Abstract
The determinants of the negative association between Streptococcus pneumoniae and Stapylococcus aureus colonization are unknown. In this matched case-control study, the odds of co-colonization with S. aureus were significantly lower for individuals carrying a piliated vs. nonpiliated S. pneumoniae strain, suggesting the pilus may be a determinant of the negative association.
Keywords: S. pneumoniae, S. aureus, pneumococcal pilus, case-control
Staphylococcus aureus and Streptococcus pneumoniae are important pathogens causing high morbidity and mortality worldwide [1, 2]. S. aureus is carried by 30% of healthy adults and ~10% of young children, most consistently in the anterior nares [2]. In contrast, S. pneumoniae is mainly carried by children [1], most frequently in the nasopharynx (NP) [3].
Carriage by healthy individuals is the source of transmission for both pathogens, and carriage is the initial step of invasion[4, 5]. Several epidemiologic studies have reported a negative association between S. pneumoniae nasopharyngeal colonization and S. aureus nasal colonization [6–9], which was most significant for S. pneumoniae serotypes included in the 7-valent pneumococcal conjugate vaccine (PCV7) [6, 7]. This finding raised public health concern that a rise in S. aureus colonization and disease may follow PCV7 implementation [10].
We have been studying possible mechanisms of the negative association between these two pathogens. We have shown that hydrogen peroxide (H2O2) produced by S. pneumoniae is directly bactericidal to S. aureus in vitro [11]. While high-H2O2-producing strains were less likely to be found in a host co-colonized with S. aureus, the effect was modest and not statistically significant, thus leaving the serotype-specificity of this negative association largely unexplained. Therefore the effect of other factors described earlier was sought [11, 12].
Two groups identified the presence in S. pneumoniae of a pilus-like structure [13, 14], which they characterized as an adhesin and an inflammatory virulence factor [13, 15]. This pilus is present mainly in PCV7 serotypes [16–18]. Thus we tested the hypothesis that piliated pneumococcal strains are less likely to be co-carried with S. aureus than non-piliated strains, using a collection of strains from a previous carriage study in Israel. Using a matched analysis comparing strains of the same serotype, we were able to avoid the confounding effect of serotype and to ask whether, within each serotype, the presence of the pilus was independently predictive of a lower probability of S. aureus co-colonization.
Methods
The original study (details given in [6]) took place during 2002–2005 in primary care clinics of Maccabi Healthcare Services, an Israeli HMO. Approximately 4,500 children <40 months old were screened for carriage of nasal S. aureus and nasopharyngeal S. pneumoniae. None of the subjects received any pneumococcal vaccine.
The pilus operon encodes three structural proteins, RrgA, B, and C. The rrgC gene has been shown to be 100% conserved across strains, and its presence as detected by PCR is an excellent predictor of the presence of the pilus by Western Blot analysis [14, 16]. To screen strains, boilates of bacterial colonies were used as DNA templates for a PCR assay for the amplification of rrgC. Primers were 5’GCTCTGTGTTTTTCTCTTGTATGG3’ and 5’ATCAATCCGTGGTCGCTTGTTATTTTTA3’ and the reaction conditions were 30 cycles of 94°C for 15 s, 55°C for 30 s and 72°C for 1min/kb, followed by 5 min at 72°C.
270 strains selected initially to assess H2O2 production in VT vs. non-VT were reassessed to determine the prevalence of the pilus. Since these strains were not randomly selected, we also estimated the prevalence of the pilus in the study population by standardizing for serotype and age frequencies observed in the 270 strains to the full study population frequencies.
To determine whether pneumococcal strains from individuals co-colonized with S. aureus and S. pneumoniae are less frequently piliated than strains from individuals colonized with S. pneumoniae only, we conducted a case-control study. Given the prevalence results in this study population, we focused only on strains of serotypes that sometimes carry the pilus, ie. VT strains, excluding 18C (which is not piliated here or in other collections [17, 18]). Cases and controls were selected from the same collection of approximately 2000 NP strains mentioned above. Cases were defined as pneumococcal strains isolated from individuals who were co-colonized with S. aureus and controls were defined as strains isolated from individuals colonized only with S. pneumoniae. Each case was matched with three to five controls by: age (within 6 months), DCC attendance and serotype. After limiting the full collection to VT strains, 78 cases were available. For several of the cases, we could not identify three matching controls; these cases were thus excluded from analysis and a total of 61 cases and 236 controls were included. A matched analysis was performed using conditional logistic regression.
Results
The 270 selected strains consisted of 129 VT strains, 32 VT-related strains (6A, 9A/B/N, 19A and 23A/B) strains and 107 non-VT strains. The non-vaccine strains were of 16 different capsular types, of which 37% were of serogroup 15; 9.3% were of serotype 3; 8.4% were of serotype 16F; 6.5% were of serogroup 35 and the remaining 40 strains (38.8%) belonged to 12 different serotypes.
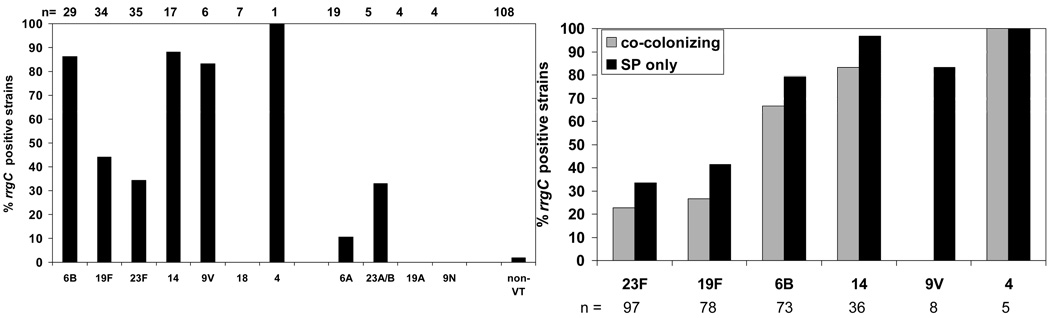
The pilus was present in 79 of 270 strains (29.2%). The prevalence of the pilus was highest among the VT strains (67 of 130, 51.5%), with the exception of serotype 18C, in which none of the 7 strains tested were positive. The pilus was significantly less prevalent in strains of vaccine-related serotype (4 of 32, 12.5%; two each of 23A and 6A P=0.0001; compared to pilus prevalence in VT) or non VT strains (2 of 108, 1.8%; one each of 17F and 11A, P<0.0001; compared to pilus prevalence in VT). (See Figure 1a).
Figure 1.
Prevalence of the pilus by the serotype, as determined by rrgC postive PCR a. in the 270 selected strains. b. among VT strains in the case-control study Grey bars – cases, Black bars – controls.
After standardization, the pilus prevalence in the Israeli study population is estimated to be 30%, with 62.6% of VT strains, 17.8% of VT-related and <1% of non-VT strains. These figures are all within 4% of the crude (unstandardized) estimates, indicating that the nonrandom strain selection did not importantly affect our estimates of pilus frequency.
To determine whether pneumococcal strains that carry the pilus are particularly 'protective' against S. aureus carriage, we conducted a case-control study focusing on VT strains. Sixty one cases and 236 matched controls were included in the analysis (Table 1).
Table 1.
Study population of the case-control study.
| Cases n=61 (co-colonized with SA) |
Controls n=236 (SP only) |
|||
|---|---|---|---|---|
| Adults | 13 (21.3%) | 45 (19.1%) | ||
| Children | 48 (79.7%) | 191 (80.9% | ||
| Age: | 0–12m | 13 (21.3%) | 44 (18.6%) | |
| 13–30m | 16 (26.2%) | 91 (38.6%) | ||
| 31–40m | 19 (31.1%) | 56 (23.7%) | ||
| DCC attendance | 34 (69.4%) | 139 (72.8%) | ||
| SP serotype | 23F | 22 (36.1%) | 75 (31.8%) | |
| 19F | 15 (24.6%) | 63 (26.7%) | ||
| 6B | 15 (24.6%) | 58 (24.6%) | ||
| 14 | 6 (9.8%) | 30 (12.7%) | ||
| 9V | 2 (3.3%) | 6 (2.5%) | ||
| 4 | 1 (1.6%) | 4 (1.7%) | ||
The frequency of the pilus among S. pneumoniae strains found in children co-colonized with S. aureus was less than or equal to that among strains isolated from non-cocolonized children for every serotype considered (Figure 1b). To further adjust for all matched factors (age and DCC attendance) a conditional logistic analysis was performed and determined that the odds to be co-colonized with S. aureus were 2.13-fold lower (OR 0.47, 95%CI 0.24 – 0.95) for individuals carrying a piliated vs. a nonpiliated S. pneumoniae strain.
Discussion
The mechanism(s) of the negative association between S. pneumoniae and S. aureus colonization remain to be defined. Based on prior studies [6–8, 11, 12, 19] it is likely that the mechanism is multi-factorial, probably involving both host immune responses to colonization and bacterial characteristics that may promote inhibition of the other pathogen. The hypothesis tested here was based on the epidemiologic studies showing that the negative association between carriage of S. pneumoniae and S. aureus is particularly strong for VT strains and our own prior data regarding the prevalence of the pilus in VT strains [16] Our analysis shows that the pneumococcal pilus is negatively associated with staphylococcal co-colonization, even when controlling for confounders such as serotype, age and DCC attendance.
Our finding that the presence of the pilus in carried pneumococci is negatively associated with S. aureus carriage could be explained by at least two mechanisms: Since the pilus is an inflammatory structure [13], piliated strains may directly induce a host immune response deleterious to S. aureus colonization. A non-mutually exclusive alternative is that piliated pneumococci are more adherent [15], and for that reason are more able to antagonize staphylococcal colonization by other (non-pilus-mediated) inhibitory effects, such as H2O2 secretion or some other mechanism.
Our study is inherently limited in its ability to establish a causal relation between carriage of the pilus and inhibition of S. aureus colonization; a case-control study can reveal an association which can only be suggestive of a causal relation. Unknown confounders can never be fully ruled out in such studies. An additional limitation, also inherent to the study design, is that the prevalence of co-colonization was determined in a point prevalence study, which does not provide a direct estimate of the impact of S. pneumoniae on preventing incidence or shortening duration of S. aureus carriage.
Despite these limitations, this study suggests that the pilus is a determinant of the negative association between S. pneumoniae and S. aureus carriage. The fact that the association was reproduced in 5 of 6 serotypes examined reduces the likelihood that some other bacterial factor, more common in piliated strains, was responsible for the negative association, since one would expect that the same factor would not be consistently associated with the pilus in unrelated serotypes. Further mechanistic studies will be required to assess how the pilus may play such a role. In addition, ongoing epidemiologic studies of the prevalence of the pilus in different populations will be required to test a key prediction of this hypothesis, that the impact of pneumococcal vaccination on S. aureus carriage will depend importantly on whether it continues to reduce the frequency of piliated strains relative to unvaccinated populations.
Acknowledgements
We would like to acknowledge all the physicians, study coordinators and technicians who were involved in the originial Israeli study. We thank Krzysztof Trzcinski and Yingjie Lu for thoughtful advice and suggestions. This study was supported by NIH grants AI066013 to RM and AI048935 to ML.
This study was funded by NIH grant AI066013 (to R.M.)
Footnotes
This study was partially presented at the 6th International Symposium on Pneumococci and Pneumococcal Diseases in Iceland, June, 2008.
All authors have no conflict of interest.
References
- 1.O'Brien KL, Nohynek H. Report from a WHO Working Group: standard method for detecting upper respiratory carriage of Streptococcus pneumoniae. Pediatr Infect Dis J. 2003;22(2):e1–e11. doi: 10.1097/01.inf.0000049347.42983.77. [DOI] [PubMed]
- 2.Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, Nouwen JL. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005;5(12):751–762. doi: 10.1016/S1473-3099(05)70295-4. [DOI] [PubMed] [Google Scholar]
- 3.Ghaffar F, Friedland IR, McCracken GH., Jr Dynamics of nasopharyngeal colonization by Streptococcus pneumoniae. Pediatr Infect Dis J. 1999;18(7):638–646. doi: 10.1097/00006454-199907000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Huang SS, Diekema DJ, Warren DK, et al. Strain-relatedness of methicillin-resistant Staphylococcus aureus isolates recovered from patients with repeated infection. Clin Infect Dis. 2008;46(8):1241–1247. doi: 10.1086/529381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bogaert D, De Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004;4(3):144–154. doi: 10.1016/S1473-3099(04)00938-7. [DOI] [PubMed] [Google Scholar]
- 6.Regev-Yochay G, Dagan R, Raz M, Carmeli Y, Shainberg B, Derazne E, Rahav G, Rubinstein E. Association between carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children. Jama. 2004;292(6):716–720. doi: 10.1001/jama.292.6.716. [DOI] [PubMed] [Google Scholar]
- 7.Bogaert D, van Belkum A, Sluijter M, Luijendijk A, de Groot R, Rumke HC, Verbrugh HA, Hermans PW. Colonisation by Streptococcus pneumoniae and Staphylococcus aureus in healthy children. Lancet. 2004;363(9424):1871–1872. doi: 10.1016/S0140-6736(04)16357-5. [DOI] [PubMed] [Google Scholar]
- 8.McNally LM, Jeena PM, Gajee K, Sturm AW, Tomkins AM, Coovadia HM, Goldblatt D. Lack of association between the nasopharyngeal carriage of Streptococcus pneumoniae and Staphylococcus aureus in HIV-1-infected South African children. J Infect Dis. 2006;194(3):385–390. doi: 10.1086/505076. [DOI] [PubMed] [Google Scholar]
- 9.Watson K, Carville K, Bowman J, Jacoby P, Riley TV, Leach AJ, Lehmann D. Upper respiratory tract bacterial carriage in Aboriginal and non-Aboriginal children in a semi-arid area of Western Australia. Pediatr Infect Dis J. 2006;25(9):782–790. doi: 10.1097/01.inf.0000232705.49634.68. [DOI] [PubMed] [Google Scholar]
- 10.Veenhoven R, Bogaert D, Uiterwaal C, et al. Effect of conjugate pneumococcal vaccine followed by polysaccharide pneumococcal vaccine on recurrent acute otitis media: a randomised study. Lancet. 2003;361(9376):2189–2195. doi: 10.1016/S0140-6736(03)13772-5. [DOI] [PubMed] [Google Scholar]
- 11.Regev-Yochay G, Trzcinski K, Thompson CM, Malley R, Lipsitch M. Interference between Streptococcus pneumoniae and Staphylococcus aureus: In Vitro Hydrogen Peroxide-Mediated Killing by Streptococcus pneumoniae. J Bacteriol. 2006;188(13):4996–5001. doi: 10.1128/JB.00317-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Regev-Yochay G, Malley R, Rubinstein E, Raz M, Dagan R, Lipsitch M. In vitro bactericidal activity of Streptococcus pneumoniae and bactericidal susceptibility of Staphylococcus aureus strains isolated from cocolonized versus noncocolonized children. J Clin Microbiol. 2008;46(2):747–749. doi: 10.1128/JCM.01781-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barocchi MA, Ries J, Zogaj X, et al. A pneumococcal pilus influences virulence and host inflammatory responses. Proc Natl Acad Sci U S A. 2006;103(8):2857–2862. doi: 10.1073/pnas.0511017103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LeMieux J, Hava DL, Basset A, Camilli A. RrgA and RrgB are components of a multisubunit pilus encoded by the Streptococcus pneumoniae rlrA pathogenicity islet. Infect Immun. 2006;74(4):2453–2456. doi: 10.1128/IAI.74.4.2453-2456.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson AL, Ries J, Bagnoli F, et al. RrgA is a pilus-associated adhesin in Streptococcus pneumoniae. Mol Microbiol. 2007;66(2):329–340. doi: 10.1111/j.1365-2958.2007.05908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basset A, Trzcinski K, Hermos C, et al. Association of the pneumococcal pilus with certain capsular serotypes but not with increased virulence. J Clin Microbiol. 2007;45(6):1684–1689. doi: 10.1128/JCM.00265-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moschioni M, Donati C, Muzzi A, et al. Streptococcus pneumoniae contains 3 rlrA pilus variants that are clonally related. J Infect Dis. 2008;197(6):888–896. doi: 10.1086/528375. [DOI] [PubMed] [Google Scholar]
- 18.Aguiar SI, Serrano I, Pinto FR, Melo-Cristino J, Ramirez M. The presence of the pilus locus is a clonal property among pneumococcal invasive isolates. BMC Microbiol. 2008;8:41. doi: 10.1186/1471-2180-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park B, Nizet V, Liu GY. Role of Staphylococcus aureus catalase in niche competition against Streptococcus pneumoniae. J Bacteriol. 2008;190(7):2275–2278. doi: 10.1128/JB.00006-08. [DOI] [PMC free article] [PubMed] [Google Scholar]