Abstract
Biliary lipids are a family of four dissimilar molecular species consisting of a mixture of bile salts (substituted cholanoic acids), phospholipids, mostly (>96%) diacylphosphatidylcholines, unesterified cholesterol, and bilirubin conjugates known trivially as lipopigments. The primary pathophysiological defect in cholesterol gallstone disease is hypersecretion of hepatic cholesterol into bile with less frequent hyposecretion of bile salts and/or phospholipids. Several other gallbladder abnormalities contribute and include hypomotility, immune-mediated inflammation, hypersecretion of gelling mucins, and accelerated phase transitions; there is also reduced intestinal motility that augments “secondary” bile salt synthesis by the anaerobic microflora. Cholesterol nucleation is initiated when unilamellar vesicles of cholesterol plus biliary phospholipids fuse to form multilamellar vesicles. From these “plate-like” cholesterol monohydrate crystals, the building blocks of macroscopic stones are nucleated heterogeneously by mucin gel. Multiple Lith gene loci have been identified in inbred mice, paving the way for discovery of an ever-increasing number of LITH genes in humans. Because of the frequency of the metabolic syndrome today, insulin resistance and LITH genes all interact with a number of environmental cholelithogenic factors to cause the gallstone phenotype. This review summarizes current concepts of the physical-chemical state of biliary lipids in health and in lithogenic bile and outlines the molecular, genetic, hepatic, and cholecystic factors that underlie the pathogenesis of cholesterol gallstones.
Keywords: bile flow, bile salt, biliary lipid secretion, cholesterol, crystallization, lipid transporter, liquid crystal, LITH gene, micelle, mucin, nucleation, phase diagram, phospholipid, vesicle, hydrophilic-hydrophobic balance
In the United States, cholelithiasis [mostly cholesterol (∼85%) and “black” pigment (∼15%) stones] is one of the most prevalent and costly digestive diseases, with at least 20 million Americans affected (1). Prevalence of cholesterol stones is increasing because of the epidemic of obesity, with insulin resistance being a fundamental feature of the metabolic syndrome. Approximately one million new cases of gallstones are discovered each year, 700,000 cholecystectomies are performed, and unavoidable complications result in 3,000 deaths in the United States. Furthermore, medical expenses for the treatment of gallstone disease exceeded $6 billion in the bimillenial year.
Recent studies on both humans and mouse models have demonstrated that polygenes underlie the predisposition to develop most cholesterol gallstones (2–4). The powerful genetic technique of quantitative trait locus (QTL) analysis has identified multiple cholesterol gallstone (Lith) gene loci in inbred mice (4). Dissecting the physical-chemical, pathophysiological, and genetic influences of individual Lith genes has provided a logical framework to elucidate the genetic mechanisms of cholesterol gallstone disease in humans. Here, we summarize biliary lipid physical chemistry and the molecular pathogenesis of cholesterol gallstone formation, focusing principally on recent progress.
PHYSICAL CHEMISTRY OF BILIARY LIPIDS
Cholesterol, phospholipids, and bile salts are the major lipid components of bile (Fig. 1). Biliary cholesterol is nonesterified and accounts for at least 97% of total sterols, the remainder comprising cholesterol precursors and dietary phyto- and conchosterols. The major phospholipids of bile are mixed diacylphosphatidylcholines. These insoluble, swelling amphiphiles are structured with a hydrophilic, zwitterionic phosphocholine headgroup and two hydrophobic fatty acid chains. Because cholesterol and phospholipids are insoluble in an aqueous medium, mixed micelles with bile salts and unilamellar (single-bilayered) vesicles are required to maintain them in solution. The common bile salts are soluble amphiphiles that consist of a hydrophobic steroid nucleus of four fused hydrocarbon rings, subtending polar hydroxyl functions on one face, and a flexible aliphatic side chain amidated with glycine or taurine. Cholate and chenodeoxycholate, the principal bile salts of humans, are “primary” species synthesized directly from cholesterol in the liver. The “secondary” bile salts, deoxycholate and lithocholate, are modifications of the primary bile salts by specialized anaerobic intestinal bacteria (5). “Tertiary” bile salts, ursodeoxycholates, the 7βOH-epimer of chenodeoxycholate, and lithocholate-3-SO4, are the result of modifications of secondary bile salts by intestinal flora and hepatocytes. All of these cycle continuously in humans in a highly efficient enterohepatic circulation.
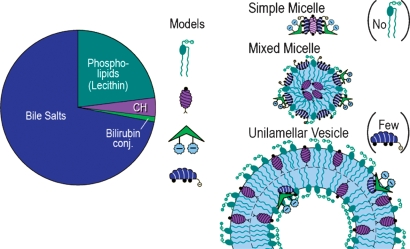
Fig. 1.
Pie diagram representation of the relative proportions of the four biliary lipids in humans with conventional presentations of their space-filling molecular models and the three common macromolecular structures that they form in bile. Molecules of bilirubin conjugates, although highly water soluble, are bound to the hydrophilic faces of bile salt molecules in solution and on micelles and vesicles by π-orbital-OH interactions (see text for further description).
Bile salt monomers self-associate spontaneously to form simple micelles when their concentrations exceed the critical micellar concentration (Fig. 1). These simple micelles are small (∼3 nm in diameter), thermodynamically stable aggregates that solubilize small quantities of biliary cholesterol. Mixed micelles are larger (∼4 to 8 nm in diameter), quasispherical, and thermodynamically stable aggregates that are composed of bile salts, cholesterol, and phospholipids with a high capacity to solubilize cholesterol (Fig. 1). Vesicles are spherical structures (40 to 100 nm in diameter) composed of unilamellar phospholipids and cholesterol bilayers but little bile salt (Fig. 1). Liquid crystals (>500 nm in diameter) are multilamellar vesicles derived from fusion of unilamellar vesicles principally in the gallbladder (6, 7). Unilamellar vesicles are usually stable and constitute an additional transport system for cholesterol molecules, but liquid crystals invariably imply initiation of the cholesterol nucleation sequence. Although conjugated bilirubin molecules in “ridge-tile” conformation (Fig. 1) are water soluble, they are bound to the hydrophilic faces of bile salt molecules in tight π-orbital-OH interactions.
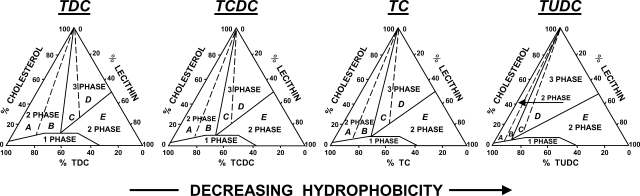
As demonstrated by ternary phase diagrams (Fig. 2), cholesterol is solubilized in thermodynamically stable simple and mixed micelles in small one-phase micellar zones. By contrast, “supersaturated” bile implies cholesterol present in concentrations above and beyond what can be solubilized in the micellar zones; however “true” micellar supersaturation is transient, and excess micellar cholesterol becomes dispersed in cholesterol-phospholipid vesicles (8). For a relative lipid composition in a native bile sample plotted on an appropriate triangular phase diagram, the proportional distance along an axis joined to the cholesterol apex (Fig. 2), i.e., ratio of the actual amount of cholesterol present to the maximal micellar solubility, is defined as the cholesterol saturation index (9).
Fig. 2.
Equilibrium phase diagrams for common taurine-conjugated bile salts, lecithin (egg yolk), and cholesterol in 0.15 M NaCl as functions of hydrophilic-hydrophobic balance of the bile salt (37°C, pH 7.0, total lipid concentration 7.5 g/dl). As bile salt hydrophobicity is decreased (TDC > TCDC > TC > TUDC), the maximum micellar cholesterol solubility is reduced; concomitantly, the multiphase regions above the micellar zone are all shifted to the left, i.e., to lower phospholipids-to-bile salt ratios. Because of this, the crystallization pathways (labeled A to E) are also moved to the left. Reproduced with permission from Ref. 22.
PHYSIOLOGY OF BILIARY LIPID SECRETION
Physical-chemical and imaging studies demonstrate that bile salts stimulate the biliary secretion of unilamellar vesicles (10) from the external hemileaflet of the canalicular membrane (7, 11). The radii of vesicles within the canalicular spaces of rat liver by transmission electron microscopy (7) and dynamic light-scattering spectroscopy (12) vary between 60 and 80 nm. Dynamic light scattering spectroscopy (10) has also been applied to quantify the changing proportions of vesicles as they are slowly transformed into mixed micelles in native bile.
In contrast with the otherwise insoluble lipids, bile salts enter the canalicular space as monomers and include those that are newly synthesized (<5%) and those that have undergone enterohepatic cycling (>95%). The principal driving forces for biliary lipid secretion are ATP binding cassette (ABC) transporters located on the canalicular membrane of the hepatocyte. ABCB11 is the dedicated common bile salt export pump (13, 14). The relationship between bile salt secretion and both cholesterol and phospholipid secretion is curvilinear. At low bile salt secretion rates (<10 μmol/h/kg in humans), more cholesterol is secreted per molecule of bile salt than at higher rates. At high bile salt secretion rates, for example, during and after eating, biliary saturation is less than during the interprandial periods. This diurnal rhythm persists, but is set to higher cholesterol levels, in the lithogenic state (15).
Hepatic secretion of biliary phosphatidylcholines is dependent on the product of the Abcb4 gene in mice (16). ABCB4 is uniquely responsible for translocation or “flipping” of biliary-destined phosphatidylcholine molecules from the inner to outer bilayer leaflet of the canalicular membrane. As evidenced by transmission electron microscopy, when Abcb4 is knocked out in mice, vesicles disappear from the canalicular space only to reappear with the introduction of the expressed human homolog ABCB4 (17, 18).
Overexpression of the canalicular heterodimeric ABCG5/ABCG8 transporter increases the cholesterol content of gallbladder bile (19). However, ABCG5/ABCG8 requires a functioning ABCB4, indicating the necessity for a hydrophobic “sink” for solubilizing the secreted cholesterol molecules. Gallstone formation is observed in ABCG5 or ABC/G8 knockout mice challenged with a lithogenic diet (20), suggesting that an ABCG5/ABCG8-independent pathway for biliary cholesterol secretion exists.
PATHOPHYSIOLOGY OF CHOLESTEROL GALLSTONE FORMATION
The primary pathophysiologic defect in most cholelithogenic humans is hepatic hypersecretion of cholesterol, which may be accompanied by normal, high, or low secretion rates of biliary bile salts and phospholipids. Singly or in combination, this represents the cardinal hepatic pathophysiology inducing cholesterol supersaturation of gallbladder bile (8, 21).
Triangular phase diagrams for model systems of cholesterol, egg yolk lecithin, and bile salts in 0.15 M NaCl not only act as templates to determine the physical states of natural biles at equilibrium (8, 21) but also reveal cholesterol crystallization pathways (Fig. 2). Five different crystallization pathways with individual phase transition sequences (A to E) have been identified as functions of bile salt-to-lecithin ratio, common bile salt species (with varying hydrophilic/hydrophobic balance), total lipid concentration, and temperature, as well as cholesterol saturation indices (22). In region A (Fig. 2) with the lowest phospholipid contents, arc-like crystals, representing a monoclinic polymorph of cholesterol monohydrate of an elongated habit (23), appear first and evolve via helical and tubular crystalline structures to form classic plate-like triclinic cholesterol monohydrate crystals. In region B (Fig. 2) with higher phospholipid contents, classic cholesterol monohydrate crystals form earlier than polymorphic cholesterol monohydrate crystals. In region C (Fig. 2) with typical physiological phospholipid contents, early multilamellar liquid crystals are followed by classic plate-like cholesterol monohydrate crystals; subsequently, the polymorphic cholesterol monohydrate crystals appear. In region D (Fig. 2) with still higher lecithin contents, liquid crystals are followed by classic plate-like cholesterol monohydrate crystals only. In region E (Fig. 2) at the highest lecithin contents, liquid crystals are stable indefinitely, and solid cholesterol crystals never form. Decreases in temperature (37°C to 4°C), total lipid concentration (7.5–2.5 g/dl), and bile salt hydrophobicity (Fig. 2) progressively shift all crystallization pathways to lower lecithin contents as well as retarding crystallization and reducing micellar cholesterol solubilities (22). The cholesterol crystallization pathways and sequences observed in human gallbladder bile are identical to those occurring in appropriately matched model bile (24). Nonetheless, the kinetics of these phase transitions are faster in lithogenic human bile compared with either model bile (24) or supersaturated gallbladder bile from control subjects (25). It is believed that the principal heterogenous pronucleating/kinetic agent in gallbladder bile is mucin gel (26).
Gallbladder motility is compromised early in cholesterol gallstone formation (27) in part because of absorption of cholesterol molecules (28) and their incorporation into and stiffening of sarcolemmal membranes (29). The result is diversion of more hepatic bile into the intestine and as a consequence elevation in deoxycholate conjugate levels in bile (15). This in turn further promotes cholesterol hypersecretion as well as more rapid nucleation and crystallization in gallbladder bile (22). It is still far from settled whether endogenous or infective intestinal bacteria and an activated immune system (30) play facilitating roles in human cholesterol gallstone formation.
Studies in many laboratory animals indicate that altering intestinal cholesterol absorption greatly influences cholesterol cholelithogenesis (31, 32), mostly because these diets contain massive amounts of cholesterol and cholic acid to facilitate intestinal absorption. Nonetheless, it appears that the extent of intestinal cholesterol absorption may play only a minor role in human cholesterol gallstone disease (33).
GENETIC ANALYSIS OF CHOLESTEROL GALLSTONE FORMATION
Evidence for a genetic basis of cholesterol gallstone disease in humans rests on geographic and ethnic differences as well as on family and twin studies (34). A genetic predisposition is present in Pima Indians (age-adjusted prevalence 48%), certain other North and South American Indians, and Chileans (34). By contrast, the overall age-adjusted prevalence in American Caucasians and Europeans is ∼20%, with the lowest prevalence (<5%) being observed in African and Central Asian populations. Recently, a study of 43,141 Swedish twin pairs (3) provided conclusive evidence for a role of genetic factors (25% of phenotype) in clinically symptomatic cholesterol gallstone patients. Interestingly, most Western gallstone disease seems to have an Amerindian or Viking genetic inheritance, apparently “thrifty” genes that emerged during the last glacial epoch (35).
Table 1 provides an inventory of human cholesterol gallstone (LITH) genes collated from the work by Lammert and Sauerbruch (36) with pathophysiological susceptibility factors and the mouse orthologous Lith genes (where known) derived by QTL analysis (34, 37). The table shows that most genes are reported in single case-control studies only and have not been replicated in larger population cohorts and other ethnic groups. Some of the genes can be termed causative, leading directly by bile lipid dysfunction (e.g., a gain in function of ABCG5/G8), whereas others (e.g., apolipoprotein B and apolipoprotein C1) represent genetic modifiers that exhibit a lithogenic effect only in the setting of a primary genetic risk factor. Where established, Table 1 also lists gene variants and potential pathophysiological mechanism involved (36).
TABLE 1.
Lammert and Sauerbruch's 2008 inventory of human cholesterol gallstone (LITH) genesa
| Databases |
Frequency |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Genes | Gene Symbols | Function | OMIMb,c | Genecardsd | Rare Monogenic | Familial Oligogenic | Common Polygenic | Gene Variants | Mouse Model | Concordant Mouse Lith Loci | Potential Mechanisms |
| ABC transporter B4 | ABCB4 (GBD1) | Hepatocanalicular phosphatidylcholine (lecithin) flippase | 171060 and 600803 | GC07M 086676 | + | Multiple | + | Biliary phospholipid secretion ↓ | |||
| ABC transporter B11 | ABCB11 | Hepatocanalicular bile salt export pump | 603201 | GC02M 169604 | + | Multiple | (+) | Lith1 | Biliary bile salt secretion ↓ | ||
| ABC transporters G5/G8 | ABCG5/G8 (GBD4) | Hepatocanalicular cholesterol transporter | 605459/605460 and 611465 | GC02P 043951/GC02P 043977 | + (Germany Sorbs, Chile, China) | ABCG8 p.D19H (rs1188753) | + | Lith9 | Biliary cholesterol secretion ↑ | ||
| β3 Adrenergic receptor | ARDB3 | 109691 | GC08M 037939 | (+) (Germany) | p.R64W (rs4944) | Gallbladder hypomotility | |||||
| Apolipoprotein A1 | APOA1 | 107680 | GC11M 116211 | (+) (China, India) | −75G>A, RFLP | Biliary cholesterol secretion ↑ secondary to reverse cholesterol transport ↑ | |||||
| Apolipoprotein B | APOB | 107730 | GC02M 021135 | + | (+) (China, Poland) | c.2488C>T, c.4154G>A | + | Biliary cholesterol secretion ↑ secondary to hepatic VLDL synthesis ↓ and intestinal cholesterol absorption ↑ | |||
| Apolipoprotein C1 | APOC1 | 107710 | GC19P 050109 | (+) (India) | RFLP | APOC1 ↑ remnant-like particle cholesterol ↑ | |||||
| Androgen receptor | AR | 313700 | GC0XP 066680 | (+) (Greece) | c.172(CAG)n | ||||||
| Cholecystokinin 1 receptor | CCK1R | 118444 | GC04M 026159 | + | (+) (India) | RFLP | + | Lith13 | Gallbladder and small intestinal hypomotility | ||
| Cholesterol ester transfer protein | CETP | 118470 | GC16P 055553 | (+) (Finland) | RFLP | Gene absent in mice | Hepatic cholesterol uptake ↑ from HDL catabolism ↑ | ||||
| Cytochrome P450 7A1 | CYP7A1 | Cholesterol 7α-hydroxylase (rate-limiting enzyme of bile salt synthesis) | 118470 | GC08M 059565 | + | (+) (China) | Promoter SNP −204A>C | + | Bile salt synthesis ↓ | ||
| Estrogen receptor 2 | ESR2 | Estrogen receptor β | 601663 | GC14M 063621 | (+) (Greece) | c.1092+3607(CA)n | (+) | Cholesterol synthesis ↑ | |||
| Low-density lipoprotein receptor-related protein associated protein 1 | LRPAP1 | 104225 | GC04M 003551 | (+) (India) | Intron 5 insertion/deletion (rs11267919) | + | Lith13 | Hepatic cholesterol uptake ↑ from chylomicron remnants via LRP ↑ | |||
Reproduced from Ref. 38 (slightly modified) by permission of the copyright holders (Springer-Verlag/Falk Foundation) and the authors; individual references are cited therein.
Abbreviations used: OMIM, Online Mendelian inheritance in man; GBD, gallbladder disease; RFLP, restriction fragment length polymorphism; SNP, single nucleotide polymorphism; LRP, low-density lipoprotein receptor-related protein.
The table also lists the rare monogenic cholesterol gallstone syndromes. The first evidence that human cholesterol gallstones might be caused by a single gene defect arose from studies showing that homozygous deletion mutation in the rate-limiting cholesterol 7α-hydroxylase (CYP7A1) gene, resulting in loss of enzyme function (38). Missense mutations in the ABCB4 gene are the basis for another type of monogenic cholelithiasis (39) where cholesterol gallbladder stones and even recurrent cholesterol stones forming in the bile ducts are associated with very low phospholipids-to-bile salt ratios in bile. Moreover, Asian patients with hepatolithiasis also exhibit low levels of ABCB4 plus hepatic phosphatidylcholine transfer protein causing markedly decreased biliary phospholipid secretion rates (40). The genes for cholecystokinin (CCK) and the CCK-1 receptor (CCK-1R), which regulates gallbladder motility, are attractive cholelithogenic candidate genes (Table 1) in the setting of supersaturated bile. An aberrant splicing of CCK-1R, which is predicted to result in a nonfunctional receptor, is found in some obese patients with cholesterol gallstones (34).
With respect to the common polygenic gallstone disease (Table 1), associations between gene polymorphisms and cholesterol gallstone formation indicate that the causative genes are highly heterogenous (Table 1). For example, a common variant (D19H) of the canalicular cholesterol transporter ABCG5/G8 gene (Table 1) confers odds ratios of 2 to 3 in heterozygotes and 7 in homozygous carriers based on genome-wide association (41) and linkage (42) studies from Germany and Chile. Interestingly this common susceptibility gene (Table 1) was predicted by QTL mapping in inbred mice (43). By contrast, polymorphisms in the apolipoprotein (APO) AI, B, and C1 genes and the cholesterol ester transfer protein are modifiers, but a cholelithogenic role for APOE polymorphisms has been discounted (36).
FUTURE RESEARCH DIRECTIONS
Hepatocanalicular hypersecretion of cholesterol into bile caused by LITH genes and insulin resistance upregulating ABCG5/G8 via the dysregulation of the FOX01 transcription factor (44) will most likely prevail as the key primary pathogenic risk factors for inducing supersaturation of human bile. Once all gene-gene and gene-environment interactions are defined in humans at risk, we anticipate that such fundamental knowledge will lead to critical diagnostic and preventive measures for this exceptionally common and expensive disease.
Acknowledgments
We are most grateful to Drs. Lammert and Sauerbruch, the authors of Ref. 38, as well as Springer-Verlag and the Falk Foundation for permission to republish Table 1 in slightly modified form.
Abbreviations
ABC, ATP binding cassette (transporter)
APO, apolipoprotein
CCK, cholecystokinin
CYP7A1, cholesterol 7α-hydroxylase
QTL, quantitative trait locus
This work was supported in part by grants DK-54012, DK-73917 (to D.Q-H.W.), DK-56626, DK-48873 (to D.E.C.), DK-36588, and DK-73687 (to M.C.C.) from the National Institutes of Health (U.S. Public Health Services).
Published, JLR Papers in Press, November 17, 2008.
References
- 1.Liver Disease Subcommittee of the Digestive Disease Interagency Coordinating Committee. 2004. Action Plan for Liver Disease Research. National Institutes of Health, Bethesda, MD.
- 2.Wang D. Q-H., B. Paigen, and M. C. Carey. 1997. Phenotypic characterization of Lith genes that determine susceptibility to cholesterol cholelithiasis in inbred mice: physical-chemistry of gallbladder bile. J. Lipid Res. 38 1395–1411. [PubMed] [Google Scholar]
- 3.Katsika D., A. Grjibovski, C. Einarsson, F. Lammert, P. Lichtenstein, and H. U. Marschall. 2005. Genetic and environmental influences on symptomatic gallstone disease: a Swedish study of 43,141 twin pairs. Hepatology. 41 1138–1143. [DOI] [PubMed] [Google Scholar]
- 4.Khanuja B., Y. C. Cheah, M. Hunt, P. M. Nishina, D. Q-H. Wang, H. W. Chen, J. T. Billheimer, M. C. Carey, and B. Paigen. 1995. Lith1, a major gene affecting cholesterol gallstone formation among inbred strains of mice. Proc. Natl. Acad. Sci. USA. 92 7729–7733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hofmann A. F. 2007. Biliary secretion and excretion in health and disease: current concepts. Ann. Hepatol. 6 15–27. [PubMed] [Google Scholar]
- 6.Mazer N. A., and M. C. Carey. 1983. Quasi-elastic light-scattering studies of aqueous biliary lipid systems. Cholesterol solubilization and precipitation in model bile solutions. Biochemistry. 22 426–442. [DOI] [PubMed] [Google Scholar]
- 7.Crawford J. M., G. M. Möckel, A. R. Crawford, S. J. Hagen, V. C. Hatch, S. Barnes, J. J. Godleski, and M. C. Carey. 1995. Imaging biliary lipid secretion in the rat: ultrastructural evidence for vesiculation of the hepatocyte canalicular membrane. J. Lipid Res. 36 2147–2163. [PubMed] [Google Scholar]
- 8.Carey M. C., and D. M. Small. 1978. The physical chemistry of cholesterol solubility in bile. Relationship to gallstone formation and dissolution in man. J. Clin. Invest. 61 998–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carey M. C. 1978. Critical tables for calculating the cholesterol saturation of native bile. J. Lipid Res. 19 945–955. [PubMed] [Google Scholar]
- 10.Cohen D. E., M. Angelico, and M. C. Carey. 1989. Quasielastic light scattering evidence for vesicular secretion of biliary lipids. Am. J. Physiol. 257 G1–G8. [DOI] [PubMed] [Google Scholar]
- 11.Sömjen G. J., Y. Marikovsky, P. Lelkes, and T. Gilat. 1986. Cholesterol-phospholipid vesicles in human bile: an ultrastructural study. Biochim. Biophys. Acta. 879 14–21. [DOI] [PubMed] [Google Scholar]
- 12.Möckel G. M., S. Gorti, R. K. Tandon, T. Tanaka, and M. C. Carey. 1995. Microscope laser light-scattering spectroscopy of vesicles within canaliculi of rat hepatocytes couplets. Am. J. Physiol. 269 G73–G84. [DOI] [PubMed] [Google Scholar]
- 13.Gerloff T., B. Stieger, B. Hagenbuch, J. Madon, L. Landmann, J. Roth, A. F. Hofmann, and P. J. Meier. 1998. The sister of P-glycoprotein represents the canalicular bile salt export pump of mammalian liver. J. Biol. Chem. 273 10046–10050. [DOI] [PubMed] [Google Scholar]
- 14.Wang R., M. Salem, I. M. Yousef, B. Tuchweber, P. Lam, S. J. Childs, C. D. Helgason, C. Ackerley, M. J. Phillips, and V. Ling. 2001. Targeted inactivation of sister of P-glycoprotein gene (spgp) in mice results in nonprogressive but persistent intrahepatic cholestasis. Proc. Natl. Acad. Sci. USA. 98 2011–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carey, M. C., and W. Duane. 1994. Enterohepatic circulation. In The Liver: Biology and Pathobiology. 3rd Edition. I. M. Arias, J. L. Boyer, N. Fausto, W. B. Jakoby, D. Schachter, and D. A. Shafritz, editors. Raven Press, New York. 719–767.
- 16.Smit J. J., A. H. Schinkel, R. P. Oude Elferink, A. K. Groen, E. Wagenaar, L. van Deemter, C. A. Mol, R. Ottenhoff, N. M. van der Lugt, M. A. van Roon, et al. 1993. Homozygous disruption of the murine mdr2 P-glycoprotein gene leads to a complete absence of phospholipid from bile and to liver disease. Cell. 75 451–462. [DOI] [PubMed] [Google Scholar]
- 17.Crawford A. R., A. J. Smith, V. C. Hatch, R. P. Oude Elferink, P. Borst, and J. M. Crawford. 1997. Hepatic secretion of phospholipid vesicles in the mouse critically depends on mdr2 or MDR3 P-glycoprotein expression. Visualization by electron microscopy. J. Clin. Invest. 100 2562–2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oude Elferink R. P., R. Ottenhoff, M. van Wijland, J. J. Smit, A. H. Schinkel, and A. K. Groen. 1995. Regulation of biliary lipid secretion by mdr2 P-glycoprotein in the mouse. J. Clin. Invest. 95 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu L., J. Li-Hawkins, R. E. Hammer, K. E. Berge, J. D. Horton, J. C. Cohen, and H. H. Hobbs. 2002. Overexpression of ABCG5 and ABCG8 promotes biliary cholesterol secretion and reduces fractional absorption of dietary cholesterol. J. Clin. Invest. 110 671–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang H. H., S. B. Patel, M. C. Carey, and D. Q-H. Wang. 2007. Quantifying anomalous intestinal sterol uptake, lymphatic transport, and biliary secretion in Abcg8(−/−) mice. Hepatology. 45 998–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Admirand W. H., and D. M. Small. 1968. The physicochemical basis of cholesterol gallstone formation in man. J. Clin. Invest. 47 1043–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang D. Q-H., and M. C. Carey. 1996. Complete mapping of crystallization pathways during cholesterol precipitation from model bile: influence of physical-chemical variables of pathophysiologic relevance and identification of a stable liquid crystalline state in cold, dilute and hydrophilic bile salt-containing systems. J. Lipid Res. 37 606–630. [PubMed] [Google Scholar]
- 23.Weihs D., J. Schmidt, I. Goldiner, D. Danino, M. Rubin, Y. Talmon, and F. M. Konikoff. 2005. Biliary cholesterol crystallization characterized by single-crystal cryogenic electron diffraction. J. Lipid Res. 46 942–948. [DOI] [PubMed] [Google Scholar]
- 24.Wang D. Q-H., and M. C. Carey. 1996. Characterization of crystallization pathways during cholesterol precipitation from human gallbladder biles: identical pathways to corresponding model biles with three predominating sequences. J. Lipid Res. 37 2539–2549. [PubMed] [Google Scholar]
- 25.Holan K. R., R. T. Holzbach, R. E. Hermann, A. M. Cooperman, and W. J. Claffey. 1979. Nucleation time: a key factor in the pathogenesis of cholesterol gallstone disease. Gastroenterology. 77 611–617. [PubMed] [Google Scholar]
- 26.Lee S. P., J. T. LaMont, and M. C. Carey. 1981. Role of gallbladder mucus hypersecretion in the evolution of cholesterol gallstones. J. Clin. Invest. 67 1712–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Portincasa P., A. Di Ciaula, G. Vendemiale, V. Palmieri, A. Moschetta, G. P. Vanberge-Henegouwen, and G. Palasciano. 2000. Gallbladder motility and cholesterol crystallization in bile from patients with pigment and cholesterol gallstones. Eur. J. Clin. Invest. 30 317–324. [DOI] [PubMed] [Google Scholar]
- 28.Erranz B., J. F. Miquel, W. S. Argraves, J. L. Barth, F. Pimentel, and M. P. Marzolo. 2004. Megalin and cubilin expression in gallbladder epithelium and regulation by bile acids. J. Lipid Res. 45 2185–2198. [DOI] [PubMed] [Google Scholar]
- 29.Yu P., Q. Chen, K. M. Harnett, J. Amaral, P. Biancani, and J. Behar. 1995. Direct G protein activation reverses impaired CCK signaling in human gallbladders with cholesterol stones. Am. J. Physiol. 269 G659–G665. [DOI] [PubMed] [Google Scholar]
- 30.Maurer K. J., V. P. Rao, Z. Ge, A. B. Rogers, T. J. Oura, M. C. Carey, and J. G. Fox. 2007. T-cell function is critical for murine cholesterol gallstone formation. Gastroenterology. 133 1304–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buhman K. K., M. Accad, S. Novak, R. S. Choi, J. S. Wong, R. L. Hamilton, S. Turley, and R. V. Farese, Jr. 2000. Resistance to diet-induced hypercholesterolemia and gallstone formation in ACAT2-deficient mice. Nat. Med. 6 1341–1347. [DOI] [PubMed] [Google Scholar]
- 32.Wang H. H., P. Portincasa, N. Mendez-Sanchez, M. Uribe, and D. Q-H. Wang. 2008. Effect of ezetimibe on the prevention and dissolution of cholesterol gallstones. Gastroenterology. 134 2101–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kern F., Jr. 1994. Effects of dietary cholesterol on cholesterol and bile acid homeostasis in patients with cholesterol gallstones. J. Clin. Invest. 93 1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paigen, B., and M. C. Carey. 2002. Gallstones. In Genetic Basis of Common Diseases. 2nd editon. R. A. King, J. I. Rotter, and A. G. Motulsky, editors. Oxford University Press, London. 298–335.
- 35.Carey M. C., and B. Paigen. 2002. Epidemiology of the American Indians' burden and its likely genetic origins. Hepatology. 36 781–791. [DOI] [PubMed] [Google Scholar]
- 36.Lammert, F., and T. Sauerbruch. 2008. Pathogenesis of gallstone formation: updated inventory of human lithogenic genes. In Future Perspectives in Gastroenterology (Falk Symposium 161). M. C. Carey, P. Dité, A. Gabryelewicz, V. Keim, and J. Mössner, editors. Springer-Verlang, Dordrecht, The Netherlands. 99–107.
- 37.Lyons M. A., and H. Wittenburg. 2006. Cholesterol gallstone susceptibility loci: a mouse map, candidate gene evaluation, and guide to human LITH genes. Gastroenterology. 131 1943–1970. [DOI] [PubMed] [Google Scholar]
- 38.Pullinger C. R., C. Eng, G. Salen, S. Shefer, A. K. Batta, S. K. Erickson, A. Verhagen, C. R. Rivera, S. J. Mulvihill, M. J. Malloy, et al. 2002. Human cholesterol 7α-hydroxylase (CYP7A1) deficiency has a hypercholesterolemic phenotype. J. Clin. Invest. 110 109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosmorduc O., B. Hermelin, P. Y. Boelle, R. Parc, J. Taboury, and R. Poupon. 2003. ABCB4 gene mutation-associated cholelithiasis in adults. Gastroenterology. 125 452–459. [DOI] [PubMed] [Google Scholar]
- 40.Shoda J., K. Oda, H. Suzuki, Y. Sugiyama, K. Ito, D. E. Cohen, L. Feng, J. Kamiya, Y. Nimura, H. Miyazaki, et al. 2001. Etiologic significance of defects in cholesterol, phospholipid, and bile acid metabolism in the liver of patients with intrahepatic calculi. Hepatology. 33 1194–1205. [DOI] [PubMed] [Google Scholar]
- 41.Buch S., C. Schafmayer, H. Volzke, C. Becker, A. Franke, H. von Eller-Eberstein, C. Kluck, I. Bassmann, M. Brosch, F. Lammert, et al. 2007. A genome-wide association scan identifies the hepatic cholesterol transporter ABCG8 as a susceptibility factor for human gallstone disease. Nat. Genet. 39 995–999. [DOI] [PubMed] [Google Scholar]
- 42.Grünhage F., M. Acalovschi, S. Tirziu, M. Walier, T. F. Wienker, A. Ciocan, O. Mosteanu, T. Sauerbruch, and F. Lammert. 2007. Increased gallstone risk in humans conferred by common variant of hepatic ATP-binding cassette transporter for cholesterol. Hepatology. 46 793–801. [DOI] [PubMed] [Google Scholar]
- 43.Wittenburg H., M. A. Lyons, R. Li, G. A. Churchill, M. C. Carey, and B. Paigen. 2003. FXR and ABCG5/ABCG8 as determinants of cholesterol gallstone formation from quantitative trait locus mapping in mice. Gastroenterology. 125 868–881. [DOI] [PubMed] [Google Scholar]
- 44.Biddinger S. B., J. T. Haas, B. B. Yu, O. Bezy, E. Jing, W. Zhang, T. G. Unterman, M. C. Carey, and C. R. Kahn. 2008. Hepatic insulin resistance directly promotes formation of cholesterol gallstones. Nat. Med. 14 778–782. [DOI] [PMC free article] [PubMed] [Google Scholar]