJ, Lander ES. High-resolution haplotype structure in the human genome. Nat. Genet. 2001;29:229–232. doi: 10.1038/ng1001-229. [DOI] [PubMed] [Google Scholar]
- 10.Patil N, Berno AJ, Hinds DA, Barrett WA, Doshi JM, Hacker CR, Kautzer CR, Lee DH, Marjoribanks C, McDonough DP, Nguyen BT, Norris MC, Sheehan JB, Shen N, Stern D, Stokowski RP, Thomas DJ, Trulson MO, Vyas KR, Frazer KA, Fodor SP, Cox DR. Blocks of limited haplotype diversity revealed by high-resolution scanning of human chromosome 21. Science. 2001;294:1719–1723. doi: 10.1126/science.1065573. [DOI] [PubMed] [Google Scholar]
- 11.Dawson E, Abecasis GR, Bumpstead S, Chen Y, Hunt S, Beare DM, Pabial J, Dibling T, Tinsley E, Kirby S, Carter D, Papaspyridonos M, Livingstone S, Ganske R, Lohmussaar E, Zernant J, Tonisson N, Remm M, Magi R, Puurand T, Vilo J, Kurg A, Rice K, Deloukas P, Mott R, Metspalu A, Bentley DR, Cardon LR, Dunham I. A first-generation linkage disequilibrium map of human chromosome 22. Nature. 2002;418:544–548. doi: 10.1038/nature00864. [DOI] [PubMed] [Google Scholar]
- 12.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D. The structure of haplotype blocks in the human genome. Science. 2002;296:2225–2229. doi: 10.1126/science.1069424. [DOI] [PubMed] [Google Scholar]
- 13.Phillips MS, Lawrence R, Sachidanandam R, Morris AP, Balding DJ, Donaldson MA, Studebaker JF, Ankener WM, Alfisi SV, Kuo FS, Camisa AL, Pazorov V, Scott KE, Carey BJ, Faith J, Katari G, Bhatti HA, Cyr JM, Derohannessian V, Elosua C, Forman AM, Grecco NM, Hock CR, Kuebler JM, Lathrop JA, Mockler MA, Nachtman EP, Restine SL, Varde SA, Hozza MJ, Gelfand CA, Broxholme J, Abecasis GR, Boyce-Jacino MT, Cardon LR. Chromosome-wide distribution of haplotype blocks and the role of recombination hot spots. Nat. Genet. 2003;33:382–387. doi: 10.1038/ng1100. [DOI] [PubMed] [Google Scholar]
- 14.The International HapMapConsortium. A second generation human haplotype map of over 3.1 million SNPs. Nature. 2007:851–861. doi: 10.1038/nature06258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas PD, Campbell MJ, Kejariwal A, Mi H, Karlak B, Daverman R, Diemer K, Muruganujan A, Narechania A. PANTHER: a library of protein families and subfamilies indexed by function. Genome Res. 2003;13:2129–2141. doi: 10.1101/gr.772403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas PD, Kejariwal A. Coding single-nucleotide polymorphisms associated with complex vs. Mendelian disease: evolutionary evidence for differences in molecular effects. Proc. Natl. Acad. Sci. U. S. A. 2004;101:15398–15403. doi: 10.1073/pnas.0404380101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas PD, Kejariwal A, Guo N, Mi H, Campbell MJ, Muruganujan A, Lazareva-Ulitsky B. Applications for protein sequence-function evolution data: mRNA/protein expression analysis and coding SNP scoring tools. Nucleic Acids Res. 2006;34:W645–650. doi: 10.1093/nar/gkl229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cardon LR, Palmer LJ. Population stratification and spurious allelic association. Lancet. 2003;361:598–604. doi: 10.1016/S0140-6736(03)12520-2. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein JL, Brown MS. Familial hypercholesterolemia: The Metabolic Basis of Inherited Disease. 6th. New York: McGraw Hill; 1989. [Google Scholar]
- 20.Breslow JL, Deeb S, Lalouel JM, Le Boeuf R, Schaefer EJ, Tyroler HA, Wilson P, Young S. Genetic susceptibility to atherosclerosis. Circulation. 1989;80:724–728. doi: 10.1161/01.cir.80.3.724. [DOI] [PubMed] [Google Scholar]
- 21.Lusis AJ, Fogelman AM, Fonarow GC. Genetic basis of atherosclerosis: part I: new genes and pathways. Circulation. 2004;110:1868–1873. doi: 10.1161/01.CIR.0000143041.58692.CC. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein JL, Brown MS. Expression of the familial hypercholesterolemia gene in heterozygotes: model for a dominant disorder in man. Trans. Assoc. Am. Physicians. 1974;87:120–131. [PubMed] [Google Scholar]
- 23.Lindgren V, Luskey KL, Russell DW, Francke U. Human genes involved in cholesterol metabolism: chromosomal mapping of the loci for the low density lipoprotein receptor and 3-hydroxy-3-methylglutaryl-coenzyme A reductase with cDNA probes. Proc. Natl. Acad. Sci. U. S. A. 1985;82:8567–8571. doi: 10.1073/pnas.82.24.8567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Francke U, Brown MS, Goldstein JL. Assignment of the human gene for the low density lipoprotein receptor to chromosome 19: synteny of a receptor, a ligand, and a genetic disease. Proc. Natl. Acad. Sci. U. S. A. 1984;81:2826–2830. doi: 10.1073/pnas.81.9.2826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamamoto T, Davis CG, Brown MS, Schneider WJ, Casey ML, Goldstein JL, Russell DW. The human LDL receptor: a cysteine-rich protein with multiple Alu sequences in its mRNA. Cell. 1984;39:27–38. doi: 10.1016/0092-8674(84)90188-0. [DOI] [PubMed] [Google Scholar]
- 26.Hobbs HH, Brown MS, Goldstein JL. Molecular genetics of the LDL receptor gene in familial hypercholesterolemia. Hum. Mutat. 1992;1:445–466. doi: 10.1002/humu.1380010602. [DOI] [PubMed] [Google Scholar]
- 27.Varret M, Rabes JP, Collod-Beroud G, Junien C, Boileau C, Beroud C. Software and database for the analysis of mutations in the human LDL receptor gene. Nucleic Acids Res. 1997;25:172–180. doi: 10.1093/nar/25.1.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soutar AK. Update on low density lipoprotein receptor mutations. Curr. Opin. Lipidol. 1998;9:141–147. doi: 10.1097/00041433-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Heath KE, Day IN, Humphries SE. Universal primer quantitative fluorescent multiplex (UPQFM) PCR: a method to detect major and minor rearrangements of the low density lipoprotein receptor gene. J. Med. Genet. 2000;37:272–280. doi: 10.1136/jmg.37.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Villeger L, Abifadel M, Allard D, Rabes JP, Thiart R, Kotze MJ, Beroud C, Junien C, Boileau C, Varret M. The UMD-LDLR database: additions to the software and 490 new entries to the database. Hum. Mutat. 2002;20:81–87. doi: 10.1002/humu.10102. [DOI] [PubMed] [Google Scholar]
- 31.Humphries S, King-Underwood L, Gudnason V, Seed M, Delattre S, Clavey V, Fruchart JC. Six DNA polymorphisms in the low density lipoprotein receptor gene: their genetic relationship and an example of their use for identifying affected relatives of patients with familial hypercholesterolaemia. J. Med. Genet. 1993;30:273–279. doi: 10.1136/jmg.30.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chaves FJ, Puig O, Garcia-Sogo M, Real J, Gil JV, Ascaso J, Carmena R, Armengod ME. Seven DNA polymorphisms in the LDL receptor gene: application to the study of familial hypercholesterolemia in Spain. Clin. Genet. 1996;50:28–35. doi: 10.1111/j.1399-0004.1996.tb02342.x. [DOI] [PubMed] [Google Scholar]
- 33.Puig O, Chaves FJ, Garcia-Sogo M, Real J, Gil JV, Armengod ME. A three-allelic polymorphic system in exon 12 of the LDL receptor gene is highly informative for segregation analysis of familial hypercholesterolemia in the Spanish population. Clin. Genet. 1996;50:50–53. doi: 10.1111/j.1399-0004.1996.tb02346.x. [DOI] [PubMed] [Google Scholar]
- 34.Salazar LA, Cavalli SA, Hirata MH, Diament J, Forti N, Giannini SD, Nakandakare ER, Bertolami MC, Hirata RD. Polymorphisms of the low-density lipoprotein receptor gene in Brazilian individuals with heterozygous familial hypercholesterolemia. Braz. J. Med. Biol. Res. 2000;33:1301–1304. doi: 10.1590/s0100-879x2000001100006. [DOI] [PubMed] [Google Scholar]
- 35.Mavroidis N, Traeger-Synodinos J, Kanavakis E, Drogari E, Matsaniotis N, Humphries SE, Day IN, Kattamis C. A high incidence of mutations in exon 6 of the low-density lipoprotein receptor gene in Greek familial hypercholesterolemia patients, including a novel mutation. Hum. Mutat. 1997;9:274–276. doi: 10.1002/(SICI)1098-1004(1997)9:3<274::AID-HUMU10>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 36.Traeger-Synodinos J, Mavroidis N, Kanavakis E, Drogari E, Humphries SE, Day IN, Kattamis C, Matsaniotis N. Analysis of low density lipoprotein receptor gene mutations and microsatellite haplotypes in Greek FH heterozygous children: six independent ancestors account for 60% of probands. Hum. Genet. 1998;102:343–347. doi: 10.1007/s004390050703. [DOI] [PubMed] [Google Scholar]
- 37.Kane JP, Hardman DA, Paulus HE. Heterogeneity of apolipoprotein B: isolation of a new species from human chylomicrons. Proc. Natl. Acad. Sci. U. S. A. 1980;77:2465–2469. doi: 10.1073/pnas.77.5.2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deeb SS, Disteche C, Motulsky AG, Lebo RV, Kan YW. Chromosomal localization of the human apolipoprotein B gene and detection of homologous RNA in monkey intestine. Proc. Natl. Acad. Sci. U. S. A. 1986;83:419–422. doi: 10.1073/pnas.83.2.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang CY, Gu ZW, Weng SA, Kim TW, Chen SH, Pownall HJ, Sharp PM, Liu SW, Li WH, Gotto AM. Structure of apolipoprotein B-100 of human low density lipoproteins. Arteriosclerosis. 1989;9:96–108. doi: 10.1161/01.atv.9.1.96. [DOI] [PubMed] [Google Scholar]
- 40.Young SG. Recent progress in understanding apolipoprotein B. Circulation. 1990;82:1574–1594. doi: 10.1161/01.cir.82.5.1574. [DOI] [PubMed] [Google Scholar]
- 41.Innerarity TL, Weisgraber KH, Arnold KS, Mahley RW, Krauss RM, Vega GL, Grundy SM. Familial defective apolipoprotein B-100: low density lipoproteins with abnormal receptor binding. Proc. Natl. Acad. Sci. U. S. A. 1987;84:6919–6923. doi: 10.1073/pnas.84.19.6919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schonfeld G. Familial hypobetalipoproteinemia: a review. J. Lipid Res. 2003;44:878–883. doi: 10.1194/jlr.R300002-JLR200. [DOI] [PubMed] [Google Scholar]
- 43.Defesche JC, Pricker KL, Hayden MR, van der Ende BE, Kastelein JJ. Familial defective apolipoprotein B-100 is clinically indistinguishable from familial hypercholesterolemia. Arch Intern. Med. 1993;153:2349–2356. [PubMed] [Google Scholar]
- 44.Soria LF, Ludwig EH, Clarke HR, Vega GL, Grundy SM, McCarthy BJ. Association between a specific apolipoprotein B mutation and familial defective apolipoprotein B-100. Proc. Natl. Acad. Sci. U. S. A. 1989;86:587–591. doi: 10.1073/pnas.86.2.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Innerarity TL, Mahley RW, Weisgraber KH, Bersot TP, Krauss RM, Vega GL, Grundy SM, Friedl W, Davignon J, McCarthy BJ. Familial defective apolipoprotein B-100: a mutation of apolipoprotein B that causes hypercholesterolemia. J. Lipid. Res. 1990;31:1337–1349. [PubMed] [Google Scholar]
- 46.Horvath A, Ganev V. The mutation APOB-100 R3500Q in Eastern Europe. Atherosclerosis. 2001;156:241–242. doi: 10.1016/s0021-9150(01)00482-8. [DOI] [PubMed] [Google Scholar]
- 47.Schuster H, Rauh G, Kormann B, Hepp T, Humphries S, Keller C, Wolfram G, Zollner N. Familial defective apolipoprotein B-100. Comparison with familial hypercholesterolemia in 18 cases detected in Munich. Arteriosclerosis. 1990;10:577–581. doi: 10.1161/01.atv.10.4.577. [DOI] [PubMed] [Google Scholar]
- 48.Gasparovic J, Basistova Z, Fabryova L, Wsolova L, Vohnout B, Raslova K. Familial defective apolipoprotein B-100 in Slovakia: are differences in prevalence of familial defective apolipoprotein B-100 explained by ethnicity? Atherosclerosis. 2007;194:e95–107. doi: 10.1016/j.atherosclerosis.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 49.Pullinger CR, Gaffney D, Gutierrez MM, Malloy MJ, Schumaker VN, Packard CJ, Kane JP. The apolipoprotein B R3531C mutation. Characteristics of 24 subjects from 9 kindreds. J. Lipid Res. 1999;40:318–327. [PubMed] [Google Scholar]
- 50.Boren J, Ekstrom U, Agren B, Nilsson-Ehle P, Innerarity TL. The molecular mechanism for the genetic disorder familial defective apolipoprotein B100. J. Biol. Chem. 2001;276:9214–9218. doi: 10.1074/jbc.M008890200. [DOI] [PubMed] [Google Scholar]
- 51.Boerwinkle E, Chan L. A three codon insertion/deletion polymorphism in the signal peptide region of the human apolipoprotein B (APOB) gene directly typed by the polymerase chain reaction. Nucleic Acids Res. 1989;17:4003. doi: 10.1093/nar/17.10.4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boerwinkle E, Lee SS, Butler R, Schumaker VN, Chan L. Rapid typing of apolipoprotein B DNA polymorphisms by DNA amplification. Association between Ag epitopes of human apolipoprotein B-100, a signal peptide insertion/deletion polymorphism, and a 3'flanking DNA variable number of tandem repeats polymorphism of the apolipoprotein B gene. Atherosclerosis. 1990;81:225–232. doi: 10.1016/0021-9150(90)90070-y. [DOI] [PubMed] [Google Scholar]
- 53.Visvikis S, Chan L, Siest G, Drouin P, Boerwinkle E. An insertion deletion polymorphism in the signal peptide of the human apolipoprotein B gene. Hum. Genet. 1990;84:373–375. doi: 10.1007/BF00196239. [DOI] [PubMed] [Google Scholar]
- 54.Turner PR, Talmud PJ, Visvikis S, Ehnholm C, Tiret L. DNA polymorphisms of the apoprotein B gene are associated with altered plasma lipoprotein concentrations but not with perceived risk of cardiovascular disease: European Atherosclerosis Research Study. Atherosclerosis. 1995;116:221–234. doi: 10.1016/0021-9150(94)05550-3. [DOI] [PubMed] [Google Scholar]
- 55.Renges HH, Wile DB, McKeigue PM, Marmot MG, Humphries SE. Apolipoprotein B gene polymorphisms are associated with lipid levels in men of South Asian descent. Atherosclerosis. 1991;91:267–275. doi: 10.1016/0021-9150(91)90174-2. [DOI] [PubMed] [Google Scholar]
- 56.Hansen PS, Gerdes LU, Klausen IC, Gregersen N, Faergeman O. Polymorphisms in the apolipoprotein B-100 gene contributes to normal variation in plasma lipids in 464 Danish men born in 1948. Hum. Genet. 1993;91:45–50. doi: 10.1007/BF00230221. [DOI] [PubMed] [Google Scholar]
- 57.Kammerer CM, VandeBerg JL, Haffner SM, Hixson JE. Apolipoprotein B (apo B) signal peptide length polymorphisms are associated with apo B, low density lipoprotein cholesterol, and glucose levels in Mexican Americans. Atherosclerosis. 1996;120:37–45. doi: 10.1016/0021-9150(95)05674-2. [DOI] [PubMed] [Google Scholar]
- 58.Choong ML, Koay ES, Khaw MC, Aw TC. Apolipoprotein B 5'-Ins/Del and 3'-VNTR polymorphisms in Chinese, malay and Indian singaporeans. Hum. Hered. 1999;49:31–40. doi: 10.1159/000022837. [DOI] [PubMed] [Google Scholar]
- 59.Boekholdt SM, Peters RJ, Fountoulaki K, Kastelein JJ, Sijbrands EJ. Molecular variation at the apolipoprotein B gene locus in relation to lipids and cardiovascular disease: a systematic meta-analysis. Hum. Genet. 2003;113:417–425. doi: 10.1007/s00439-003-0988-3. [DOI] [PubMed] [Google Scholar]
- 60.Jemaa R, Mebazaa A, Fumeron F. Apolipoprotein B signal peptide polymorphism and plasma LDL-cholesterol response to low-calorie diet. Int. J. Obes. Relat. Metab. Disord. 2004;28:902–905. doi: 10.1038/sj.ijo.0802648. [DOI] [PubMed] [Google Scholar]
- 61.Cantor RM, de Bruin T, Kono N, Napier S, van Nas A, Allayee H, Lusis AJ. Quantitative trait loci for apolipoprotein B, cholesterol, and triglycerides in familial combined hyperlipidemia pedigrees. Arterioscler. Thromb. Vasc. Biol. 2004;24:1935–1941. doi: 10.1161/01.ATV.0000142358.46276.a7. [DOI] [PubMed] [Google Scholar]
- 62.Collaku A, Rankinen T, Rice T, Leon AS, Rao DC, Skinner JS, Wilmore JH, Bouchard C. A genome-wide linkage scan for dietary energy and nutrient intakes: the Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) Family Study. Am. J. Clin. Nutr. 2004;79:881–886. doi: 10.1093/ajcn/79.5.881. [DOI] [PubMed] [Google Scholar]
- 63.Hsueh WC, St Jean PL, Mitchell BD, Pollin TI, Knowler WC, Ehm MG, Bell CJ, Sakul H, Wagner MJ, Burns DK, Shuldiner AR. Genome-wide and fine-mapping linkage studies of type 2 diabetes and glucose traits in the Old Order Amish: evidence for a new diabetes locus on chromosome 14q11 and confirmation of a locus on chromosome 1q21-q24. Diabetes. 2003;52:550–557. doi: 10.2337/diabetes.52.2.550. [DOI] [PubMed] [Google Scholar]
- 64.Baima J, Nicolaou M, Schwartz F, DeStefano AL, Manolis A, Gavras I, Laffer C, Elijovich F, Farrer L, Baldwin CT, Gavras H. Evidence for linkage between essential hypertension and a putative locus on human chromosome 17. Hypertension. 1999;34:4–7. doi: 10.1161/01.hyp.34.1.4. [DOI] [PubMed] [Google Scholar]
- 65.Levy D, DeStefano AL, Larson MG, O'Donnell CJ, Lifton RP, Gavras H, Cupples LA, Myers RH. Evidence for a gene influencing blood pressure on chromosome 17. Genome scan linkage results for longitudinal blood pressure phenotypes in subjects from the framingham heart study. Hypertension. 2000;36:477–483. doi: 10.1161/01.hyp.36.4.477. [DOI] [PubMed] [Google Scholar]
- 66.Priestley L, Knott T, Wallis S, Powell L, Pease R, Simon A, Scott J. RFLP for the human apolipoprotein B gene: I, BamHI. Nucleic Acids Res. 1985;13:6789. doi: 10.1093/nar/13.18.6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wei CF, Chen SH, Yang CY, Marcel YL, Milne RW, Li WH, Sparrow JT, Gotto AM Jr, Chan L. Molecular cloning and expression of partial cDNAs and deduced amino acid sequence of a carboxyl-terminal fragment of human apolipoprotein B-100. Proc. Natl. Acad. Sci. U. S. A. 1985;82:7265–7269. doi: 10.1073/pnas.82.21.7265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pan JP, Chiang AN, Tai JJ, Wang SP, Chang MS. Restriction fragment length polymorphisms of apolipoprotein B gene in Chinese population with coronary heart disease. Clin. Chem. 1995;41:424–429. [PubMed] [Google Scholar]
- 69.Ludwig EH, Hopkins PN, Allen A, Wu LL, Williams RR, Anderson JL, Ward RH, Lalouel JM, Innerarity TL. Association of genetic variations in apolipoprotein B with hypercholesterolemia, coronary artery disease, and receptor binding of low density lipoproteins. J. Lipid Res. 1997;38:1361–1373. [PubMed] [Google Scholar]
- 70.Corbo RM, Scacchi R, Mureddu L, Mulas G, Castrechini S, Rivasi AP. Apolipoprotein B, apolipoprotein E, and angiotensin-converting enzyme polymorphisms in 2 Italian populations at different risk for coronary artery disease and comparison of allele frequencies among European populations. Hum. Biol. 1999;71:933–945. [PubMed] [Google Scholar]
- 71.Guzman EC, Hirata MH, Quintao EC, Hirata RD. Association of the apolipoprotein B gene polymorphisms with cholesterol levels and response to fluvastatin in Brazilian individuals with high risk for coronary heart disease. Clin. Chem. Lab. Med. 2000;38:731–736. doi: 10.1515/CCLM.2000.103. [DOI] [PubMed] [Google Scholar]
- 72.Yan SK, Song YH, Zhu WL, Yan XW, Xue H, Du H, Chen BS. Apolipoprotein B gene 3'VNTR polymorphism: association with plasma lipids and coronary heart disease in Han Chinese. Clin. Chem. Lab. Med. 2006;44:1199–1205. doi: 10.1515/CCLM.2006.221. [DOI] [PubMed] [Google Scholar]
- 73.Mahley RW. Apolipoprotein E: cholesterol transport protein with expanding role in cell biology. Science. 1988;240:622–630. doi: 10.1126/science.3283935. [DOI] [PubMed] [Google Scholar]
- 74.Beisiegel U, Weber W, Ihrke G, Herz J, Stanley KK. The LDL-receptor-related protein, LRP, is an apolipoprotein E-binding protein. Nature. 1989;341:162–164. doi: 10.1038/341162a0. [DOI] [PubMed] [Google Scholar]
- 75.Huang Y, von Eckardstein A, Wu S, Maeda N, Assmann G. A plasma lipoprotein containing only apolipoprotein E and with gamma mobility on electrophoresis releases cholesterol from cells. Proc. Natl. Acad. Sci. U. S. A. 1994;91:1834–1838. doi: 10.1073/pnas.91.5.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kypreos KE, Zannis VI. Pathway of biogenesis of apolipoprotein E-containing HDL in vivo with the participation of ABCA1 and LCAT. Biochem. J. 2007;403:359–367. doi: 10.1042/BJ20061048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ji ZS, Brecht WJ, Miranda RD, Hussain MM, Innerarity TL, Mahley RW. Role of heparan sulfate proteoglycans in the binding and uptake of apolipoprotein E-enriched remnant lipoproteins by cultured cells. J. Biol. Chem. 1993;268:10160–10167. [PubMed] [Google Scholar]
- 78.Ji ZS, Fazio S, Lee YL, Mahley RW. Secretion-capture role for apolipoprotein E in remnant lipoprotein metabolism involving cell surface heparan sulfate proteoglycans. J. Biol. Chem. 1994;269:2764–2772. [PubMed] [Google Scholar]
- 79.Havel RJ. Receptor and non-receptor mediated uptake of chylomicron remnants by the liver. Atherosclerosis. 1998;141(Suppl 1):S1–7. doi: 10.1016/s0021-9150(98)00211-1. [DOI] [PubMed] [Google Scholar]
- 80.Olaisen B, Teisberg P, Gedde-Dahl T Jr. The locus for apolipoprotein E (apoE) is linked to the complement component C3 (C3) locus on chromosome 19 in man. Hum. Genet. 1982;62:233–236. doi: 10.1007/BF00333526. [DOI] [PubMed] [Google Scholar]
- 81.Das HK, McPherson J, Bruns GA, Karathanasis SK, Breslow JL. Isolation, characterization, and mapping to chromosome 19 of the human apolipoprotein E gene. J. Biol. Chem. 1985;260:6240–6247. [PubMed] [Google Scholar]
- 82.Lauer SJ, Walker D, Elshourbagy NA, Reardon CA, Levy-Wilson B, Taylor JM. Two copies of the human apolipoprotein C-I gene are linked closely to the apolipoprotein E gene. J. Biol. Chem. 1988;263:7277–7286. [PubMed] [Google Scholar]
- 83.Paik YK, Chang DJ, Reardon CA, Davies GE, Mahley RW, Taylor JM. Nucleotide sequence and structure of the human apolipoprotein E gene. Proc. Natl. Acad. Sci. U. S. A. 1985;82:3445–3449. doi: 10.1073/pnas.82.10.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Utermann G, Langenbeck U, Beisiegel U, Weber W. Genetics of the apolipoprotein E system in man. Am. J. Hum. Genet. 1980;32:339–347. [PMC free article] [PubMed] [Google Scholar]
- 85.Zannis VI, Breslow JL. Human very low density lipoprotein apolipoprotein E isoprotein polymorphism is explained by genetic variation and posttranslational modification. Biochemistry. 1981;20:1033–1041. doi: 10.1021/bi00507a059. [DOI] [PubMed] [Google Scholar]
- 86.Utermann G, Steinmetz A, Weber W. Genetic control of human apolipoprotein E polymorphism: comparison of one- and two-dimensional techniques of isoprotein analysis. Hum. Genet. 1982;60:344–351. doi: 10.1007/BF00569216. [DOI] [PubMed] [Google Scholar]
- 87.Rall SC Jr, Weisgraber KH, Mahley RW. Human apolipoprotein E. The complete amino acid sequence. J. Biol. Chem. 1982;257:4171–4178. [PubMed] [Google Scholar]
- 88.Weisgraber KH, Innerarity TL, Mahley RW. Abnormal lipoprotein receptor-binding activity of the human E apoprotein due to cysteine-arginine interchange at a single site. J. Biol. Chem. 1982;257:2518–2521. [PubMed] [Google Scholar]
- 89.Martins RN, Clarnette R, Fisher C, Broe GA, Brooks WS, Montgomery P, Gandy SE. ApoE genotypes in Australia: roles in early and late onset Alzheimer's disease and Down's syndrome. Neuroreport. 1995;6:1513–1516. [PubMed] [Google Scholar]
- 90.Gregg RE, Brewer HB Jr. The role of apolipoprotein E and lipoprotein receptors in modulating the in vivo metabolism of apolipoprotein B-containing lipoproteins in humans. Clin. Chem. 1988;34:B28–32. [PubMed] [Google Scholar]
- 91.Banares VG, Peterson G, Aguilar D, Gulayin R, Sisu E, Wyszynski DF, Pivetta OH, Tavella MJ. Association between the APOE*4 allele and atherosclerosis is age dependent among Argentine males. Hum. Biol. 2005;77:247–256. doi: 10.1353/hub.2005.0036. [DOI] [PubMed] [Google Scholar]
- 92.Taylor JM, Lauer S, Elshourbagy N, Reardon C, Taxman E, Walker D, Chang D, Paik YK. Structure and evolution of human apolipoprotein genes: identification of regulatory elements of the human apolipoprotein E gene. Ciba Found Symp. 1987;130:70–86. doi: 10.1002/9780470513507.ch6. [DOI] [PubMed] [Google Scholar]
- 93.Artiga MJ, Bullido MJ, Sastre I, Recuero M, Garcia MA, Aldudo J, Vazquez J, Valdivieso F. Allelic polymorphisms in the transcriptional regulatory region of apolipoprotein E gene. FEBS Lett. 1998;421:105–108. doi: 10.1016/s0014-5793(97)01543-3. [DOI] [PubMed] [Google Scholar]
- 94.Nickerson DA, Taylor SL, Fullerton SM, Weiss KM, Clark AG, Stengard JH, Salomaa V, Boerwinkle E, Sing CF. Sequence diversity and large-scale typing of SNPs in the human apolipoprotein E gene. Genome Res. 2000;10:1532–1545. doi: 10.1101/gr.146900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roks G, Cruts M, Houwing-Duistermaat JJ, Dermaut B, Serneels S, Havekes LM, Hofman A, Breteler MM, Van Broeckhoven C, van Duijn CM. Effect of the APOE-491A/T promoter polymorphism on apolipoprotein E levels and risk of Alzheimer disease: The Rotterdam Study. Am. J. Med. Genet. 2002;114:570–573. doi: 10.1002/ajmg.10407. [DOI] [PubMed] [Google Scholar]
- 96.Viiri LE, Raitakari OT, Huhtala H, Kahonen M, Rontu R, Juonala M, Hutri-Kahonen N, Marniemi J, Viikari JS, Karhunen PJ, Lehtimaki T. Relations of APOE promoter polymorphisms to LDL cholesterol and markers of subclinical atherosclerosis in young adults. J. Lipid Res. 2006;47:1298–1306. doi: 10.1194/jlr.M600033-JLR200. [DOI] [PubMed] [Google Scholar]
- 97.Lawn RM, Wade DP, Garvin MR, Wang X, Schwartz K, Porter JG, Seilhamer JJ, Vaughan AM, Oram JF. The Tangier disease gene product ABC1 controls the cellular apolipoprotein-mediated lipid removal pathway. J. Clin. Invest. 1999;104:R25–31. doi: 10.1172/JCI8119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Oram JF. HDL apolipoproteins and ABCA1: partners in the removal of excess cellular cholesterol. Arterioscler. Thromb. Vasc. Biol. 2003;23:720–727. doi: 10.1161/01.ATV.0000054662.44688.9A. [DOI] [PubMed] [Google Scholar]
- 99.Wang N, Tall AR. Regulation and mechanisms of ATP-binding cassette transporter A1-mediated cellular cholesterol efflux. Arterioscler. Thromb. Vasc. Biol. 2003;23:1178–1184. doi: 10.1161/01.ATV.0000075912.83860.26. [DOI] [PubMed] [Google Scholar]
- 100.Bodzioch M, Orso E, Klucken J, Langmann T, Bottcher A, Diederich W, Drobnik W, Barlage S, Buchler C, Porsch-Ozcurumez M, Kaminski WE, Hahmann HW, Oette K, Rothe G, Aslanidis C, Lackner KJ, Schmitz G. The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. Nat. Genet. 1999;22:347–351. doi: 10.1038/11914. [DOI] [PubMed] [Google Scholar]
- 101.Brooks-Wilson A, Marcil M, Clee SM, Zhang LH, Roomp K, van Dam M, Yu L, Brewer C, Collins JA, Molhuizen HO, Loubser O, Ouelette BF, Fichter K, Ashbourne-Excoffon KJ, Sensen CW, Scherer S, Mott S, Denis M, Martindale D, Frohlich J, Morgan K, Koop B, Pimstone S, Kastelein JJ, Genest J Jr, Hayden MR. Mutations in ABC1 in Tangier disease and familial high-density lipoprotein deficiency. Nat. Genet. 1999;22:336–345. doi: 10.1038/11905. [DOI] [PubMed] [Google Scholar]
- 102.Rust S, Rosier M, Funke H, Real J, Amoura Z, Piette JC, Deleuze JF, Brewer HB, Duverger N, Denefle P, Assmann G. Tangier disease is caused by mutations in the gene encoding ATP-binding cassette transporter 1. Nat. Genet. 1999;22:352–355. doi: 10.1038/11921. [DOI] [PubMed] [Google Scholar]
- 103.Remaley AT, Rust S, Rosier M, Knapper C, Naudin L, Broccardo C, Peterson KM, Koch C, Arnould I, Prades C, Duverger N, Funke H, Assman G, Dinger M, Dean M, Chimini G, Santamarina-Fojo S, Fredrickson DS, Denefle P, Brewer HB Jr. Human ATP-binding cassette transporter 1 (ABC1): genomic organization and identification of the genetic defect in the original Tangier disease kindred. Proc. Natl. Acad. Sci. U. S. A. 1999;96:12685–12690. doi: 10.1073/pnas.96.22.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Luciani MF, Denizot F, Savary S, Mattei MG, Chimini G. Cloning of two novel ABC transporters mapping on human chromosome 9. Genomics. 1994;21:150–159. doi: 10.1006/geno.1994.1237. [DOI] [PubMed] [Google Scholar]
- 105.Wang J, Burnett JR, Near S, Young K, Zinman B, Hanley AJ, Connelly PW, Harris SB, Hegele RA. Common and rare ABCA1 variants affecting plasma HDL cholesterol. Arterioscler. Thromb. Vasc. Biol. 2000;20:1983–1989. doi: 10.1161/01.atv.20.8.1983. [DOI] [PubMed] [Google Scholar]
- 106.Clee SM, Zwinderman AH, Engert JC, Zwarts KY, Molhuizen HO, Roomp K, Jukema JW, van Wijland M, van Dam M, Hudson TJ, Brooks-Wilson A, Genest J Jr, Kastelein JJ, Hayden MR. Common genetic variation in ABCA1 is associated with altered lipoprotein levels and a modified risk for coronary artery disease. Circulation. 2001;103:1198–1205. doi: 10.1161/01.cir.103.9.1198. [DOI] [PubMed] [Google Scholar]
- 107.Lutucuta S, Ballantyne CM, Elghannam H, Gotto AM Jr, Marian AJ. Novel polymorphisms in promoter region of atp binding cassette transporter gene and plasma lipids, severity, progression, and regression of coronary atherosclerosis and response to therapy. Circ. Res. 2001;88:969–973. doi: 10.1161/hh0901.090301. [DOI] [PubMed] [Google Scholar]
- 108.Zwarts KY, Clee SM, Zwinderman AH, Engert JC, Singaraja R, Loubser O, James E, Roomp K, Hudson TJ, Jukema JW, Kastelein JJ, Hayden MR. ABCA1 regulatory variants influence coronary artery disease independent of effects on plasma lipid levels. Clin. Genet. 2002;61:115–125. doi: 10.1034/j.1399-0004.2002.610206.x. [DOI] [PubMed] [Google Scholar]
- 109.Hodoglugil U, Williamson DW, Huang Y, Mahley RW. Common polymorphisms of ATP binding cassette transporter A1, including a functional promoter polymorphism, associated with plasma high density lipoprotein cholesterol levels in Turks. Atherosclerosis. 2005;183:199–212. doi: 10.1016/j.atherosclerosis.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 110.Saleheen D, Khanum S, Haider SR, Nazir A, Ahmad U, Khalid H, Hussain I, Shuja F, Shahid K, Habib A, Frossard PM. A novel haplotype in ABCA1 gene effects plasma HDL-C concentration. Int. J. Cardiol. 2007;115:7–13. doi: 10.1016/j.ijcard.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 111.Knoblauch H, Bauerfeind A, Toliat MR, Becker C, Luganskaja T, Gunther UP, Rohde K, Schuster H, Junghans C, Luft FC, Nurnberg P, Reich JG. Haplotypes and SNPs in 13 lipid-relevant genes explain most of the genetic variance in high-density lipoprotein and low-density lipoprotein cholesterol. Hum. Mol. Genet. 2004;13:993–1004. doi: 10.1093/hmg/ddh119. [DOI] [PubMed] [Google Scholar]
- 112.Tregouet DA, Ricard S, Nicaud V, Arnould I, Soubigou S, Rosier M, Duverger N, Poirier O, Mace S, Kee F, Morrison C, Denefle P, Tiret L, Evans A, Deleuze JF, Cambien F. In-depth haplotype analysis of ABCA1 gene polymorphisms in relation to plasma ApoA1 levels and myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 2004;24:775–781. doi: 10.1161/01.ATV.0000121573.29550.1a. [DOI] [PubMed] [Google Scholar]
- 113.Cohen JC, Cali JJ, Jelinek DF, Mehrabian M, Sparkes RS, Lusis AJ, Russell DW, Hobbs HH. Cloning of the human cholesterol 7 alpha-hydroxylase gene (CYP7) and localization to chromosome 8q11-q12. Genomics. 1992;14:153–161. doi: 10.1016/s0888-7543(05)80298-8. [DOI] [PubMed] [Google Scholar]
- 114.Chiang JY. Regulation of bile acid synthesis: pathways, nuclear receptors, and mechanisms. J. Hepatol. 2004;40:539–551. doi: 10.1016/j.jhep.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 115.Wang J, Freeman DJ, Grundy SM, Levine DM, Guerra R, Cohen JC. Linkage between cholesterol 7alpha-hydroxylase and high plasma low-density lipoprotein cholesterol concentrations. J. Clin. Invest. 1998;101:1283–1291. doi: 10.1172/JCI1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Couture P, Otvos JD, Cupples LA, Wilson PW, Schaefer EJ, Ordovas JM. Association of the A-204C polymorphism in the cholesterol 7alpha-hydroxylase gene with variations in plasma low density lipoprotein cholesterol levels in the Framingham Offspring Study. J. Lipid Res. 1999;40:1883–1889. [PubMed] [Google Scholar]
- 117.Hofman MK, Weggemans RM, Zock PL, Schouten EG, Katan MB, Princen HM. CYP7A1 A-278C polymorphism affects the response of plasma lipids after dietary cholesterol or cafestol interventions in humans. J. Nutr. 2004;134:2200–2204. doi: 10.1093/jn/134.9.2200. [DOI] [PubMed] [Google Scholar]
- 118.Lin JP, Myers RH, Almasy L, Coon HH, Arnett DK, Hong Y, Hunt SC. Linkage of the cholesterol 7alpha-hydroxylase gene and low-density lipoprotein cholesterol conditional on apolipoprotein E association: the National Heart, Lung, and Blood Institute Family Heart Study. Chin. Med. J. (Engl) 2005;118:362–369. [PubMed] [Google Scholar]
- 119.Han Z, Heath SC, Shmulewitz D, Li W, Auerbach SB, Blundell ML, Lehner T, Ott J, Stoffel M, Friedman JM, Breslow JL. Candidate genes involved in cardiovascular risk factors by a family-based association study on the island of Kosrae, Federated States of Micronesia. Am. J. Med. Genet. 2002;110:234–242. doi: 10.1002/ajmg.10445. [DOI] [PubMed] [Google Scholar]
- 120.Klos KL, Sing CF, Boerwinkle E, Hamon SC, Rea TJ, Clark A, Fornage M, Hixson JE. Consistent effects of genes involved in reverse cholesterol transport on plasma lipid and apolipoprotein levels in CARDIA participants. Arterioscler. Thromb. Vasc. Biol. 2006;26:1828–1836. doi: 10.1161/01.ATV.0000231523.19199.45. [DOI] [PubMed] [Google Scholar]
- 121.Patel SB, Salen G, Hidaka H, Kwiterovich PO, Stalenhoef AF, Miettinen TA, Grundy SM, Lee MH, Rubenstein JS, Polymeropoulos MH, Brownstein MJ. Mapping a gene involved in regulating dietary cholesterol absorption. The sitosterolemia locus is found at chromosome 2p21. J. Clin. Invest. 1998;102:1041–1044. doi: 10.1172/JCI3963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lu K, Lee MH, Carpten JD, Sekhon M, Patel SB. High-resolution physical and transcript map of human chromosome 2p21 containing the sitosterolaemia locus. Eur. J. Hum. Genet. 2001;9:364–374. doi: 10.1038/sj.ejhg.5200627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yu L, Hammer RE, Li-Hawkins J, Von Bergmann K, Lutjohann D, Cohen JC, Hobbs HH. Disruption of Abcg5 and Abcg8 in mice reveals their crucial role in biliary cholesterol secretion. Proc. Natl. Acad. Sci. U. S. A. 2002;99:16237–16242. doi: 10.1073/pnas.252582399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, Kwiterovich P, Shan B, Barnes R, Hobbs HH. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290:1771–1775. doi: 10.1126/science.290.5497.1771. [DOI] [PubMed] [Google Scholar]
- 125.Hubacek JA, Berge KE, Cohen JC, Hobbs HH. Mutations in ATP-cassette binding proteins G5 (ABCG5) and G8 (ABCG8) causing sitosterolemia. Hum. Mutat. 2001;18:359–360. doi: 10.1002/humu.1206. [DOI] [PubMed] [Google Scholar]
- 126.Lee MH, Lu K, Hazard S, Yu H, Shulenin S, Hidaka H, Kojima H, Allikmets R, Sakuma N, Pegoraro R, Srivastava AK, Salen G, Dean M, Patel SB. Identification of a gene, ABCG5, important in the regulation of dietary cholesterol absorption. Nat. Genet. 2001;27:79–83. doi: 10.1038/83799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Heimerl S, Langmann T, Moehle C, Mauerer R, Dean M, Beil FU, von Bergmann K, Schmitz G. Mutations in the human ATP-binding cassette transporters ABCG5 and ABCG8 in sitosterolemia. Hum. Mutat. 2002;20:151. doi: 10.1002/humu.9047. [DOI] [PubMed] [Google Scholar]
- 128.Bhattacharyya AK, Connor WE. Beta-sitosterolemia and xanthomatosis. A newly described lipid storage disease in two sisters. J. Clin. Invest. 1974;53:1033–1043. doi: 10.1172/JCI107640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kempen HJ, de Knijff P, Boomsma DI, van der Voort HA, Gevers Leuven JA, Havekes L. Plasma levels of lathosterol and phytosterols in relation to age, sex, anthropometric parameters, plasma lipids, and apolipoprotein E phenotype, in 160 Dutch families. Metabolism. 1991;40:604–611. doi: 10.1016/0026-0495(91)90051-w. [DOI] [PubMed] [Google Scholar]
- 130.Berge KE, von Bergmann K, Lutjohann D, Guerra R, Grundy SM, Hobbs HH, Cohen JC. Heritability of plasma noncholesterol sterols and relationship to DNA sequence polymorphism in ABCG5 and ABCG8. J. Lipid Res. 2002;43:486–494. [PubMed] [Google Scholar]
- 131.Gylling H, Hallikainen M, Pihlajamaki J, Agren J, Laakso M, Rajaratnam RA, Rauramaa R, Miettinen TA. Polymorphisms in the ABCG5 and ABCG8 genes associate with cholesterol absorption and insulin sensitivity. J. Lipid Res. 2004;45:1660–1665. doi: 10.1194/jlr.M300522-JLR200. [DOI] [PubMed] [Google Scholar]
- 132.Plat J, Bragt MC, Mensink RP. Common sequence variations in ABCG8 are related to plant sterol metabolism in healthy volunteers. J. Lipid Res. 2005;46:68–75. doi: 10.1194/jlr.M400210-JLR200. [DOI] [PubMed] [Google Scholar]
- 133.Acalovschi M, Ciocan A, Mostean O, Tirziu S, Chiorean E, Keppeler H, Schirin-Sokhan R, Lammert F. Are plasma lipid levels related to ABCG5/ABCG8 polymorphisms? A preliminary study in siblings with gallstones. Eur. J. Intern. Med. 2006;17:490–494. doi: 10.1016/j.ejim.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 134.Miwa K, Inazu A, Kobayashi J, Higashikata T, Nohara A, Kawashiri M, Katsuda S, Takata M, Koizumi J, Mabuchi H. ATP-binding cassette transporter G8 M429V polymorphism as a novel genetic marker of higher cholesterol absorption in hypercholesterolaemic Japanese subjects. Clin. Sci. (Lond) 2005;109:183–188. doi: 10.1042/CS20050030. [DOI] [PubMed] [Google Scholar]
- 135.Pandit B, Ahn GS, Hazard SE, Gordon D, Patel SB. A detailed Hapmap of the Sitosterolemia locus spanning 69 kb, differences between Caucasians and African-Americans. BMC Med. Genet. 2006;7:13. doi: 10.1186/1471-2350-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kajinami K, Brousseau ME, Ordovas JM, Schaefer EJ. Interactions between common genetic polymorphisms in ABCG5/G8 and CYP7A1 on LDL cholesterol-lowering response to atorvastatin. Atherosclerosis. 2004;175:287–293. doi: 10.1016/j.atherosclerosis.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 137.Rigotti A, Acton SL, Krieger M. The class B scavenger receptors SR-BI and CD36 are receptors for anionic phospholipids. J. Biol. Chem. 1995;270:16221–16224. doi: 10.1074/jbc.270.27.16221. [DOI] [PubMed] [Google Scholar]
- 138.Murphy JE, Tedbury PR, Homer-Vanniasinkam S, Walker JH, Ponnambalam S. Biochemistry and cell biology of mammalian scavenger receptors. Atherosclerosis. 2005;182:1–15. doi: 10.1016/j.atherosclerosis.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 139.Adachi H, Tsujimoto M. Endothelial scavenger receptors. Prog. Lipid Res. 2006;45:379–404. doi: 10.1016/j.plipres.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 140.Cao G, Garcia CK, Wyne KL, Schultz RA, Parker KL, Hobbs HH. Structure and localization of the human gene encoding SR-BI/CLA-1. Evidence for transcriptional control by steroidogenic factor 1. J. Biol. Chem. 1997;272:33068–33076. doi: 10.1074/jbc.272.52.33068. [DOI] [PubMed] [Google Scholar]
- 141.Fox CS, Cupples LA, Chazaro I, Polak JF, Wolf PA, D'Agostino RB, Ordovas JM, O'Donnell CJ. Genomewide linkage analysis for internal carotid artery intimal medial thickness: evidence for linkage to chromosome 12. Am. J. Hum. Genet. 2004;74:253–261. doi: 10.1086/381559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Acton S, Osgood D, Donoghue M, Corella D, Pocovi M, Cenarro A, Mozas P, Keilty J, Squazzo S, Woolf EA, Ordovas JM. Association of polymorphisms at the SR-BI gene locus with plasma lipid levels and body mass index in a white population. Arterioscler. Thromb. Vasc. Biol. 1999;19:1734–1743. doi: 10.1161/01.atv.19.7.1734. [DOI] [PubMed] [Google Scholar]
- 143.McCarthy JJ, Lewitzky S, Permutt A. SR-B1 variants associated with HDL cholesterol levels in three populations. A. J. Hum. Genet. 2001;69:383A. doi: 10.1159/000073986. [DOI] [PubMed] [Google Scholar]
- 144.McCarthy JJ, Lehner T, Reeves C, Moliterno DJ, Newby LK, Rogers WJ, Topol EJ. Association of genetic variants in the HDL receptor, SR-B1, with abnormal lipids in women with coronary artery disease. J. Med. Genet. 2003;40:453–458. doi: 10.1136/jmg.40.6.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Imperatore G, Knowler WC, Pettitt DJ, Kobes S, Fuller JH, Bennett PH, Hanson RL. A locus influencing total serum cholesterol on chromosome 19p: results from an autosomal genomic scan of serum lipid concentrations in Pima Indians. Arterioscler. Thromb. Vasc. Biol. 2000;20:2651–2656. doi: 10.1161/01.atv.20.12.2651. [DOI] [PubMed] [Google Scholar]
- 146.Mahaney MC, Almasy L, Rainwater DL, VandeBerg JL, Cole SA, Hixson JE, Blangero J, MacCluer JW. A quantitative trait locus on chromosome 16q influences variation in plasma HDL-C levels in Mexican Americans. Arterioscler. Thromb. Vasc. Biol. 2003;23:339–345. doi: 10.1161/01.atv.0000051406.14162.6a. [DOI] [PubMed] [Google Scholar]
- 147.Bosse Y, Chagnon YC, Despres JP, Rice T, Rao DC, Bouchard C, Perusse L, Vohl MC. Genome-wide linkage scan reveals multiple susceptibility loci influencing lipid and lipoprotein levels in the Quebec Family Study. J. Lipid. Res. 2004;45:419–426. doi: 10.1194/jlr.M300401-JLR200. [DOI] [PubMed] [Google Scholar]
- 148.Feitosa MF, Province MA, Heiss G, Arnett DK, Myers RH, Pankow JS, Hopkins PN, Borecki IB. Evidence of QTL on 15q21 for high-density lipoprotein cholesterol: the National Heart, Lung, and Blood Institute Family Heart Study (NHLBI FHS) Atherosclerosis. 2007;190:232–237. doi: 10.1016/j.atherosclerosis.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 149.Chen W, Li S, Srinivasan SR, Boerwinkle E, Berenson GS. A genome scan for loci influencing levels and trends of lipoprotein lipid-related traits since childhood: The Bogalusa Heart Study. Atherosclerosis. 2007;190:248–255. doi: 10.1016/j.atherosclerosis.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 150.Duggirala R, Blangero J, Almasy L, Dyer TD, Williams KL, Leach RJ, O'Connell P, Stern MP. A major susceptibility locus influencing plasma triglyceride concentrations is located on chromosome 15q in Mexican Americans. Am. J. Hum. Genet. 2000;66:1237–1245. doi: 10.1086/302849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Li WD, Dong C, Li D, Garrigan C, Price RA. A genome scan for serum triglyceride in obese nuclear families. J. Lipid Res. 2005;46:432–438. doi: 10.1194/jlr.M400391-JLR200. [DOI] [PubMed] [Google Scholar]
- 152.Abifadel M, Varret M, Rabes JP, Allard D, Ouguerram K, Devillers M, Cruaud C, Benjannet S, Wickham L, Erlich D, Derre A, Villeger L, Farnier M, Beucler I, Bruckert E, Chambaz J, Chanu B, Lecerf JM, Luc G, Moulin P, Weissenbach J, Prat A, Krempf M, Junien C, Seidah NG, Boileau C. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat. Genet. 2003;34:154–156. doi: 10.1038/ng1161. [DOI] [PubMed] [Google Scholar]
- 153.Leren TP. Mutations in the PCSK9 gene in Norwegian subjects with autosomal dominant hypercholesterolemia. Clin. Genet. 2004;65:419–422. doi: 10.1111/j.0009-9163.2004.0238.x. [DOI] [PubMed] [Google Scholar]
- 154.Timms KM, Wagner S, Samuels ME, Forbey K, Goldfine H, Jammulapati S, Skolnick MH, Hopkins PN, Hunt SC, Shattuck DM. A mutation in PCSK9 causing autosomal-dominant hypercholesterolemia in a Utah pedigree. Hum. Genet. 2004;114:349–353. doi: 10.1007/s00439-003-1071-9. [DOI] [PubMed] [Google Scholar]
- 155.Allard D, Amsellem S, Abifadel M, Trillard M, Devillers M, Luc G, Krempf M, Reznik Y, Girardet JP, Fredenrich A, Junien C, Varret M, Boileau C, Benlian P, Rabes JP. Novel mutations of the PCSK9 gene cause variable phenotype of autosomal dominant hypercholesterolemia. Hum. Mutat. 2005;26:497. doi: 10.1002/humu.9383. [DOI] [PubMed] [Google Scholar]
- 156.Cohen J, Pertsemlidis A, Kotowski IK, Graham R, Garcia CK, Hobbs HH. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat. Genet. 2005;37:161–165. doi: 10.1038/ng1509. [DOI] [PubMed] [Google Scholar]
- 157.Garcia CK, Wilund K, Arca M, Zuliani G, Fellin R, Maioli M, Calandra S, Bertolini S, Cossu F, Grishin N, Barnes R, Cohen JC, Hobbs HH. Autosomal recessive hypercholesterolemia caused by mutations in a putative LDL receptor adaptor protein. Science. 2001;292:1394–1398. doi: 10.1126/science.1060458. [DOI] [PubMed] [Google Scholar]
- 158.Arca M, Zuliani G, Wilund K, Campagna F, Fellin R, Bertolini S, Calandra S, Ricci G, Glorioso N, Maioli M, Pintus P, Carru C, Cossu F, Cohen J, Hobbs HH. Autosomal recessive hypercholesterolaemia in Sardinia, Italy, and mutations in ARH: a clinical and molecular genetic analysis. Lancet. 2002;359:841–847. doi: 10.1016/S0140-6736(02)07955-2. [DOI] [PubMed] [Google Scholar]
- 159.Paoletti R, Gotto AM Jr, Hajjar DP. Inflammation in atherosclerosis and implications for therapy. Circulation. 2004;109:III20–26. doi: 10.1161/01.CIR.0000131514.71167.2e. [DOI] [PubMed] [Google Scholar]
- 160.Yoon S, Tromp G, Vongpunsawad S, Ronkainen A, Juvonen T, Kuivaniemi H. Genetic analysis of MMP3, MMP9, and PAI-1 in Finnish patients with abdominal aortic or intracranial aneurysms. Biochem. Biophys. Res. Commun. 1999;265:563–568. doi: 10.1006/bbrc.1999.1721. [DOI] [PubMed] [Google Scholar]
- 161.Fujii D, Brissenden JE, Derynck R, Francke U. Transforming growth factor beta gene (TGFB) maps to human chromosome 19. Cytogenet. Cell Genet. 1985;40:632. doi: 10.1007/BF01570787. [DOI] [PubMed] [Google Scholar]
- 162.Fujii D, Brissenden JE, Derynck R, Francke U. Transforming growth factor beta gene maps to human chromosome 19 long arm and to mouse chromosome 7. Somat. Cell Mol. Genet. 1986;12:281–288. doi: 10.1007/BF01570787. [DOI] [PubMed] [Google Scholar]
- 163.Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor beta in human disease. N. Engl. J. Med. 2000;342:1350–1358. doi: 10.1056/NEJM200005043421807. [DOI] [PubMed] [Google Scholar]
- 164.Grainger DJ, Heathcote K, Chiano M, Snieder H, Kemp PR, Metcalfe JC, Carter ND, Spector TD. Genetic control of the circulating concentration of transforming growth factor type beta1. Hum. Mol. Genet. 1999;8:93–97. doi: 10.1093/hmg/8.1.93. [DOI] [PubMed] [Google Scholar]
- 165.Shah R, Hurley CK, Posch PE. A molecular mechanism for the differential regulation of TGF-beta1 expression due to the common SNP -509C-T (c. -1347C > T) Hum. Genet. 2006;120:461–469. doi: 10.1007/s00439-006-0194-1. [DOI] [PubMed] [Google Scholar]
- 166.Grainger DJ, Kemp PR, Liu AC, Lawn RM, Metcalfe JC. Activation of transforming growth factor-beta is inhibited in transgenic apolipoprotein(a) mice. Nature. 1994;370:460–462. doi: 10.1038/370460a0. [DOI] [PubMed] [Google Scholar]
- 167.Grainger DJ, Kemp PR, Metcalfe JC, Liu AC, Lawn RM, Williams NR, Grace AA, Schofield PM, Chauhan A. The serum concentration of active transforming growth factor-beta is severely depressed in advanced atherosclerosis. Nat. Med. 1995;1:74–79. doi: 10.1038/nm0195-74. [DOI] [PubMed] [Google Scholar]
- 168.Mallat Z, Gojova A, Marchiol-Fournigault C, Esposito B, Kamate C, Merval R, Fradelizi D, Tedgui A. Inhibition of transforming growth factor-beta signaling accelerates atherosclerosis and induces an unstable plaque phenotype in mice. Circ. Res. 2001;89:930–934. doi: 10.1161/hh2201.099415. [DOI] [PubMed] [Google Scholar]
- 169.Mallat Z, Tedgui A. The role of transforming growth factor beta in atherosclerosis: novel insights and future perspectives. Curr. Opin. Lipidol. 2002;13:523–529. doi: 10.1097/00041433-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 170.Sie MP, Uitterlinden AG, Bos MJ, Arp PP, Breteler MM, Koudstaal PJ, Pols HA, Hofman A, van Duijn CM, Witteman JC. TGF-beta 1 polymorphisms and risk of myocardial infarction and stroke: the Rotterdam Study. Stroke. 2006;37:2667–2671. doi: 10.1161/01.STR.0000244779.30070.1a. [DOI] [PubMed] [Google Scholar]
- 171.Akira S, Hemmi H. Recognition of pathogen-associated molecular patterns by TLR family. Immunol. Lett. 2003;85:85–95. doi: 10.1016/s0165-2478(02)00228-6. [DOI] [PubMed] [Google Scholar]
- 172.Hajjar AM, Ernst RK, Tsai JH, Wilson CB, Miller SI. Human Toll-like receptor 4 recognizes host-specific LPS modifications. Nat. Immunol. 2002;3:354–359. doi: 10.1038/ni777. [DOI] [PubMed] [Google Scholar]
- 173.Dybdahl B, Wahba A, Lien E, Flo TH, Waage A, Qureshi N, Sellevold OF, Espevik T, Sundan A. Inflammatory response after open heart surgery: release of heat-shock protein 70 and signaling through toll-like receptor-4. Circulation. 2002;105:685–690. doi: 10.1161/hc0602.103617. [DOI] [PubMed] [Google Scholar]
- 174.Ueki K, Tabeta K, Yoshie H, Yamazaki K. Self-heat shock protein 60 induces tumour necrosis factor-alpha in monocyte-derived macrophage: possible role in chronic inflammatory periodontal disease. Clin. Exp. Immunol. 2002;127:72–77. doi: 10.1046/j.1365-2249.2002.01723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Underhill DM, Ozinsky A. Toll-like receptors: key mediators of microbe detection. Curr. Opin. Immunol. 2002;14:103–110. doi: 10.1016/s0952-7915(01)00304-1. [DOI] [PubMed] [Google Scholar]
- 176.Uematsu S, Akira S. Toll-like receptors and innate immunity. J. Mol. Med. 2006;84:712–725. doi: 10.1007/s00109-006-0084-y. [DOI] [PubMed] [Google Scholar]
- 177.Pasterkamp G, Van Keulen JK, De Kleijn DP. Role of Toll-like receptor 4 in the initiation and progression of atherosclerotic disease. Eur. J. Clin. Invest. 2004;34:328–334. doi: 10.1111/j.1365-2362.2004.01338.x. [DOI] [PubMed] [Google Scholar]
- 178.Xu XH, Shah PK, Faure E, Equils O, Thomas L, Fishbein MC, Luthringer D, Xu XP, Rajavashisth TB, Yano J, Kaul S, Arditi M. Toll-like receptor-4 is expressed by macrophages in murine and human lipid-rich atherosclerotic plaques and upregulated by oxidized LDL. Circulation. 2001;104:3103–3108. doi: 10.1161/hc5001.100631. [DOI] [PubMed] [Google Scholar]
- 179.Hoebe K, Georgel P, Rutschmann S, Du X, Mudd S, Crozat K, Sovath S, Shamel L, Hartung T, Zahringer U, Beutler B. CD36 is a sensor of diacylglycerides. Nature. 2005;433:523–527. doi: 10.1038/nature03253. [DOI] [PubMed] [Google Scholar]
- 180.Seimon TA, Obstfeld A, Moore KJ, Golenbock DT, Tabas I. Combinatorial pattern recognition receptor signaling alters the balance of life and death in macrophages. Proc. Natl. Acad. Sci. U. S. A. 2006;103:19794–19799. doi: 10.1073/pnas.0609671104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rock FL, Hardiman G, Timans JC, Kastelein RA, Bazan JF. A family of human receptors structurally related to Drosophila Toll. Proc. Natl. Acad. Sci. U. S. A. 1998;95:588–593. doi: 10.1073/pnas.95.2.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Arbour NC, Lorenz E, Schutte BC, Zabner J, Kline JN, Jones M, Frees K, Watt JL, Schwartz DA. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat. Genet. 2000;25:187–191. doi: 10.1038/76048. [DOI] [PubMed] [Google Scholar]
- 183.Ameziane N, Beillat T, Verpillat P, Chollet-Martin S, Aumont MC, Seknadji P, Lamotte M, Lebret D, Ollivier V, de Prost D. Association of the Toll-like receptor 4 gene Asp299Gly polymorphism with acute coronary events. Arterioscler. Thromb. Vasc. Biol. 2003;23:e61–64. doi: 10.1161/01.ATV.0000101191.92392.1D. [DOI] [PubMed] [Google Scholar]
- 184.Edfeldt K, Bennet AM, Eriksson P, Frostegard J, Wiman B, Hamsten A, Hansson GK, de Faire U, Yan ZQ. Association of hypo-responsive toll-like receptor 4 variants with risk of myocardial infarction. Eur. Heart J. 2004;25:1447–1453. doi: 10.1016/j.ehj.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 185.Holloway JW, Yang IA, Ye S. Variation in the toll-like receptor 4 gene and susceptibility to myocardial infarction. Pharmacogenet. Genomics. 2005;15:15–21. doi: 10.1097/01213011-200501000-00003. [DOI] [PubMed] [Google Scholar]
- 186.Hernesniemi J, Lehtimaki T, Rontu R, Islam MS, Eklund C, Mikkelsson J, Ilveskoski E, Kajander O, Goebeler S, Viiri LE, Hurme M, Karhunen PJ. Toll-like receptor 4 polymorphism is associated with coronary stenosis but not with the occurrence of acute or old myocardial infarctions. Scand. J. Clin. Lab. Invest. 2006;66:667–675. doi: 10.1080/00365510600933011. [DOI] [PubMed] [Google Scholar]
- 187.Koch W, Hoppmann P, Pfeufer A, Schomig A, Kastrati A. Toll-like receptor 4 gene polymorphisms and myocardial infarction: no association in a Caucasian population. Eur. Heart J. 2006;27:2524–2529. doi: 10.1093/eurheartj/ehl231. [DOI] [PubMed] [Google Scholar]
- 188.Kunjathoor VV, Febbraio M, Podrez EA, Moore KJ, Andersson L, Koehn S, Rhee JS, Silverstein R, Hoff HF, Freeman MW. Scavenger receptors class A-I/II and CD36 are the principal receptors responsible for the uptake of modified low density lipoprotein leading to lipid loading in macrophages. J. Biol. Chem. 2002;277:49982–49988. doi: 10.1074/jbc.M209649200. [DOI] [PubMed] [Google Scholar]
- 189.Matsumoto A, Naito M, Itakura H, Ikemoto S, Asaoka H, Hayakawa I, Kanamori H, Aburatani H, Takaku F, Suzuki H, Kobari Y, Miyai T, Takahashi K, Cohen E H, Wydro R, Housman DE, Kodama T. Human macrophage scavenger receptors: primary structure, expression, and localization in atherosclerotic lesions. Proc. Natl. Acad. Sci. U. S. A. 1990;87:9133–9137. doi: 10.1073/pnas.87.23.9133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Emi M, Asaoka H, Matsumoto A, Itakura H, Kurihara Y, Wada Y, Kanamori H, Yazaki Y, Takahashi E, Lepert M, Lalouel JM, Kodama T, Mukai T. Structure, organization, and chromosomal mapping of the human macrophage scavenger receptor gene. J. Biol. Chem. 1993;268:2120–2125. [PubMed] [Google Scholar]
- 191.Xu J, Zheng SL, Komiya A, Mychaleckyj JC, Isaacs SD, Hu JJ, Sterling D, Lange EM, Hawkins GA, Turner A, Ewing CM, Faith DA, Johnson JR, Suzuki H, Bujnovszky P, Wiley KE, DeMarzo AM, Bova GS, Chang B, Hall MC, McCullough DL, Partin AW, Kassabian VS, Carpten JD, Bailey-Wilson JE, Trent JM, Ohar J, Bleecker ER, Walsh PC, Isaacs WB, Meyers DA. Germline mutations and sequence variants of the macrophage scavenger receptor 1 gene are associated with prostate cancer risk. Nat. Genet. 2002;32:321–325. doi: 10.1038/ng994. [DOI] [PubMed] [Google Scholar]
- 192.Giachelli CM, Steitz S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 2000;19:615–622. doi: 10.1016/s0945-053x(00)00108-6. [DOI] [PubMed] [Google Scholar]
- 193.Ikeda T, Shirasawa T, Esaki Y, Yoshiki S, Hirokawa K. Osteopontin mRNA is expressed by smooth muscle-derived foam cells in human atherosclerotic lesions of the aorta. J. Clin. Invest. 1993;92:2814–2820. doi: 10.1172/JCI116901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Fitzpatrick LA, Severson A, Edwards WD, Ingram RT. Diffuse calcification in human coronary arteries. Association of osteopontin with atherosclerosis. J. Clin. Invest. 1994;94:1597–1604. doi: 10.1172/JCI117501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Srivatsa SS, Harrity PJ, Maercklein PB, Kleppe L, Veinot J, Edwards WD, Johnson CM, Fitzpatrick LA. Increased cellular expression of matrix proteins that regulate mineralization is associated with calcification of native human and porcine xenograft bioprosthetic heart valves. J. Clin. Invest. 1997;99:996–1009. doi: 10.1172/JCI119265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Liaw L, Almeida M, Hart CE, Schwartz SM, Giachelli CM. Osteopontin promotes vascular cell adhesion and spreading and is chemotactic for smooth muscle cells in vitro. Circ. Res. 1994;74:214–224. doi: 10.1161/01.res.74.2.214. [DOI] [PubMed] [Google Scholar]
- 197.Senger DR, Ledbetter SR, Claffey KP, Papadopoulos-Sergiou A, Peruzzi CA, Detmar M. Stimulation of endothelial cell migration by vascular permeability factor/vascular endothelial growth factor through cooperative mechanisms involving the alphavbeta3 integrin, osteopontin, and thrombin. Am. J. Pathol. 1996;149:293–305. [PMC free article] [PubMed] [Google Scholar]
- 198.Crosby AH, Lyu MS, Lin K, McBride OW, Kerr JM, Aplin HM, Fisher LW, Young MF, Kozak CA, Dixon MJ. Mapping of the human and mouse bone sialoprotein and osteopontin loci. Mamm. Genome. 1996;7:149–151. doi: 10.1007/s003359900037. [DOI] [PubMed] [Google Scholar]
- 199.Taylor BC, Schreiner PJ, Doherty TM, Fornage M, Carr JJ, Sidney S. Matrix Gla protein and osteopontin genetic associations with coronary artery calcification and bone density: the CARDIA study. Hum. Genet. 2005;116:525–528. doi: 10.1007/s00439-005-1258-3. [DOI] [PubMed] [Google Scholar]
- 200.Brenner D, Labreuche J, Touboul PJ, Schmidt-Petersen K, Poirier O, Perret C, Schonfelder J, Combadiere C, Lathrop M, Cambien F, Brand-Herrmann SM, Amarenco P. Cytokine polymorphisms associated with carotid intima-media thickness in stroke patients. Stroke. 2006;37:1691–1696. doi: 10.1161/01.STR.0000226565.76113.6c. [DOI] [PubMed] [Google Scholar]
- 201.Tan K B, Harrop J, Reddy M, Young P, Terrett J, Emery J, Moore G, Truneh A. Characterization of a novel TNF-like ligand and recently described TNF ligand and TNF receptor superfamily genes and their constitutive and inducible expression in hematopoietic and non-hematopoietic cells. Gene. 1997;204:35–46. doi: 10.1016/s0378-1119(97)00509-x. [DOI] [PubMed] [Google Scholar]
- 202.Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen H, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309–319. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 203.Min H, Morony S, Sarosi I, Dunstan CR, Capparelli C, Scully S, Van G, Kaufman S, Kostenuik PJ, Lacey DL, Boyle WJ, Simonet WS. Osteoprotegerin reverses osteoporosis by inhibiting endosteal osteoclasts and prevents vascular calcification by blocking a process resembling osteoclastogenesis. J. Exp. Med. 2000;192:463–474. doi: 10.1084/jem.192.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Golledge J, McCann M, Mangan S, Lam A, Karan M. Osteoprotegerin and osteopontin are expressed at high concentrations within symptomatic carotid atherosclerosis. Stroke. 2004;35:1636–1641. doi: 10.1161/01.STR.0000129790.00318.a3. [DOI] [PubMed] [Google Scholar]
- 205.Rhee EJ, Oh KW, Jung CH, Lee WY, Oh ES, Yun EJ, Baek KH, Kang MI, Kim SW. The relationship between four single nucleotide polymorphisms in the promoter region of the osteoprotegerin gene and aortic calcification or coronary artery disease in Koreans. Clin. Endocrinol. (Oxf) 2006;64:689–697. doi: 10.1111/j.1365-2265.2006.02530.x. [DOI] [PubMed] [Google Scholar]
- 206.Soufi M, Schoppet M, Sattler AM, Herzum M, Maisch B, Hofbauer LC, Schaefer JR. Osteoprotegerin gene polymorphisms in men with coronary artery disease. J. Clin. Endocrinol. Metab. 2004;89:3764–3768. doi: 10.1210/jc.2003-032054. [DOI] [PubMed] [Google Scholar]
- 207.Greenlee KJ, Werb Z, Kheradmand F. Matrix metalloproteinases in lung: multiple, multifarious, and multifaceted. Physiol. Rev. 2007;87:69–98. doi: 10.1152/physrev.00022.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Loftus IM, Naylor AR, Goodall S, Crowther M, Jones L, Bell PR, Thompson MM. Increased matrix metalloproteinase-9 activity in unstable carotid plaques. A potential role in acute plaque disruption. Stroke. 2000;31:40–47. doi: 10.1161/01.str.31.1.40. [DOI] [PubMed] [Google Scholar]
- 209.Ghilardi G, Biondi ML, DeMonti M, Turri O, Guagnellini E, Scorza R. Matrix metalloproteinase-1 and matrix metalloproteinase-3 gene promoter polymorphisms are associated with carotid artery stenosis. Stroke. 2002;33:2408–2412. doi: 10.1161/01.str.0000031929.05665.da. [DOI] [PubMed] [Google Scholar]
- 210.Fiotti N, Altamura N, Fisicaro M, Carraro N, Uxa L, Grassi G, Torelli L, Gobbato R, Guarnieri G, Baxter BT, Giansante C. MMP-9 microsatellite polymorphism and susceptibility to carotid arteries atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2006;26:1330–1336. doi: 10.1161/01.ATV.0000219233.31702.c9. [DOI] [PubMed] [Google Scholar]
- 211.Lange LA, Lange EM, Bielak LF, Langefeld CD, Kardia SL, Royston P, Turner ST, Sheedy PF 2nd, Boerwinkle E, Peyser PA. Autosomal genome-wide scan for coronary artery calcification loci in sibships at high risk for hypertension. Arterioscler. Thromb. Vasc. Biol. 2002;22:418–423. doi: 10.1161/hq0302.105721. [DOI] [PubMed] [Google Scholar]
- 212.Smith CL, Anthony S, Hubank M, Leiper JM, Vallance P. Effects of ADMA upon gene expression: an insight into the pathophysiological significance of raised plasma ADMA. PLoS. Med. 2005;2:e264. doi: 10.1371/journal.pmed.0020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Boger RH, Vallance P, Cooke JP. Asymmetric dimethylarginine (ADMA): a key regulator of nitric oxide synthase. Atheroscler Supp1. 2003;4:1–3. doi: 10.1016/s1567-5688(03)00027-8. [DOI] [PubMed] [Google Scholar]
- 214.Wang D, Yang H, Quinones MJ, Bulnes-Enriquez I, Jimenez X, De La Rosa R, Modilevsky T, Yu K, Li Y, Taylor KD, Hsueh WA, Hodis HN, Rotter JI. A genome-wide scan for carotid artery intima-media thickness: the Mexican-American Coronary Artery Disease family study. Stroke. 2005;36:540–545. doi: 10.1161/01.STR.0000155746.65185.4e. [DOI] [PubMed] [Google Scholar]
- 215.Pajukanta P, Cargill M, Viitanen L, Nuotio I, Kareinen A, Perola M, Terwilliger JD, Kempas E, Daly M, Lilja H, Rioux JD, Brettin T, Viikari JS, Ronnemaa T, Laakso M, Lander ES, Peltonen L. Two loci on chromosomes 2 and X for premature coronary heart disease identified in early- and late-settlement populations of Finland. Am. J. Hum. Genet. 2000;67:1481–1493. doi: 10.1086/316902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Francke S, Manraj M, Lacquemant C, Lecoeur C, Lepretre F, Passa P, Hebe A, Corset L, Yan SL, Lahmidi S, Jankee S, Gunness TK, Ramjuttun US, Balgobin V, Dina C, Froguel P. A genome-wide scan for coronary heart disease suggests in Indo-Mauritians a susceptibility locus on chromosome 16p13 and replicates linkage with the metabolic syndrome on 3q27. Hum. Mol. Genet. 2001;10:2751–2765. doi: 10.1093/hmg/10.24.2751. [DOI] [PubMed] [Google Scholar]
- 217.Broeckel U, Hengstenberg C, Mayer B, Holmer S, Martin LJ, Comuzzie AG, Blangero J, Nurnberg P, Reis A, Riegger GA, Jacob HJ, Schunkert H. A comprehensive linkage analysis for myocardial infarction and its related risk factors. Nat. Genet. 2002;30:210–214. doi: 10.1038/ng827. [DOI] [PubMed] [Google Scholar]
- 218.Harrap SB, Zammit KS, Wong ZY, Williams FM, Bahlo M, Tonkin AM, Anderson ST. Genome-wide linkage analysis of the acute coronary syndrome suggests a locus on chromosome 2. Arterioscler. Thromb. Vasc. Biol. 2002;22:874–878. doi: 10.1161/01.atv.0000016258.40568.f1. [DOI] [PubMed] [Google Scholar]
- 219.Hauser ER, Crossman DC, Granger CB, Haines JL, Jones CJ, Mooser V, McAdam B, Winkelmann BR, Wiseman AH, Muhlestein JB, Bartel AG, Dennis CA, Dowdy E, Estabrooks S, Eggleston K, Francis S, Roche K, Clevenger PW, Huang L, Pedersen B, Shah S, Schmidt S, Haynes C, West S, Asper D, Booze M, Sharma S, Sundseth S, Middleton L, Roses AD, Hauser MA, Vance JM, Pericak-Vance MA, Kraus WE. A genomewide scan for early-onset coronary artery disease in 438 families: the GENECARD Study. Am. J. Hum. Genet. 2004;75:436–447. doi: 10.1086/423900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Helgadottir A, Manolescu A, Thorleifsson G, Gretarsdottir S, Jonsdottir H, Thorsteinsdottir U, Samani NJ, Gudmundsson G, Grant SF, Thorgeirsson G, Sveinbjornsdottir S, Valdimarsson EM, Matthiasson SE, Johannsson H, Gudmundsdottir O, Gurney ME, Sainz J, Thorhallsdottir M, Andresdottir M, Frigge ML, Topol EJ, Kong A, Gudnason V, Hakonarson H, Gulcher JR, Stefansson K. The gene encoding 5-lipoxygenase activating protein confers risk of myocardial infarction and stroke. Nat. Genet. 2004;36:233–239. doi: 10.1038/ng1311. [DOI] [PubMed] [Google Scholar]
- 221.Wang Q, Rao S, Shen GQ, Li L, Moliterno DJ, Newby LK, Rogers WJ, Cannata R, Zirzow E, Elston RC, Topol EJ. Premature myocardial infarction novel susceptibility locus on chromosome 1P34-36 identified by genomewide linkage analysis. Am. J. Hum. Genet. 2004;74:262–271. doi: 10.1086/381560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Samani NJ, Burton P, Mangino M, Ball SG, Balmforth AJ, Barrett J, Bishop T, Hall A. A genomewide linkage study of 1,933 families affected by premature coronary artery disease: The British Heart Foundation (BHF) Family Heart Study. Am. J. Hum. Genet. 2005;77:1011–1020. doi: 10.1086/498653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Helgadottir A, Manolescu A, Helgason A, Thorleifsson G, Thorsteinsdottir U, Gudbjartsson DF, Gretarsdottir S, Magnusson KP, Gudmundsson G, Hicks A, Jonsson T, Grant SF, Sainz J, O'Brien SJ, Sveinbjornsdottir S, Valdimarsson EM, Matthiasson SE, Levey AI, Abramson JL, Reilly MP, Vaccarino V, Wolfe ML, Gudnason V, Quyyumi AA, Topol EJ, Rader DJ, Thorgeirsson G, Gulcher JR, Hakonarson H, Kong A, Stefansson K. A variant of the gene encoding leukotriene A4 hydrolase confers ethnicity-specific risk of myocardial infarction. Nat. Genet. 2006;38:68–74. doi: 10.1038/ng1692. [DOI] [PubMed] [Google Scholar]
- 224.Peacock JM, Arnett DK, Atwood LD, Myers RH, Coon H, Rich SS, Province MA, Heiss G. Genome scan for quantitative trait loci linked to high-density lipoprotein cholesterol: The NHLBI Family Heart Study. Arterioscler. Thromb. Vasc. Biol. 2001;21:1823–1828. doi: 10.1161/hq1101.097804. [DOI] [PubMed] [Google Scholar]
- 225.Gagnon F, Jarvik GP, Badzioch MD, Motulsky AG, Brunzell JD, Wijsman EM. Genome scan for quantitative trait loci influencing HDL levels: evidence for multilocus inheritance in familial combined hyperlipidemia. Hum. Genet. 2005;117:494–505. doi: 10.1007/s00439-005-1338-4. [DOI] [PubMed] [Google Scholar]
- 226.Soro A, Pajukanta P, Lilja HE, Ylitalo K, Hiekkalinna T, Perola M, Cantor RM, Viikari JS, Taskinen MR, Peltonen L. Genome scans provide evidence for low-HDL-C loci on chromosomes 8q23, 16q24.1-24.2, and 20q13.11 in Finnish families. Am. J. Hum. Genet. 2002;70:1333–1340. doi: 10.1086/339988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pollin TI, Hsueh WC, Steinle NI, Snitker S, Shuldiner AR, Mitchell BD. A genome-wide scan of serum lipid levels in the Old Order Amish. Atherosclerosis. 2004;173:89–96. doi: 10.1016/j.atherosclerosis.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 228.Austin MA, Edwards KL, Monks SA, Koprowicz KM, Brunzell JD, Motulsky AG, Mahaney MC, Hixson JE. Genome-wide scan for quantitative trait loci influencing LDL size and plasma triglyceride in familial hypertriglyceridemia. J. Lipid Res. 2003;44:2161–2168. doi: 10.1194/jlr.M300272-JLR200. [DOI] [PubMed] [Google Scholar]
- 229.Shearman AM, Ordovas JM, Cupples LA, Schaefer EJ, Harmon MD, Shao Y, Keen JD, DeStefano AL, Joost O, Wilson PW, Housman DE, Myers RH. Evidence for a gene influencing the TG/HDL-C ratio on chromosome 7q32.3-qter: a genome-wide scan in the Framingham study. Hum. Mol. Genet. 2000;9:1315–1320. doi: 10.1093/hmg/9.9.1315. [DOI] [PubMed] [Google Scholar]
- 230.de Lange M, Spector TD, Andrew T. Genome-wide scan for blood pressure suggests linkage to chromosome 11, and replication of loci on 16, 17, and 22. Hypertension. 2004;44:872–877. doi: 10.1161/01.HYP.0000148994.89903.fa. [DOI] [PubMed] [Google Scholar]