Abstract
AIMS
To study the influence of patients’ education and cardiovascular risk factors on the probability of statin treatment.
METHODS
A prospective cohort study of participants in regional health surveys in Norway 2000–2002 with statin use recorded in the Norwegian Prescription Database 2004–2006 as outcome measure. Information on history of cardiovascular disease (CVD) and diabetes, lipid levels, blood pressure, use of cardiovascular drugs, body mass index, family history, smoking, physical activity, marital status and place of residence was obtained at baseline. A total of 20 212 men and women aged 40–41, 45–46 and 59–61 years who reported never use of statins were included. Educational level was retrieved from Statistics Norway. Adjusted relative risks (RR) were estimated by Poisson regression.
RESULTS
Whereas 655 participants reported a history of CVD or diabetes, 19 557 reported no such history. In the non-CVD/diabetes group 1620 persons (8%) became statin users and 222 persons (34%) in the CVD/diabetes group. RR of becoming a statin user for high vs. low education increased from 0.64 [95% confidence interval (CI) 0.55, 0.73] to 0.91 (95% CI 0.79, 1.05) after adjustment in the non-CVD/diabetes group and from 0.94 (95% CI 0.70, 1.26) to 1.35 (95% CI 1.00, 1.81) in the CVD/diabetes group.
CONCLUSIONS
Patients with no history of CVD/diabetes were prescribed statins according to cardiovascular risk independent of education. There was a tendency to a higher probability of statin treatment among highly educated compared with people of lower educational level in the group with a history of CVD or diabetes, after adjustment for other CVD risk factors, particularly in women.
Keywords: pharmacoepidemiology, prescription database, risk factors, statins, socioeconomic status, education
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Use of statins reduces cardiovascular morbidity and mortality.
Little is known about educational inequalities in use of statins.
WHAT THIS STUDY ADDS
In Norway in patients with no history of cardiovascular disease or diabetes, start of statin treatment was not associated with educational level after adjustment for cardiovascular risk factors.
In patients with a history of cardiovascular disease or diabetes, especially highly educated women tended to start statin treatment more often than women of low educational level.
Persistence of statin treatment did not vary by educational level.
Introduction
There has been a widening gap in mortality between people with high and low socioeconomic position in Norway and several other Western European countries [1]. A Norwegian cohort study showed that a great part of educational inequalities in ischaemic heart disease mortality was attributed to differences in cardiovascular risk factors [2]. Educational inequalities in ischaemic heart disease mortality persisted within the cohort during the period 1974–1988 [3], whereas the relative inequality in cardiovascular mortality increased between successive birth cohorts. Educational inequalities in prevention of cardiovascular morbidity and mortality are therefore of major concern.
High cholesterol is one of the major risk factor for coronary heart disease (CHD). Together with sex, age, blood pressure and smoking it enters into the risk chart that has been constructed for Europe [Systematic COronary Risk Evaluation (SCORE)][4]. In 1994 the 4S study was the first to document that use of simvastatin significantly reduced mortality in patients with CHD [5]. There is now convincing evidence that statins have beneficial effects on cardiovascular morbidity and mortality. However, most statin studies have been in the population with established CHD for secondary prevention, and it has been questioned whether primary prevention with statins in the population at risk is evidence based [6].
Norway has the highest statin use in Europe [7, 8]. However, little is known about variation in statin use by socioeconomic class within Norway. The aim of this study was to analyse if there are educational inequalities in use of statins in 2004–2006 when adjusting for the cardiovascular risk factors observed at baseline in participants from population-based health surveys 2000–2002.
Methods
This was a prospective cohort study of participants in regional health surveys in Norway 2000–2002 with statin use as recorded in the Norwegian Prescription Database (NorPD) 2004–2006 as outcome measure. The following surveys were included: The Oslo Health Study, Oppland and Hedmark studies, Finnmark and Troms studies inclusive of the Tromsø Study 5. These five counties cover both rural and urban regions in northern and southern Norway. They are part of Cohort Norway (CONOR) [9]. Height, weight and blood pressure were measured at the screening site and a nonfasting blood sample was drawn to measure serum total cholesterol, high-density lipoprotein (HDL)-cholesterol and triglycerides. Participants also filled in a questionnaire about whether they used medicines for treatment of hypertension, cholesterol-lowering drugs (statins) and other medicines, smoking habits, physical activity, family history of CHD, marital status, and previous or present history of myocardial infarction, angina pectoris, stroke or diabetes [10, 11]. These variables were considered as baseline characteristics.
All inhabitants in the selected age cohorts in the health survey areas were invited [9]. Our study participants were 40–41, 45–46 and 59–61 years old at baseline examination. In these age cohorts 44 157 persons were invited, of whom 23 288 (53%) participated and agreed to store and to link data to other health registers for research purposes. A total of 1% (n = 267) were excluded due to death or emigration before 1 January 2004, varying from 0.7% in the highest to 1.1% in the lowest educational group. Participants who did not answer the question about use of statins at screening (n = 427) were also excluded. Of the remaining 22 594 participants, 20 925 (93%) reported never use of statins at baseline. Of these, 20 887 had obtained measurements of serum total cholesterol at baseline in 2000–2002. Finally, 220 persons with missing information about education and 455 with missing information about history of cardiovascular disease (CVD) or diabetes were excluded. Our final study population included 20 212 men and women, which was reduced to 19 156 in multivariate analyses due to missing covariates. The study was approved by The Norwegian Data Inspectorate, and the Regional Committee for Medical Research Ethics evaluated it. Informed consent was obtained from the study participants. The study was conducted in accordance with the World Declaration of Helsinki.
We analysed two subgroups: (i) the CVD/diabetes group included participants who reported at least one of the conditions myocardial infarction, angina, stroke or diabetes at baseline, and (ii) the non-CVD/diabetes group included participants reporting none of these. The questionnaire did not include questions about peripheral arterial disease.
The analytic strategy included (i) stratified analyses by subgroup, age and sex, (ii) Poisson regression for each subgroup including age and sex as covariates and (iii) an overall Poisson regression model including subgroup, age and sex as covariates. Cardiovascular risk factors and other confounding variables were included in the multivariate models. The number of participants included in the crude analyses and the analyses adjusted for age and sex only was 19 557 in the non-CVD/diabetes group and 655 in the CVD/diabetes group. Due to missing values the numbers included in multivariate analyses were reduced to 18 547 in the non-CVD/diabetes group and 609 in the CVD/diabetes group. In the age- and sex-stratified analyses there were no further adjustments for age. Age was included as two groups, age 40, 41, 45, 46 and 59, 60, 61 years, in Poisson regression. Total and HDL-cholesterol, systolic blood pressure (SBP) and body mass index were included as continuous variables in multivariate analyses. Categorical confounders included medication for hypertension (yes/no), family history of CHD (yes/no), daily smoking (yes/no), physical activity in leisure time (active/inactive), married (yes/no) and five counties of residence, defined as four dummy variables.
Education statistics are register based and different levels were taken from the 2001 Census registered by Statistics Norway. Education was classified according to NUS 2000 (Norwegian standard for categorization of education) into three groups: low (primary or lower secondary school), middle (higher secondary or high school) and high (college/university) [12]. The information on the population's highest level of education was first collected as part of the Population and Housing Census in 1970. Information on the population's highest level of education has since then been updated each year with annual files on education completed in Norway. The number of immigrants listed with an unknown level of education has been substantially reduced since ‘Education Completed Abroad’ surveys were conducted in 1991 and 1999. Information about level of education from Statistics Norway was linked by the unique person identity number to health survey records.
Data from the health survey records were also linked to NorPD. NorPD includes prescription data from the total population (4.75 million) in Norway since 2004 [13, 14]. It contains information from all prescription drugs, reimbursed or not, dispensed at pharmacies to individual patients living outside institutions. The identity of patients has been encrypted, but each record contains a unique person identifier, which makes it possible to identify and follow all prescriptions for each individual and to link data to other registries and health surveys. The medicines are classified according to the Anatomical Therapeutic Chemical (ATC) classification system [15]. Data used in this study are: patients’ unique identifier, sex and age, the date of dispensing, and ATC code. Participants in the health surveys, who had at least one prescription of a statin (ATC group C10AA) dispensed during 2004–2006 were defined as statin users.
We used Poisson regression analyses to calculate relative risk (RR) of becoming a statin user when adjusting for confounding factors [16]. Baseline characteristics were presented as age-adjusted means and percentages by analysis of covariance. Adjusted means were evaluated at age 50 years. Differences in distribution of number of statin prescriptions were tested by Pearson's χ2 tests. P < 0.05 was regarded as significant and no attempt was made to adjust for multiple testing.
Results
Persons with the highest education (college/university) had generally the most favourable cardiovascular risk profiles at baseline in both subgroups (Table 1).
Table 1.
Baseline characteristics of study participants according to education and two subgroups
| Non-CVD/diabetes group (n = 19 557†)Education | CVD/diabetes group (n = 655‡)Education | |||||
|---|---|---|---|---|---|---|
| Low | Middle | High | Low | Middle | High | |
| n | 2903 | 10 427 | 6227 | 188 | 333 | 134 |
| Men (%) | 46.1 | 45.1 | 44.1 | 49.5 | 56.8 | 58.2 |
| Age, mean | 52 | 48 | 47 | 56 | 53 | 53 |
| Age adjusted: | ||||||
| Total cholesterol, mean (mmol l−1) | 5.9 | 5.8 | 5.7*** | 5.7 | 5.6 | 5.5 |
| Total cholesterol ≥ 8 mmol l−1, % | 3.2 | 2.8 | 2.1** | 0.6 | 1.3 | 2.0 |
| HDL-cholesterol, mean (mmol l−1) | 1.4 | 1.4 | 1.5*** | 1.3 | 1.3 | 1.4*** |
| Triglycerides, mean (mmol l−1) | 1.8 | 1.7 | 1.5*** | 2.2 | 2.1 | 1.6*** |
| Systolic blood pressure, mean (mmHg) | 132 | 131 | 128*** | 135 | 134 | 129* |
| Medication for hypertension, % | 8.6 | 6.9 | 5.4*** | 26.0 | 23.0 | 17.5 |
| Body mass index, mean (kg m−2) | 26.9 | 26.5 | 25.6*** | 28.3 | 28.0 | 26.4** |
| Family history of CHD, % | 44.9 | 44.4 | 40.9*** | 48.3 | 49.2 | 45.5 |
| Daily smoking, % | 45.7 | 35.0 | 17.7*** | 41.3 | 35.4 | 19.9*** |
| Physical activity, % | 72.9 | 77.8 | 81.5*** | 66.1 | 70.5 | 70.0 |
| Married, % | 61.1 | 62.4 | 64.5*** | 56.0 | 59.3 | 62.6 |
P (equality) < 0.05;
P (equality) < 0.01;
P (equality) < 0.001.
Of these, 1010 (5%) had at least one missing value.
Of these, 46 (7%) had at least one missing value. Education: low, primary or lower secondary; middle, higher secondary or high school; high, college/university. Age-adjusted means evaluated at age 50 years. CVD, cardiovascular disease; HDL, high-density lipoprotein; CHD, coronary heart disease.
Of the 19 557 participants who reported no history of CVD/diabetes at baseline (Table 2), 1620 (8%) became statin users. The probability of statin treatment was negatively associated with level of education in both age groups and both sexes in crude stratified analyses. The association was attenuated in all groups after adjusting for baseline cardiovascular risk factors. Overall, RR of becoming a statin user was 0.64 in the highest educational group vs. the lowest educated after adjustment for age and sex, increasing to 0.91 [95% confidence interval (CI) 0.79, 1.05] after further adjustment for known cardiovascular risk factors.
Table 2.
Number of statin users 2004–2006 among participants in population-based studies 2000–2002, who reported never use of statins at baseline
| Non-CVD/diabetes group | CVD/diabetes group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Education† | n | % | Crude RR (n = 19 557) | 95% CI | Adjusted RR‡ (n = 18 547) | 95% CI | n | % | Crude RR (n = 655) | 95% CI | Adjusted RR‡ (n = 609) | 95% CI |
| Men 40–41, 45–46 | ||||||||||||
| Low | 57 | 8.1 | 1.00 | Ref | 1.00 | Ref | 7 | 35.0 | 1.00 | Ref | 1.00 | Ref |
| Middle | 228 | 6.8 | 0.84 | 0.64, 1.11 | 0.97 | 0.73, 1.29 | 20 | 23.8 | 0.68 | 0.33, 1.39 | 0.67 | 0.29, 1.57 |
| High | 95 | 4.9 | 0.61 | 0.45, 0.84 | 0.94 | 0.68, 1.31 | 4 | 16.0 | 0.46 | 0.15, 1.35 | 0.59 | 0.22, 1.58 |
| Total | 380 | 6.4 | 31 | 24.0 | ||||||||
| Men 59–61 | ||||||||||||
| Low | 129 | 20.5 | 1.00 | Ref | 1.00 | Ref | 36 | 49.3 | 1.00 | Ref | 1.00 | Ref |
| Middle | 243 | 18.0 | 0.88 | 0.73, 1.06 | 0.90 | 0.74, 1.09 | 46 | 43.8 | 0.89 | 0.65, 1.22 | 0.92 | 0.65, 1.29 |
| High | 131 | 16.0 | 0.78 | 0.63, 0.97 | 0.84 | 0.67, 1.05 | 26 | 49.1 | 0.99 | 0.69, 1.43 | 1.09 | 0.74, 1.60 |
| Total | 503 | 18.0 | 108 | 46.8 | ||||||||
| Women 40–41, 45–46 | ||||||||||||
| Low | 43 | 5.7 | 1.00 | Ref | 1.00 | Ref | 11 | 34.4 | 1.00 | Ref | 1.00 | Ref |
| Middle | 159 | 3.9 | 0.68 | 0.49, 0.95 | 1.02 | 0.71, 1.47 | 12 | 19.7 | 0.57 | 0.28, 1.15 | 0.66 | 0.32, 1.35 |
| High | 63 | 2.3 | 0.41 | 0.28, 0.59 | 1.01 | 0.66, 1.56 | 8 | 23.5 | 0.68 | 0.31, 1.49 | 1.20 | 0.48, 3.03 |
| Total | 265 | 3.5 | 31 | 24.4 | ||||||||
| Women 59–61 | ||||||||||||
| Low | 136 | 16.7 | 1.00 | Ref | 1.00 | Ref | 19 | 30.2 | 1.00 | Ref | 1.00 | Ref |
| Middle | 250 | 15.0 | 0.90 | 0.74, 1.09 | 1.13 | 0.91, 1.37 | 24 | 28.9 | 0.96 | 0.58, 1.59 | 1.15 | 0.69, 1.92 |
| High | 86 | 11.0 | 0.66 | 0.51, 0.85 | 0.97 | 0.75, 1.26 | 9 | 40.9 | 1.36 | 0.72, 2.54 | 1.94 | 0.98, 3.81 |
| Total | 472 | 14.4 | 52 | 31.0 | ||||||||
| Total – adjusted for sex and age | ||||||||||||
| Low | 365 | 12.6 | 1.00 | Ref | 1.00 | Ref | 73 | 38.8 | 1.00 | Ref | 1.00 | Ref |
| Middle | 880 | 8.4 | 0.86 | 0.77, 0.96 | 1.00 | 0.89, 1.12 | 102 | 30.6 | 0.83 | 0.65, 1.06 | 0.94 | 0.73, 1.21 |
| High | 375 | 6.0 | 0.64 | 0.55, 0.73 | 0.91 | 0.79, 1.05 | 47 | 35.1 | 0.94 | 0.70, 1.26 | 1.35 | 1.00, 1.81 |
| Total | 1620 | 8.3 | 222 | 33.9 | ||||||||
Crude and adjusted relative risk (RR) of starting statin treatment in two subgroups stratified by age and sex.
Education: low, no, primary or lower secondary; middle, higher secondary or high school; high, college/university.
Adjusted for serum total cholesterol and high-density lipoprotein-cholesterol, systolic blood pressure, treatment for hypertension, body mass index, family history of coronary heart disease, daily smoking, physical activity, marital status and county of residence. Adjusted values were based on participants with complete data.
Of the 655 participants who reported a history of CVD or diabetes at baseline, 222 (34%) became statin users. There were no significant associations with level of education in crude analyses. A borderline significant positive effect was seen in the highest education group of women aged 59–61 years after adjustment (RR = 1.94; 95% CI 0.98, 3.81). Overall, RR of becoming a statin user was 0.94 in the highest educational group vs. the lowest educated, adjusted for age and sex, increasing to 1.35 (95% CI 1.00, 1.81) after further adjustment for known cardiovascular risk factors.
Table 3 shows the Poisson regression models including all covariates for each subgroup and for the total. Women had lower probability of statin treatment than men after adjustment in both subgroups (Table 3). At each educational level the probability of statin treatment increased by level of total cholesterol in unadjusted analyses (Figure 1). The probability was doubled per 1 mmol l−1 increase in serum total cholesterol (Table 3) in adjusted analyses of the non-CVD/diabetes group. A lower relative increase was seen in the CVD/diabetes group. Serum HDL-cholesterol showed a negative association with probability of statin treatment in both groups. There was a positive association with triglycerides in crude analyses, which was attenuated and turned nonsignificant after inclusion of HDL-cholesterol (not shown). Furthermore, inclusion of triglycerides did not influence the association between education and use of statins, and was therefore omitted from the multiple regression models. Medication for hypertension and family history of CHD were both highly significant predictors in both groups. Other significant predictors were SBP and smoking in the non-CVD/diabetes and marital status in the CVD/diabetes group. Participants with a history of CVD or diabetes had an almost three times higher probability of starting statin treatment compared with those with no such history (Table 3).
Table 3.
Adjusted relative risk (RR) of starting statin treatment among participants in population-based studies 2000–2002, who reported never use of statins at baseline
| Non-CVD/diabetes group (n #x003D; 18 547†) | CVD/diabetes group (n = 609†) | Total (n = 19 156†) | ||||
|---|---|---|---|---|---|---|
| Covariate | RR‡ | 95% CI | RR‡ | 95% CI | RR‡ | 95% CI |
| Education*: | ||||||
| Low | 1.00 | Ref | 1.00 | Ref | 1.00 | Ref |
| Middle | 1.00 | 0.89, 1.12 | 0.94 | 0.73, 1.21 | 0.99 | 0.89, 1.11 |
| High | 0.91 | 0.79, 1.05 | 1.35 | 1.00, 1.81 | 0.95 | 0.83, 1.08 |
| Women vs. men | 0.85 | 0.77, 0.93 | 0.82 | 0.66, 1.04 | 0.84 | 0.77, 0.93 |
| Age 59–61 vs. 40–46 | 1.91 | 1.72, 2.14 | 1.39 | 1.06, 1.82 | 1.88 | 1.69, 2.08 |
| CVD/diabetes vs. non-CVD/diabetes | – | – | – | – | 2.81 | 2.45, 3.22 |
| Serum total cholesterol per mmol l−1 | 1.98 | 1.91, 2.06 | 1.36 | 1.22, 1.51 | 1.93 | 1.86, 2.00 |
| HDL-cholesterol per mmol l−1 | 0.47 | 0.40, 0.54 | 0.43 | 0.30, 0.62 | 0.46 | 0.40, 0.53 |
| Systolic blood pressure per 10 mmHg | 1.13 | 1.10, 1.15 | 1.05 | 0.99, 1.12 | 1.12 | 1.10, 1.15 |
| Medication for hypertension at baseline vs. no medication | 1.63 | 1.42, 1.88 | 1.33 | 1.06, 1.67 | 1.56 | 1.38, 1.76 |
| BMI per 5 kg m−2 | 1.05 | 0.99, 1.11 | 0.97 | 0.86, 1.10 | 1.04 | 0.98, 1.10 |
| Family history yes vs. no | 1.43 | 1.30, 1.56 | 1.28 | 1.03, 1.59 | 1.41 | 1.29, 1.53 |
| Smoking yes vs. no | 1.21 | 1.10, 1.34 | 1.14 | 0.90, 1.44 | 1.21 | 1.10, 1.32 |
| Physical active vs. inactive | 0.95 | 0.85, 1.05 | 1.09 | 0.87, 1.37 | 0.96 | 0.87, 1.06 |
| Married yes vs. no | 1.07 | 0.97, 1.19 | 1.32 | 1.05, 1.68 | 1.10 | 1.01, 1.21 |
Separate models for two subgroups and the total.
Education: low, no, primary or lower secondary; middle, higher secondary or high school; high, college/university.
Only participants with complete data.
Adjusted for all covariates in the model and county of residence. CVD, cardiovascular disease; HDL, high-density lipoprotein; BMI, body mass index.
Figure 1.
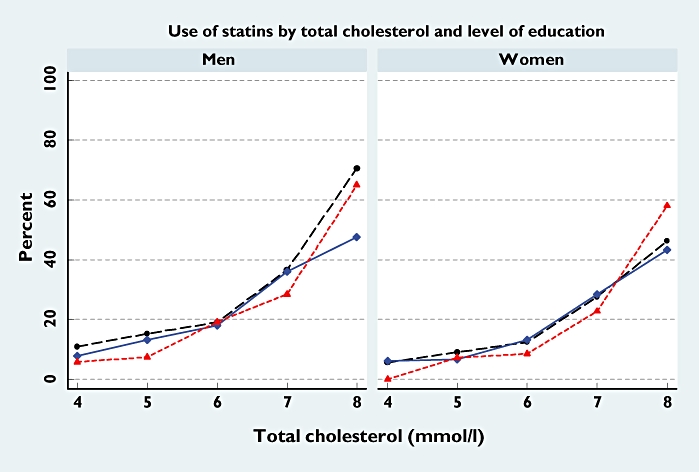
Probability of statin treatment in 2004–2006 according to total cholesterol at baseline in 2000–2002 and educational level (low, primary or lower secondary; middle, higher secondary or high school; high, college/university); 2800 men and 3268 women aged 59–61 years at baseline who reported never use of statins and no history of cardiovascular disease or diabetes at baseline. Low ( ); Middle (
); Middle ( ); High (
); High ( )
)
The mean number of statin prescriptions dispensed during 2004–2006 was seven in the non-CVD/diabetes group and eight in the CVD/diabetes group (Table 4). The distribution of number of prescriptions did not vary significantly between educational groups. Additional analyses showed that 57% of statin users in the non-CVD/diabetes group were prescribed a statin in 2004 compared with 67% in the CVD/diabetes group, with no variation by education. Eighty-eight percent of the statin users in 2004 had a statin prescribed in 2006 in the non-CVD/diabetes group compared with 87% in the CVD/diabetes group with no variation between educational groups (data not shown).
Table 4.
Number of statin prescriptions dispensed in the period 2004–2006 among study participants (n = 1842), by level of education and subgroup
| Number of statin prescriptions dispensed | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group/ | 1 | 2–9 | 10+ | |||||
| Education† | n | % | n | % | n | % | Mean | n |
| Non-CVD/diabetes | ||||||||
| Low | 47 | 12.9 | 189 | 51.8 | 129 | 35.3 | 7 | 365 |
| Middle | 113 | 12.8 | 478 | 54.3 | 289 | 32.8 | 7 | 880 |
| High | 36 | 9.6 | 204 | 54.4 | 135 | 36.0 | 7 | 375 |
| Total | 196 | 12.1 | 871 | 53.8 | 553 | 34.1* | 7 | 1620 |
| CVD/diabetes | ||||||||
| Low | 11 | 15.1 | 26 | 35.6 | 36 | 49.3 | 9 | 73 |
| Middle | 9 | 8.8 | 50 | 49.0 | 43 | 42.2 | 8 | 102 |
| High | 6 | 12.8 | 22 | 46.8 | 19 | 40.4 | 7 | 47 |
| Total | 26 | 11.7 | 98 | 44.1 | 98 | 44.1* | 8 | 222 |
Pearson χ2: P (independence) = 0.4.
Education: low, no, primary or lower secondary; middle, higher secondary or high school; high, college/university. CVD, cardiovascular disease.
Discussion
In the non-CVD/diabetes group the highest educated participants had the lowest probability of statin treatment. The educational differences disappeared after adjustment for known cardiovascular risk factors at baseline. There was no significant association with level of education in crude analyses of the CVD/diabetes group, but a borderline significant positive association after adjustment for cardiovascular risk factors.
Most study participants belonged to the non-CVD/diabetes group. Cross-sectional analyses of the Oslo Study 2000–2001 and the Tromsø Study 2001 have shown that educational level was associated with lower self-reported use of statins in primary prevention [17, 18]. We have extended the results to longitudinal analyses, and demonstrated that the association with education could be explained by different cardiovascular risk profiles at baseline. The main strength of our study is that we could adjust for risk factors obtained before initiation of statin treatment. A recent Swedish study has shown a lower prevalence of statin prescribing at higher level of education, in accordance with our findings [19]. It was not, however, possible to adjust for cardiovascular risk factors or compare use in subgroups in the Swedish study.
Level of education could influence the decision to start statin medication in different ways. Highly educated people may be more aware of their own health and new treatments, probably leading to a more positive attitude towards treatment if the attributed risk reductions are perceived to be large. People with high education may also be more likely to follow lifestyle recommendations in order to reduce cardiovascular risk, which would reduce their need for statin treatment. A sample of participants in a health survey in the county of Finnmark in northern Norway was randomly presented different hypothetical scenarios regarding risk reduction benefits of medical therapies [20]. In this study consent to therapy decreased by length of education. However, whether the response to hypothetical scenarios would reflect decisions in real life is not known. Our results indicate that the probability of being a statin user depends on overall cardiovascular risk factors, with no effect of education in people with no history of CVD or diabetes.
In the Tromsø Study in 2001 only 50% of participants with a history of CHD reported use of statins at screening [18]. In the Oslo Study 2000–2001 45% of men and 35% of women with a history of CVD or diabetes reported use of statins [17]. Percent statin users did not vary by educational level in these two studies. In the present longitudinal study there were no educational differences in unadjusted analyses of the CVD/diabetes group. A borderline significant positive association was seen after adjustment. This effect was mainly seen in women. Highly educated women may be more aware of their own health and new treatments than women of low educational level. However, it may be questioned if it is appropriate to adjust for risk factors in the CVD/diabetes group. According to European guidelines, all patients with established CHD or diabetes should be treated independent of risk factors. Our results suggest that cardiovascular risk factors are independent predictors of statin use in the CVD/diabetes group, although with a lower RR than in the non-CVD/diabetes group.
A cross-sectional Danish study has demonstrated a socioeconomic gradient in use of statins in men, with a higher proportion of statin users among top managers than among basic-level workers [21]. A longitudinal study in Denmark of patients discharged from hospital after myocardial infarction showed that patients with low income less frequently initiated statin treatment than patients with high income [22]. There are several differences between Denmark and Norway. The use of statins is higher in Norway than in Denmark [7] and the reimbursement regulations have been different. Denmark had a restrictive reimbursement policy for statins when the study was performed in 1995–1999, which could probably explain the differences in the socioeconomic gradient. In Norway the costs of statin use are mainly covered by the Norwegian National Insurance Administration through the reimbursement scheme system [23]. The total population in Norway is covered by this tax-supported insurance programme. The aim of the reimbursement policy in Norway is that everyone with chronic diseases should have the same access to pharmaceuticals independent of socioeconomic status. Medications used for treatment of hypercholesterolaemia in a high-risk population are included in this reimbursement system. Our results indicate that there is no educational gradient in use of statins in Norway in participants with no history of CVD or diabetes, but a borderline significant positive effect was seen in the CVD/diabetes group after adjustment for known cardiovascular risk factors.
As expected, serum total cholesterol and HDL-cholesterol were the main predictors of statin use. Similar to the former cross-sectional study in Oslo [17], treatment for hypertension and family history were important predictors in both the non-CVD/diabetes group and the CVD/diabetes group. SBP and self-reported daily smoking were positive predictors of starting statin treatment in the non-CVD/diabetes group, indicating that overall risk is taken into account [4]. The association was weak, however, with only 13% increase per 10 mmHg increase in SBP and 21% higher probability of becoming a statin user among smokers than nonsmokers.
The number of statin prescriptions dispensed in the period 2004–2006 was higher in the CVD/diabetes than in the non-CVD/diabetes group, but similar in all educational groups. As a higher proportion in the CVD/diabetes group was using statins in 2004, this explains the overall higher number of prescriptions in this group. Persistence of statin treatment is generally high in Norway. Of patients receiving a statin in 2005, 92% had a statin prescription dispensed also in 2006 (S. Sakshaug, personal communication). In our study 87–88% of statin users in 2004 in both subgroups had a statin prescribed in 2006 and there was no educational difference. Our results indicate that persistence and number of prescriptions do not vary by level of education.
A couple of weeks after health examination all participants received written feedback on their cardiovascular risk profiles. Individuals with calculated high risk were recommended to visit their physician. There is a time gap between baseline (2000–2002) and outcome measures in NorPD (2004–2006). Unfortunately, we do not know exactly when statin treatment was initiated and how the risk factors have changed during follow-up (e.g. new cardiovascular events, lifestyle interventions), but this lack of information has probably not influenced the educational comparisons.
Our cohort covers both urban and rural areas in north and south and is thus fairly representative of the Norwegian population. We have compared 3-year prevalence of statin use among the health survey participants with 3-year total prevalence 2004–2006 in Norway for the same age groups. The prevalence was almost similar. The overall response rate was 53% in the health surveys. Nonresponse analyses in the Oslo Health Study showed that participants had a slightly higher education than nonparticipants. Selection bias may occur in association studies due to selective attendance [24]. We have made sensitivity analyses assuming that attendance varied by level of education, as in the Oslo Health Study. If we further assumed that the ratio between attendance among new statin users and non-users was the same within each educational group, there was no or negligible bias in RRs. A related problem to selective attendance is potential bias due to exclusion of participants with missing covariates in multivariate analyses. Additional crude analyses of the reduced dataset gave similar results, indicating no bias due to missing covariates. In sum, any lack of representativeness, selective attendance or missing covariates have probably not influenced the comparison between educational groups in any important way.
In this study we included only participants with self-reported no use of statins at baseline 2000–2002. A validity study of the drug questions has shown that the item response rates among participants reporting use of cholesterol-lowering drugs or antihypertensives were nearly 100% [11]. This means that the answers from participants reporting present or former statin use are probably valid. We cannot exclude the possibility that some participants may have been included because they incorrectly reported no use of statins at baseline. If the misreport was higher in participants with low education, this may have influenced the association between statin use and education. The outcome measure is retrieved from the NorPD and is not influenced by recall bias.
Conclusion
Highly educated people with no history of CVD or diabetes had lower probability of statin treatment than people of low educational level, corresponding to their better cardiovascular risk profile. At similar levels of known cardiovascular risk factors there was a tendency to more statin use among highly educated people compared with those of low educational level in the CVD/diabetes group, in particular for women.
Competing interests
None to declare.
Sources of funding: Norwegian Institute of Public Health and The Research Council of Norway.
REFERENCES
- 1.Mackenbach JP, Bos V, Andersen O, Cardano M, Costa G, Harding S, Reid A, Hemström Ö, Valkonen T, Kunst AE. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32:830–7. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 2.Strand BH, Tverdal A. Can cardiovascular risk factors and lifestyle explain the educational inequalities in mortality from ischaemic heart disease and from other heart diseases? 26 year follow up of 50,000 Norwegian men and women. J Epidemiol Community Health. 2004;58:705–9. doi: 10.1136/jech.2003.014563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strand BH, Tverdal A. Trends in educational inequalities in cardiovascular risk factors: a longitudinal study among 48,000 middle-aged Norwegian men and women. Eur J Epidemiol. 2006;21:731–9. doi: 10.1007/s10654-006-9046-5. [DOI] [PubMed] [Google Scholar]
- 4.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori S, Pyörälä K, Reiner Z, Ruilope L, Sans-Menendez S, Reimer W, Weissberg P, Wood D, Yarnell J, Zamarano J. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur J Cardiovasc Prev Rehabil. 2007;14:E1, 40. doi: 10.1097/01.hjr.0000277984.31558.c4. [DOI] [PubMed] [Google Scholar]
- 5.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 6.Abramson J, Wright JM. Are lipid-lowering guidelines evidence-based? Lancet. 2007;369:168–9. doi: 10.1016/S0140-6736(07)60084-1. [DOI] [PubMed] [Google Scholar]
- 7.Nomesco. Health Statistics in the Nordic Countries 2006. Copenhagen, Denmark: Nomesco; 2008. [19 December 2008]. p. 208. Available at http://nomesco-eng.nom-nos.dk/default.asp?side=88. [Google Scholar]
- 8.Walley T, Folino-Gallo P, Stephens P, Van Ganse E. Trends in prescribing and utilization of statins and other lipid lowering drugs across Europe 1997–2003. Br J Clin Pharmacol. 2005;60:543–51. doi: 10.1111/j.1365-2125.2005.02478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Næss O, Søgaard AJ, Arnesen E, Beckstrøm AC, Bjertness E, Engeland A, Hjort PF, Holmen J, Magnus P, Njølstad I, Tell GS, Vatten L, Vollset SE, Aamodt G. Cohort profile: cohort of Norway (CONOR) Int J Epidemiol. 2008;37:481–5. doi: 10.1093/ije/dym217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CONOR questions. [19 December 2008]; Available at http://www.fhi.no/dav/6feb85397d.xls.
- 11.Furu K, Skurtveit S, Rosvold E. Drug use questions in Norwegian health surveys—response rate and agreement between specific and open-ended questions. Nor J Epidemiol. 2003;13:147–54. [Google Scholar]
- 12.Education register- Statistics Norway. [19 December 2008]. Available at http://www.ssb.no/english/subjects/04/01/utniv_en/
- 13.Norwegian Prescription Database. [19 December 2008]; Available at http://www.norpd.no/
- 14.Furu K. Establishment of the nationwide Norwegian Prescription Database (NorPD) – new opportunities for research in pharmacoepidemiology in Norway. Nor J Epidemiol. 2008;18:129–36. [Google Scholar]
- 15.Guidelines for ATC Classification and DDD Assignment 2008. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology; 2007. [Google Scholar]
- 16.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 17.Tonstad S, Rosvold EO, Furu K, Skurtveit S. Undertreatment and overtreatment with statins: the Oslo Health Study 2000–2001. J Intern Med. 2004;255:494–502. doi: 10.1111/j.1365-2796.2004.01315.x. [DOI] [PubMed] [Google Scholar]
- 18.Hartz I, Eggen AE, Grimsgaard S, Skjold F, Njølstad I. Whom are we treating with lipid-lowering drugs? Are we following the guidelines? Evidence from a population-based study: the Tromsø study 2001. Eur J Clin Pharmacol. 2004;60:643–9. doi: 10.1007/s00228-004-0827-z. [DOI] [PubMed] [Google Scholar]
- 19.Weitoft GR, Rosen M, Ericsson O, Ljung R. Education and drug use in Sweden – a nationwide register-based study. Pharmacoepidemiol Drug Saf. 2008;17:1020–8. doi: 10.1002/pds.1635. [DOI] [PubMed] [Google Scholar]
- 20.Halvorsen PA, Selmer R, Kristiansen IS. Different ways to describe the benefits of risk-reducing treatments: a randomized trial. Ann Intern Med. 2007;146:848–56. doi: 10.7326/0003-4819-146-12-200706190-00006. [DOI] [PubMed] [Google Scholar]
- 21.Thomsen RW, Johnsen SP, Olesen AV, Mortensen JT, Boggild H, Olsen J, Sørensen HT. Socioeconomic gradient in use of statins among Danish patients: population-based cross-sectional study. Br J Clin Pharmacol. 2005;60:534–42. doi: 10.1111/j.1365-2125.2005.02494.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rasmussen JN, Gislason GH, Rasmussen S, Abildstrøm SZ, Schramm TK, Køber L, Diderichsen F, Osler M, Torp-Pedersen C, Madsen M. Use of statins and beta-blockers after acute myocardial infarction according to income and education. J Epidemiol Community Health. 2007;61:1091–7. doi: 10.1136/jech.2006.055525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haga A, Sverre JM. Pricing and reimbursement of pharmaceuticals in Norway. Eur J Health Econ. 2002;3:215–20. doi: 10.1007/s10198-002-0135-4. [DOI] [PubMed] [Google Scholar]
- 24.Kleinbaum DG, Kupper LL, Morgenstern H, editors. Epidemiologic Research – Principles and Quantitative Methods. New York: Van Nostrand Reinhold; 1982. Selection bias; –194.pp. 219 [Google Scholar]


