Abstract
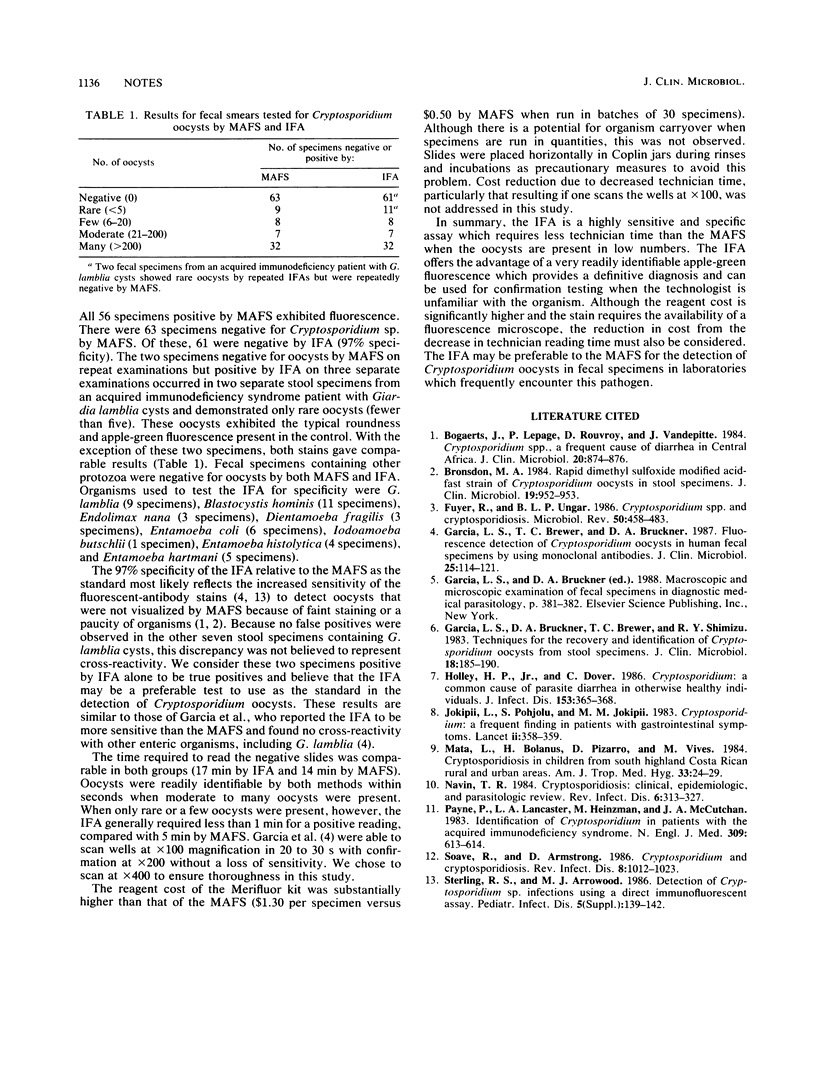
An indirect fluorescence assay (IFA) with monoclonal antibodies developed for the detection of Cryptosporidium oocysts in fecal smears (Meridian Diagnostics, Inc., Cincinnati, Ohio) was compared with the Zeihl-Neelsen-modified acid-fast stain (MAFS) in 119 human fecal specimens collected between 1984 and 1987. The sensitivity of the IFA was 100%; all 56 specimens positive by MAFS exhibited fluorescence. There were 63 specimens negative for Cryptosporidium sp. by MAFS; of these, 61 were negative by IFA (97% specificity). This discrepancy may reflect an increased sensitivity of the IFA to detect oocysts that were not visualized by MAFS because of faint staining or a paucity of organisms. On average, the IFA required less time than the MAFS (1 versus 5 min, respectively) when only rare or few oocysts were present. Cost comparison of reagents showed the IFA to be three times more expensive. The IFA offers a reasonable alternative to the MAFS because of its high sensitivity and specificity, the simplicity of performing it and interpreting results, and its capability of providing a definitive diagnosis of Cryptosporidium oocysts.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bogaerts J., Lepage P., Rouvroy D., Vandepitte J. Cryptosporidium spp., a frequent cause of diarrhea in Central Africa. J Clin Microbiol. 1984 Nov;20(5):874–876. doi: 10.1128/jcm.20.5.874-876.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronsdon M. A. Rapid dimethyl sulfoxide-modified acid-fast stain of Cryptosporidium oocysts in stool specimens. J Clin Microbiol. 1984 Jun;19(6):952–953. doi: 10.1128/jcm.19.6.952-953.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayer R., Ungar B. L. Cryptosporidium spp. and cryptosporidiosis. Microbiol Rev. 1986 Dec;50(4):458–483. doi: 10.1128/mr.50.4.458-483.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Brewer T. C., Bruckner D. A. Fluorescence detection of Cryptosporidium oocysts in human fecal specimens by using monoclonal antibodies. J Clin Microbiol. 1987 Jan;25(1):119–121. doi: 10.1128/jcm.25.1.119-121.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Bruckner D. A., Brewer T. C., Shimizu R. Y. Techniques for the recovery and identification of Cryptosporidium oocysts from stool specimens. J Clin Microbiol. 1983 Jul;18(1):185–190. doi: 10.1128/jcm.18.1.185-190.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holley H. P., Jr, Dover C. Cryptosporidium: a common cause of parasitic diarrhea in otherwise healthy individuals. J Infect Dis. 1986 Feb;153(2):365–368. doi: 10.1093/infdis/153.2.365. [DOI] [PubMed] [Google Scholar]
- Jokipii L., Pohjola S., Jokipii A. M. Cryptosporidium: a frequent finding in patients with gastrointestinal symptoms. Lancet. 1983 Aug 13;2(8346):358–361. doi: 10.1016/s0140-6736(83)90341-0. [DOI] [PubMed] [Google Scholar]
- Mata L., Bolaños H., Pizarro D., Vives M. Cryptosporidiosis in children from some highland Costa Rican rural and urban areas. Am J Trop Med Hyg. 1984 Jan;33(1):24–29. doi: 10.4269/ajtmh.1984.33.24. [DOI] [PubMed] [Google Scholar]
- Navin T. R., Juranek D. D. Cryptosporidiosis: clinical, epidemiologic, and parasitologic review. Rev Infect Dis. 1984 May-Jun;6(3):313–327. doi: 10.1093/clinids/6.3.313. [DOI] [PubMed] [Google Scholar]
- Payne P., Lancaster L. A., Heinzman M., McCutchan J. A. Identification of Cryptosporidium in patients with the acquired immunologic syndrome. N Engl J Med. 1983 Sep 8;309(10):613–614. doi: 10.1056/NEJM198309083091014. [DOI] [PubMed] [Google Scholar]
- Soave R., Armstrong D. Cryptosporidium and cryptosporidiosis. Rev Infect Dis. 1986 Nov-Dec;8(6):1012–1023. doi: 10.1093/clinids/8.6.1012. [DOI] [PubMed] [Google Scholar]


