Abstract
Background
Current models for assessing breast cancer risk are complex and do not include breast density, a strong risk factor for breast cancer that is routinely reported with mammography.
Objective
To develop and validate an easy-to-use breast cancer risk prediction model that includes breast density.
Design
Empirical model based on Surveillance, Epidemiology, and End Results incidence, and relative hazards from a prospective cohort.
Setting
Screening mammography sites participating in the Breast Cancer Surveillance Consortium.
Patients
1 095 484 women undergoing mammography who had no previous diagnosis of breast cancer.
Measurements
Self-reported age, race or ethnicity, family history of breast cancer, and history of breast biopsy. Community radiologists rated breast density by using 4 Breast Imaging Reporting and Data System categories.
Results
During 5.3 years of follow-up, invasive breast cancer was diagnosed in 14 766 women. The breast density model was well calibrated overall (expected–observed ratio, 1.03 [95% CI, 0.99 to 1.06]) and in racial and ethnic subgroups. It had modest discriminatory accuracy (concordance index, 0.66 [CI, 0.65 to 0.67]). Women with low-density mammograms had 5-year risks less than 1.67% unless they had a family history of breast cancer and were older than age 65 years.
Limitation
The model has only modest ability to discriminate between women who will develop breast cancer and those who will not.
Conclusion
A breast cancer prediction model that incorporates routinely reported measures of breast density can estimate 5-year risk for invasive breast cancer. Its accuracy needs to be further evaluated in independent populations before it can be recommended for clinical use.
In 2007, breast cancer will have been diagnosed in more than 178 000 women in the United States, and more than 40 000 women will have died of breast cancer (1). Most of these women never had their risk for breast cancer assessed, and even fewer considered chemoprevention (2–5). Providing women with an estimate of their risk for breast cancer would provide an opportunity for them to consider options to decrease their risk. Women at low short-term risk for breast cancer may experience less anxiety about their health and would be less likely to benefit from prevention efforts. Women at very high risk may warrant additional screening tests, such as breast magnetic resonance imaging (6), and might benefit from chemoprevention of breast cancer with tamoxifen or raloxifene. The standard risk assessment model available to practitioners (the Gail model) (7) identifies only a minority of women who eventually develop breast cancer being at high risk (8). Better breast cancer risk prediction tools are needed (9).
The radiographic appearance of the breast has been consistently shown to be a major risk factor for breast cancer, whether it is defined by a qualitative assessment of the parenchymal pattern or a quantitative measure of percentage of density (10–12). Women in whom more than 50% of total breast area is mammographically dense have high breast density and are at 3- to 5-fold greater risk for breast cancer than women in whom breast density is less than 25% (10, 13–16). The increased risk for breast cancer associated with breast density is due in part to the lower sensitivity of mammography in dense breasts (17–19), but the association remains strong after accounting for masking (20, 21). Mammographically dense breast tissue is rich in epithelium and stroma (10), and the association could represent activation of epithelial cells or fibroblasts (22–25). Recently, several models have been published that incorporate breast density: One uses a continuous measure of breast density that is not available to clinicians and has not been validated (26), and the other predicts 1-year risk for breast cancer (27).
We previously demonstrated that a simple model based on age, ethnicity, and a categorical measure of breast density had predictive accuracy similar to that of the Gail model in a multiethnic cohort of women receiving screening mammograms in northern California (28). We expand on that work by using data from more than 1 million ethnically diverse women throughout the United States to develop and validate a risk assessment tool that incorporates breast density and therefore might improve breast cancer screening and prevention efforts.
Methods
Study Population
We included 1 095 484 women age 35 years or older who had had at least 1 mammogram with breast density measured by using the Breast Imaging Reporting and Data System (BI-RADS) classification system in any of the 7 mammography registries participating in the National Cancer Institute–funded Breast Cancer Surveillance Consortium (BCSC) (available at http://breastscreening.cancer.gov) (29). The BCSC is a community-based, ethnically and geographically diverse sample that broadly represents the United States (30).
We excluded women who had a diagnosis of breast cancer before their first eligible mammography examination. Because our goal was to develop a model of long-term risk for invasive breast cancer, we excluded women with cancer diagnosed in the first 6 months of follow-up to minimize the number of cases of cancer included in the model that were diagnosed on the basis of the mammogram used for risk assessment. Women were also excluded if they had breast implants. Women in whom ductal carcinoma in situ was diagnosed were censored at the time of diagnosis in the primary analysis. When women had several mammograms, we based our analysis on findings from the first mammogram.
Each registry obtains annual approval from its institutional review board for consenting processes or a waiver of consent, enrollment of participants, and ongoing data linkage for research purposes. All registries have received a Certificate of Confidentiality from the federal government that protects the identities of research participants.
Measurement of Risk Factors
Patient information was obtained primarily from self-report at the time of mammography. We selected 2 risk factors in addition to breast density for inclusion in the model on the basis of simplicity (yes or no) and a high attributable risk: history of breast cancer in a first-degree relative and history of a breast biopsy. Body mass index was later considered for addition to the model, but it was excluded to maintain parsimony and because it had minimal effect on model discrimination (the increase in the concordance statistic [c-statistic] was only 0.003). For modeling and validation, missing data for relatives with breast cancer and number of breast biopsies were set to 0. The 5-year Gail risk was computed for each woman by using the algorithms provided by the National Cancer Institute to calculate the Gail model risk for individual women (31). For Gail model calculations, missing data were coded as specified by that model (age at menarche as ≥14 years, age at first live birth as <20 years, number of breast biopsies as 0, and number of first-degree relatives as 0). Ethnicity was coded by using the expanded race and ethnicity definition currently used in the Surveillance, Epidemiology, and End Results (SEER) database and U.S. Vital Statistics (non-Hispanic White, non-Hispanic Black, Asian or Pacific Islander, Native American/Alaskan Native, Hispanic, or other). We classified women who self-identified as mixed or other race with participants who did not report race and ethnicity.
Breast Density
Community radiologists at each site classified breast density on screening mammograms as part of routine clinical practice by using the American College of Radiology BI-RADS density categories (32): almost entirely fat (category 1), scattered fibroglandular densities (category 2), heterogeneously dense (category 3), and extremely dense (category 4). The BI-RADS category 2 was used as the reference group for breast density because it formed the largest group.
Ascertainment of Breast Cancer Cases
Breast cancer outcomes (invasive cancer and ductal carcinoma in situ) were obtained at each site through linkage with the regional population-based SEER program, state tumor registries, and pathology databases.
Vital Status
Vital status was obtained through linkage to SEER registries, state tumor registries, and the individual state vital statistics or the National Death Index.
Model Development
We used a proportional hazards model of invasive breast cancer to estimate the hazard ratios for each BI-RADS breast density category. Women entered the model 6 months after the index mammogram and were censored at the time of death, diagnosis of ductal carcinoma in situ, or the end of follow-up. All models were adjusted for age (in 5-year intervals) and race and ethnicity. The strength of the breast density association with breast cancer was greater for women younger than age 65 years (P for interaction < 0.001). Thus, separate models were fitted for women younger than age 65 years and for women age 65 years or older. No other interaction terms were included in the final model. We calculated similar estimates for first-degree relatives with breast cancer (yes or no) and a personal history of breast biopsy (yes or no) from the BCSC. All predictors met the proportional hazards assumption that was assessed by log–log plots and by including interaction terms with time for each predictor variable.
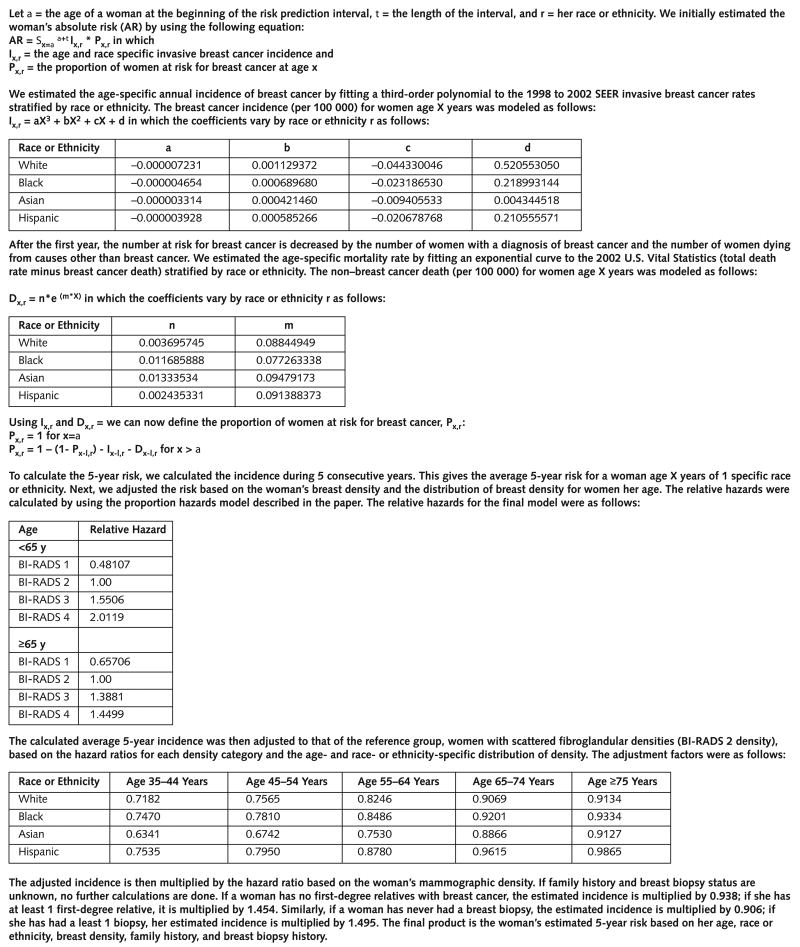
We then developed an absolute risk model by using methods described in the Appendix Figure (available at www.annals.org). The model primarily estimates predicted incidence of invasive breast cancer by using age, race or ethnicity, and breast density. These estimates are then adjusted for family history and biopsy history if available. We based our estimates of breast cancer incidence on the SEER age- and ethnicity-specific risk for invasive breast cancer (1992 to 2002) (33). Age-specific incidence for each ethnic group was estimated by fitting a third-order polynomial model to the SEER data. Age-specific incidence rates for the Native American and Alaskan Native group were inconsistent in SEER, so we excluded this group from further analyses. We calculated the baseline risk for the model by adjusting SEER incidence for the population's attributable risk for each breast density subgroup. We estimated the age- and ethnicity-specific distribution of mammographic breast density needed for these calculations by using data from a larger set of 3 343 047 mammograms from the BCSC. The distribution of breast density varied statistically significantly by age and by race or ethnicity (P < 0.001 for each comparison). The model used these variations by age and race to distribute the 5-year risk for invasive breast cancer across the 4 breast density subgroups. We used the methods described by Gail and colleagues (7) to translate the hazard ratios and risk factor distributions into absolute risks. The age-, sex-, and ethnicity-specific competing risks for death for women were calculated by using 2002 U.S. Vital Statistics (34). Age-specific death for each ethnic group was estimated by fitting an exponential model to the 2002 U.S. Vital Statistics. To assess the effect of breast density on the model, we developed a similar model, the risk factor model, by using the same approach but excluding breast density.
Statistical Analysis
We developed the model by using a random sample of 60% of the women and validated it in the remaining 40%. Model calibration was assessed by calculating the ratio of expected cases of breast cancer to observed cases of breast cancer (expected–observed ratio) by age group, race or ethnicity, individual risk factor distributions, decile of predicted risk, and Gail risk. The 95% CI for this ratio was calculated by assuming that the observed breast cancer events follow a Poisson distribution; thus, we calculated the CI as follows: (expected–observed ratio)*exp (± 1.96*1/sqrt [O]). For a group of women, calibration assesses how closely the number of women in whom the model predicts that breast cancer will develop matches the actual number of women in whom breast cancer is diagnosed. An expected–observed ratio of 1.0 would indicate perfect calibration.
We summarized the discriminatory accuracy of the model by using the c-statistic (35). Standard errors used to calculate 95% CIs around the c-statistic were estimated by using the method of DeLong and colleagues (36). We calculated the age-adjusted c-statistic by using the method of Rockhill and colleagues (37). We also used a 5-fold cross-validation to confirm the internal validity of the model (38, 39). The c-statistic measures the ability of the model to separate women who will develop breast cancer from those who will not by calculating the proportion of pairs of women in which the woman with breast cancer has a higher predicted risk than the woman without breast cancer. A c-statistic of 0.5 is equivalent to no discrimination, and a c-statistic of 1.0 indicates perfect discrimination between women who develop breast cancer and women who do not.
We used the derivation sample to guide model development and the validation sample to assess calibration and discrimination of the model predictions. To evaluate the contribution of breast density in addition to clinical risk factors and for comparisons with the Gail model, we limited analyses to the 629 229 women with complete follow-up information from 0.5 to 5.5 years from the index mammogram (a 5-year interval). We used the method advocated by Cook and colleagues (40, 41) to compare the model based on breast density with a model based on clinical risk factors. Because data were missing, direct comparisons between the breast density model and the Gail model may be biased against the Gail model and should be interpreted with caution. We reported incidence rates per 500 woman-years in the larger data set of women with variable follow-up length to approximate 5-year risks. A 2-sided P value of 0.05 or less was considered statistically significant. All analyses were done by using Stata, version 9.2 (Stata, College Station, Texas).
Role of the Funding Source
The BCSC and Building Interdisciplinary Research Careers in Women's Health had no role in the design, conduct, and analysis of this study, nor did they participate in the decision to submit the manuscript for publication.
Results
At the time of their earliest mammogram in the BCSC, 46% of women in our study were younger than age 50 years (Table 1). The majority of women were white (71%), but more than 25 000 women represented each of the black, Asian, and Hispanic groups. During a median follow-up of 5.3 years, 14 766 women developed invasive breast cancer. As expected, older age, non-Hispanic white race or ethnicity, a family history of breast cancer, a personal history of breast biopsies, and high breast density were all associated with the development of breast cancer (Table 1).
Table 1. Baseline Patient Characteristics*.
| Risk Factor | Patients without Breast Cancer, n (%) | Patients with Breast Cancer, n (%) | All Patients, n (%) |
|---|---|---|---|
| Age | |||
| 35–39 y | 102 884 (10) | 518 (4) | 103 402 (9) |
| 40–44 y | 213 318 (20) | 1557 (11) | 214 875 (20) |
| 45–49 y | 182 151 (17) | 2038 (14) | 184 189 (17) |
| 50–54 y | 162 150 (15) | 2284 (15) | 164 434 (15) |
| 55–59 y | 113 155 (10) | 2049 (14) | 115 204 (11) |
| 60–64 y | 89 792 (8) | 1753 (12) | 91 545 (8) |
| 65–69 y | 79 944 (7) | 1718 (12) | 81 662 (7) |
| 70–74 y | 66 482 (6) | 1543 (10) | 68 025 (6) |
| 75–79 y | 47 031 (4) | 904 (6) | 47 935 (4) |
| 80–84 y | 23 811 (2) | 402 (3) | 24 213 (2) |
| Race or ethnicity | |||
| White, non-Hispanic | 764 265 (71) | 11 181 (76) | 775 446 (71) |
| Black, non-Hispanic | 72 995 (7) | 853 (6) | 73 848 (7) |
| Asian or Pacific Islander | 28 931 (3) | 249 (2) | 29 180 (3) |
| Native American | 8746 (1) | 59 (0.4) | 8805 (1) |
| Hispanic | 81 866 (8) | 694 (5) | 82 560 (8) |
| Other, mixed, unknown | 123 915 (11) | 1730 (12) | 125 645 (11) |
| First-degree relatives with breast cancer | |||
| 0 | 891 022 (82) | 11 246 (76) | 902 268 (82) |
| 1 | 90 144 (8) | 1821 (12) | 91 965 (8) |
| ≥2 | 35 626 (3) | 951 (6) | 36 577 (3) |
| Missing | 69 926 (6) | 748 (5) | 64 674 (6) |
| Age at menarche | |||
| ≥14 y | 80 559 (7) | 1212 (8) | 81 771 (7) |
| 12 or 13 y | 98 980 (9) | 1557 (11) | 100 537 (9) |
| <12 y | 147 535 (14) | 2417 (16) | 149 952 (14) |
| Missing | 753 644 (70) | 9580 (65) | 763 224 (70) |
| Age at first birth | |||
| <20 y | 91 284 (8) | 979 (7) | 92 263 (8) |
| 20–24 y | 149 142 (14) | 2089 (14) | 151 231 (14) |
| 25–29 y or nulliparous | 183 772 (17) | 2744 (19) | 186 516 (17) |
| ≥30 y | 74 317 (7) | 1132 (8) | 75 449 (7) |
| Missing | 582 203 (54) | 7822 (53) | 590 025 (54) |
| Breast biopsies | |||
| 0 | 671 587 (62) | 7184 (49) | 678 771 (62) |
| ≥1 | 168 784 (16) | 4212 (28) | 172 996 (16) |
| Missing | 240 347 (22) | 3370 (23) | 243 717 (22) |
| BI-RADS breast density classification | |||
| Almost entirely fat (category 1) | 100 502 (9) | 831 (6) | 101 333 (9) |
| Scattered fibroglandular densities (category 2) | 474 282 (44) | 5968 (40) | 480 250 (44) |
| Heterogeneously dense (category 3) | 407 050 (38) | 6281 (43) | 413 331 (38) |
| Extremely dense (category 4) | 98 884 (9) | 1686 (11) | 100 570 (9) |
BI-RADS — Breast Imaging Reporting and Data System.
The strength of the association between breast density and breast cancer was greater for women younger than age 65 years (the relative hazard for extremely dense versus almost entirely fat breasts decreased from 4.2 to 2.2; P for interaction < 0.001). The distribution of breast density also varied by age and race or ethnicity (P < 0.001). The proportion of women with extremely dense breasts was greatest among Asian women at all age ranges (Table 2) and decreased with age across all race or ethnicity groups.
Table 2. Variation in the Distribution of Mammographic Density, by Age and Race or Ethnicity*.
| BI-RADS Density Category | Race or Ethnicity, n (%) | |||
|---|---|---|---|---|
| White | Black | Asian | Hispanic | |
| Age <50 y | ||||
| Almost entirely fat | 30 969 (4) | 4579 (6) | 349 (1) | 6133 (7) |
| Scattered fibroglandular densities | 265 277 (35) | 31 741 (38) | 4852 (19) | 33 418 (38) |
| Heterogeneously dense | 354 545 (47) | 38 619 (47) | 12 978 (52) | 38 071 (44) |
| Extremely dense | 103 397 (14) | 8085 (10) | 6752 (27) | 9320 (11) |
| Age 50–64 y | ||||
| Almost entirely fat | 66 005 (7) | 6671 (9) | 1188 (4) | 11 426 (12) |
| Scattered fibroglandular densities | 413 961 (47) | 37 267 (49) | 10 450 (35) | 45 999 (49) |
| Heterogeneously dense | 351 884 (40) | 28 956 (38) | 14 438 (48) | 30 833 (33) |
| Extremely dense | 56 931 (6) | 3427 (4) | 3945 (13) | 5027 (5) |
| Age ≥65 y | ||||
| Almost entirely fat | 66 184 (11) | 5807 (12) | 1889 (13) | 9697 (20) |
| Scattered fibroglandular densities | 320 899 (54) | 26 411 (56) | 6825 (46) | 25 593 (54) |
| Heterogeneously dense | 187 657 (32) | 13 600 (29) | 5049 (34) | 10 984 (23) |
| Extremely dense | 20 535 (3) | 1205 (3) | 982 (7) | 1348 (3) |
BI-RADS — Breast Imaging Reporting and Data System.
The model was well calibrated in the validation sample (Table 3). Within a subset of the validation cohort with 5 years of follow-up, the observed rate of invasive breast cancer was 1.38% (3465 cases of cancer among 251 789 women). The expected rate according to the model was 1.41% (expected–observed ratio, 1.03 [CI, 0.99% to 1.06%]). Model discrimination measured by the c-statistic in the validation set was 0.660 (CI, 0.651 to 0.669), which was statistically and possibly clinically significantly greater than that of the Gail model (c-statistic, 0.613 [CI, 0.604 to 0.622]). In addition, the average c-statistic from 5-fold cross-validation was 0.6576. As expected, age-adjusted c-statistics were lower for both the breast density model (0.622) and the Gail model (0.562).
Table 3. Overall Calibration and Discrimination of the Breast Cancer Surveillance Consortium Breast Density Model among Women with 5 Years of Follow-up.
| Sample | Women, n | Expected 5-Year Rate | Observed 5-Year Rate | Expected–Observed Rate Ratio (95% CI)* | Concordance Statistic (95% CI) |
|---|---|---|---|---|---|
| Development | 377 440 | 1.41 | 1.41 | 1.00 (0.98–1.03) | 0.657 (0.65–0.67) |
| Validation | 251 789 | 1.41 | 1.38 | 1.03 (0.99–1.06) | 0.660 (0.65–0.66) |
| Total | 629 229 | 1.41 | 1.40 | 1.01 (0.99–1.03) | 0.658 (0.65–0.66) |
Expected rate divided by the observed rate. The observed 5-year rate is the actual rate observed in the individual subcohorts. The expected rate is the average of the Breast Cancer Surveillance Consortium breast density model predicted risk for each woman in the subcohort. No additional adjustments were done.
Calibration of the model was reasonably accurate across risk factor subgroups (Table 4). The model slightly underestimated breast cancer rates in younger women (expected– observed ratio, 0.94 for women age 40 to 44 years). It also underestimated cancer rates among Asian (expected– observed ratio, 0.95) and Hispanic women (expected–observed ratio, 0.94). The model was well calibrated across other risk factor subgroups, including those defined by the Gail model.
Table 4. Calibration of the Breast Cancer Surveillance Consortium Breast Density Model in Risk Factor Subgroups*.
| Risk Factor Group | Expected 5-Year Rate | Observed 5-Year Rate | Expected–Observed Rate Ratio (95% CI) | Concordance Statistic |
|---|---|---|---|---|
| Total cohort | 1.41 | 1.40 | 1.01 (0.99–1.03) | 0.66 |
| Age | ||||
| 40–44 y | 0.68 | 0.73 | 0.94 (0.89–1.00) | 0.63 |
| 45–49 y | 1.06 | 1.07 | 0.99 (0.94–1.04) | 0.61 |
| 50–54 y | 1.33 | 1.38 | 0.96 (0.92–1.01) | 0.62 |
| 55–59 y | 1.72 | 1.77 | 0.97 (0.92–1.02) | 0.64 |
| 60–64 y | 1.94 | 1.87 | 1.04 (0.98–1.10) | 0.63 |
| 65–69 y | 2.23 | 1.97 | 1.13 (1.07–1.20) | 0.60 |
| 70–74 y | 2.34 | 2.17 | 1.08 (1.02–1.15) | 0.61 |
| Race or ethnicity | ||||
| White, non-Hispanic | 1.48 | 1.46 | 1.02 (0.99–1.04) | 0.66 |
| Black, non-Hispanic | 1.17 | 1.18 | 1.00 (0.91–1.09) | 0.63 |
| Asian | 0.95 | 0.99 | 0.95 (0.81–1.12) | 0.66 |
| Hispanic | 0.95 | 1.01 | 0.94 (0.85–1.04) | 0.67 |
| Other, mixed, unknown | 1.45 | 1.41 | 1.03 (0.97–1.09) | 0.65 |
| BI-RADS breast density classification | ||||
| Almost entirely fat (category 1) | 0.78 | 0.75 | 1.04 (0.95–1.14) | 0.67 |
| Scattered fibroglandular densities (category 2) | 1.27 | 1.24 | 1.02 (0.99–1.06) | 0.64 |
| Heterogeneously dense (category 3) | 1.66 | 1.65 | 1.00 (0.97–1.04) | 0.65 |
| Extremely dense (category 4) | 1.80 | 1.81 | 1.00 (0.94–1.06) | 0.64 |
| First-degree relatives with breast cancer | ||||
| 0 | 1.30 | 1.32 | 0.99 (0.96–1.01) | 0.65 |
| 1 | 2.11 | 1.98 | 1.07 (1.01–1.13) | 0.64 |
| ≥2 | 2.52 | 2.44 | 1.04 (0.95–1.13) | 0.62 |
| Breast biopsies | ||||
| 0 | 1.19 | 1.16 | 1.03 (0.99–1.06) | 0.64 |
| ≥1 | 2.35 | 2.37 | 0.99 (0.96–1.03) | 0.62 |
| Decile of predicted risk | ||||
| 1st | 0.40 | 0.39 | 1.04 (0.92–1.18) | 0.64 |
| 2nd | 0.61 | 0.66 | 0.93 (0.84–1.02) | 0.56 |
| 3rd | 0.76 | 0.84 | 0.91 (0.83–0.99) | 0.57 |
| 4th | 0.92 | 0.95 | 0.97 (0.89–1.05) | 0.58 |
| 5th | 1.12 | 1.07 | 1.04 (0.97–1.12) | 0.57 |
| 6th | 1.30 | 1.37 | 0.95 (0.89–1.02) | 0.58 |
| 7th | 1.53 | 1.47 | 1.04 (0.98–1.11) | 0.58 |
| 8th | 1.85 | 1.87 | 0.99 (0.93–1.05) | 0.57 |
| 9th | 2.26 | 2.27 | 0.99 (0.94–1.05) | 0.55 |
| 10th | 3.40 | 3.10 | 1.10 (1.05–1.15) | 0.58 |
| Quintile of Gail risk | ||||
| 1st | 0.75 | 0.76 | 0.99 (0.93–1.05) | 0.62 |
| 2nd | 1.04 | 1.05 | 0.99 (0.94–1.04) | 0.64 |
| 3rd | 1.30 | 1.29 | 1.01 (0.96–1.06) | 0.62 |
| 4th | 1.72 | 1.69 | 1.02 (0.98–1.06) | 0.62 |
| 5th | 2.26 | 2.20 | 1.03 (0.99–1.07) | 0.61 |
| Gail high risk | ||||
| No (<1.67%) | 1.22 | 1.21 | 1.00 (0.98–1.03) | 0.65 |
| Yes (≥1.67%) | 2.37 | 2.29 | 1.03 (0.99–1.07) | 0.61 |
Among the 629 229 women with complete 5-year follow-up. The observed 5-year rate is the actual rate observed in the individual subcohorts. The expected rate is the average of the Breast Cancer Surveillance Consortium breast density model predicted risk for each woman in the subcohort. No additional adjustments were done. BI-RADS = Breast Imaging Reporting and Data System.
Table 5 shows the predicted 5-year risk for women in the study, by age and breast density groups and by subgroups defined by the presence or absence of a first-degree relative with breast cancer and a history of breast biopsy. Women with the lowest mammographic breast density (almost entirely fat) had a 5-year risk greater than 1.66% only if they were at least age 65 years and had both a first-degree relative with breast cancer and a personal history of a breast biopsy. In contrast, women with extremely dense breasts had an observed risk greater than 2% by age 45 years if they had either a family history of breast cancer or a personal history of a breast biopsy and by age 50 years, regardless of whether they had had previous biopsies or a family history of breast cancer.
Table 5.
Five-Year Risk for Invasive Breast Cancer, by Age and Breast Imaging Reporting and Data System Breast Density and by Risk Factor Subgroup*
| BI-RADS Density Category | 5-Year Risk for Breast Cancer† | 5-Year Risk with No Family History† | 5-Year Risk with Family History† | ||
|---|---|---|---|---|---|
| No Breast Biopsy | History of Breast Biopsy | No Breast Biopsy | History of Breast Biopsy | ||
| Age 40–44 y | |||||
| Almost entirely fat | 0.2 | 0.2 | 0.3 | 0.3 | 0.5 |
| Scattered fibroglandular densities | 0.5 | 0.4 | 0.7 | 0.7 | 1.1 |
| Heterogeneously dense | 0.7 | 0.7 | 1.1 | 1.0 | 1.7 |
| Extremely dense | 1.0 | 0.8 | 1.4 | 1.3 | 2.2 |
| Age 45–49 y | |||||
| Almost entirely fat | 0.4 | 0.3 | 0.5 | 0.5 | 0.8 |
| Scattered fibroglandular densities | 0.8 | 0.7 | 1.0 | 1.0 | 1.7 |
| Heterogeneously dense | 1.2 | 1.0 | 1.7 | 1.6 | 2.6 |
| Extremely dense | 1.6 | 1.3 | 2.1 | 2.1 | 3.3 |
| Age 50–54 y | |||||
| Almost entirely fat | 0.5 | 0.4 | 0.7 | 0.7 | 1.1 |
| Scattered fibroglandular densities | 1.0 | 0.9 | 1.4 | 1.4 | 2.2 |
| Heterogeneously dense | 1.6 | 1.3 | 2.2 | 2.1 | 3.4 |
| Extremely dense | 2.1 | 1.7 | 2.8 | 2.7 | 4.4 |
| Age 55–59 y | |||||
| Almost entirely fat | 0.7 | 0.6 | 0.9 | 0.9 | 1.5 |
| Scattered fibroglandular densities | 1.4 | 1.2 | 1.9 | 1.9 | 3.0 |
| Heterogeneously dense | 2.2 | 1.8 | 3.0 | 2.8 | 4.6 |
| Extremely dense | 3.0 | 2.3 | 3.8 | 3.6 | 5.9 |
| Age 60–64 y | |||||
| Almost entirely fat | 0.8 | 0.7 | 1.1 | 1.1 | 1.7 |
| Scattered fibroglandular densities | 1.7 | 1.4 | 2.3 | 2.2 | 3.5 |
| Heterogeneously dense | 2.6 | 2.1 | 3.5 | 3.3 | 5.4 |
| Extremely dense | 3.4 | 2.7 | 4.4 | 4.2 | 6.9 |
| Age 65–69 y | |||||
| Almost entirely fat | 1.3 | 1.1 | 1.8 | 1.8 | 2.9 |
| Scattered fibroglandular densities | 2.0 | 1.7 | 2.8 | 2.6 | 4.3 |
| Heterogeneously dense | 2.9 | 2.3 | 3.8 | 3.6 | 5.9 |
| Extremely dense | 3.0 | 2.4 | 4.0 | 3.8 | 6.2 |
| Age 70–74 y | |||||
| Almost entirely fat | 1.4 | 1.2 | 1.9 | 1.8 | 3.0 |
| Scattered fibroglandular densities | 2.1 | 1.8 | 2.9 | 2.8 | 4.5 |
| Heterogeneously dense | 3.1 | 2.5 | 4.0 | 3.8 | 6.2 |
| Extremely dense | 3.3 | 2.5 | 4.2 | 3.9 | 6.4 |
BI-RADS = Breast Imaging Reporting and Data System.
Mean predicted risk among the 629 229 women with complete 5-year follow-up. A woman was considered to have a family history of breast cancer if invasive breast cancer was diagnosed in ≥1 first-degree relative.
We used reclassification tables to compare the breast density model with other models. We divided women into 4 risk categories: low (<1%), low or intermediate (1% to 1.66%), high or intermediate (1.67% to 2.5%), and high (≥2.5%). Using the method suggested by Cook and colleagues (40, 41), we calculated the proportion of women reclassified correctly (patients with cancer reassigned to a higher-risk category and patients without cancer reassigned to a lower-risk category) and patients reclassified incorrectly. The addition of breast density to age, race or ethnicity, family history, and history of breast biopsy correctly reclassified 22% of women and incorrectly reclassified 16% of women (Table 6). When we used a cut-point greater than 1.66% to define high risk, the true-positive rate increased slightly (from 52% to 53%) and the false-positive rate decreased slightly (from 33% to 30%). The positive predictive value thus increased slightly from 2.2% to 2.4%. Compared with the Gail model, the model we developed correctly reclassified 14% of women but incorrectly reclassified 35% of women (Table 7). Nonetheless, the true-positive rate increased from 28% to 53% and the positive predictive value increased from 2.3% to 2.4%. The false-positive rate also increased from 17% to 30%. Results were similar when we used a cut-point greater than 2% to define high risk (Appendix Tables 1 and 2, available at www.annals.org).
Table 6. Change in Risk Categorization by Using the Breast Cancer Surveillance Consortium Breast Density Model Compared with the Risk Factor Model*.
| 5-Year Risk in Risk Factor Model | 5-Year Risk in BCSC Breast Density Model | Row Totals | Events (95% CI), n (%) | Accuracy of Model without Breast Density for Women with Risk ≥1.67% | Accuracy of Model with Breast Density for Women with Risk ≥1.67% | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to <1% | 1% to 1.66% | 1.67% to 2.49% | ≥2.5% | Correctly Reclassified† | Incorrectly Reclassified‡ | ||||
| Total, n | 249 959 | 186 106 | 124 420 | 68 744 | 629 229 | 137 404 (22) | 99 777 (16) | ||
| Events | 1761 | 2390 | 2513 | 2120 | 8784 | – | – | ||
| Nonevents | 248 198 | 183 716 | 121 907 | 66 624 | 620 445 | ||||
| 0 to <1%, n | 176 831 | 38 500 | 71 | 0 | 215 402 | 415 (0.2) | 38 156 (18) | ||
| Events | 1161 | 415 | 0 | 0 | 1576 | – | – | ||
| Nonevents | 175 670 | 38 085 | 71 | 0 | 213 826 | ||||
| 1% to 1.66%, n | 64 297 | 99 456 | 37 149 | 1025 | 201 927 | 64 557 (32) | 37 914 (19) | ||
| Events | 526 | 1328 | 754 | 32 | 2640 | – | – | ||
| Nonevents | 63 771 | 98 128 | 36 395 | 993 | 199 287 | ||||
| 1.67% to 2.49%, n | 8741 | 45 478 | 71 309 | 23 267 | 148 795 | 54 157 (36) | 23 329 (16) | True positive: 4568 (52%) | True positive: 4633 (53%) |
| Events | 74 | 609 | 1419 | 621 | 2723 | ||||
| Nonevents | 8667 | 44 869 | 69 890 | 22 646 | 146 072 | False positive: 207 332 (33%) | False positive: 188 531 (30%) | ||
| ≥2.5%, n | 90 | 2672 | 15 891 | 44 452 | 63 105 | 18 275 (29) | 378 (0.6) | ||
| Events | 0 | 38 | 340 | 1467 | 1845 | PPV: 2.16% | PPV: 2.40% | ||
| Nonevents | 90 | 2634 | 15 551 | 42 985 | 61 260 | ||||
The risk factor model uses the same algorithm as the breast density model, but breast density was removed from the calculations. BCSC = Breast Cancer Surveillance Consortium; PPV = positive predictive value.
Events were reassigned to higher-risk categories and nonevents were reassigned to lower-risk categories.
Events were reassigned to lower-risk categories and nonevents were reassigned to higher-risk categories.
Table 7. Change in Risk Categorization by Using the Breast Cancer Surveillance Consortium Breast Density Model Compared with the Gail Model*.
| 5-Year Risk in Gail Model | 5-Year Risk in BCSC Breast Density Model | Row Totals | Events (95% CI), n (%) | Accuracy of Gail Model for Women with Risk ≥1.67% | Accuracy of for Women with Risk ≥1.67% | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to <1% | 1% to 1.66% | 1.67% to 2.49% | ≥2.5% | Correctly Reclassified† | Incorrectly Reclassified‡ | ||||
| Total, n | 249 959 | 186 106 | 124 420 | 68 744 | 629 229 | 85 262 (14) | 222 672 (35) | – | – |
| Events | 1761 | 2390 | 2513 | 2120 | 8784 | ||||
| Nonevents | 248 198 | 183 716 | 121 907 | 66 624 | 620 445 | ||||
| 0 to <1%, n | 201 037 | 94 843 | 27 582 | 4019 | 327 481 | 1879 (0.6) | 124 565 (38) | – | – |
| Events | 1350 | 1192 | 582 | 105 | 3229 | ||||
| Nonevents | 199 687 | 93 651 | 27 000 | 3914 | 324 252 | ||||
| 1% to 1.66%, n | 42 444 | 69 051 | 59 604 | 24 355 | 195 454 | 44 000 (23) | 82 403 (42) | – | – |
| Events | 341 | 875 | 1188 | 709 | 3113 | ||||
| Nonevents | 42 103 | 68 176 | 58 416 | 23 646 | 192 341 | ||||
| 1.67% to 2.49%, n | 4833 | 17 117 | 26 355 | 15 518 | 63 823 | 22 083 (35) | 15 385 (24) | True positive: 2442 (28%) | True positive: 4633 (53%) |
| Events | 51 | 253 | 513 | 437 | 1254 | ||||
| Nonevents | 4782 | 16 864 | 25 842 | 15 081 | 62 569 | False positive: 103 852 (17%) | False positive: 188 531 (30%) | ||
| ≥2.5%, n | 1645 | 5095 | 10 879 | 24 852 | 42 471 | 17 300 (41) | 319 (0.8) | ||
| Events | 19 | 70 | 230 | 869 | 1188 | PPV: 2.30% | PPV: 2.40% | ||
| Nonevents | 1626 | 5025 | 10 649 | 23 983 | 41 283 | ||||
BCSC = Breast Cancer Surveillance Consortium; PPV = positive predictive value.
Events were reassigned to higher-risk categories and nonevents were reassigned to lower-risk categories.
Events were reassigned to lower-risk categories and nonevents were reassigned to higher-risk categories.
Discussion
We developed a risk prediction model to assess 5-year risk for invasive breast cancer that is based on breast density and demonstrate that the model has some features that might make it useful for risk prediction. The model is well calibrated in major race and ethnic groups in the United States. In addition, it has modest ability to discriminate between women who will develop breast cancer and those who will not.
Two other risk assessment models have incorporated mammographic breast density (26, 27). The first, a refinement of the Gail model by Chen and colleagues (26), used a continuous measure of breast density in addition to age, age at first live birth, number of first-degree relatives with breast cancer, body weight, number of breast biopsies, and presence of atypical hyperplasia on biopsy to estimate a woman's future risk for breast cancer. This improves risk discrimination compared with the Gail model, but calibration of the model in different demographic and risk factor subgroups has not yet been published. In addition, the model is based on a continuous measure of breast density that is not routinely available in clinical practice because it requires digital scanning of the mammogram and specialized software to estimate the percentage of the total breast area on the mammogram that is dense, a relatively expensive and labor-intensive process. Thus, it cannot be readily implemented among women receiving mammography today. Barlow and colleagues (27) also developed a model in a different subset of the BCSC that used BI-RADS as its measure of breast density. However, their model focused on 1-year risk for breast cancer and was validated on the basis of cases of breast cancer diagnosed by the index mammogram. This method may overestimate a woman's long-term risk for breast cancer by including incident cancers detected by the first mammogram.
Our model has advantages over these other models. It uses simple, easily obtained variables and is based on many races and ethnicities. Despite these advantages and its excellent calibration, however, its discriminatory accuracy was modest (c-statistic, 0.660). The age-adjusted c-statistic, a better measure for comparing models across different study populations because it removes the age distribution of the sample from the measure (the strongest risk factor for breast cancer), was even lower (0.622). We believe that these modest measures of discrimination must be interpreted with the understanding that extremely high relative risks (>100) are required for risk factor models to have high c-statistics (42–44) and that other risk models with modest discriminatory accuracy, such as the Framingham model (c-statistic, 0.63 to 0.83) (45), are commonly used to guide clinical decisions. Thus, in our view, the range of c-statistics we report does not exclude the model as a potential risk prediction tool.
The Gail model without breast density (7) remains the standard risk assessment tool for clinicians. In a previous study (28), we demonstrated that a model based on BI-RADS density alone had predictive accuracy similar to one based on the Gail model variables. Adding breast density to the Gail model was statistically significant (P < 0.001), although the small increase in the c-statistic was unlikely to be clinically important (28). In that analysis, we directly compared a simple proportional hazards model by using Gail model variables with the same model plus breast density. The model that we report here differs from our previous model in several ways, including the use of SEER data to estimate breast cancer incidence based on age and race or ethnicity and the use of different coefficients for BI-RADS density for younger (age <65 years) and older women (age ≥65 years). It also more carefully accounts for differences in the age- and race- or ethnicity-specific distribution in breast density.
Compared with the Gail model, the breast density model reclassified a larger percentage of women incorrectly than correctly. However, it reclassified a higher proportion of women who developed breast cancer into higher-risk categories, and the positive predictive value and c-statistic of the breast density model were higher than that of the Gail model. This paradoxical finding can occur when 1 of the models is not well calibrated in a population. The Gail model has recently been shown to underestimate the risk for invasive breast cancer in black women by a factor of 1.5 to 3.2 (46). The racial diversity of our cohort and missing data for some Gail model risk factors produced an inappropriately low risk estimate for some women when using the Gail model (expected–observed ratio, 0.88 for Gail model). When the same women were reclassified by using the breast density model, their risk was appropriately increased so that the overall model would be well calibrated, even though this meant that some women in whom breast cancer was not diagnosed had their risk estimate increased. Further comparisons of the 2 models in additional populations will help to clarify their relative value.
The BI-RADS measure of breast density has modest reproducibility. In an earlier study (47), we found that without specific training of the radiologists, intraobserver variability for the measure was fair (κ = 0.72; 83% agreement) and interobserver variability was modest (κ = 0.59; 75% agreement). Therefore, a woman's estimated risk for breast cancer might differ somewhat from radiologist to radiologist and from one examination to the next. One study has reported that 2 longitudinal measures of BI-RADS breast density may better predict a woman's risk for breast cancer than a single measure (48).
Alternatively, a more precise and reproducible measure than BI-RADS breast density that did not depend on the subjective impression of radiologists may improve the utility of breast density for risk prediction. Breast density can be measured as a continuous risk factor, and recent studies have preferred to use the percentage of mammographic density (area of density divided by total breast area) as the unit of measure (10, 13, 49). The extremes of BI-RADS breast density, which capture most of risk for breast cancer attributed to breast density, correlate well with quantitative measures (50, 51). This implies that a categorical measurement may be sufficient for risk assessment. However, new automated approaches being pilot tested include a phantom calibrator in the mammographic image that should more precisely and accurately characterize breast tissue composition (52, 53). However, none of these quantitative approaches are available for clinical use. As better measurements of breast density become available, our model can be updated by using the more precise measurement.
No single model can address all needs in breast cancer risk assessment. For example, our breast density model does not adequately capture risk in women with a very strong family history of breast cancer and other diseases associated with hereditary breast cancer syndromes, such as ovarian cancer, prostate cancer, sarcomas, and thyroid disease. These patients should be identified and referred to genetic counselors for detailed pedigree analysis and for genetic testing when appropriate. None of the general risk assessment tools, including those developed to capture detailed family history (54 –56), adequately quantifies the nuances of these patients' family and personal history. For the general population, the most cost-effective and efficient approach may be stepwise, starting with a simple model and family history. Women above a certain risk level may then be referred for more detailed risk assessment by using a comprehensive model, such as that of Tyrer and colleagues (56). In women at average or low risk for breast cancer, risk assessment should be repeated periodically to capture changes in risk over time. In either scenario, risk estimates apply to populations, not individuals, and those estimates should always be combined with the potential benefits and harms of tests and treatments (along with a woman's preference for those tests and treatments) to make the best clinical decisions for individual patients.
In summary, we developed a risk prediction model that incorporates breast density to estimate a woman's 5-year risk for invasive breast cancer. It is well calibrated in the major race and ethnicity groups in the United States and across the age range of women who would be considered candidates for chemoprophylaxis for breast cancer. It is convenient enough that it could be incorporated into routine breast cancer screening, and primary care physicians could use it to calculate an individual woman's breast cancer risk. However, its accuracy must be further evaluated in independent populations before it can be recommended for clinical use.
Acknowledgments
The authors thank the BCSC investigators, participating mammography facilities, and radiologists for the data they provided for the study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes are available at http://breastscreening.cancer.gov/.
Grant Support: By the National Cancer Institute–funded Breast Cancer Surveillance Consortium cooperative agreement (grants U01CA63740, U01CA86076, U01CA86082, U01CA63736, U01CA70013, U01CA69976, U01CA63731, and U01CA70040) and a Building Interdisciplinary Research Careers in Women's Health faculty development grant (K12 AR47659).
Appendix Figure. The Breast Cancer Surveillance Consortium breast density model algorithm.
BI-RADS = Breast Imaging Reporting and Data System; SEER = Surveillance, Epidemiology, and End Results.
Appendix Table 1. Change in Risk Categorization by Using the Breast Cancer Surveillance Consortium Breast Density Model Compared with the Risk Factor Model*.
| 5-Year Risk in Risk Factor Model | 5-Year Risk in BCSC Breast Density Model | Row Totals | Events (95% CI), n (%) | Accuracy of Model without Breast Density for Women with Risk ≥2% | Accuracy of Model with Breast Density for Women with Risk ≥2% | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to <1% | 1% to 2% | 2% to 2.99% | ≥3% | Correctly Reclassified† | Incorrectly Reclassified‡ | ||||
| Total, n | 249 959 | 253 656 | 90 201 | 35 413 | 629 229 | 118 943 (19) | 95 401 (15) | – | – |
| Events | 1761 | 3649 | 2129 | 1245 | 8784 | ||||
| Nonevents | 248 198 | 250 007 | 88 072 | 34 168 | 620 445 | ||||
| 0 to <1%, n | 176 831 | 38 571 | 0 | 0 | 215 402 | 415 (0.2) | 38 156 (18) | – | – |
| Events | 1161 | 415 | 0 | 0 | 1576 | ||||
| Nonevents | 175 670 | 38 156 | 0 | 0 | 213 826 | ||||
| 1% to 2%, n | 71 012 | 184 299 | 43 767 | 476 | 299 554 | 71 446 (24) | 43 809 (15) | – | – |
| Events | 585 | 2749 | 1002 | 17 | 4353 | ||||
| Nonevents | 70 427 | 181 550 | 42 765 | 459 | 295 201 | ||||
| 2% to 2.99%, n | 2116 | 26 990 | 31 805 | 12 987 | 73 898 | 29 109 (39) | 12 984 (18) | True positive: 2855 (32%) | True positive: 3374 (38%) |
| Events | 15 | 422 | 738 | 440 | 1615 | ||||
| Nonevents | 2101 | 26 568 | 31 067 | 12 547 | 72 283 | False positive: 111 418 (18%) | False positive: 122 240 (20%) | ||
| ≥3%, n | 0 | 3796 | 14 629 | 21 950 | 40 375 | 17 973 (44) | 452 (1.1) | PPV: 2.50% | PPV: 2.69% |
| Events | 0 | 63 | 389 | 788 | 1240 | ||||
| Nonevents | 0 | 3733 | 14 240 | 21 162 | 39 135 | ||||
The risk factor model uses the same algorithm as the breast density model, but breast density was removed from the calculations. BCSC = Breast Cancer Surveillance Consortium; PPV = positive predictive value.
Events were reassigned to higher-risk categories and nonevents were reassigned to lower-risk categories.
Events were reassigned to lower-risk categories and nonevents were reassigned to higher-risk categories.
Appendix Table 2. Change in Risk Categorization by Using the Breast Cancer Surveillance Consortium Breast Density Model Compared with the Gail Model*.
| 5-Year Risk in | 5-Year Risk in BCSC Breast Density Model | Row Totals | Events (95% CI), n (%) | Accuracy of Gail Model for Women with Risk ≥2% | Accuracy of for Women with Risk ≥2% | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0 to <1% | 1% to 2% | 2% to 2.99% | ≥3% | Correctly Reclassified† | Incorrectly Reclassified‡ | ||||
| Total, n | 249 959 | 253 656 | 90 201 | 35 413 | 629 229 | 81 786 (13) | 197 741 (31) | – | – |
| Events | 1761 | 3649 | 2129 | 1245 | 8784 | ||||
| Nonevents | 248 198 | 250 007 | 88 072 | 34 168 | 620 445 | ||||
| 0 to <1%, n | 201 037 | 111 008 | 14 552 | 884 | 327 481 | 1879 (0.6) | 124 565 (38) | – | – |
| Events | 1350 | 1552 | 306 | 21 | 3229 | ||||
| Nonevents | 199 687 | 109 456 | 14 246 | 863 | 324 252 | ||||
| 1% to 2%, n | 45 598 | 121 807 | 51 984 | 12 912 | 232 301 | 46 865 (20) | 63 629 (27) | – | – |
| Events | 379 | 1760 | 1223 | 423 | 3785 | ||||
| Nonevents | 45 219 | 120 047 | 50 761 | 12 489 | 228 516 | ||||
| 2% to 2.99%, n | 2361 | 14 506 | 14 497 | 9256 | 40 620 | 16 943 (42) | 9180 (23) | True positive: 1770 (20%) | True positive: 3374 (38%) |
| Events | 19 | 230 | 353 | 325 | 927 | ||||
| Nonevents | 2342 | 14 276 | 14 144 | 8931 | 39 693 | False positive: 67 677 (11%) | False positive: 122 240 (20%) | ||
| ≥3%, n | 963 | 6335 | 9168 | 12 361 | 28 827 | 16 099 (56) | 367 (1.3) | ||
| Events | 13 | 107 | 247 | 476 | 843 | PPV: 2.55% | PPV: 2.69% | ||
| Nonevents | 950 | 6228 | 8921 | 11 885 | 27 984 | ||||
BCSC = Breast Cancer Surveillance Consortium; PPV = positive predictive value.
Events were reassigned to higher-risk categories and nonevents were reassigned to lower-risk categories.
Events were reassigned to lower-risk categories and nonevents were reassigned to higher-risk categories
Footnotes
Potential Financial Conflicts of Interest: Consultancies: S.R. Cummings (Eli Lilly). Honoraria: S.R. Cummings (Eli Lilly). Grants received: J.A. Tice (Building Interdisciplinary Careers in Women's Health [career development award]), S.R. Cummings (Eli Lilly, Lilly Foundation). Grants pending: S.R. Cummings (Eli Lilly, Lilly Foundation).
Reproducible Research Statement: The data set is available through the BCSC Web site (available at http://breastscreening.cancer.gov/).
Author Contributions: Conception and design: J.A. Tice, S.R. Cummings, W.E. Barlow, K. Kerlikowske.
Analysis and interpretation of the data: J.A. Tice, S.R. Cummings, W.E. Barlow, K. Kerlikowske.
Drafting of the article: J.A. Tice, K. Kerlikowske.
Critical revision of the article for important intellectual content: J.A. Tice, S.R. Cummings, L. Ichikawa, K. Kerlikowske.
Final approval of the article: J.A. Tice, S.R. Cummings, L. Ichikawa, W.E. Barlow, K. Kerlikowske.
Provision of study materials or patients: K. Kerlikowske.
Statistical expertise: J.A. Tice, W.E. Barlow.
Obtaining of funding: J.A. Tice, W.E. Barlow, K. Kerlikowske.
Administrative, technical, or logistic support: S.R. Cummings, K. Kerlikowske.
Collection and assembly of data: L. Ichikawa, W.E. Barlow, K. Kerlikowske.
References
- 1.American Cancer Society. Cancer Facts & Figure 2007. Atlanta: American Cancer Soc; 2007. [Google Scholar]
- 2.Freedman AN, Graubard BI, Rao SR, McCaskill-Stevens W, Ballard-Barbash R, Gail MH. Estimates of the number of US women who could benefit from tamoxifen for breast cancer chemoprevention. J Natl Cancer Inst. 2003;95:526–32. doi: 10.1093/jnci/95.7.526. [DOI] [PubMed] [Google Scholar]
- 3.Tchou J, Hou N, Rademaker A, Jordan VC, Morrow M. Acceptance of tamoxifen chemoprevention by physicians and women at risk. Cancer. 2004;100:1800–6. doi: 10.1002/cncr.20205. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong K, Quistberg DA, Micco E, Domchek S, Guerra C. Prescription of tamoxifen for breast cancer prevention by primary care physicians. Arch Intern Med. 2006;166:2260–5. doi: 10.1001/archinte.166.20.2260. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan CP, Haas JS, Pérez-Stable EJ, Gregorich SE, Somkin C, Des Jarlais G, et al. Breast cancer risk reduction options: awareness, discussion, and use among women from four ethnic groups. Cancer Epidemiol Biomarkers Prev. 2006;15:162–6. doi: 10.1158/1055-9965.EPI-04-0758. [DOI] [PubMed] [Google Scholar]
- 6.Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75–89. doi: 10.3322/canjclin.57.2.75. [DOI] [PubMed] [Google Scholar]
- 7.Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- 8.Rockhill B, Spiegelman D, Byrne C, Hunter DJ, Colditz GA. Validation of the Gail et al. model of breast cancer risk prediction and implications for chemoprevention. J Natl Cancer Inst. 2001;93:358–66. doi: 10.1093/jnci/93.5.358. [DOI] [PubMed] [Google Scholar]
- 9.Freedman AN, Seminara D, Gail MH, Hartge P, Colditz GA, Ballard-Barbash R, et al. Cancer risk prediction models: a workshop on development, evaluation, and application. J Natl Cancer Inst. 2005;97:715–23. doi: 10.1093/jnci/dji128. [DOI] [PubMed] [Google Scholar]
- 10.Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ. Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 1998;7:1133–44. [PubMed] [Google Scholar]
- 11.Oza AM, Boyd NF. Mammographic parenchymal patterns: a marker of breast cancer risk. Epidemiol Rev. 1993;15:196–208. doi: 10.1093/oxfordjournals.epirev.a036105. [DOI] [PubMed] [Google Scholar]
- 12.Warner E, Lockwood G, Tritchler D, Boyd NF. The risk of breast cancer associated with mammographic parenchymal patterns: a meta-analysis of the published literature to examine the effect of method of classification. Cancer Detect Prev. 1992;16:67–72. [PubMed] [Google Scholar]
- 13.Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, et al. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995;87:670–5. doi: 10.1093/jnci/87.9.670. [DOI] [PubMed] [Google Scholar]
- 14.Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, et al. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995;87:1622–9. doi: 10.1093/jnci/87.21.1622. [DOI] [PubMed] [Google Scholar]
- 15.Saftlas AF, Wolfe JN, Hoover RN, Brinton LA, Schairer C, Salane M, et al. Mammographic parenchymal patterns as indicators of breast cancer risk. Am J Epidemiol. 1989;129:518–26. doi: 10.1093/oxfordjournals.aje.a115163. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe JN, Saftlas AF, Salane M. Mammographic parenchymal patterns and quantitative evaluation of mammographic densities: a case-control study. AJR Am J Roentgenol. 1987;148:1087–92. doi: 10.2214/ajr.148.6.1087. [DOI] [PubMed] [Google Scholar]
- 17.Kerlikowske K, Grady D, Barclay J, Sickles EA, Ernster V. Effect of age, breast density, and family history on the sensitivity of first screening mammography. JAMA. 1996;276:33–8. [PubMed] [Google Scholar]
- 18.van Gils CH, Otten JD, Verbeek AL, Hendriks JH. Mammographic breast density and risk of breast cancer: masking bias or causality? Eur J Epidemiol. 1998;14:315–20. doi: 10.1023/a:1007423824675. [DOI] [PubMed] [Google Scholar]
- 19.van Gils CH, Otten JD, Verbeek AL, Hendriks JH, Holland R. Effect of mammographic breast density on breast cancer screening performance: a study in Nijmegen, The Netherlands. J Epidemiol Community Health. 1998;52:267–71. doi: 10.1136/jech.52.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–36. doi: 10.1056/NEJMoa062790. [DOI] [PubMed] [Google Scholar]
- 21.Vachon CM, Brandt KR, Ghosh K, Scott CG, Maloney SD, Carston MJ, et al. Mammographic breast density as a general marker of breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2007;16:43–9. doi: 10.1158/1055-9965.EPI-06-0738. [DOI] [PubMed] [Google Scholar]
- 22.Boyd NF, Stone J, Martin LJ, Jong R, Fishell E, Yaffe M, et al. The association of breast mitogens with mammographic densities. Br J Cancer. 2002;87:876–82. doi: 10.1038/sj.bjc.6600537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo YP, Martin LJ, Hanna W, Banerjee D, Miller N, Fishell E, et al. Growth factors and stromal matrix proteins associated with mammographic densities. Cancer Epidemiol Biomarkers Prev. 2001;10:243–8. [PubMed] [Google Scholar]
- 24.Hawes D, Downey S, Pearce CL, Bartow S, Wan P, Pike MC, et al. Dense breast stromal tissue shows greatly increased concentration of breast epithelium but no increase in its proliferative activity. Breast Cancer Res. 2006;8:R24. doi: 10.1186/bcr1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li T, Sun L, Miller N, Nicklee T, Woo J, Hulse-Smith L, et al. The association of measured breast tissue characteristics with mammographic density and other risk factors for breast cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:343–9. doi: 10.1158/1055-9965.EPI-04-0490. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Pee D, Ayyagari R, Graubard B, Schairer C, Byrne C, et al. Projecting absolute invasive breast cancer risk in white women with a model that includes mammographic density. J Natl Cancer Inst. 2006;98:1215–26. doi: 10.1093/jnci/djj332. [DOI] [PubMed] [Google Scholar]
- 27.Barlow WE, White E, Ballard-Barbash R, Vacek PM, Titus-Ernstoff L, Carney PA, et al. Prospective breast cancer risk prediction model for women undergoing screening mammography. J Natl Cancer Inst. 2006;98:1204–14. doi: 10.1093/jnci/djj331. [DOI] [PubMed] [Google Scholar]
- 28.Tice JA, Cummings SR, Ziv E, Kerlikowske K. Mammographic breast density and the Gail model for breast cancer risk prediction in a screening population. Breast Cancer Res Treat. 2005;94:115–22. doi: 10.1007/s10549-005-5152-4. [DOI] [PubMed] [Google Scholar]
- 29.Ballard-Barbash R, Taplin SH, Yankaskas BC, Ernster VL, Rosenberg RD, Carney PA, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR Am J Roentgenol. 1997;169:1001–8. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 30.Sickles EA, Miglioretti DL, Ballard-Barbash R, Geller BM, Leung JW, Rosenberg RD, et al. Performance benchmarks for diagnostic mammography. Radiology. 2005;235:775–90. doi: 10.1148/radiol.2353040738. [DOI] [PubMed] [Google Scholar]
- 31.Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91:1541–8. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- 32.D'Orsi CJ, Bassett LW, Berg WA, et al. Breast Imaging Reporting and Data System—Mammography. 4th. Reston: American Coll of Radiology; 2003. [Google Scholar]
- 33.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database. Incidence-SEER 9 Regs Public-Use, Nov 2004 Sub (1973–2002) National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch; [9 December 2005]. released April 2005, based on the November 2004 submission. Accessed at www.seer.cancer.gov on. [Google Scholar]
- 34.Kochanek KD, Murphy SL, Anderson RN, Scott C. Deaths: final data for 2002. Natl Vital Stat Rep. 2004;53:1–115. [PubMed] [Google Scholar]
- 35.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 36.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 37.Rockhill B, Byrne C, Rosner B, Louie MM, Colditz G. Breast cancer risk prediction with a log-incidence model: evaluation of accuracy. J Clin Epidemiol. 2003;56:856–61. doi: 10.1016/s0895-4356(03)00124-0. [DOI] [PubMed] [Google Scholar]
- 38.Stone M. Cross-validatory choice and assessment of statistical predictions. J Roy Stat Soc B. 1974;26:111–47. [Google Scholar]
- 39.Stone M. An asymptotic equivalence of choice of model by cross-validation and Akaike's criterion. J Roy Stat Soc B. 1977;39:44–7. [Google Scholar]
- 40.Cook NR, Buring JE, Ridker PM. The effect of including C-reactive protein in cardiovascular risk prediction models for women. Ann Intern Med. 2006;145:21–9. doi: 10.7326/0003-4819-145-1-200607040-00128. [DOI] [PubMed] [Google Scholar]
- 41.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–35. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 42.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004;159:882–90. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 43.Wald NJ, Hackshaw AK, Frost CD. When can a risk factor be used as a worthwhile screening test? BMJ. 1999;319:1562–5. doi: 10.1136/bmj.319.7224.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ware JH. The limitations of risk factors as prognostic tools. N Engl J Med. 2006;355:2615–7. doi: 10.1056/NEJMp068249. [DOI] [PubMed] [Google Scholar]
- 45.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 46.Gail MH, Costantino JP, Pee D, Bondy M, Newman L, Selvan M, et al. Projecting individualized absolute invasive breast cancer risk in African American Women. J Natl Cancer Inst. 2007;99:1782–1792. doi: 10.1093/jnci/djm223. [DOI] [PubMed] [Google Scholar]
- 47.Kerlikowske K, Grady D, Barclay J, Frankel SD, Ominsky SH, Sickles EA, et al. Variability and accuracy in mammographic interpretation using the American College of Radiology Breast Imaging Reporting and Data System. J Natl Cancer Inst. 1998;90:1801–9. doi: 10.1093/jnci/90.23.1801. [DOI] [PubMed] [Google Scholar]
- 48.Kerlikowske K, Ichikawa L, Miglioretti DL, Buist DS, Vacek PM, Smith-Bindman R, et al. National Institutes of Health Breast Cancer Surveillance Consortium. Longitudinal measurement of clinical mammographic breast density to improve estimation of breast cancer risk. J Natl Cancer Inst. 2007;99:386–95. doi: 10.1093/jnci/djk066. [DOI] [PubMed] [Google Scholar]
- 49.Ursin G, Ma H, Wu AH, Bernstein L, Salane M, Parisky YR, et al. Mammographic density and breast cancer in three ethnic groups. Cancer Epidemiol Biomarkers Prev. 2003;12:332–8. [PubMed] [Google Scholar]
- 50.Martin KE, Helvie MA, Zhou C, Roubidoux MA, Bailey JE, Paramagul C, et al. Mammographic density measured with quantitative computer-aided method: comparison with radiologists' estimates and BI-RADS categories. Radiology. 2006;240:656–65. doi: 10.1148/radiol.2402041947. [DOI] [PubMed] [Google Scholar]
- 51.Nicholson BT, LoRusso AP, Smolkin M, Bovbjerg VE, Petroni GR, Harvey JA. Accuracy of assigned BI-RADS breast density category definitions. Acad Radiol. 2006;13:1143–9. doi: 10.1016/j.acra.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 52.Shepherd JA, Herve L, Landau J, Fan B, Kerlikowske K, Cummings SR. Novel use of single X-ray absorptiometry for measuring breast density. Technol Cancer Res Treat. 2005;4:173–82. doi: 10.1177/153303460500400206. [DOI] [PubMed] [Google Scholar]
- 53.Shepherd JA, Herve L, Landau J, Fan B, Kerlikowske K, Cummings SR. Clinical comparison of a novel breast DXA technique to mammographic density. Med Phys. 2006;33:1490–8. doi: 10.1118/1.2193691. [DOI] [PubMed] [Google Scholar]
- 54.Claus EB, Risch N, Thompson WD. The calculation of breast cancer risk for women with a first degree family history of ovarian cancer. Breast Cancer Res Treat. 1993;28:115–20. doi: 10.1007/BF00666424. [DOI] [PubMed] [Google Scholar]
- 55.Parmigiani G, Berry D, Aguilar O. Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet. 1998;62:145–58. doi: 10.1086/301670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111–30. doi: 10.1002/sim.1668. [DOI] [PubMed] [Google Scholar]