Abstract
Purpose
This study describes the adversities experienced by a sample of children of opiate-addicted parents, examines criteria for young adulthood functional resilience, and tests parent, child, and school predictors of resilience.
Methods
The Focus on Families (FOF) project was a randomized trial of a family-focused intervention with opiate addicts in methadone treatment and their children. Analyses were conducted on data from the children in treatment and control families during the original study (1991–1995) and a long-term follow-up interview (2005–2006).
Results
While all participants had an opiate-addicted parent, 70% experienced 2 or more and 20% experienced 4 or more additional types of childhood adversity. Twenty-four percent met the following three criteria for functional resilience at the time of their young-adult interview: (1) working or being enrolled in school, (2) no history of substance abuse or dependence, and (3) no adult criminal charges in the prior 5 years. The FOF intervention did not significantly predict functional resilience. Girls were approximately four times more likely to exhibit resilience than boys. Experiencing a wider range of adversities in addition to having an opiate-addicted parent did not reduce the likelihood of functional resilience. Of the 5 child, family, and school predictors tested after, only externalizing or internalizing problems in childhood were significantly associated with the likelihood of functional resilience (OR = .30, p = .04) as a young adult.
Conclusions
These findings suggest that early intervention with families with addicted parents to prevent and reduce internalizing and externalizing problems in their children holds the most promise of supporting resilient adaptation in early adulthood.
Keywords: Resilience, children of drug abusers, addiction
Introduction
Almost 2 decades ago Johnson and colleagues [1] identified a relatively healthy subgroup of children born to opiate-addicted mothers in methadone treatment. They found that positive maternal attention was linked to better early developmental outcomes. Since then, resilience, or positive development in the face of adversity, has received growing scholarly attention (for review see Luthar, 2006 [2]). The current study uses data from the Focus on Families (FOF) study [3–5] to describe the level and variability of early adversity in a sample of young-adult children of opiate-addicted parents, examines criteria for functional resilience based on behavioral outcomes in young adulthood, and tests parent, child, and school predictors of functional resilience.
Exposure to Adversity
Having an opiate-addicted parent has been linked to a wide range of negative outcomes (for review see Hogan, 1998 [6]), including learning disabilities, attention deficits, and increased risk for problem behaviors, including drug abuse and delinquency [7]. Difficult life circumstances, such as poverty, parental trouble with the law, frequent moves, illness, drug and alcohol use by household members, and abusive intimate relationships make parenting more difficult [8]. These circumstances produce families characterized by disorganization, poor family management skills, low cohesion, and high stress, [9]. A series of studies have found that the number of adverse conditions in childhood is linked to negative outcomes in adulthood [10]. These studies have employed a retrospective measure of adverse childhood experiences including emotional, physical, and sexual abuse; familial drug abuse and mental illness; domestic violence in the home; parental incarceration; and early separation from the parent due to death or divorce. While children of heroin-addicted parents are exposed to familial drug abuse, there is still substantial variability in their exposure to other childhood adversities [11]. Within this high-risk population, more childhood adversity may reduce positive functioning in early adulthood.
Achieving Positive Adaptation
Resilience has been conceptualized as positive adaptation in the face of significant threats to development [12]. Resilience may refer to the achievement of adaptation or some individual characteristics which lead to positive adaptation [12]. Masten [13] was careful to discourage the use of the word ‘resiliency’ because it suggested some quality of the person rather than the achievement of positive outcomes. Some studies focus on resilience in a particular area such as substance abuse [14], while others look at successful outcomes across several domains [12]. Werner and colleagues used a multi-domain approach in their work on resilience among children raised in poverty [15], and specifically, children of alcoholics [16]. We have adopted a similar approach focusing on functional resilience [17]. We define resilience in young adulthood as successfully functioning across these 3 broad domains (avoiding drug abuse, obeying the law, and school/work involvement) which lay the foundation for a positive adult life [18]. This definition cuts across several levels since failure in any domain could threaten physical, psychological, or social survival [13, 17]. We define resilience as attaining normative adaptation under circumstances where it might not be expected [19].
Predictors of Resilience Among Children of Substance Abusers
Resilience among children of substance-abusing parents has been associated with predictors across domains of individual characteristics, family, school, and neighborhood [20]. We explore 3 of these domains. Individual disposition has been linked to positive outcomes among adult children of alcoholics (ACOA) [16]. Children with more positive behavioral dispositions and more skillful problem solving may garner more external resources than those with aggressive or depressive profiles. The quality of the parent-child relationship (attachment or bonding) has also been linked to resilience among ACOA [21]. Likewise, parenting behavior (sometimes referred to as family management) [22, 23] has been associated with better outcomes among children of substance abusers [24]. Families in which normal rules, parental awareness of the child’s whereabouts, and appropriate responses to misbehavior, provide a buffer against the effects of having substance-dependent parents. Academic success and positive teachers may promote resilience among children at risk [25]. School engagement (positive attitudes about teachers, academics, and other school activities) is indicative of a student who is taking advantage of the school environment and thereby accrues its protective benefits.
We examine indicators of functional resilience in young adulthood and examine possible effects of the intervention, the extent of adversity, and other individual, family, and school variables on functional resilience. We add to prior research on children of substance-abusing parents by developing a measure of adversity and testing whether variability in adversity reduces functional resilience in this high-risk group. We then control for level of adversity while testing for the impact of potential protective factors.
Methods
Participants
One hundred thirty families (which included 144 parents and 177 children) were recruited from 2 Seattle-area methadone clinics between 1991 and 1993. Parents had to be in methadone treatment for a minimum of 90 days and have one or more children between the ages of 3 and 15 years residing with them at least 50% of the time. Seventy-five percent of eligible parents consented. Families were randomly assigned to the experimental or control condition after blocking on parents’ race, parents’ age at first drug use, whether parents lived with a spouse or partner, and ages of children. The original study included parent and child interviews at baseline, and 6, 12, and 24 months following the intervention.
In 2005, 98% of the original sample of parents and young-adult children were located. One hundred and fifty-one (85.3%) of the 177 children completed an interview between March 2005 and May 2006 [26]. The in-person interview took approximately 90 minutes and participants were paid $60. We include only those participants who were 18 years or older at the time of their interview (n = 125). Average age at baseline was 9.23 years (s.d. = 3.35). Average age at follow-up was 23.15 years (s.d. = 3.18), with a maximum age of 29 years. Fifty percent were male. Fifty-nine percent were white, based on self-report. Those who completed the interview (n = 125) did not differ from noncompleters (n = 22) in terms of race, gender, age, experimental condition, or cigarette, alcohol, or marijuana use at baseline.
Measures
Age, education, marital status, and number of children, are based on items in the young-adult interview and are provided to give a general description of the sample (see Table 1).
Table 1.
Descriptive information on 125 young-adult children of opiate-addicted parents
| Descriptor | Category | Male (n = 63)% | Female n = 62)% | Total (n = 125)% |
|---|---|---|---|---|
| Race | Caucasian | 59 | 48 | 54 |
| African American | 16 | 21 | 18 | |
| Pacific Islander | 0 | 2 | 1 | |
| mixed | 25 | 29 | 27 | |
| Education | < high school graduate | 37 | 29 | 33 |
| high school grad or GED | 29 | 34 | 31 | |
| some college/trade school | 32 | 35 | 34 | |
| college graduate | 3 | 2 | 2 | |
| Marital status | ever | 8 | 18 | 12 |
| Number of children | 0 | 70 | 58 | 64 |
| 1 | 17 | 24 | 21 | |
| 2+ | 13 | 18 | 15 | |
| Parent recovery | 24 | 32 | 28 | |
| mean (s.d.) | mean (s.d.) | mean (s.d.) | ||
| Age at baseline | 9.22 (3.46) | 9.24 (3.26) | 9.23 (3.35) | |
| Early adverse experiences | 3.95 (1.08) | 3.87 (1.19) | 3.91 (1.14) | |
| Internalizing | 1.74 (0.56) | 1.63 (0.43) | 1.69 (0.50) | |
| Externalizing | 1.87 (0.49) | 1.68* (0.38) | 1.78 (0.45) | |
| Parent-child bond | −0.11 (0.85) | 0.11 (1.14) | 0.0 (1.0) | |
| Family management | 0.03 (0.63) | −.05 (0.87) | 0.0 (0.75) | |
| School engagement | 1.22 (1.04) | 1.39 (1.25) | 1.30 (1.14) |
gender difference significant p<.05
Functional resilience included 1) being employed or enrolled in an educational program (self-report), 2) having no lifetime substance abuse or dependence (self-report based on diagnostic interview), and 3) having no adult criminal charges for at least 5 years. To qualify as employed or enrolled in an educational program, participants had to respond affirmatively to 1 of 2 survey questions, ‘Are you currently employed?’, and ‘Are you currently in school?’ To allow for stay-at-home parents of young children, we included 4 participants in the resilience category who had a child age 5 or younger and were not employed or in school, but met the criteria for no substance abuse or adult criminal charges in the last 5 years.
The Diagnostic and Statistical Manual (DSM) IV lifetime diagnoses for substance abuse or dependence in eight categories (alcohol, marijuana, opiates, sedatives, amphetamines, cocaine, hallucinogens, and inhalants) was measured using the Composite International Diagnostic Interview (CIDI) [27, 28]. Participants who ever met the criteria for abuse or dependence in any category did not meet the criteria for functional resilience. Washington State criminal records were used to determine recent adult criminal charges. Participants with any adult criminal charge in Washington that was not dropped or acquitted in the past 5 years did not meet the criteria for functional resilience. Thirteen participants who met this criterion had not been adults for the full 5 years. In these cases we checked juvenile records and found 2 who had juvenile charges 3 or more years in the past. All 13 were coded as resilient. Criminal records were not available from other states. Of the 125 participants who completed a young-adult interview, 18 (14%) were located outside of Washington. Self-report data for these participants indicated that none were incarcerated in the prior 5 years or had any Washington criminal charges.
Predictors of Resilience
The early adverse experiences index included 8 areas based on the Adverse Childhood Experiences (ACE) questionnaire [10]. Each area was coded as having been adverse (1) or not (0), and the total number of areas of adversity indicated the extent of adverse experiences. We used both prospective and retrospective accounts from children and parents to determine the presence of childhood adversities (see Table 2). Not all of the ACE measures could be included. For instance, we did not have data on whether the participant’s parents were divorced, or on any measure of neglect.
Table 2.
Components of early adverse experiences measure
| Adverse experiences | Source | Items | Response | Scoring |
|---|---|---|---|---|
| Emotional abuse | Child original study | When you misbehave do your parents yell, shout, or scream at you? | 1 – 4 | If maximum across 4 times ≥3 (yes, YES) |
| NO, no, yes, YES | ||||
| Physical abuse | Child original study | When you misbehave do your parents spank, slap, or hit you? | 1 – 4 | If maximum across 4 times ≥ (yes, YES) |
| NO, no, yes, YES | ||||
| Retrospective young-adult interview | My parent or caregiver hit me so hard it left bruises or marks. | 1 - never true | If either ≥ 4 (often) | |
| 2 - seldom | ||||
| I believe I was physically abused by my parent or caregiver. | 3 -sometimes | |||
| 4 - often | ||||
| 5 - always true | ||||
| Sexual abuse | Retrospective young-adult interview | Has anyone ever forced you to have sex with them? | 0 = no, 1 = yes | If yes and age ≤ 18 |
| How old were you the first time this happened? | Age | |||
| Family substance abuse | Parent qualified as heroin addict in methadone treatment | 1 = yes | Yes for all participants | |
| Family mental illness | Retrospective young-adult interview | Has anyone in your immediate family had problems with depression? | Biological mom, dad, sisters or brothers | If Yes to any of 4 family members |
| Mother treated violently | Parent original study | In the past year has your spouse/partner slapped, hit, or shoved you? | 0 = no | If mom reported being hit or dad reported hitting at any time |
| 1 = yes | ||||
| In the past year have you slapped, hit or shoved your spouse/partner? | ||||
| Incarcerated household member | Parent original study | Have you ever been sent to jail or prison? | 0 = no | If yes at any time for self or spouse |
| Has your spouse ever been sent to jail or prison? | 1 = yes | |||
| Loss of parent | Follow-up locating | Parent in original study confirmed dead | 0 = no | If either parent deceased |
| 1 = yes |
Parent recovery was based on parent report in a retrospective life-history calendar collected in the follow-up interview. For each of the past 10 years, parents reported if they had a drug problem or were incarcerated in that year. Parents reporting no drug problems or incarcerations in the past 10 years were coded 1; otherwise coded 0.
Parent/child bonding was measured with a child-report scale calculated as the average of 14 items from the original study, such as ‘Do you share your thoughts and feelings with your mother?’ Responses were coded on a scale from 1 to 4 (NO, no, yes, YES) or 1 to 5 (almost always, fairly often, sometimes, seldom, almost never). Items referring specifically to mother or father were averaged for children who reported on 2 parents. Each item was standardized (z-score) then averaged (Cronbach’s alphas = .80 – .88). The scales were calculated for each time point (baseline, 6, 12, and 24 months) and averaged across time points. If children were too young to answer the questions at earlier time points, their score was based on data from the later time points only.
Family management was a composite measure based on 3 constructs (guidelines, monitoring, and appropriate consequences) assessed with child reports from the original study. Guidelines were measured as the total number of family rules across 7 areas such as drug use and curfews. Monitoring was measured with a single item, ‘Do your parents know where you are and who you are with when you are away from home?’ Responses ranged from 1 to 4 (NO, no, yes, YES). Appropriate consequences was the average of 2 items, ‘When you misbehave do your parents take away privileges?’ and ‘When you misbehave do your parents send you to your room?’ (r = .30 – .46). Scores were calculated for each construct at each time point, then averaged across time and standardized. If children were not old enough to answer the questions at the earlier time points their scores were based on the later time points only. The overall family management score was computed by averaging the standardized scores across constructs (alpha =.64).
Lacking more direct measures of individual disposition [15], we used parent reports at the 24-month follow-up of child internalizing and externalizing problems derived from the Child Behavior Checklist (CBCL) [29]. Internalizing was based on 6 items including nervous, fearful or anxious, sudden changes in mood, unhappy, sad or depressed, worries, and complains no one loves him or her. Externalizing was based on 7 items including argues, acts cruel, mean or bullies, is disobedient, stubborn, sullen or irritable, lies, temper tantrums, and doesn’t feel bad about misbehaving. The 2 scores were correlated r = .54. The final score was either internalizing or externalizing, whichever one indicated the greater problems.
School engagement was a composite score based on child reports from the original study of average grades, academically involved friends, and bonding to school. Grades were measured with a single item, ‘What were your grades like this year?’ scored on a 1 – 5 scale (1 = mostly E’s and F’s; 5 = mostly A’s). Academically involved friends was measured with a single item asked about 4 different friends at the 12- and 24-month follow-ups: ‘Does this friend try to do well in school?’ Out of 8 opportunities, if children answered “yes” 4 or more times, they were scored as having academically involved friends (0/1). Bonding to school was a scale of 4 items such as ‘Do you like school’ answered on a 4-point scale (NO, no, yes, YES; alpha = .57 – .76). The scale scores were averaged across time, standardized, and averaged across constructs.
Control Variables
Childhood poverty was measured using parent report of receiving Aid for Families with Dependent Children (AFDC) at baseline, 6-, 12-, and 24-month follow-ups. The number of assessments at which the parent reported receiving AFDC ranged from 0 (no AFDC) to 4 (received AFDC at all assessments). Race and gender were based on self-reports, and age at the baseline of the study was based on parent reports of the child’s birth date and the date of the initial interview. Intervention status was randomly assigned at baseline after stratifying on parents’ race, parents’ age at first drug use, whether parents lived with a spouse or partner, and ages of the children.
Analysis
We provide descriptive information on level and variability in early adverse experiences and rates of functional resilience in terms of school/work, drug abuse, and crime. We then present chi square statistics on the relationship between treatment assignment and functional resilience. Finally, logistic regression models are presented to test for individual, family, and school predictors of resilience, controlling for treatment assignment, race, gender, age, and poverty. Missing data were imputed [30] and implemented in SAS v.9.1 [31]. Missingness ranged from 0 to 35% across variables. Forty imputations were calculated and regression coefficient estimates were averaged. Appropriate standard errors were computed using the MIANALYZE procedure [31]. Some of the 125 children were in sibling clusters (74 families total). The SAS GENMOD procedure [31] was used to adjust the standard errors of model coefficients to account for clustering using the generalized estimating equations method [32].
Results
Profiles of Risk and Resilience
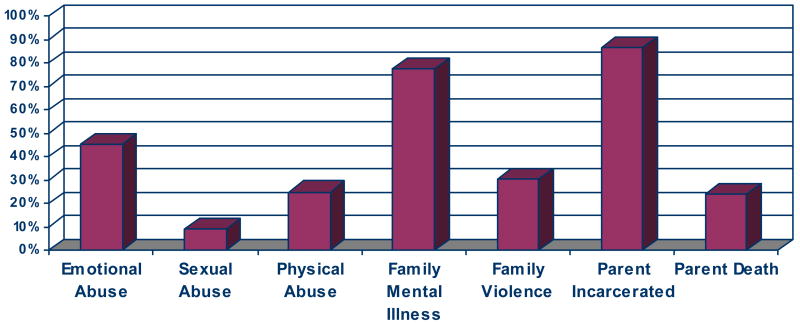
Figure 1 illustrates the range of adversity experienced in this sample. Only 4 (3.2%) young adults had no adverse experiences other than having an opiate-addicted parent. Almost 70% experienced 2 or more additional adversities and 20% experienced 4 or more. The majority (61.6%) experienced 3 or more additional adverse experiences (mean = 3.58, sd = 1.12). By comparison, in a sample of over 15,000 adult members of a hospital plan in California in 1995 to 1997, only 21.5% reported 3 or more types of childhood adversity [10], and over 36% reported none. The most common adversities in our sample were parent incarceration and familial mental illness. No data were available on whether the parents were separated or divorced, but 26% had lost one or both parents due to death.
Figure 1.
Percent of sample who experienced each adverse experience before age 18.
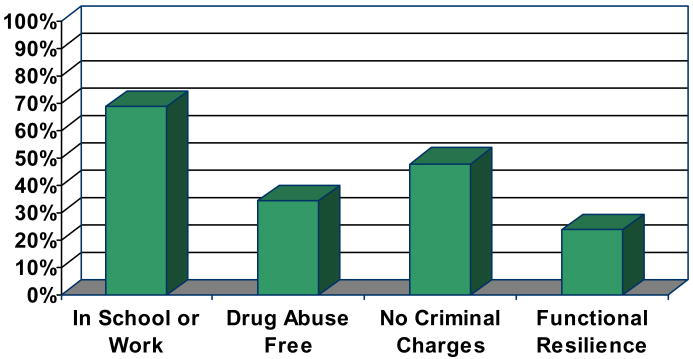
Functional resilience comprises three domains. At the time of the young-adult interview, almost 69% were working or in school. Only 34.4% had been resilient to substance abuse or dependence, and 48.0% had avoided criminal charges in Washington State (see Figure 2). The majority of abuse/dependence was to alcohol or marijuana. Crimes ranged from possession of illegal drugs to murder. Only 24.% of the sample met all 3 criteria for functional resilience. Girls were more likely than boys to be resilient (32% vs. 13%, X2 = 6.88, df = 1, p = .009), primarily because they were less likely to have an adult criminal record. Whites and non-whites were equally likely to be resilient (22% vs. 24%, X2 = 0.06, df = 1, p = .80).
Figure 2.
Percent of sample succeeding across 3 categories of functional resilience
Intervention Versus Control Differences in Resilience
Treatment effects on resilience were examined before proceeding with etiological analyses. The bivariate relationship between treatment group and resilience was not significant (X2 = 0.57, p = 0.45). Previous analyses [33] showed positive treatment effects on substance abuse for the boys only. We found no difference in meeting criteria for resilience by treatment group for girls (32% vs. 32%, X2 = 0, df = 1, p = 1.0). The difference for the boys (4% vs. 19%) was substantial, but not statistically significant (X2 = 3.12, df = 1, p = .08). Of the 8 boys in the resilient group, 7 were from families assigned to the treatment condition. Assignment to intervention group was included as a control variable in subsequent analyses.
Individual, Family, and School Predictors of Functional Resilience
Six logistic regression models were conducted to test for predictors of resilience (see Table 3), controlling for intervention assignment, age, gender, race, and childhood poverty. In Model 1 we included the index of early adverse experiences. In Models 2 – 6 we retained early adverse experiences as a control variable and separately added each of the child, parent, or school factors as predictors.
Table 3.
Odds ratios from logistic regressions predicting functional resilience in young adulthood
| Model |
||||||
|---|---|---|---|---|---|---|
| Predictor | 1 | 2 | 3 | 4 | 5 | 6 |
| Gender (female) | 4.26** | 3.94** | 4.18** | 4.55** | 4.10** | 4.38** |
| Internalizing or externalizing problems | 0.30* | |||||
| Parent recovery | 1.31 | |||||
| Parent-child bond | 0.64 | |||||
| Family management | 0.72 | |||||
| School engagement | 0.90 | |||||
p< .05,
p< .01
The gender difference was significant in every model. Girls were almost 4 times (OR ranged from 3.94 to 4.55) more likely to exhibit functional resilience in young adulthood than boys. We found no significant relationship between the number of early adverse experiences, race, age, or poverty and later resilience.
Of the additional child, parent, and school predictors, only the child-level factor of internalizing or externalizing problems significantly predicted young-adult functional resilience. Higher scores on either internalizing or externalizing were associated with less likelihood to demonstrate functional resilience. Parent recovery, parent-child bonding, family management, and school engagement were not associated with later resilience. A final step in which significant predictors were included together in a model to assess their independent effects was not necessary since only one of the tested predictors was significant.
Discussion
Despite the high level of risk faced by children in this sample, many accomplished important developmental milestones such as graduating from high school, but only 30 (24%) met the 3 criteria of working or being in school, avoiding substance abuse, and staying out of trouble with the law.
Girls were 4 times as likely to meet the criteria for resilience as boys, primarily due to higher rates of criminal charges among the boys. This gender difference is consistent with earlier studies which found girls less vulnerable to family stress [34]. The FOF treatment may have increased resilience among the boys by reducing alcohol and drug abuse [33]; however, few males achieved resilience, making conclusions about the impact of the treatment tentative. No difference in the rate of resilience was found between whites and non-whites. In our sample it was not possible to make meaningful distinctions between non-white ethnic groups.
The majority of the participants experienced adversity in 2 or more domains other than parental substance abuse. Contrary to evidence in other samples [10], the number of adverse experiences in childhood did not predict functional resilience in the FOF sample. The FOF sample is a higher risk sample than those examined in the prior studies. It may be that when multiple adversity is so common, its power to predict later outcomes is diminished.
Earlier externalizing or internalizing problems significantly reduced the chances of functional resilience such that a one standard deviation reduction in externalizing or internalizing problems made resilience 5 times more likely. This may reflect the stability of individual characteristics, particularly aggression, across developmental periods since these characteristics likely account for failures to achieve developmental tasks of young adulthood [35]. Neither parent-child bonding nor family management predicted later resilience. Successful recovery for the parent did not significantly improve resilience for their children.
This study has several limitations. Resilience is measured at only one time without providing information on the ups and downs in these young people’s lives. Werner and Smith’s [15] study of children from disadvantaged families illustrates stability and change in resilience over the life course. Children with opiate-addicted parents might show similar patterns. We used parent report of child behavior as the best available measure of individual disposition. Given the status of the parents, these reports may reflect the parent’s disposition rather than the child’s. This measure assessed the higher of either internalizing or externalizing, which may obscure the effects of two very different types of behavior. Post hoc analyses confirmed that both internalizing and externalizing behaviors were predictive of functional resilience when tested separately. When both were included together, neither was significant due to the correlation between them. Unfortunately the items from the CBCL did not include the full diagnostic scales, so we cannot determine how many of the children met clinical definitions of problem behavior. This study is further limited by the sample size which prohibits reliably testing for moderating effects of age or gender. Finally, we have no measure of IQ or reading achievement, which have been identified as protective factors among high-risk children [36].
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (R01 DA17908-01). An earlier version of this research was presented as a poster at the 3rd Annual Symposium on Addictive and Health Behavior Research in Amelia Island, FL, September, 2007. Focus on Families was conducted by the Social Development Research Group, University of Washington, in cooperation with Therapeutic Health Services of Seattle, WA. The authors gratefully acknowledge the assistance of Norman O. Johnson, Executive Director, and all the staff of Therapeutic Health Services.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Johnson HL, Glassman MB, Fiks KB, Rosen TS. Resilient children: Individual differences in developmental outcomes of children born to drug abusers. J Genet Psychol. 1990;15:523–39. doi: 10.1080/00221325.1990.9914637. [DOI] [PubMed] [Google Scholar]
- 2.Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. 2. New York: Wiley; 2006. pp. 739–95. [Google Scholar]
- 3.Catalano RF, Gainey RR, Fleming CB, Haggerty KP, Johnson NO. An experimental intervention with families of substance abusers: One-year follow-up of the Focus on Families project. Addiction. 1999;94:241–54. doi: 10.1046/j.1360-0443.1999.9422418.x. [DOI] [PubMed] [Google Scholar]
- 4.Catalano RF, Haggerty KP, Fleming CB, Skinner ML. Focus on Families: Integration of relapse prevention and child drug abuse prevention training with parents in methadone treatment. In: Witkiewitz KA, Marlatt GA, editors. Therapist’s guide to evidence-based relapse prevention. Burlington, MA: Elsevier; 2007. pp. 237–57. [Google Scholar]
- 5.Catalano RF, Haggerty KP, Gainey RR, Hoppe MJ. Reducing parental risk factors for children’s substance misuse: preliminary outcomes with opiate-addicted parents. Subst Use Misuse. 1997;32:699–721. doi: 10.3109/10826089709039371. [DOI] [PubMed] [Google Scholar]
- 6.Hogan DM. Annotation: the psychological development and welfare of children of opiate and cocaine users: review and research needs. J Child Psychol Psychiatry. 1998;39:609–20. [PubMed] [Google Scholar]
- 7.Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction. 2004;99:552–59. doi: 10.1111/j.1360-0443.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- 8.Jester JM, Jacobson SW, Sokol RJ, Tuttle BS, Jacobson JL. The influence of maternal drinking and drug use on the quality of the home environment of school-aged children. Alcohol Clin Exp Res. 2000;24:1187–97. [PubMed] [Google Scholar]
- 9.Kumpfer KL. Special populations: Etiology and prevention of vulnerability to chemical dependency in children of substance abusers. In: Brown BS, Mills AR, editors. Youth at high risk for substance abuse. Rockville, MD: National Institute on Drug Abuse; 1987. pp. 1–72. [Google Scholar]
- 10.Anda RF, Brown DW, Felitti VJ, et al. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–94. doi: 10.1016/j.amepre.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richters JE, Weintraub S. Beyond diathesis: Toward an understanding of high-risk environments. In: Rolf J, Masten A, Cicchetti D, Nuechterlein KG, Weintraub S, editors. Risk and protective factors in the development of psychopathology. New York: Cambridge University Press; 1990. pp. 67–96. [Google Scholar]
- 12.Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000;71:543–62. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masten AS. Resilience in individual development: Successful adaptation despite risk and adversity. In: Wang MC, Gordon EW, editors. Educational resilience in inner-city American: Challenges and prospects. Hillsdale, NJ: Erlbaum; 1994. [Google Scholar]
- 14.Kumpfer KL, Bluth B. Parent/child transactional processes predictive of resilience or vulnerability to “substance abuse disorders”. Subst Use Misuse. 2004;39:671–98. doi: 10.1081/ja-120034011. [DOI] [PubMed] [Google Scholar]
- 15.Werner EE, Smith RS. Journeys from childhood to midlife: Risk, resilience, and recovery. Ithaca, NY: Cornell University Press; 2001. [DOI] [PubMed] [Google Scholar]
- 16.Werner EE. Resilient offspring of alcoholics: A longitudinal study from birth to age 18. J Stud Alcohol. 1986;47:34–40. doi: 10.15288/jsa.1986.47.34. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan HB. Toward an understanding of resilience: A critical review of definitions and models. In: Glantz MD, Johnson JL, editors. Resilience and development: Positive life adaptations. New York: Kluwer Academic/Plenum Publishers; 1999. [Google Scholar]
- 18.Schulenberg JE, Bryant AL, O’Malley PM. Taking hold of some kind of life: How developmental tasks relate to trajectories of well-being during the transition to adulthood. Dev Psychopathol. 2004;16:1119–40. doi: 10.1017/s0954579404040167. [DOI] [PubMed] [Google Scholar]
- 19.Rutter M. Psychosocial resilience and protective mechanisms. In: Rolf JE, Masten AS, Cicchette D, Neuchterlein K, Weintraub S, editors. Risk and protective factors in the development of psychopathology. New York: Cambridge University Press; 1990. pp. 181–214. [Google Scholar]
- 20.Dawe S, Harnett PH, Staiger P, Dadds MR. Parent training skills and methadone maintenance: Clinical opportunities and challenges. Drug Alcohol Depend. 2000;60:1–11. doi: 10.1016/s0376-8716(99)00144-1. [DOI] [PubMed] [Google Scholar]
- 21.Clair DJ, Genest M. Variables associated with the adjustment of children of alcoholics. In: Lotterhos JF, McGuire MD, editors. Nurse care planning on alcoholism: A resource guide. Greenville, NC: East Carolina University, Alcoholism Training Program; 1987. [Google Scholar]
- 22.Luthar SS, Sexton CC. Maternal drug abuse versus maternal depression: Vulnerability and resilience among school-age and adolescent offspring. Dev Psychopathol. 2007;19:205–25. doi: 10.1017/S0954579407070113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson JL, Leff M. Children of substance abusers: overview of research findings. Pediatrics. 1999;103:1085–99. [PubMed] [Google Scholar]
- 24.Wolin SJ, Bennett LA, Jocobs JS. Assessing family rituals in alcoholic families. In: Imber-Black E, Roberts J, Whitney R, editors. Rituals in families and family therapy. New York: WW Norton &Company; 1988. [Google Scholar]
- 25.Rutter M. Psychosocial resilience and protective mechanism. Am J Orthopsychiatry. 1987;57:317–31. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 26.Haggerty KP, Fleming CB, Catalano RF, et al. Ten years later: Locating and interviewing children of drug abusers. Evaluation and Program Planning. 2008;31:1–9. doi: 10.1016/j.evalprogplan.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowley TJ, Mikulich SK, Ehlers KM, Whitmore EA, Macdonald MJ. Validity of structured clinical evaluations in adolescents with conduct and substance problems. J Am Acad Child Adolesc Psychiatry. 2001;40:265–73. doi: 10.1097/00004583-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF) Int J Methods Psychiatric Res. 1998;7:171–85. [Google Scholar]
- 29.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 30.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- 31.SAS Institute. SAS/STAT Software, Version 8.2: The MIANALYZE Procedure. SAS Institute Inc; [Accessed October 1, 2007]. Available at: http://www.sas.com/rnd/app/papers/miv802.pdf. [Google Scholar]
- 32.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 33.Haggerty KP, Skinner ML, Fleming CB, Gainey RR, Catalano RF. Long-term effects of Focus on Families on substance abuse onset among children of parents in methadone treatment. Addiction. doi: 10.1111/j.1360-0443.2008.02360.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hetherington EM. Coping with family transitions: Winners, losers, and survivors. Child Dev. 1989;60:1–14. doi: 10.1111/j.1467-8624.1989.tb02690.x. [DOI] [PubMed] [Google Scholar]
- 35.Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. Am Psychol. 1989;44:329–35. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- 36.Petras H, Schaeffer CM, Ialongo N, et al. When the course of aggressive behavior in childhood does not predict antisocial outcomes in adolescence and young adulthood: An examination of potential explanatory variables. Dev Psychopathol. 2004;16:919–41. doi: 10.1017/s0954579404040076. [DOI] [PubMed] [Google Scholar]